Cancer and COVID-19
If you have cancer, COVID-19 can make you very sick. Treatments for many types of cancer can weaken your body’s ability to fight off infections. Studies show that having a history of cancer may also increase your risk of serious illness and death from COVID-19.
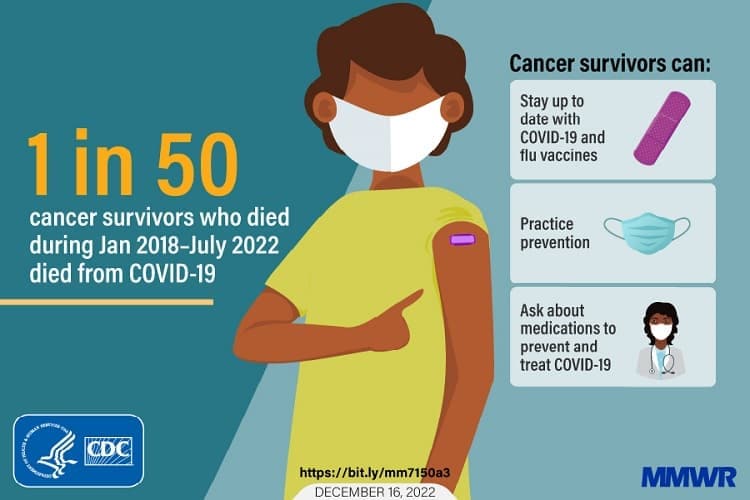
One study looked at COVID-19 and cancer deaths. Findings from the study show that—
- Many people with cancer died due to COVID-19 and other diseases during the pandemic. A higher number of deaths occurred during peaks in COVID-19 infections.
- In 2021, a higher percentage of cancer deaths with COVID-19 as the underlying cause occurred among non-Hispanic American Indian and Alaska Native people, Hispanic and Latino people, and non-Hispanic Black people compared with members of other racial and ethnic groups.
Studies Show Effects on Cancer Screening
Many preventive services, including cancer screenings, were put on hold because of the pandemic. Scientists in CDC’s Division of Cancer Prevention and Control have done research to find out how the COVID-19 pandemic has affected cancer screening.
One study looked at whether the COVID-19 test positivity was linked to changes in cancer screening among women in CDC’s National Breast and Cervical Cancer Early Detection Program. The study found that—
- During April 2020, breast and cervical cancer screening declined by 87% and 84%, respectively, compared with the previous 5-year average for that month.
- Some states were able to screen as many people during the pandemic as they did before the pandemic. Further studies will be done to find out how.
A previous study on CDC’s National Breast and Cervical Cancer Early Detection Program looked at breast and cervical cancer screening by race and ethnicity. From January through June 2020, the largest decreases in screening were among American Indian and Alaska Native women for breast cancer screening (98% decline) and Asian and Pacific Islander women for cervical cancer screening (92% decline), compared with the previous 5-year averages.
Previous studies have shown that breast cancer deaths among women in the United States have dropped, but non-Hispanic Black women have higher death rates. CDC scientists conducted a study to look for changes in these trends. They found that—
- Overall, breast cancer death decreased from 1999 to 2020. But rates decreased less in recent years, from 2008 to 2020, than they did from 2002 to 2008.
- Compared to women in other racial and ethnic groups, non-Hispanic Black women had the highest breast cancer death rates.
Another CDC-authored study found that cervical cancer screening dropped 80% among about 1.5 million women in the Kaiser Permanente Southern California network during California’s stay-at-home order.
Guidance to Prevent COVID-19 and Other Illnesses
CDC offers guidance on what cancer survivors, their families, and caregivers can do to lower their risk of getting COVID-19 and other illnesses.
People Who Are Immunocompromised explains that some people who are immunocompromised (have a weakened immune system), including some cancer patients, are more likely to get sick with COVID-19 or be sick for a longer period.
Preventing Infections in Cancer Patients explains how cancer patients can avoid life-threatening infections during chemotherapy treatment. People with cancer who are treated with chemotherapy are more likely to get infections because cancer and chemotherapy can damage their immune system.
Programs Overcome Challenges to Cancer Screening
Despite the challenges, CDC-funded programs found ways to provide cancer screening during the COVID-19 pandemic. Some of this work is highlighted here.
- The Inter-Tribal Council of Michigan started the Three Fires Cancer Consortium to help American Indian people in the state get services that help prevent and find cancer early. Colorectal cancer is a leading cause of cancer death in Michigan, and screening dropped sharply during the early months of the COVID-19 pandemic. Tribal health clinics used education and patient reminders to reach out to patients about the importance of colorectal cancer screening, even during the pandemic. The number of patients up to date on colorectal cancer screening increased from about 62% in July 2020 to almost 67% in June 2021.
- San Juan Basin Public Health is a public health agency serving residents of rural southwestern Colorado. Hispanic women with low incomes living in these counties have trouble getting health care. Few clinics provide interpreters, help with scheduling an appointment, or information about financial assistance. These services became even more important during the COVID-19 pandemic. The clinic worked with organizations that serve the Hispanic community to connect women with health care, housing, food, transportation, and other financial assistance during the pandemic.
Cancer Survivor Stories: Treatment and Staying Healthy
April Donaldson was diagnosed with and treated for breast cancer during the COVID-19 pandemic. In her blog post, she says, “It really felt like trying to battle two monsters at the same time… While COVID is deadlier for people with a lower immune system, so is cancer when left untreated.”
David Brown, a colon cancer survivor, shared his blog post about why physical distancing has been his biggest challenge during the pandemic. “I am a people person who enjoys shaking hands, high fives, fist bumps, handshakes, and hugs,” he said.