Continue to check our website for further updates on when we will reopen. When the museum reopens, all visitors will need to make reservations at least a week in advance. Walk-in visits are no longer permitted.
Teen Newsletter: Ebola
March 2022
The David J. Sencer CDC Museum (CDCM) Public Health Academy Teen Newsletter was created to introduce teens to public health topics. Each newsletter focuses on a different public health topic that CDC studies. Newsletter sections: Introduction, CDC’s Work, The Public Health Approach, Out of the CDC Museum Collection, and Teen Talk.
Watch the Ebola Teen Talk.
Introduction – Ebola
Ebola Virus Disease (EVD), one of the deadliest viral diseases, was discovered in 1976 when two consecutive outbreaks of fatal hemorrhagic fever occurred in different parts of Central Africa. The first outbreak occurred in the Democratic Republic of the Congo (formerly Zaire) in a village near the Ebola River, which gave the virus its name. The second outbreak occurred in what is now South Sudan, approximately 500 miles (850 km) away. Since its discovery in 1976, the majority of cases and outbreaks of EVD have occurred in Africa.
EVD most commonly affects people and nonhuman primates (such as monkeys, gorillas, and chimpanzees). It is caused by an infection with a group of viruses within the genus Ebolavirus – of these, only four (Ebola, Sudan, Taï Forest, and Bundibugyo viruses) have caused diseases in people.
Scientists think people are initially infected with Ebola virus through contact with an infected animal, such as a fruit bat or nonhuman primate. Infected animals carrying the virus can transmit it to other animals, like apes, monkeys, duikers and humans. This is called a spillover event. After that, the virus spreads from person to person, potentially affecting a large number of people. The virus spreads through direct contact (such as through broken skin or mucous membranes in the eyes, nose, or mouth) with:
- Blood or body fluids (urine, saliva, sweat, feces, vomit, breast milk, amniotic fluid, and semen) of a person who is sick with or has died from EVD.
- Objects (such as clothes, bedding, needles, and medical equipment) contaminated with body fluids from a person who is sick with or has died from EVD.
- Infected fruit bats or nonhuman primates (apes or monkeys).
- Semen from a man who recovered from EVD.
Once exposed, the course of the illness typically progresses from “dry” symptoms initially (such as fever, aches and pains, and fatigue), to “wet” symptoms (such as diarrhea and vomiting) as the person becomes sicker. Other symptoms may include red eyes, skin rash, and hiccups (late-stage). Ebola virus can be detected in blood after onset of symptoms. However, diagnosing EVD shortly after infection can be difficult. Many common illnesses can have the same symptoms as EVD, including influenza (flu), malaria, and typhoid fever.
Recovery from EVD depends on good supportive clinical care and the patient’s immune response. Ebola survivors may experience side effects after their recovery. These may include tiredness, muscle aches, eye and vision problems and stomach pain.

CDC’s Work – Ebola
At CDC, there are two centers that work on Ebola:
- The National Center for Emerging and Zoonotic Infectious Diseases (NCEZID) works to protect people at home and around the world from emerging and zoonotic infections ranging from A to Z—anthrax to Zika, including Ebola. Within NCEZID is the Division of High Consequence Pathogens and Pathology (DHCPP) that improves public health and safety nationally and globally through investigating, monitoring, and controlling sickness, disability, and death caused by highly lethal viral, bacterial, prion, and related infections and diseases of unknown origin. Did you know that one-third of the world’s population lives in an area at risk for viral hemorrhagic fevers (VHFs), like Ebola virus disease? The consequences of an outbreak like that can be devastating. DHCPP’s Viral Special Pathogens Branch (VSPB) plays a leading role in building capacity to detect, prevent, and control diseases like VHFs and others that are caused by dangerous viruses.

- The Office of Readiness and Response (ORR) is America’s public health defense hub. Within CPR is the Division of Emergency Operations (DEO) that coordinates CDC’s preparedness, assessment, response, recovery, and evaluation prior to and during public health emergencies. The CDC Emergency Operations Center (EOC) is staffed around the clock, and provides worldwide situational awareness of public health emergencies. Check out next month’s Teen Newsletter to learn more about the EOC. CDC activated its EOC in July 2014 for the Ebola outbreak in West Africa and in June 2019 for the Ebola outbreak in eastern Democratic Republic of the Congo (DRC). CDC staff assisted with surveillance, contact tracing, data management, laboratory testing, health education, logistics, communication, analytics, and management. CDC works with other partners to protect people from Ebola even when the EOC is not activated, including during the most recent Ebola outbreak. On October 8, 2021, the Ministry of Health (MOH) in the DRC announced an outbreak of EVD in Beni Health Zone, North Kivu Province. Subsequent cases were confirmed in the same health zone and three probable cases were retrospectively identified from September 2021. Beni, one of the epicenters of the 2018-2020 EVD outbreak in DRC, is not far from Butembo City, the site of two recent EVD outbreaks, one in 2018 and another earlier in 2021. CDC worked with the MOH and the World Health Organization (WHO) to implement response activities. An EVD surveillance system was put into place, and contact tracing and vaccination activities were carried out. This outbreak, the 13th EVD outbreak in DRC, was declared officially over on December 16, 2021, 42 days after the last confirmed case of EVD was released from the Ebola treatment unit after testing negative twice for Ebola.

The Public Health Approach – Ebola
Public health problems are diverse and can include infectious diseases, chronic diseases, emergencies, injuries, environmental health problems, as well as other health threats. Regardless of the topic, we take the same systematic, science-based approach to a public health problem by following four general steps.
For ease of explaining and understanding the public health approach for this public health problem (Ebola), let’s focus on the 2014-2016 West African Ebola outbreak.
- Surveillance (What is the problem?). In public health, we identify the problem by using surveillance systems to monitor health events and behaviors occurring among a population.
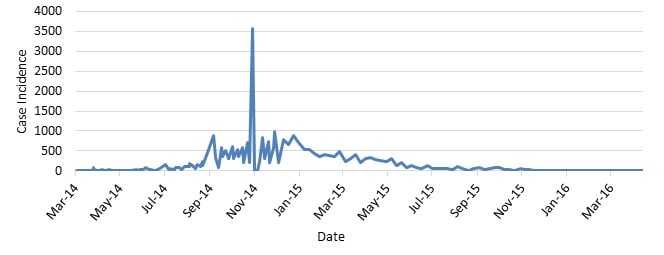
This graph shows the frequency of newly reported cases in Guinea, Liberia, and Sierra Leone provided in WHO Situation Reports beginning on March 25, 2014, through the last situation report on June 10, 2016. The numbers are a total of suspected, probable, and confirmed cases.
For this outbreak, the first case of Ebola was reported by the World Health Organization (WHO) in Guinea in March 2014. Over the span of a year, the Ebola epidemic caused more than 10 times as many cases of Ebola than the combined total of all those reported in previous Ebola outbreaks.
CDC and partners were heavily involved in implementing case-based surveillance systems, sustaining case surveillance and contact tracing, and interpreting surveillance data.
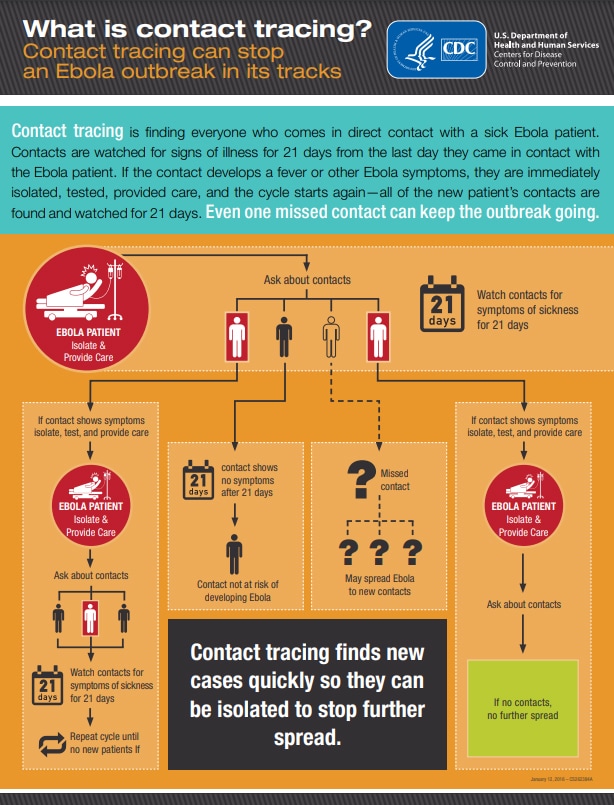
Contact tracing was used to identify new Ebola cases quickly, which increased patients’ chances of survival, and isolated patients as soon as they showed symptoms, which prevented spread to others.
Public health laboratories perform limited diagnostic testing, reference testing, and disease surveillance. They also provide emergency response support, perform applied research, and provide training for laboratory personnel. Fast and accurate laboratory tests and reporting enable communities to track disease trends and identify outbreaks, as well as help diagnose and treat health conditions. In collaboration with the National Institutes of Health, CDC expanded laboratory capacity in Liberia and Sierra Leone, which improved patient management and resulted in a shift toward reporting primarily confirmed cases.
To learn more about Ebola surveillance, check out the MMWR Ebola Reports.
- Risk Factor Identification (What is the cause?). After we’ve identified the problem, the next question is, “What is the cause of the problem?” For example, are there factors that might make certain populations more susceptible to disease, such as something in the environment or certain behaviors that people are practicing?
- Throughout history, the use of contaminated needles and syringes during the earliest outbreaks enabled transmission and amplification of Ebola virus. Close contact with infected blood, reusing of contaminated needles, and improper nursing techniques were the sources for much of the human-to-human transmission during early Ebola outbreaks. During the 2014-2016 West Africa outbreak, the majority of transmission events were between family members (74%). Direct contact with the bodies of those who died from EVD proved to be one of the most dangerous – and effective – methods of transmission. See the Ebola Virus Ecology and Transmission infographic in the Introduction section above. In addition, sociodemographic factors that contributed to virus spread included high mobility and intermixing of population, as well as general unfamiliarity with how to respond to Ebola outbreaks. Ebola poses little risk to travelers or the general public who have not cared for or been in close contact (within 3 feet or 1 meter) with someone sick with Ebola.
- Intervention Evaluation (What works?). Once we’ve identified the risk factors related to the problem, we ask, “what intervention works to address the problem?” We look at what has worked in the past in addressing this same problem and if a proposed intervention makes sense with our affected population.
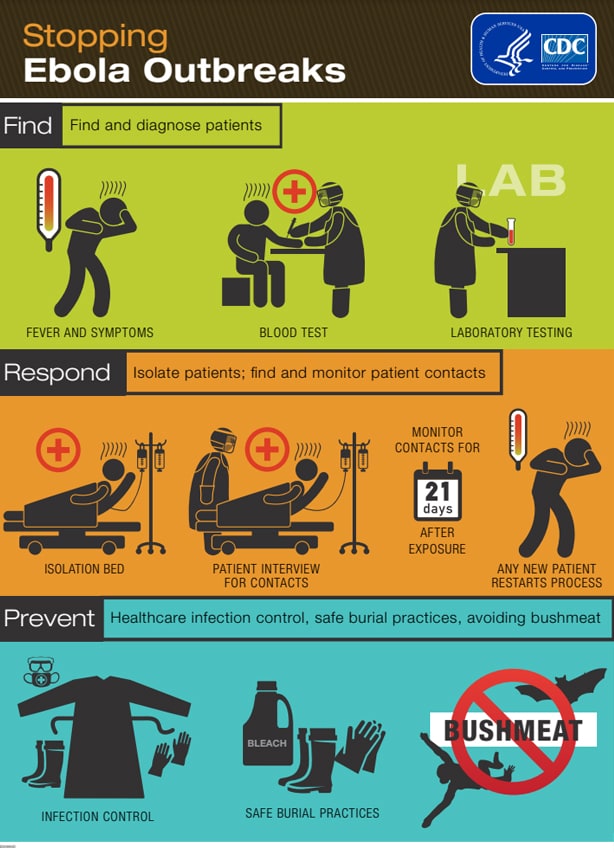
- Drawing on experience from previous Ebola outbreaks, CDC worked with governments and partners to detect and break chains of transmission and end the epidemic. Because lack of reliable epidemiologic data was a major challenge from the outset, the teams quickly began to improve surveillance, laboratory, and information management systems to collect, analyze, and report data needed to guide response actions. CDC field teams regularly traveled to districts and villages to work with community teams on patient identification and isolation, contact tracing, infection control, social mobilization, and safe burials. Local public health officials encouraged hand washing in communities, discouraged the consumption of bushmeat or contact with bats for locals, and highly cautioned travelers against visiting the countries.
- Implementation (How did we do it?). In the last step, we ask, “How can we implement the intervention? Given the resources we have and what we know about the affected population, will this work?”
- CDC’s response to the 2014-2016 Ebola epidemic was the largest emergency response in the agency’s history before the current COVID-19 pandemic response. The response to the Ebola epidemic in Guinea, Liberia, and Sierra Leone varied by country and involved many international partners working with government ministries, including:
- U.S. Agency for International Development’s Office of Foreign Disaster Assistance Disaster Assistance Response Teams (DARTs)
- National Ebola Training and Education Center (NETEC)
- What Fellows Do | Epidemic Intelligence Service
- Emory University’s electronic surveillance system
These collaborations provided some of the most successful interventions.
The Rapid Isolation and Treatment of Ebola (RITE) strategy was developed by CDC and the Liberian Ministry of Health and Social Welfare. Launched in October 2014, the strategy focuses on maintaining investigation and response-ready health teams (RITE teams) ready to deploy to remote areas as soon as a report of a suspected Ebola case is received. Their goal: stop the chain of Ebola transmission. By November, the strategy had expanded to include the packaging of “RITE kits” for rapid delivery to affected counties, containing commodities essential for the first 14 days of response. The enhanced capacity of county health teams to investigate outbreaks in remote areas provided a faster, more tailored response to local needs. Cases had declined substantially, enabling focus on individual transmission chains, and Liberia was eventually declared free of Ebola transmission by WHO on May 9, 2015.
A marked resistance among Guinean residents to report suspected Ebola cases hampered an early effective response and accessibility to villages. When the initial outbreak seemed to be waning, some cases were unreported. To establish community outreach, several approaches were undertaken by the response incident management system. These included working with village elders, engaging Conakry residents who had family in the villages, deploying social anthropologists as members of investigation teams, and using security forces to maintain the peace. WHO declared Guinea free of Ebola transmission on December 29, 2015.
Unlike in Guinea and Liberia, in Sierra Leone, CDC established, managed, and staffed an Ebola testing laboratory. CDC supported laboratory coordination, assisted with the development of sample transport and data reporting systems, and provided support to ministries of health to conduct proficiency testing of international Ebola laboratories in Sierra Leone. WHO declared the end of the epidemic in Sierra Leone on November 7, 2015. Rapid and effective contact tracing, as well as implementation of control measures, quickly controlled the sporadic clusters that have occurred since then.
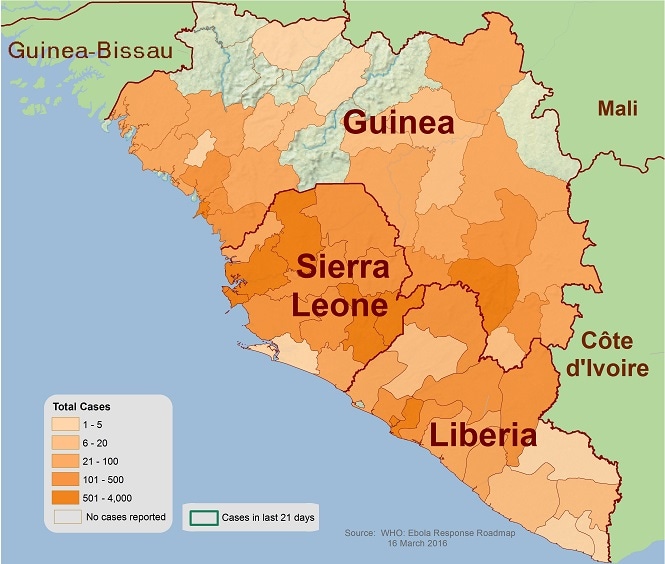
Two and a half years after the first case was discovered, the outbreak ended with more than 28,600 cases and 11,325 deaths.
Despite the necessary challenges to overcome during this historic event, CDC’s response to the Ebola epidemic in West Africa was made possible by the tireless work, unbridled dedication, and extraordinary resilience of thousands of agency staff members overseas and in the United States. CDC worked to strengthen critical control strategies, including case management, meticulous contact tracing, early treatment with supportive care, and social mobilization, and helped to develop creative new strategies relevant to this epidemic. CDC’s activities strengthened epidemiologic and data management capacity to improve routine surveillance in the countries affected, even after the Ebola epidemic ended, and enhanced local capacity to respond quickly to future public health emergencies.
Using the Public Health Approach helps public health professionals identify a problem, find out what is causing it, and determine what solutions and interventions work.
Out of the CDC Museum Collection – Ebola
This month’s Out of CDC Museum Collection takes us into the EBOLA: People + Public Health + Political Will exhibition that looked at the historic 2014-16 epidemic in West Africa, the U.S., and around the world (the epidemic described in the Public Health Approach). The exhibit was displayed from June 19, 2017 – June 15, 2018. Featured below are images and documents that were on display. They are from a nonprofit that assisted with the Ebola outbreak.
Riders for Health® (Riders) is an international non-governmental organization (NGO) that has provided health care to rural African villages using motorcycles and motorcycle ambulances since 1986. The Ebola epidemic in West Africa underscored that reliable transport is essential to a strong and far-reaching health system.




These motorcycle couriers offer an innovative solution for safely getting samples from local clinics to diagnostic labs. Riders for Health has a fleet of trained couriers who transport samples, allowing lifesaving results to quickly be obtained and used by healthcare workers.
In Liberia, Riders set up a program with support from CDC, the CDC Foundation, and the World Health Organization to provide the Liberian government with a sample transport system. Starting in April 2015, 70 motorcycle couriers across 15 different counties connected health centers to laboratories—transporting blood and sputum samples to test for the disease.
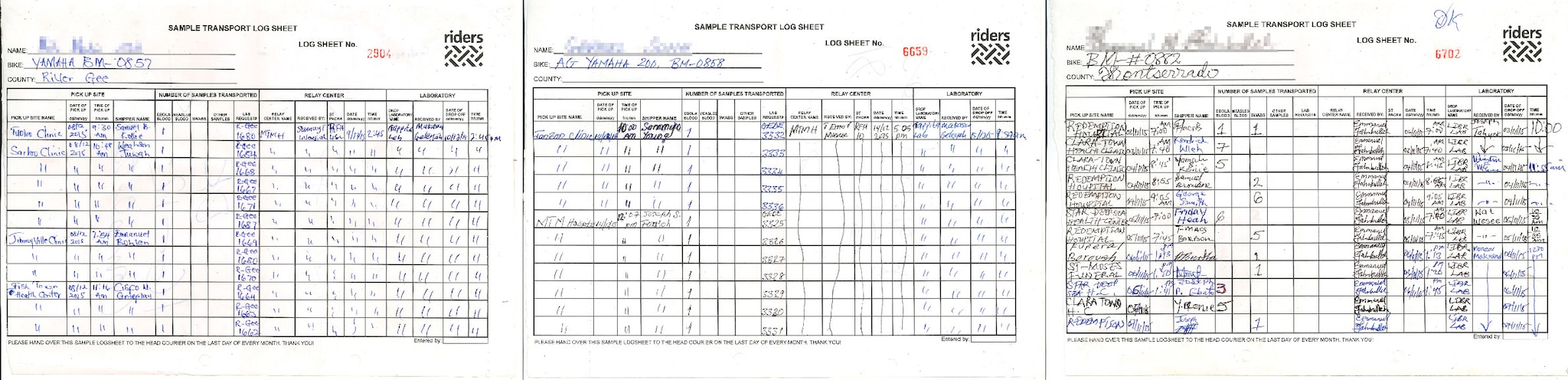
Three sample transport log sheets filled out by Riders couriers with the driver's name, bike, county, and logistical information used in Lofa County, Liberia during the Ebola response.
Explore the full digital exhibition of EBOLA: People + Public Health + Political Will and learn more about when EVD was discovered in 1976 through the online exhibit, The Story of CDC.

