Where Resistance Spreads: Your Community

Germs are part of everyday life. Many germs do not cause harm and some even help us stay healthy. Only a small portion of germs are known to cause infection. Unfortunately, there have been rising antimicrobial-resistant infections in U.S. communities.
CDC is concerned about antimicrobial-resistant germs in the community for several reasons.
- Community-associated infections can happen to healthy people who have not had a recent interaction with health care (healthcare-associated germs tend to impact sicker, more vulnerable people while they receive care)
- Infections in the community can be difficult to identify and control spread
- New forms of resistance can emerge and spread quickly, especially resistance shared among germs through mobile genetic elements
- Antimicrobial-resistant germs can share their resistance genes with other germs, making them more difficult to treat
We can slow the spread of resistant threats in the community using simple interventions, such as good hygiene, routine vaccination, safer sex practices, and safe food preparation. Many of these interventions have already proven successful. Learn more about steps everyone can take to reduce your risk of getting an infection.
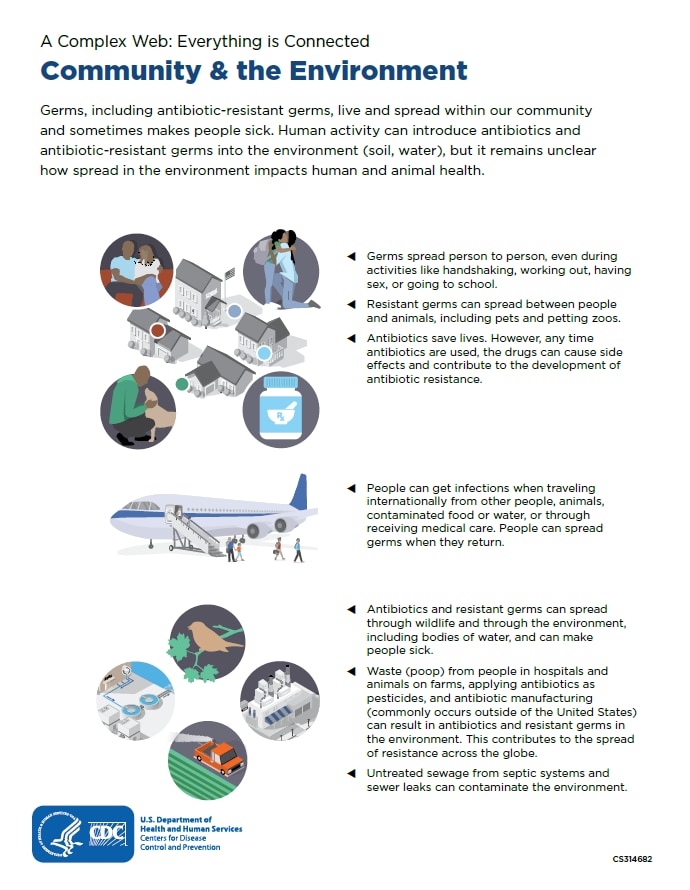
How Germs Can Spread in Community
Germs, including resistant germs, can spread between people, animals, and food, through common activities. For example, germs can spread from food to people and between people and animals without appropriate hand hygiene. People can also get an infection when traveling, then spread these germs when they return. Other examples include gonorrhea, a common sexually transmitted disease (STD) that has progressively developed resistance to almost every drug ever used to treat it. Infections associated with drug-resistant gonorrhea and group A Streptococcus, the most common cause of sore throat, have both increased since 2000.
About Antibiotic/Antifungal Use in Communities
Antibiotics and antifungals are valuable tools. However, any use — for people, animals, or plants—can cause side effects and contribute to antimicrobial resistance.
In U.S. outpatient doctors’ offices and emergency departments, at least 28% of antibiotic courses prescribed each year are unnecessary. In U.S. outpatient doctors’ offices specifically, 1 out of every 3 antibiotic drugs prescribed is unnecessary. That’s 47 million unnecessary prescriptions, each of which carries the potential for side effects, allergic reactions and Clostridioides difficile infections, which can cause deadly diarrhea.
In the community, reactions from antibiotics often require emergency treatment. In fact, reactions from antibiotics cause 1 out of 5 medication-related visits to the ER. In children, reactions from antibiotics are the most common cause of medication-related ER visits.
Download a printable fact sheet highlighting information on this webpage: Everything is Connected: Community & the Environment [PDF – 1 page].
COVID-19 Impacts Antimicrobial Resistance
Much of the U.S. progress in combating antimicrobial resistance was lost in 2020, in large part, due to the effects of the COVID-19 pandemic. The pandemic pushed healthcare facilities, health departments, and communities near their breaking points.
Find out more about the impact of COVID-19 on antimicrobial resistance in the U.S.
Misuse or mismanagement of antibiotics and antifungals can also contribute to resistance. For example, people with tuberculosis (TB)—a disease caused by bacteria that are spread from person to person through the air—can die if they do not get proper treatment. Drug-resistant TB can occur when the drugs used to treat TB are misused or mismanaged.
Clinicians should prescribe their patients antibiotics and antifungals only when the benefits outweigh the potential risks. Veterinarians can also help improve antibiotic or antifungal use when prescribing these drugs. Improving prescribing and use is critical to effectively treat infections, protect patients from harms, and combat antimicrobial resistance.