HIV and Hispanic/Latino People in the U.S.
Racism, discrimination, xenophobia, HIV-related stigma, homophobia, economic disparities, a fragmented healthcare system, and other longstanding barriers are key drivers of the disproportionate impact of HIV among Hispanic/Latino communities in the U.S.
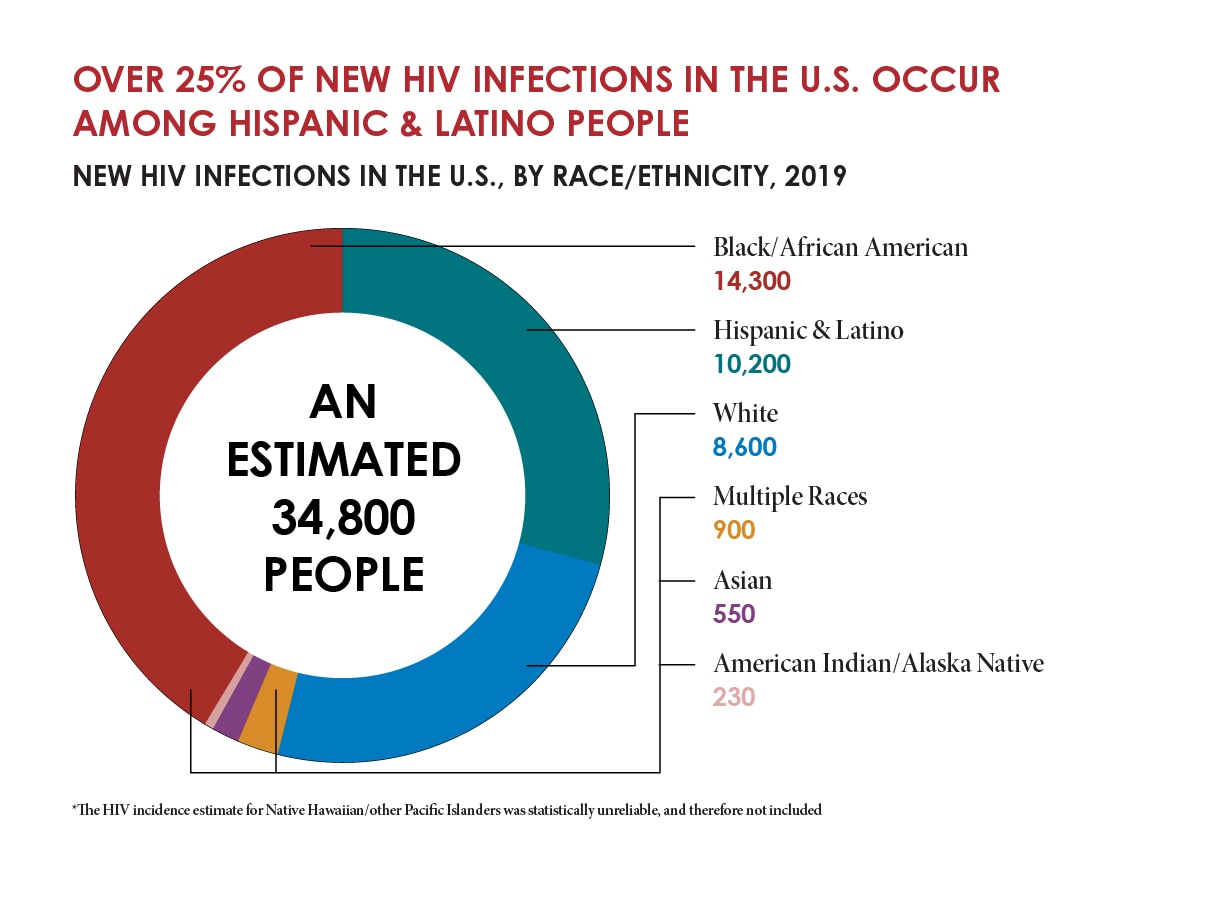
The donut graph shows the estimated 34,800 people with new HIV infections in the U.S., by race and ethnicity, in 2019
A growing body of research also shows that centuries of racism in this country has had a profound negative impact on communities of color. The impact is pervasive and deeply embedded in society—affecting where one lives, learns, works, worships, and plays and creating inequities in access to housing, quality education, wealth, employment, and a range of other social and economic benefits. These conditions—often referred to as social determinants of health—are key drivers of health inequities, causing people within some populations to experience greater risk for poor health outcomes.
For some Hispanic/Latino people, social and structural issues such as xenophobia, language barriers, poverty, mistrust of the health care system, and limited access to high-quality health care affect their access to HIV prevention and treatment and continue to drive inequities. Addressing social and structural barriers and encouraging safe and supportive communities can help improve health outcomes for Hispanic/Latino people.
With effective prevention and treatment tools at our disposal, the nation has a decades-in-the-making opportunity to end the domestic HIV epidemic and eliminate disparities in HIV prevention and care. CDC is working with partners on many fronts—including the federal Ending the HIV Epidemic in the U.S. (EHE) initiative—to deliver and scale up key, science-based HIV treatment and prevention strategies in innovative ways that reach populations equitably.
COVID-19 and HIV
The COVID-19 pandemic in the U.S. led to disruptions in HIV testing and access to clinical services throughout 2020. Although the full impact of the COVID-19 pandemic on HIV in the U.S. will not be known for some time, recent CDC data have shown concerning setbacks to HIV prevention, including sharp declines in HIV testing and diagnosis, as well as slowed pre-exposure prophylaxis (PrEP) prescriptions. In 2020, 46% fewer HIV tests were administered among Hispanic/Latino people in non-healthcare settings than in 2019.
Due to the disruptions in testing and clinical care services, CDC is not able to estimate new HIV infections (“HIV incidence”) for 2020 or to provide HIV trends through 2020. CDC is also unable to estimate the total number of diagnosed and undiagnosed HIV infections (“HIV prevalence”); or knowledge of HIV status.
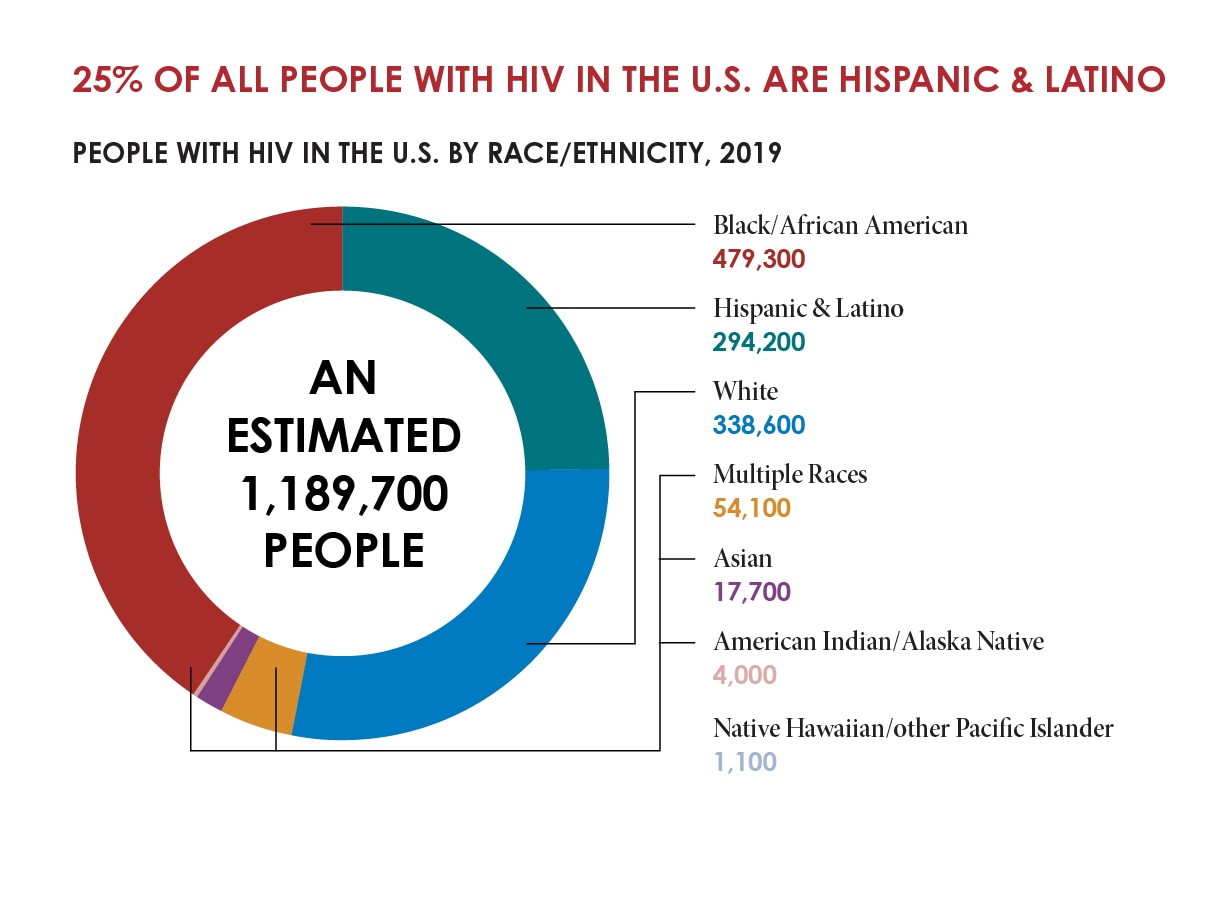
The donut chart shows people with HIV in the U.S. by race and ethnicity.
CDC estimates that, as of 2019, about 1.2 million people in the U.S. have HIV. In 2019, Hispanic/Latino people accounted for 18% of the U.S. population but 25% (294,200) of people with HIV.
While new HIV infections declined 8% overall from 2015 to 2019, they remained stable among Hispanic/Latino people during that timeframe.
New HIV Infections Disproportionately Affect Hispanic/Latino Gay and Bisexual Men and Hispanic/Latina Heterosexual Women
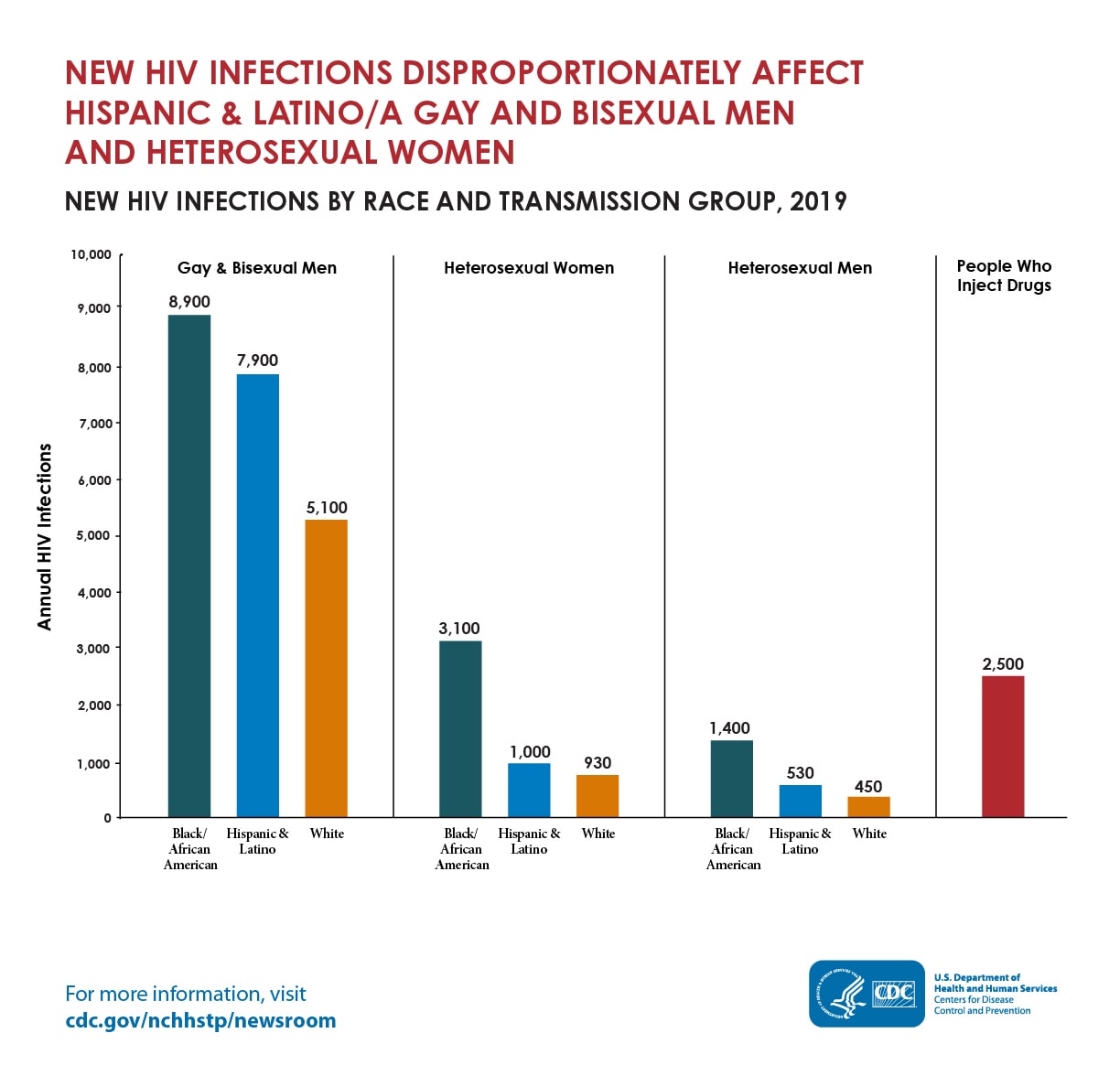
The bar chart shows the number of new HIV infections by race and ethnicity and transmission category
HISPANIC/LATINO MEN accounted for 89% of new HIV infections among all Hispanic/Latino people in the United States in 2019, with 87% of those infections attributed to male-to-male sexual contact. Furthermore, a CDC analysis found that Hispanic/Latino gay and bisexual men were the least likely to be aware of their HIV status compared to White and Black gay and bisexual men; less likely to use pre-exposure prophylaxis (PrEP) to prevent HIV; and less likely to be virally suppressed.
AMONG HISPANIC/LATINA WOMEN, 91% of new HIV infections were attributed to heterosexual contact, and the HIV infection rate among Hispanic/Latina women was 4.9%—slightly higher than the 4.5% rate among women overall.
Additionally, a recent CDC study found that HISPANIC/LATINA TRANSGENDER WOMEN accounted for 35% of HIV infections among transgender women with HIV living in seven major U.S. cities.
To end the HIV epidemic, the nation must scale up HIV testing, link people with HIV to care and treatment, and ensure equitable access to HIV prevention—including PrEP—for everyone who could benefit.
Approximately 16% of Hispanic/Latino people with HIV in the U.S. still do not know their status, and few are receiving adequate HIV care and treatment that will help them get and keep viral suppression, and live longer, healthier lives.
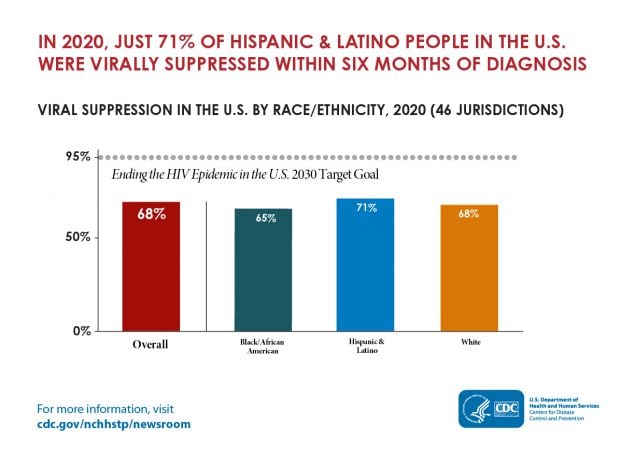
The bar chart shows the percentage of people with HIV in the U.S. who were virally suppressed by race and ethnicity
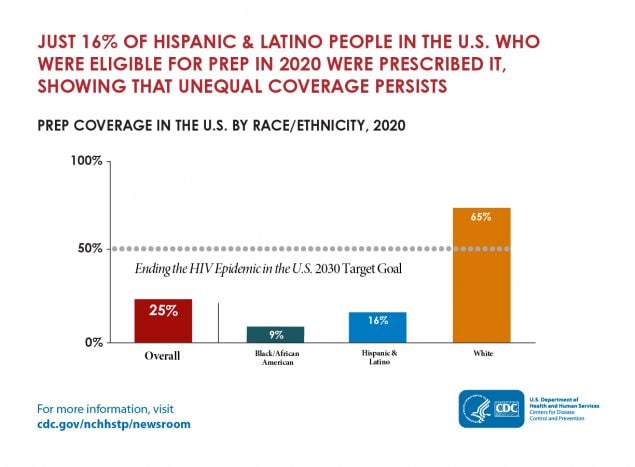
The bar chart shows the percentage of people eligible for PrEP who were prescribed it by race and ethnicity
To achieve health equity and end the HIV epidemic, the nation must overcome systemic racism, xenophobia, homophobia, transphobia, HIV-related stigma, and other persistent barriers that have contributed to disparities for far too long.
Innovation is also key. For example, a total-person approach to care integrates HIV prevention and treatment into health services that people are already seeking. This approach also addresses interconnected epidemics, such as sexually transmitted infections and hepatitis. HIV self-testing and mobile services should be maximized to reach people where they are—which, for many, is outside of traditional health care settings. And because not all areas can implement the most recent advances in HIV prevention and care, health care providers and prevention partners must deliver resources to the communities most in need.
CDC’s key efforts include:
- CDC monitors and reports HIV data, including diagnoses, linkage to care, viral suppression, and PrEP prescriptions. CDC shares these data publicly through various channels—including annual data reports and America’s HIV Epidemic Dashboard (AHEAD)—so that federal, state, and local health authorities can use this information to equitably address HIV.
- CDC analyzes data to call urgent attention to concerning trends in disparities. For example, recent CDC analyses have identified that despite overall progress, new HIV infections remained flat among Hispanic/Latino gay and bisexual men in the decade leading up to the federal EHE; and that more than a third of Hispanic/Latina transgender women surveyed in seven major U.S. cities have HIV.
- CDC awards$400 million per year to health departments for integrated HIV data collection and prevention efforts. Through these awards, health departments work to reach the populations and geographic areas with the greatest need.
- The federal EHE initiative is also working to address disparities. In July 2020, CDC awarded approximately $109 million to state and local health departments within the 57 EHE jurisdictions to begin the first year of a five-year funding program. In July 2021, CDC awarded $117 million to those areas to help rebuild and begin to expand HIV prevention and treatment efforts as the U.S. continues to respond to COVID-19.
- CDC funds community-based organizations (CBOs), which are positioned to complement the HIV prevention work of health departments, in two ways: CDC provides direct funding to CBOs, as well as indirect funding to CBOs through health departments. CDC is providing up to $210 million in direct funding over five years, through 2026, to nearly 100 CBOs to implement comprehensive HIV prevention programs. These resources are focused on Hispanic/Latino gay and bisexual men, transgender people, and people who inject drugs.
- In April 2022, CDC awarded funds to 36 CBOs to develop and implement high-impact prevention programs for young gay and bisexual men of color and transgender youth of color. These programs will be guided by a status-neutral approach to care; continually engage people who could benefit from HIV care, prevention, and essential support services; and address the social determinants of health that adversely affect HIV outcomes in young gay and bisexual men and transgender people of color.
- To help reduce stigma and encourage people who experience risk for and with HIV to seek out vital testing, treatment, and prevention services, CDC works with community partners to design and deliver education and awareness campaigns such as Let’s Stop HIV Together / Detengamos Juntos el VIH. Let’s Stop HIV Together / Detengamos Juntos el VIH reaches Hispanic/Latino people with culturally and linguistically appropriate messages about HIV testing, prevention, and treatment.
- CDC identifies evidence-based interventions and best practices through CDC’s HIV Prevention Research Synthesis (PRS) Project. The PRS Project has identified several interventions for Hispanic/Latino people, including Centralized HIV Services, Project IMAGE, Hola en Grupos, Sin Buscar Excuses, Adapted-Stage Enhanced Motivational Interviewing, and Familias Unidas.
- CDC centers its work on health equity by developing and implementing strategies and programs to address health disparities through the Office of Health Equity.
- CDC builds capacity for HIV epidemiologic and prevention research in Hispanic/Latino communities through the Minority HIV Research Initiative program.
To end the HIV epidemic once and for all, the nation must work together to increase the accessibility and uptake of powerful HIV prevention and treatment tools by everyone.
If you are a member of the news media and need more information, please visit www.cdc.gov/nchhstp/newsroom or contact CDC’s Media Office at 404-639-3286 or media@cdc.gov.