Continue to check our website for further updates on when we will reopen. When the museum reopens, all visitors will need to make reservations at least a week in advance. Walk-in visits are no longer permitted.
Teen Newsletter: November 2021 – Botulism
The David J. Sencer CDC Museum (CDCM) Public Health Academy Teen Newsletter was created to introduce teens to public health topics. Each month will focus on a different public health topic that CDC studies. Newsletter sections: Introduction, CDC’s Work, The Public Health Approach, Out of the CDC Museum Collection, and Teen Talk.
Watch the botulism Teen Talk.
Introduction – Botulism
Botulism is a rare but serious illness caused by a toxin that attacks the body’s nerves and causes difficulty breathing, muscle paralysis, and even death. This toxin is made by Clostridium botulinum and sometimes Clostridium butyricum and Clostridium baratii bacteria.
The bacteria that make botulinum toxin are found naturally in many places, but it’s rare for them to make people sick. These bacteria make spores, which act like protective coatings that help the bacteria survive, even in extreme conditions. The spores usually do not cause people to become sick, even when they’re eaten. However, these spores can grow under certain conditions and make one of the most lethal toxins known. When spores are given the correct temperature and water requirements and are in an environment with little or no oxygen, acid, sugar, or salt, they can grow and produce botulinum toxin.
There are five kinds of botulism. The most common is infant botulism, which occurs when spores grow in infant intestines. Very rarely, this can also occur in adults and is known as adult intestinal toxemia. Wound botulism is a third type that can happen if the spores of the bacteria get into a wound; it is most common among people who inject drugs. Foodborne botulism can happen from eating foods that have been contaminated with botulinum toxin, usually from homemade foods that have been improperly canned, preserved, or fermented. Finally, iatrogenic botulism can happen if too much botulinum toxin is injected for cosmetic reasons, such as for wrinkles, or medical reasons, such as for migraine headaches.
The signs and symptoms of botulism vary; however, they all result from muscle paralysis caused by the toxin. If untreated, the disease may progress and symptoms may worsen to cause full paralysis of some muscles, including those used in breathing and those in the arms, legs, and torso.
Some symptoms might include difficulty swallowing, muscle weakness, double vision, drooping eyelids, blurry vision, slurred speech, and difficulty breathing. Possible signs and symptoms in foodborne botulism might also include vomiting, nausea, stomach pain, and diarrhea. In foodborne botulism, symptoms generally begin 18 to 36 hours after eating a contaminated food.
CDC’s Work – Botulism
CDC’s National Center for Emerging and Zoonotic Infectious Diseases (NCEZID) is the center responsible for working on botulism. Within NCEZID is the Division of Foodborne, Waterborne, and Environmental Diseases (DFWED). They protect public health nationally and internationally through the prevention and control of disease, disability, and death caused by foodborne, waterborne, and environmentally transmitted infections. CDC provides clinical consultations and antitoxin for suspected botulism cases.
CDC also works in food safety to prevent cases of botulism. CDC outlines how to keep yourself and others safe when it comes to home-canned foods. Home-canned vegetables are the most common cause of botulism outbreaks in the United States. By using proper canning techniques, using the right canning equipment, and throwing out possibly contaminated foods, people can safely enjoy home-canned foods.
Read more about CDC’s guidelines to prevent botulism.
The Public Health Approach – Botulism
Public health problems are diverse and can include infectious diseases, chronic diseases, emergencies, injuries, environmental health problems, as well as other health threats. Regardless of the topic, we take the same systematic, science-based approach to a public health problem by following four general steps.
- Surveillance (What is the problem?) In public health, we identify the problem by using surveillance systems to monitor health events and behaviors occurring among a population.There are several surveillance systems that monitor for cases:
Botulism is a notifiable disease in the United States. Physicians must promptly notify the state health department of suspected cases, and laboratories must notify the state health department of all confirmed cases. State health departments report confirmed cases to CDC.
FDOSS is CDC’s program for collecting and reporting data about foodborne disease outbreaks in the United States.
The National Botulism Surveillance System collects reports of all laboratory-confirmed botulism cases in the United States and is continuously monitored for early detection of outbreaks. CDC also maintains a record of all antitoxin releases for cases in categories other than infant botulism.
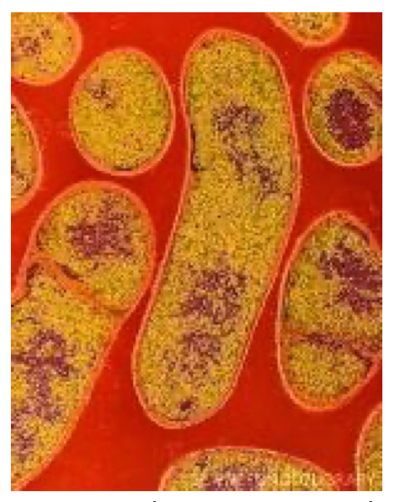
Colored transmission electron micrograph of the Gram-positive anaerobic bacteria Clostridium botulinum.
For ease of explaining and understanding the public health approach for this public health problem (botulism), let’s focus on foodborne botulism caused by home-canned foods, specifically in Native Alaskan communities.
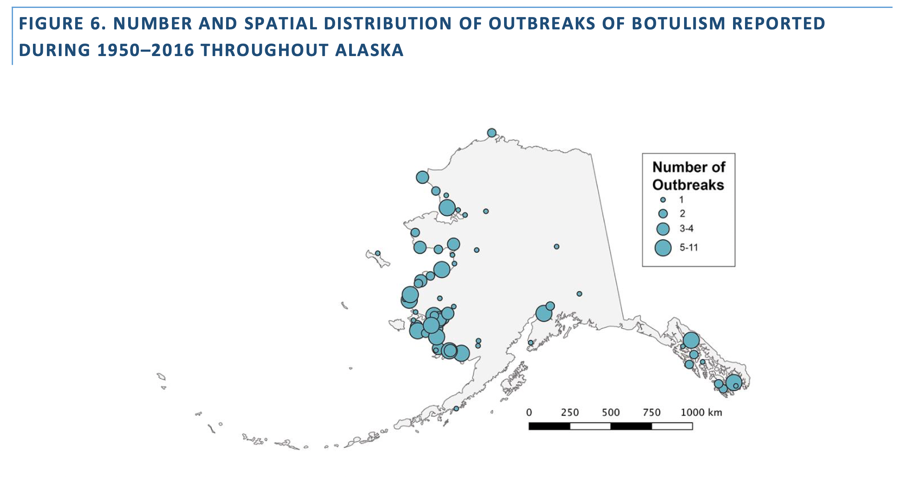
- Risk Factor Identification (What is the cause?) After we’ve identified the problem, the next question is, “What is the cause of the problem?” For example, are there factors that might make certain populations more susceptible to disease, such as something in the environment or certain behaviors that people are practicing? Alaska has more foodborne botulism than any other state in the country. From 1950 to 2017, more than 350 people in Alaska have been diagnosed with botulism and 24 people have died.
All Alaskan botulism cases have been associated with the consumption of traditional Alaskan Native foods. These include:
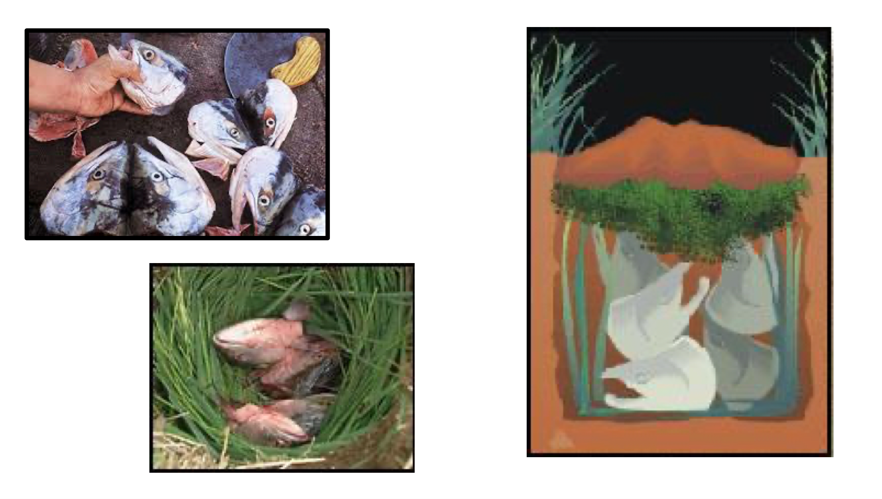
- Fermented fish heads (“stinky heads”)
- Fermented fish eggs (“stinky eggs”)
- Fermented beaver tail
- Fermented seal flipper
- Fermented walrus flipper
- Fermented whale
- Seal oil
- Dried, unsalted fish
While many of these foods are labeled as “fermented,” sea mammal food products are difficult to truly ferment because of the lack of carbohydrates in their biological structures. Fermentation requires carbohydrates and results in the production of an organic acid that lowers the food’s pH. However, because sea mammal food products do not contain enough carbohydrates to enable fermentation, pH levels remain neutral. In the more neutral environment, the bacteria thrive and produce the botulinum toxin.
Many traditional Alaskan Native methods of food preparation also increase risk. Historically, “stink” foods such as aged salmon eggs (stink eggs) or salmon heads (stink heads) were prepared by being buried in moss-lined pits or barrels in the ground. Now, these foods are more often prepared in barrels, jars, and plastic bags, which can be tightly sealed and brought indoors. The decreased oxygen levels and warmer indoor temperatures favor the growth of bacterial spores.
- Intervention Evaluation (What works?)
Once we’ve identified the risk factors related to the problem, we ask, “what intervention works to address the problem?” We look at what has worked in the past in addressing this same problem and if a proposed intervention makes sense with our affected population.
Foodborne botulism resulting from consumption of uncooked fermented seafood has been an endemic hazard among Alaska Native populations for centuries. Between 2000 and 2007, the mean annual incidence of foodborne botulism was 836 times the overall US rate.
 External Link Icon
External Link IconFermented animal paws.
The Alaska Division of Public Health, in partnership with CDC, is always working to lower the number of botulism cases and keep Alaskans healthy and safe. Here are some of their interventions that have been successful:
- Preparing culturally appropriate educational materials focusing on safer traditional fermentation processes
- Educating Alaskan healthcare providers about the importance of prompt clinical diagnosis, reporting, and antitoxin administration
- Creating and distributing antitoxin kits for hospital pharmacies located in areas most likely to need the antitoxin, based on historical usage
These interventions have been generally very successful – over time, there has been both a decrease in botulism cases and an increase in Native communities’ knowledge of the toxin. In addition, the fatality rate of botulism cases in Alaska has decreased from 40% in the 1960s to less than 5% today.
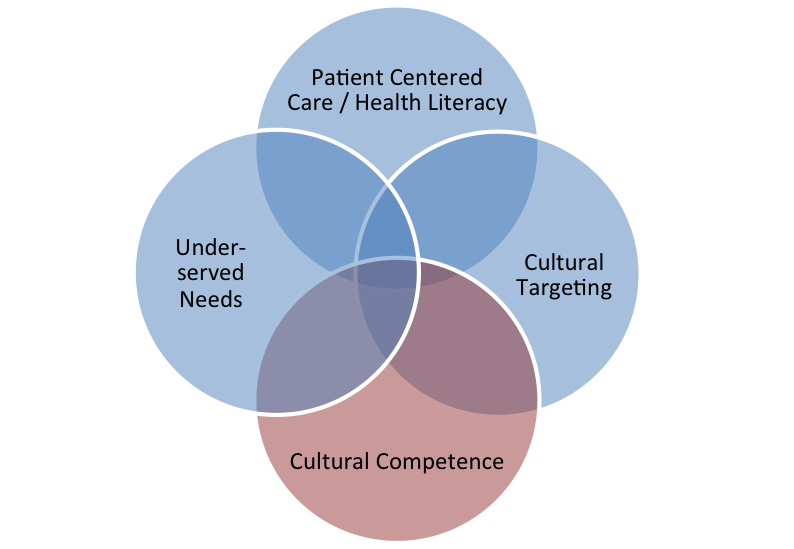
To add to these “lessons learned,” the strongest asset of these interventions – the real implementation strategy – was the fact that the public health teams remained culturally competent. Keep reading into the next section to learn more about this crucial aspect for success.
- Implementation (How did we do it?)
In the last step, we ask, “How can we implement the intervention? Given the resources we have and what we know about the affected population, will this work?”
Cultural competence is the ability of public health providers and organizations to effectively deliver health care services that meet the social, cultural, and linguistic needs of patients. It means health providers must be aware of their own cultural beliefs and values and how these may be different from other cultures – including being able to learn about and honor the different cultures of those with whom they work.
For botulism interventions in Northern Alaskan, public health officials first got to know the Native communities they were working with on a personal basis. They learned about the importance of the fermentation process to Native Alaskan culture and prepared appropriate educational materials focusing on safer fermentation processes rather than attempting to stop the practice entirely. Public health officials found a way to keep this important custom in place, while also educating the community on new practices that make fermented food safer.
Using the Public Health Approach helps public health professionals identify a problem, find out what is causing it, and determine what solutions and interventions work.
Out of the CDC Museum Collection – Botulism
This month’s Out of the CDC Museum Collection relates to the Public Health Approach section that focuses on Native Alaskan communities. Below you will find historic photographs of Gretchen Laturnus Saupe, a public health nurse. Saupe worked for the United States Public Health Service (USPHS) at the Arctic Health Research Center from 1957-1959. She worked in a few villages in the lower Yukon and Bethel regions of Alaska, developing chemotherapy programs to help treat and control tuberculosis. At the time, tuberculosis was a serious health problem in many Native Alaskan communities.

Saupe and her guide in 1957.

Mission Girls in St. Mary’s, Alaska (along the Andrefski river) cleaning fish (1957-1959).

Fish drying in Kwethluk, Alaska. The population of Kwethluck in 2019 was 769.

Saupe and her guide leaving Kwiguk for Alakanuk, Alaska.