
National Veterans Health Administration MOVE! Weight Management Program Participation During the COVID-19 Pandemic
ORIGINAL RESEARCH — Volume 19 — March 10, 2022
Kristen E. Gray, PhD, MS1,2; Katherine D. Hoerster, PhD, MPH1,2,3,4; Stephanie A. Spohr, PhD, MA5; Jessica Y. Breland, PhD6; Susan D. Raffa, PhD5,7 (View author affiliations)
Suggested citation for this article: Gray KE, Hoerster KD, Spohr SA, Breland JY, Raffa SD. National Veterans Health Administration MOVE! Weight Management Program Participation During the COVID-19 Pandemic. Prev Chronic Dis 2022;19:210303. DOI: http://dx.doi.org/10.5888/pcd19.210303.
PEER REVIEWED
What is already known on this topic?
The COVID-19 pandemic has affected physical activity and eating behaviors, resulting in weight gain. Health systems may be able to address this problem through behavioral weight management. Little is known about the pandemic’s effects on participation in weight management programs.
What is added by this report?
In the Veterans Health Administration, in-person weight management participation declined sharply because of COVID-19, whereas telehealth participation increased, accounting for 90% of participation during the pandemic versus 20% to 30% before. Total participation remained substantially lower into 2021 compared with prior years.
What are the implications for public health practice?
The demand for weight management services may increase in the postpandemic recovery period, which could be met by health care systems offering telehealth or hybrid options.
Abstract
Introduction
In response to COVID-19, the Veterans Health Administration (VHA) converted appropriate outpatient visits to virtual care, including MOVE! Weight Management Program for Veterans (MOVE!) visits. Before the pandemic, most veterans participated in MOVE! in person, with several telehealth modalities available. We sought to describe national trends in MOVE! participation during the pandemic (March 2020–January 2021) overall and by modality and to compare participation to prepandemic levels.
Methods
We conducted a national retrospective cohort study of veterans who participated in MOVE! from January 2018 through January 2021. We examined MOVE! participation across VHA aggregated at the national level by month, including the number of visits, participants, and new participants in person and via telehealth, including telephone, clinic-to-clinic synchronous video, anywhere-to-anywhere (eg, provider home to patient home) synchronous video, and remote education and monitoring. We also determined the percentage of all MOVE! visits attributable to each modality and the monthly percentage change in participation during the pandemic compared with monthly averages in prior years.
Results
Before March 2020, 20% to 30% of MOVE! was delivered via telehealth, which increased to 90% by April 2020. Early in the pandemic, telephone-delivered MOVE! was the most common modality, but anywhere-to-anywhere synchronous video participation increased over time. Compared with the same months in prior years, total monthly MOVE! participation remained 20% to 40% lower at the end of 2020 and into January 2021.
Conclusion
The VHA MOVE! program rapidly shifted to telehealth delivery of weight management services in response to the pandemic. However, a gap remained in the number of veterans receiving these services compared with prior years, suggesting potential unmet needs for weight management.
Introduction
Since 2006, the Veterans Health Administration (VHA) has offered the MOVE! Weight Management Program for Veterans (MOVE!) to veterans receiving care at all facilities to support the more than 80% who have a body mass index (BMI) of 25 or more (1). MOVE! is an evidence-based comprehensive lifestyle intervention combining dietary, physical activity, and behavioral strategies targeting clinically meaningful weight loss (≥5%) delivered in individual or group formats. Patients can participate in person or by using various technologies, including telephone, video conferencing, in-home monitoring with support, and a self-directed mobile app (2,3). MOVE! is effective, resulting in weight loss of 5% or more among 20% to 25% of participants at 12 months (4); telehealth individual modalities have been as effective as in-person group options (5). Before the COVID-19 pandemic, most MOVE! participation was through in-person group sessions at local VHA facilities. In response to the pandemic, on March 15, 2020, VHA leadership directed all facilities to convert in-person care to virtual care where appropriate (6). As of April 2, 2020, in-person MOVE! visits were suspended nationwide and transitioned to telehealth modalities.
Given that higher BMI is associated with increased risk of severe COVID-19 among veterans with a BMI of 30 or more (7), understanding the effect of the pandemic on weight management is critical for anticipating future behavioral weight management needs. This knowledge will help the VHA and other health care systems better understand how to address future local or national disruptions in care. Despite widespread availability of telehealth weight management options in the VHA, little is known about how the COVID-19 pandemic affected trends in MOVE! participation and the uptake of telehealth modalities. With pandemic-associated unintended weight gains and decreases in physical activity (8), there is likely a greater need for weight management services in the postpandemic recovery period, which telehealth may be well-suited to address. This study aims to 1) describe trends in national MOVE! participation overall and by modality and 2) compare participation with prepandemic levels. We hypothesized that in-person program participation would decrease and telehealth participation would increase.
Methods
We conducted a descriptive retrospective cohort study using VHA clinical and administrative data on MOVE! participation from the VHA Support Service Center MOVE! Visits Report. We examined MOVE! participation aggregated at the national level by month from January 2018 through January 2021. We considered the period of March 2020–January 2021 as “during the pandemic” and before March 2020 as “prepandemic.” This project was considered quality improvement and, per VHA policy, did not require institutional review board approval or waiver. We obtained a nonresearch determination (per VHA Handbook 1058.05) from the VHA National Center for Health Promotion and Disease Prevention.
MOVE! participation
We examined several dimensions of MOVE! participation each month, including the number of MOVE! visits, the number of MOVE! participants, and the number of new MOVE! participants. We identified MOVE!-related visits by clinic stop codes, which are administrative codes for identifying outpatient care. The combination of up to 2 stop codes indicated the MOVE! visit format (group [373] vs individual [372]) and the delivery modality. The combination of visit format and delivery modality resulted in more than 100 different stop code pairs.
We defined delivery modality as in person, telephone, Clinical Video Telehealth (clinic-to-clinic), VHA Video Connect (anywhere-to-anywhere [eg, provider home to veteran home]), or TeleMOVE! home telehealth. We also created a composite telehealth category, which aggregated telephone, Clinical Video Telehealth, VHA Video Connect, and TeleMOVE! home telehealth. Telephone involves delivery of the standard in-person MOVE! curriculum via telephone. Clinical Video Telehealth and VHA Video Connect are synchronous video sessions. TeleMOVE! home telehealth is an individual remote education and monitoring program completed by veterans at home using an in-home messaging device, browser-based technology, or mobile device and scale. Veterans receive daily education and transmit weight and other relevant health data for monitoring by a care coordinator, who assists participants with behavior change.
The number of MOVE! participants can include veterans more than once across stop codes. If a veteran has a MOVE! visit with a different stop code in the same month, they contribute data to each combination of stop codes (eg, to individual in-person visits and individual telephone visits). Therefore, totals summed across modalities will overestimate the unique number of participants in each month. Veterans are considered new MOVE! participants when they make their first ever MOVE! visit, and they are counted only once for this dimension of MOVE! participation.
Data analysis
We examined MOVE! participation from January 2018 through January 2021. We first characterized changes over time in the number of visits, participants, and new participants by MOVE! modality (in-person or telehealth), as well as the monthly distribution of MOVE! participation by modality (eg, percentage of all MOVE! visits attributable to each modality). We further examined trends in participation in each telehealth modality by group format versus individual format. To compare MOVE! participation during the COVID-19 pandemic to typical years, we averaged monthly participation in 2018 and 2019, assigning equal weight to each year, and calculated the percentage change in 2020 relative to the prior years’ average for that month. We calculated percentage change in January 2021 relative to the average across January 2019 and 2020, both of which were in the prepandemic period and were most proximal to January 2021 (vs averaging January 2018 and January 2019 for comparisons). We compared data from the same months in prior years because of seasonal variation in MOVE! participation, which precluded comparing data from the height of the pandemic to the months preceding it.
Results
Visits
We found 695,050 MOVE! visits in 2018, 727,585 visits in 2019, and 489,939 visits in 2020. The monthly number of MOVE! visits began to decline sharply in March 2020 because of declines in in-person visits to a nadir in May 2020 of 30,436 visits across modalities (Figure 1).
![]()
Figure 1.
Trends in national Veterans Health Administration MOVE! Weight Management Program participation by modality, January 2018 through January 2021. A, Number of MOVE! visits. B, Number of MOVE! participants. C, Number of new MOVE! participants. Note that the scale in C differs from the scale in A and B. [A tabular version of this figure is available.]
We found concomitant increases in telehealth MOVE! modalities, particularly individual telephone visits and group VHA Video Connect visits (Figure 2).
![]()
Figure 2.
Trends in national Veterans Health Administration telehealth MOVE! Weight Management Program participation by format (group vs individual) and modality, January 2018 through January 2021. A, Number of MOVE! visits. B, Number of MOVE! participants. C, Number of new MOVE! participants. Note that the scale in C differs from the scale in A and B. Abbreviations: VVC, VHA Video Connect; CVT, Clinical Video Telehealth. [A tabular version of this figure is available.]
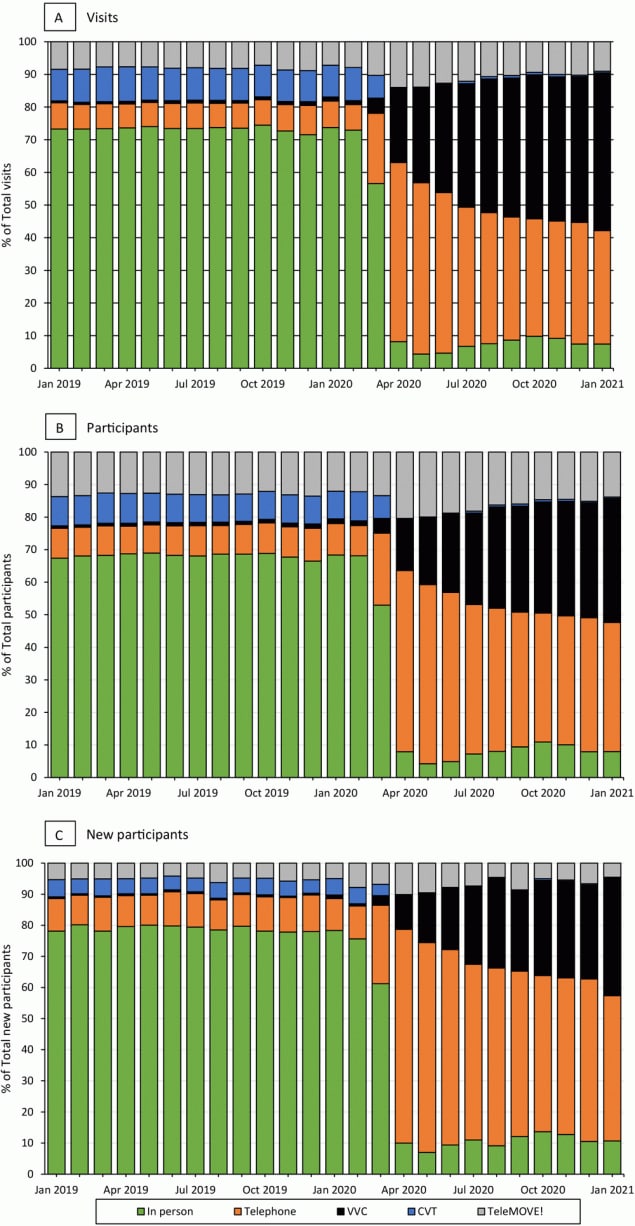
Before March 2020, telehealth modalities made up approximately 30% of MOVE! visits, which then expanded to 90% or more (Figure 3). In the initial months of the pandemic, telephone visits accounted for the largest proportion of visits, but the proportion declined over time, from 54.8% in April 2020 to 34.7% in January 2021, while the proportion of VHA Video Connect visits increased, from 23.0% in April 2020 to 48.3% in January 2021.
![]()
Figure 3.
Distribution of national Veterans Health Administration MOVE! Weight Management Program participation by modality, January 2019 through January 2021. A, MOVE! visits. B, MOVE! participants. C, New MOVE! participants. Abbreviations: VVC, VHA Video Connect; CVT, Clinical Video Telehealth. [A tabular version of this figure is available.]
When compared with the monthly average in the years before the pandemic, the number of visits dropped by more than 50% in April 2020, driven by a 95% decline in in-person visits (Figure 4). In subsequent months, in-person visits remained 92% to 97% lower than averages for corresponding months in previous years. In the same period, telehealth visits increased relative to averages in previous years, with percentage increases ranging from 66% in April to 147% in December 2020. This increase mitigated some of the decline in total MOVE! visits compared with prior years, such that differences in total number of visits generally declined over time from 51% lower in April 2020 compared with averages in April 2019 and 2018 to 35% lower in January 2021 compared with January 2020 and 2019.
![]()
Figure 4.
Monthly percentage change in national Veterans Health Administration MOVE! Weight Management Program participation by modality in January 2020 through January 2021 relative to monthly average in prior years. A, MOVE! visits. B, MOVE! participants. C, New MOVE! participants. Note that the scale in C differs from the scale in A and B. [A tabular version of this figure is available.]
Participants
Trends in the number of participants were similar to trends in the number of visits: declines began in March 2020 for the number of in-person and total participants, with the lowest numbers in May 2020 (Figure 1). The number of telehealth participants increased starting in March 2020 and continued through January 2021, with increases most pronounced in individual telephone participants and group VHA Video Connect participants (Figure 2). Before the pandemic, telehealth accounted for slightly more than 30% of participants in MOVE! but increased to 90% or more after March 2020 (Figure 3). Starting in April 2020, telephone participants accounted for the largest proportion; however, the proportion of VHA Video Connect participants increased over time, from 16% in April 2020 to 38% in January 2021 (Figure 3). Patterns in monthly participants compared with prior years were similar to patterns in visits: total participants declined by nearly 50% for April and May 2020, driven by declines in in-person participants (Figure 4). Compared with averages in prior years, telehealth participants generally increased over time, peaking at 113% in December 2020. In general, deficits compared with previous years became smaller over time, with above-noted 50% fewer total participants in April and May 2020, compared with prior years, down to 28% fewer in January 2021 relative to prior years.
New participants
The number of new MOVE! participants was 51,280 in 2018, 50,930 in 2019, and 36,829 in 2020. Declines in the number of new participants in telehealth and in-person modalities caused by the pandemic reached lows in May 2020 such that only 1,803 patients began MOVE! in that month compared with 4,813 in May 2019 (Figure 1). Increases in telehealth modalities began in March 2020 and continued through January 2021, with the most notable increases among new participants using individual telephone and group VHA Video Connect (Figure 2). Before the pandemic, telehealth accounted for approximately 20% of new participants and increased to 90% from April 2020 onward (Figure 3). Although telephone was the most common modality for new participants throughout the pandemic (69% in April 2020 and 47% in January 2021 [Figure 3]), the share attributable to VHA Video Connect continued to increase over time, from 11% in April 2020 to 38% in January 2021. When comparing the monthly number of new participants to averages in prior years, the nadir was in May 2020, when the number of new participants was 61% of the average across May 2018 and 2019, attributable to a 97% decline in in-person MOVE! relative to prior years (Figure 4). Starting in March 2020, participants seen via telehealth increased substantially, compared with previous years, and peaked at 302% in December 2020. Declines in monthly new participants compared with prior years decreased over time, such that in December 2020, there was a slight increase in new participants relative to December of prior years (2%). However, in January 2021 this dipped back to 22% lower than previous years.
Discussion
We examined national trends in VHA MOVE! Weight Management Program participation before and during the COVID-19 pandemic, from January 2018 through January 2021. As anticipated, we found dramatic declines in MOVE! participation overall, particularly for in-person modalities, beginning in March 2020. This coincided with general national VHA guidance in mid-March 2020 to convert appropriate outpatient appointments to virtual modalities (6) and subsequent MOVE!-specific national guidance to suspend in-person MOVE! visits for at least 30 days. The MOVE! program and providers responded rapidly, with 90% of participation transitioning to telehealth modalities by April 2020. In the initial months of the pandemic, telephone modalities accounted for the greatest proportion of MOVE! participation, but the share of anywhere-to-anywhere synchronous video (VHA Video Connect) participation increased over time. Compared with the same month in prior years, total monthly MOVE! participation (in person and telehealth) was 50% to 60% lower in April and May 2020. After May 2020, deficits relative to prior years generally became smaller over time (eg, approximately 40% lower in July and August 2020). However, MOVE! participation remained 20% to 30% lower in the latter months of 2020 and into January of 2021 compared with the same months in prior years.
The increase in VHA Video Connect participation over time was likely influenced by efforts to educate providers and patients on this newer technology as well as infrastructure improvements to increase bandwidth available for video appointments (6). The high utilization of telephone visits, particularly early in the pandemic, may reflect initial national guidance to use the modality with the lowest technology requirement (such as secure messaging or telephone) unless video visits had been established for MOVE! or a veteran preferred a video visit. Home telehealth (ie, TeleMOVE!) remained relatively stable over time. This stability was likely related to new COVID-19 home telehealth monitoring protocols that were developed and guidance to facilities to consider COVID-19 monitoring needs before enrolling new TeleMOVE! participants. At facilities where clinician resources were limited (eg, MOVE! staff reassigned to provide COVID-19 care), MOVE! teams were encouraged to prioritize telehealth options according to patient need and local context.
Our findings highlight that, although the VHA had existing telehealth infrastructure and programming, MOVE! participation in 2020 was 30% lower than in previous years. Therefore, many patients who would have otherwise received weight management services did not because of the pandemic. Given COVID-19–related declines in physical activity, increases in sedentary behaviors, and changes in eating patterns, there is a pressing need for accessible weight management services now and in the future (9,10). Contributors to changes in health behaviors may include COVID-19 restrictions leading to shifts in routine or access to healthy foods and safe spaces for physical activity (eg, lack of access to gyms or exercise partners). Psychological distress also increased markedly during the pandemic, which may be a factor in worsening activity and eating behaviors, given that conditions such as depression and posttraumatic stress disorder affect health behaviors and weight (10–13). Pandemic-associated stress may also lead patients to prioritize other aspects of their health (eg, coping with distress by eating comfort foods) and lives (eg, virtual schooling of children) over weight management. Related to these and other factors, 42% of US adults reported gaining unwanted weight during the pandemic, with an average gain of 29 pounds (8). With high rates of mental health conditions, food insecurity, and limited social support, veterans may be especially vulnerable to COVID-19–related behavior change and weight gain (14–18). Weight management programs, including MOVE!, may need to incorporate additional strategies to help participants overcome the challenges to modifying health behaviors in the context of heightened pandemic-related stress and anxiety (19).
Our findings also suggest that barriers to telehealth may remain at the patient, provider, or health care system level. One such potential barrier is the lack of technology necessary for telehealth weight management services. The most common telehealth MOVE! modality early in the pandemic was telephone, but use of anywhere-to-anywhere synchronous video increased over time. Veteran preferences for MOVE! participation format and modality during and after the pandemic have not been broadly assessed. However, a survey among 58 veterans who were seen during the pandemic in an intensive weight management clinic that provides interdisciplinary pre- and postbariatric surgery care may provide some insights (20). In that study, half of participants indicated telephone visits were as good as in-person visits, and a similar proportion said they would prefer to have all visits over the telephone even after pandemic-related restrictions to in-person visits were lifted (20). Although participants were not offered video visits, they were queried about preferences for video. Nearly half indicated they would have preferred video to telephone visits if they were available, and 37% endorsed a preference for all video visits after restrictions were lifted (20). A substantial number of veterans lack the technology needed for video visits, including compatible devices or high-speed internet (21). These barriers differentially affect older, unhoused, and rural veterans (22). To address these gaps, the VHA implemented the Digital Divide Consult, which enables patients to obtain internet services or technology needed for VHA telehealth and provides robust technology support and digital skills classes (23). However, the VHA will need to evaluate the extent to which the pandemic exacerbated disparities in access and the success of the Digital Divide Consult in addressing these disparities. Given anticipated long-term shifts toward reliance on telehealth, the VHA must continue to ensure equitable access for all veterans.
Strategies to promote weight management access for VHA patients may include prioritizing a return to face-to-face modalities as soon as it is safe to do so and ensuring safe practices for face-to-face visits, especially group programs, in accordance with local and federal guidance, including use of face masks, social distancing, proper ventilation, hand hygiene, and encouraging vaccination and boosters. Other strategies could include offering hybrid models with in-person and telehealth options; continuing to provide MOVE! via synchronous video and telephone; and expanding self-directed options, like app, online, or DVD-based programs, which have been effective in non-VHA settings and are currently being tested in the VHA (24–26). Offering telehealth or hybrid options may also enhance access to weight management services in non-VHA settings, where telehealth modalities may be less robust than in the VHA. For example, of the nearly 2,000 Centers for Disease Control and Prevention–recognized Diabetes Prevention Programs, which lead to clinically significant weight loss (27), less than one-quarter have telehealth options (28). Health care systems can also consider delivering weight management programs — in person, telehealth, or hybrid — in nontraditional settings, such as within mental health care, to promote access among specific patient populations (29).
Our study has several important strengths and limitations. We had readily available data on a nationally implemented weight management program with hundreds of thousands of visits over several years, allowing for investigation of trends over time. We also had information on types of program participation, including several different telehealth options, which facilitated examination of uptake of individual telehealth modalities before and during the pandemic. Limitations include use of data aggregated at the national level, precluding examination of the influence of patient-, facility-, or regional-level characteristics on MOVE! participation or understanding variation in the effects of COVID-19 on MOVE! participation. Furthermore, our study did not allow for evaluation of patient attitudes about access and preferred modalities, barriers to service delivery, or patient outreach during the pandemic. Future work should seek to understand patient perspectives on weight management program participation during COVID-19 and evaluate facility- and regional-level differences in the effects of COVID-19 on participation. We also were not able to examine trends in self-directed MOVE! participation (eg, the MOVE! app), although there is insufficient evidence to determine whether self-directed weight management programs without a clinical component are as effective as clinical interventions (30). Our findings reflect data from a single large integrated health care system and may not be generalizable to other health care systems or weight management programs, particularly those that did not offer telehealth options before the pandemic. Lastly, information on one dimension of participation — the number of monthly MOVE! participants — was limited by the potential for participants to be counted more than once in a given month if they participated in 2 or more MOVE! modalities or formats. Because of the transition of MOVE! to telehealth in March 2020, patients were more likely to be duplicated in the early months of the pandemic, because they were more likely to participate in more than 1 modality. Relatedly, we could not calculate yearly totals for participants, because individuals would contribute data to each month in which they participated in MOVE!, leading to substantial overestimates of the total annual number of participants.
In this study, we found a rapid transition of the VHA MOVE! Weight Management Program to telehealth modalities at the height of the COVID-19 pandemic. Although the VHA had been delivering MOVE! via telehealth before the pandemic, we found a sizable gap in total MOVE! participation compared with prior years that persisted into January 2021. Findings suggest potential unmet needs for weight management now and into the future, some of which telehealth may be able to address. Additional research is needed to understand whether these gaps continue and the factors driving them (eg, patient-, facility-, and regional-level factors) to promote equitable access to weight management services.
Acknowledgments
This work was supported by Career Development Award number 16-154 (K.E.G.) and number 15-257 (J.Y.B.) from the US Department of Veterans Affairs, Health Services Research and Development Program. The views expressed in this article are those of the authors and do not necessarily reflect the position or policy of the Department of Veterans Affairs or the US government. No copyrighted materials were used in this article.
Author Information
Corresponding Author: Kristen E. Gray, PhD, MS, Core Investigator, Health Services Research & Development, VA Puget Sound Health Care System, Seattle Division, 1660 S Colombian Way, S-152, Seattle, WA 98108. Telephone: 206-764-2056. Email: kristen.gray2@va.gov.
Author Affiliations: 1Health Services Research & Development, VA Puget Sound Health Care System, Seattle Division, Seattle, Washington. 2Department of Health Systems and Population Health, University of Washington School of Public Health, Seattle, Washington. 3Mental Health Service, VA Puget Sound Health Care System, Seattle Division, Seattle, Washington. 4Department of Psychiatry and Behavioral Sciences, University of Washington, Seattle, Washington. 5National Center for Health Promotion and Disease Prevention, Veterans Health Administration, Durham, North Carolina. 6Center for Innovation to Implementation, VA Palo Alto Health Care System, Palo Alto, California. 7Department of Psychiatry & Behavioral Sciences, Duke University School of Medicine, Durham, North Carolina.
References
- Breland JY, Phibbs CS, Hoggatt KJ, Washington DL, Lee J, Haskell S, et al. The obesity epidemic in the Veterans Health Administration: prevalence among key populations of women and men veterans. J Gen Intern Med 2017;32(Suppl 1):11–7. CrossRef PubMed
- Chan SH, Raffa SD. Examining the dose-response relationship in the Veterans Health Administration’s MOVE!® weight management program: a nationwide observational study. J Gen Intern Med 2017;32(Suppl 1):18–23. CrossRef PubMed
- Kinsinger LS, Jones KR, Kahwati L, Harvey R, Burdick M, Zele V, et al. Design and dissemination of the MOVE! weight-management program for Veterans. Prev Chronic Dis 2009;6(3):A98. PubMed
- Maciejewski ML, Shepherd-Banigan M, Raffa SD, Weidenbacher HJ. Systematic review of behavioral weight management program MOVE! for veterans. Am J Prev Med 2018;54(5):704–14. CrossRef PubMed
- Rutledge T, Skoyen JA, Wiese JA, Ober KM, Woods GN. A comparison of MOVE! versus TeleMOVE programs for weight loss in veterans with obesity. Obes Res Clin Pract 2017;11(3):344–51. CrossRef PubMed
- Heyworth L, Kirsh S, Zulman D, Ferguson JM, Kizer KW. Expanding access through virtual care: the VA’s early experience with COVID-19. NEJM Catalyst. July 1, 2020. https://catalyst.nejm.org/doi/full/10.1056/cat.20.0327. Accessed July 15, 2021.
- Breland JY, Wong MS, Steers WN, Yuan AH, Haderlein TP, Washington DL. BMI and risk for severe COVID-19 among Veterans Health Administration patients. Obesity (Silver Spring) 2021;29(5):825–8. CrossRef PubMed
- American Psychological Association. Stress in America: one year later, a new wave of pandemic health concerns. 2021. https://www.apa.org/news/press/releases/stress/2021/sia-pandemic-report.pdf. Accessed July 15, 2021.
- Stockwell S, Trott M, Tully M, Shin J, Barnett Y, Butler L, et al. Changes in physical activity and sedentary behaviours from before to during the COVID-19 pandemic lockdown: a systematic review. BMJ Open Sport Exerc Med 2021;7(1):e000960. CrossRef PubMed
- Robinson E, Boyland E, Chisholm A, Harrold J, Maloney NG, Marty L, et al. Obesity, eating behavior and physical activity during COVID-19 lockdown: a study of UK adults. Appetite 2021;156:104853. CrossRef PubMed
- Stanton R, To QG, Khalesi S, Williams SL, Alley SJ, Thwaite TL, et al. Depression, anxiety and stress during COVID-19: associations with changes in physical activity, sleep, tobacco and alcohol use in Australian adults. Int J Environ Res Public Health 2020;17(11):E4065. CrossRef PubMed
- Hall KS, Hoerster KD, Yancy WS Jr. Post-traumatic stress disorder, physical activity, and eating behaviors. Epidemiol Rev 2015;37(1):103–15. CrossRef PubMed
- Hoerster KD, Campbell S, Dolan M, Stappenbeck CA, Yard S, Simpson T, et al. PTSD is associated with poor health behavior and greater body mass index through depression, increasing cardiovascular disease and diabetes risk among U.S. veterans. Prev Med Rep 2019;15:100930. CrossRef PubMed
- Hoerster KD, Lehavot K, Simpson T, McFall M, Reiber G, Nelson KM. Health and health behavior differences: U.S. military, veteran, and civilian men. Am J Prev Med 2012;43(5):483–9. CrossRef PubMed
- Lehavot K, Hoerster KD, Nelson KM, Jakupcak M, Simpson TL. Health indicators for military, veteran, and civilian women. Am J Prev Med 2012;42(5):473–80. CrossRef PubMed
- Wang EA, McGinnis KA, Goulet J, Bryant K, Gibert C, Leaf DA, et al. ; Veterans Aging Cohort Study Project Team. Food insecurity and health: data from the Veterans Aging Cohort Study. Public Health Rep 2015;130(3):261–8. CrossRef PubMed
- Kuwert P, Knaevelsrud C, Pietrzak RH. Loneliness among older veterans in the United States: results from the National Health and Resilience in Veterans Study. Am J Geriatr Psychiatry 2014;22(6):564–9. CrossRef PubMed
- Campbell SB, Gray KE, Hoerster KD, Fortney JC, Simpson TL. Differences in functional and structural social support among female and male veterans and civilians. Soc Psychiatry Psychiatr Epidemiol 2021;56(3):375–86. CrossRef PubMed
- Caldwell AE, Thomas EA, Rynders C, Holliman BD, Perreira C, Ostendorf DM, et al. Improving lifestyle obesity treatment during the COVID-19 pandemic and beyond: new challenges for weight management. Obes Sci Pract 2021;10.1002/osp4.540. CrossRef PubMed
- Lohnberg JA, Salcido L, Frayne S, Mahtani N, Bates C, Hauser ME, et al. Rapid conversion to virtual obesity care in COVID-19: impact on patient care, interdisciplinary collaboration, and training. Obes Sci Pract 2021;28. PubMed
- Wireline Competition Bureau. Promoting broadband internet access service for veterans. May 2019. https://docs.fcc.gov/public/attachments/DOC-357270A1.pdf. Accessed July 15, 2021.
- Ferguson JM, Jacobs J, Yefimova M, Greene L, Heyworth L, Zulman DM. Virtual care expansion in the Veterans Health Administration during the COVID-19 pandemic: clinical services and patient characteristics associated with utilization. J Am Med Inform Assoc 2021;28(3):453–62. CrossRef PubMed
- US Department of Veterans Affairs, Veterans Health Administration, Office of Connected Care. Connecting veterans to telehealth care. 2021. https://connectedcare.va.gov/sites/default/files/telehealth-digital-divide-fact-sheet.pdf. Accessed June 25, 2021.
- Islam MM, Poly TN, Walther BA, Jack Li YC. Use of mobile phone app interventions to promote weight loss: meta-analysis. JMIR Mhealth Uhealth 2020;8(7):e17039. CrossRef PubMed
- Hoerster KD, Collins MP, Au DH, Lane A, Epler E, McDowell J, et al. Testing a self-directed lifestyle intervention among veterans: The D-ELITE pragmatic clinical trial. Contemp Clin Trials 2020;95:106045. CrossRef PubMed
- Ma J, Yank V, Xiao L, Lavori PW, Wilson SR, Rosas LG, et al. Translating the Diabetes Prevention Program lifestyle intervention for weight loss into primary care: a randomized trial. JAMA Intern Med 2013;173(2):113–21. CrossRef PubMed
- Knowler WC, Barrett-Connor E, Fowler SE, Hamman RF, Lachin JM, Walker EA, et al. Reduction in the incidence of type 2 diabetes with lifestyle intervention or metformin. N Engl J Med 2002;346(6):393–403. CrossRef PubMed
- Centers for Disease Control and Prevention. Registry of all recognized organizations. Diabetes prevention recognition program application. https://dprp.cdc.gov/Registry. Accessed July 12, 2021.
- Aschbrenner KA, Naslund JA, Reed JD, Fetter JC. Renewed call for lifestyle interventions to address obesity among individuals with serious mental illness in the COVID-19 era and beyond. Transl Behav Med 2021;11(7):1359–64. CrossRef PubMed
- LeBlanc EL, Patnode CD, Webber EM, Redmond N, Rushkin M, O’Connor EA. Behavioral and pharmacotherapy weight loss interventions to prevent obesity-related morbidity and mortality in adults: an updated systematic review for the US Preventive Services Task Force. Rockville (MD): Agency for Healthcare Research and Quality; 2018.
The opinions expressed by authors contributing to this journal do not necessarily reflect the opinions of the U.S. Department of Health and Human Services, the Public Health Service, the Centers for Disease Control and Prevention, or the authors’ affiliated institutions.