Continue to check our website for further updates on when we will reopen. When the museum reopens, all visitors will need to make reservations at least a week in advance. Walk-in visits are no longer permitted.
Teen Newsletter: August/September 2021 – Polio Eradication
The David J. Sencer CDC Museum (CDCM) Public Health Academy Teen Newsletter was created to introduce teens to public health topics. Each month will focus on a different public health topic that CDC studies. Newsletter sections: Introduction, CDC’s Work, The Public Health Approach, Special Feature, Out of the CDC Museum Collection, and Activities.
Be sure to join our live Newsletter Zoom on September 28, 2021, at 8pm ET, and check out all the activities (digital scavenger hunt—Goosechase, Zoom, social media challenge, and Ask a CDCer) at the end of each newsletter. Join in on the fun and win some prizes! Also, be on the lookout for the recently added activity, a pre-Zoom game (Kahoot) that will be emailed the day of the Zoom.
We are excited to announce a new newsletter activity prize category: Future CDCer, learn more below.
Introduction – Polio Eradication
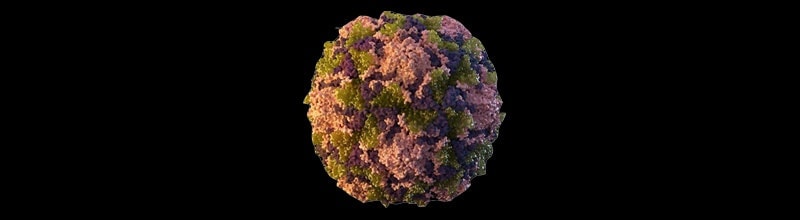
Polio, or poliomyelitis, is a disabling and life-threatening disease caused by the poliovirus. The virus spreads from person to person and can infect a person’s spinal cord, causing paralysis.
Poliovirus is very contagious and spreads through person-to-person contact. It lives in an infected person’s throat and intestines. Poliovirus only infects people. It enters the body through the mouth and spreads through either contact with the feces (poop) of an infected person or droplets from a sneeze or cough of an infected person (less common). An infected person may spread the virus to others immediately before and up to 2 weeks after symptoms appear. The virus can live in an infected person’s feces for many weeks. It can contaminate food and water in unsanitary conditions. People who don’t have symptoms can still pass the virus to others and make them sick.
Most people who get infected with poliovirus (about 72 out of 100) will not have any visible symptoms. About 1 out of 4 people with poliovirus infection will have flu-like symptoms that may include sore throat, fever, tiredness, nausea, headache, and stomach pain. These symptoms usually last 2 to 5 days, then go away on their own.
A smaller proportion of people with poliovirus infection will develop other, more serious symptoms that affect the brain and spinal cord like paresthesia (feeling of pins and needles in the legs), meningitis (infection of the covering of the spinal cord and/or brain) which occurs in about 1 out of 25 people with poliovirus infection, or paralysis (either can’t move parts of the body or weakness in the arms, legs, or both) which occurs in about 1 out of 200 people with poliovirus infection. Between 2 and 10 out of 100 people who have paralysis from poliovirus infection die, because the virus affects the muscles that help them breathe.
Even children who seem to fully recover can develop new muscle pain, weakness, or paralysis as adults, 15 to 40 years later. This is called post-polio syndrome. Note that “poliomyelitis” (or “polio” for short) is defined as the paralytic disease. So only people with the paralytic infection are considered to have the disease.
There are two types of vaccine that can prevent polio:
- Inactivated poliovirus vaccine (IPV) given as an injection in the leg or arm, depending on the patient’s age. Only IPV has been used in the United States since 2000.
- Oral poliovirus vaccine (OPV) given by mouth as drops, is still used throughout much of the world.
Polio vaccine protects children by preparing their bodies to fight the poliovirus. Almost all children (99 children out of 100) who get all the recommended doses of the inactivated polio vaccine will be protected from polio.
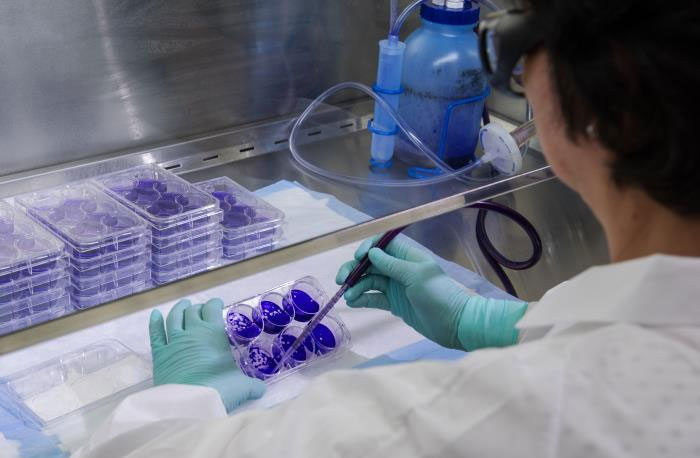
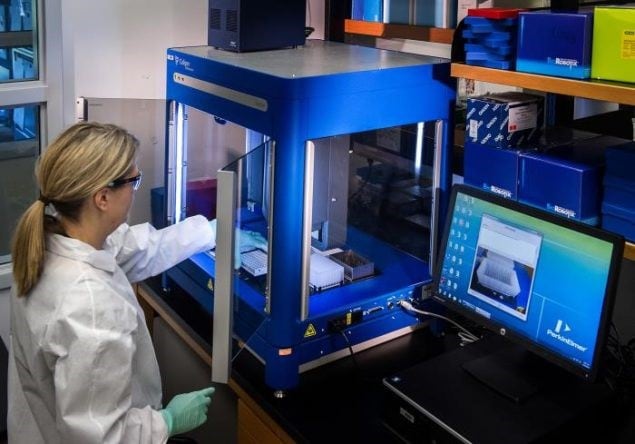
CDC laboratories conduct testing for poliovirus, including culture, intratypic differentiation, genome sequencing, and serology.
The number of worldwide polio cases has fallen from an estimated 350,000 in 1988 to 176 in 2019—a decline of more than 99% in reported cases. Only two polio-endemic countries (nations that have never interrupted the transmission of wild poliovirus) remain—Afghanistan and Pakistan.
Did you know that due to a successful vaccination program, the United States has been polio-free since 1979? Poliovirus is still a threat in some countries, and travelers could once again spread poliovirus in the US.
CDC’s Work – Polio Eradication
Two parts of CDC work on Polio eradication:
In the areas of outbreaks and program development, CDC provides support to develop micro-plans to ensure services reach every community, engage community leaders in social mobilization to raise awareness of polio and immunization campaigns, train vaccination teams conducting vaccination activities, and strengthen surveillance to address any gaps. CDC also provides technical guidance on a number of monitoring and evaluation activities such as independent monitoring of immunization campaigns, lot quality assurance sampling technique, campaign evaluation, and cold chain monitoring.
CDC and GPEI partners are actively engaged in conducting immunization activities to increase coverage and minimize the risk of further spread of the virus.
CDC’s clinical and operational research offer opportunities to take a closer look at issues such as polio vaccination dosage and schedules, as well as novel technology like drones for vaccine delivery. Results from research have an immediate impact on how CDC and its partners operate on the ground as well as on long-term policy and strategy shifts that bring us closer to getting to zero.
CDC receives direct, annual appropriations from Congress to eradicate polio, helping to protect the American people from health threats and ensure a world where people live healthier, safer, and longer lives.
Without CDC’s polio eradication efforts, more than 18 million people who are currently healthy would have been paralyzed by the virus.
Read more about Stories on Global Immunization
The Public Health Approach – Polio Eradication
Public health problems are diverse and can include infectious diseases, chronic diseases, emergencies, injuries, environmental health problems, as well as other health threats. Regardless of the topic, we take the same systematic, science-based approach to a public health problem by following four general steps.
- Surveillance (What is the problem?)
In public health, we identify the problem by using surveillance systems to monitor health events and behaviors occurring among a population.
Overall, CDC is involved in several surveillance systems and groups that track polio:
National Notifiable Diseases Surveillance System (NNDSS)
Poliovirus is a notifiable disease in the United States. Physicians must promptly notify the state health department of suspected cases, and laboratories must notify the state health department of all confirmed cases. State health departments use the NNDSS to report confirmed cases to CDC. NNDSS data is collected from states through several mechanisms, including the National Electronic Disease Surveillance System (NEDSS) Base System (NBS).
CDC is a partner of GPEI, the global partnership with the goal to complete the eradication and containment of all wild, vaccine-related and Sabin polioviruses, so no child suffers from paralytic poliomyelitis ever again. One of GPEI’s four pillars of polio eradication is surveillance. They perform active surveillance for wild poliovirus through reporting and laboratory testing of all cases of acute flaccid paralysis among children less than fifteen years of age.
Global Immunization Division (GID)
GID staff members work jointly with WHO and national Ministries of Health to plan and monitor polio surveillance and immunization activities in multiple countries worldwide.
Stop Transmission of Polio (STOP)
STOP team members currently participate in 11-month assignments in 42 countries, providing support at the national and sub-national levels. In 2018 alone, the STOP program, in collaboration with WHO and UNICEF, has deployed 314 public health professionals to improve surveillance for acute flaccid paralysis (AFP, an early sign of possible polio), support planning and implementing polio SIAs (supplementary immunization activities), responding to polio outbreaks, and enhancing polio surveillance.
Polio surveillance is primarily conducted through acute flaccid paralysis (AFP) surveillance supplemented by environmental surveillance of sewage samples. One recent Morbidity and Mortality Weekly Report (MMWR) describes recent analysis of both of these surveillance types, and how data collection has been affected by COVID-19.
Dive even deeper into polio surveillance by checking out the MMWR Polio Reports.
For ease of explaining and understanding the public health approach for this public health problem (polio), let’s focus on a 2013-2015 Middle Eastern Polio outbreak, when the World Health Organization (WHO) and CDC surveillance system known as the Early Warning Alert and Response Network (EWARN) first detected AFP cases in Syria. The lab tests identified 36 cases in Syria first, followed by confirming two more polio cases in Iraq.
- Risk Factor Identification (What is the cause?)
After we’ve identified the problem, the next question is, “What is the cause of the problem?” For example, are there factors that might make certain populations more susceptible to disease, such as something in the environment or certain behaviors that people are practicing?
Countries and regions experiencing active conflict, chronic insecurity, and large-scale displacement of persons are particularly vulnerable to outbreaks because of the disruption of health care and immunization services. The outbreak occurred 2 years after the onset of the Syrian civil war, resulted in 38 cases, and was the first time wild poliovirus as detected in Syria in approximately a decade.
Regional conflicts had prevented children from getting routine vaccinations, which put them at the highest risk for polio infection. The conflicts had forced people from their homes and into unsafe areas, challenging vaccination efforts. Other children at high risk for infection included those in remote, difficult-to-reach areas and in districts with low vaccination coverage. Routine vaccination coverage in the region was high before the war, which limited the number of children who were susceptible to the poliovirus and the size of the outbreak. The children who were most vulnerable to the disease were those born during the Syrian conflict.
- Intervention Evaluation (What works?)
Once we’ve identified the risk factors related to the problem, we ask, “what intervention works to address the problem?” We look at what has worked in the past in addressing this same problem and if a proposed intervention makes sense with our affected population.
After the polio cases were lab confirmed, Commander Derek Ehrhardt, BSN, MPH, MSN—CDC’s Global Immunization Division epidemiologist and Team Lead for the Eastern Mediterranean Region in the Polio Eradication Branch—immediately left for Geneva, Switzerland to work with other Global Polio Eradication Initiative (GPEI) partners: World Health Organization (WHO), UNICEF, Rotary Foundation, the Bill and Melinda Gates Foundation, and UNHCR, as well as eight ministries of health, which included Syria, Iraq, Jordan, Lebanon, Egypt, Iran, Palestine, and Turkey.
Ehrhardt worked closely with Mike Ryan, MD, WHO’s interagency team lead for GPEI technical experts. The interagency team traveled to the affected areas to collect and analyze information that Ehrhardt, Ryan, and other GPEI leads used to create a coordinated strategic response plan, considering each country’s unique culture.
“We needed a plan to reach the kids to vaccinate them against polio. We came up with a strategic response that involved three phases,” says Ehrhardt. Now it was up to CDC and the other GPEI partners, and the eight Middle Eastern Countries affected—Syria, Iraq, Jordan, Lebanon, Egypt, Iran, Palestine, and Turkey—to prevent polio from crossing borders and infecting polio-free countries.
- Implementation (How did we do it?)
In the last step, we ask, “How can we implement the intervention? Given the resources we have and what we know about the affected population, will this work?”
The interagency team created a 3-phase response plan, tailored to the specific challenges of the region during the conflict, to prevent additional polio spread and stop the outbreak.
The three phases they used were:
- Implementing numerous immunization campaigns in Syria and Iraq to vaccinate children against the poliovirus from October 2013 to April 2014
- Targeting intervention for high-risk groups for supplemental immunization activities (SIAs) to vaccinate those who had missed routine immunizations from May 2014 to January 2015.
- Strengthening routine immunization systems and conducting additional vaccination campaigns to catch up children who had missed some of their routine vaccines from February to October 2015 to increase polio immunity in the region.
To reach the many children who needed vaccinations, the response set up immunization sites at healthcare clinics, border crossings, and displaced person camps, as well as sent vaccinators house to house in some locations. Mobile vaccination teams also traveled to remote regions.
The response provided CDC and its global partners with insight and best-practice strategies for areas at high risk for disease outbreaks. Quick detection followed by a rapid response stopped the outbreak within six months by vaccinating about 27 million children, many of whom were in unsafe and difficult-to-access areas of conflict. Countries suffering active conflict continue to be at high risk for polio and other diseases, mainly because it is difficult to vaccinate displaced people who are in politically unstable areas.
As you can see, using The Public Health Approach helps public health professionals identify a problem, find out what is causing it, and determine what solutions/interventions work.
Special Feature – Polio Eradication
Did you know that Rotary International and their partners use the poliovirus vaccine and have immunized 2.5 billion children worldwide to date?
Unless polio is eradicated, within 10 years, as many as 200,000 new cases could occur around the world each year. In the past few years, only two countries have reported cases of polio caused by the wild virus, but no unvaccinated child anywhere is safe until every child is vaccinated.
Since Rotary International’s launch of its polio eradication program, PolioPlus, in 1985, it has contributed more than $2 billion to fight polio, including matching funds from the Gates Foundation and countless volunteer hours.
Since 1988, Rotary International has helped to reduce polio cases by 99.9%, and is a key member of the Global Polio Eradication Initiative (GPEI). Rotary International provides information about their mission on their website, including information on the history of polio, actions Rotary has already taken, and what future goals and plans are needed to eradicate polio.
The three interventions needed to ensure that polio is truly gone forever are:
- Detection: Requires continuous, costly surveillance in two parts
- Doctors and community health workers monitor children for acute flaccid paralysis (a symptom of polio).
- Local authorities collect samples from sewage systems or bodies of water in areas that don’t have adequate sanitation facilities, then send the samples to GPEI labs to test for poliovirus.
- Vaccination: Requires volunteers and funding
- Even after successful campaigns, Rotary must locate the small percentage of children who have been missed.
- Rotary helps fund planning by technical experts, large-scale communication efforts, and volunteer travel to everywhere, from large cities to rural areas.
- Eradication: Requires vaccinating children for three more years after the final case is recorded
Check out this article on the importance of eradication for more information.
Out of the CDC Museum Collection – Polio Eradication
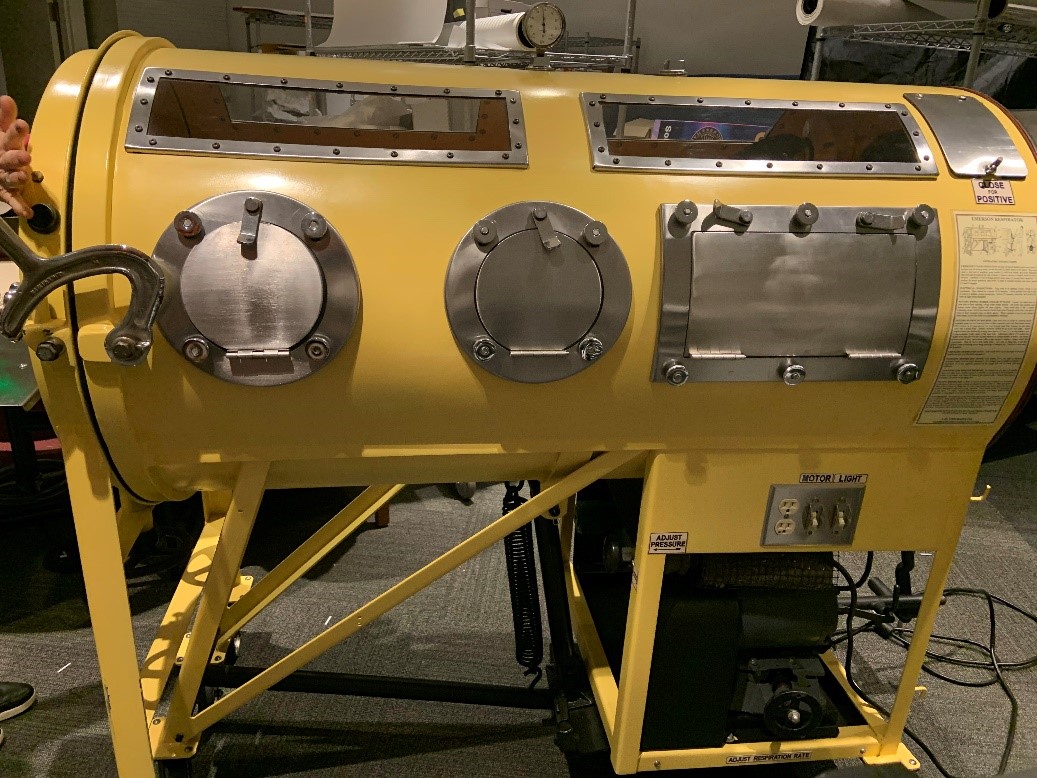
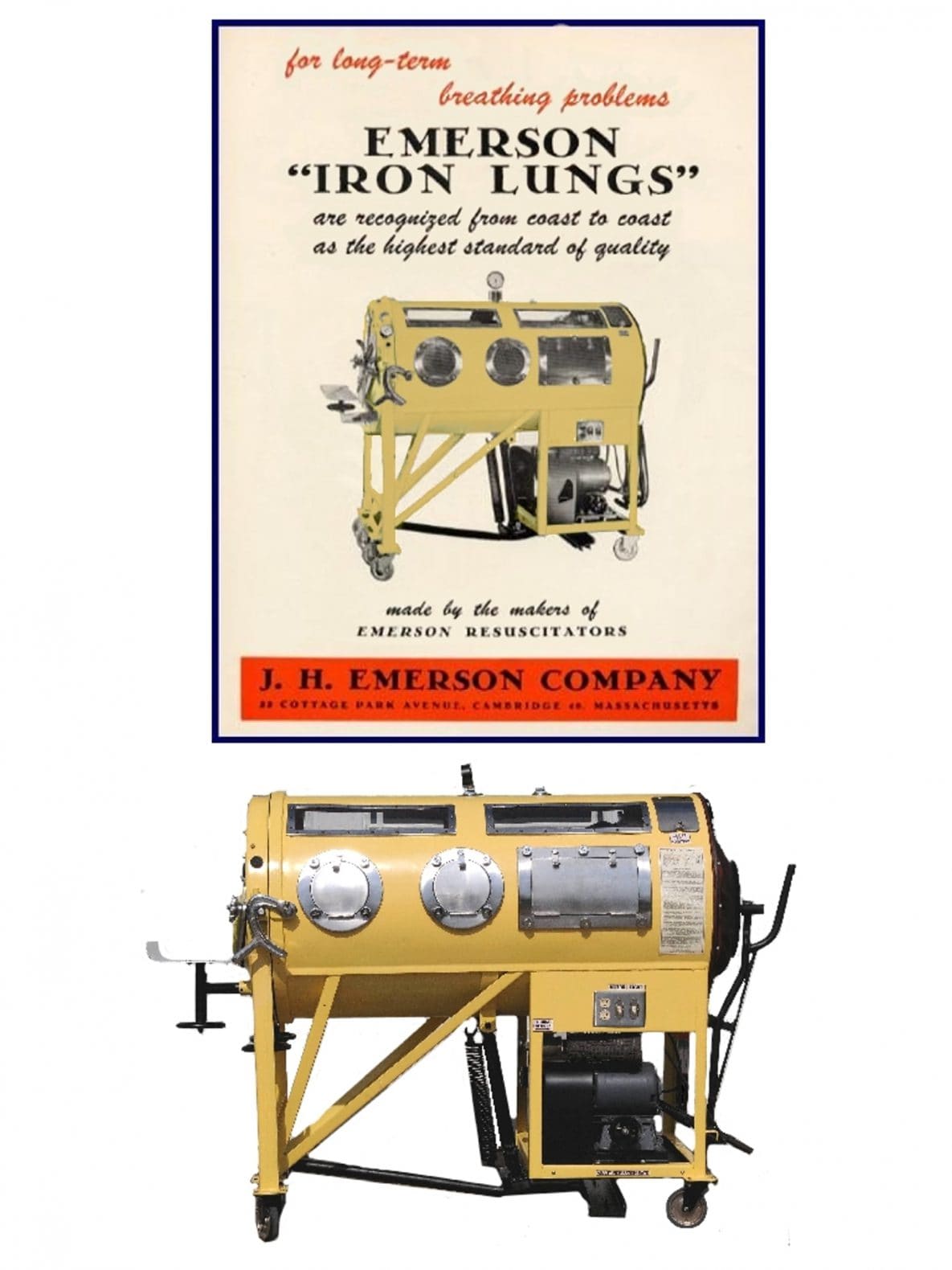
This month’s Out of the CDC Museum Collection features an object in the historic collection that serves as a reminder of the importance of eradicating polio. Pictured here is a pediatric iron lung. Iron lungs are ventilators used to help polio patients who experienced upper body paralysis breathe. This iron lung has been in the CDC Museum historic collection since 2010 when it was donated to the collection by Jack Kovalski. Mr. Kovalski is a polio survivor and works to restore iron lungs so they can be used to teach about the importance of vaccinations. Read about a polio survivor’s experience using an iron lung and watch this video on how the iron lung works.
Bonus – 75 Years of CDC!
CDC turned 75 in July!
In this August/September newsletter, our bonus will focus on some of CDC’s work from 1946-1949, specifically regarding outbreaks and response during CDC’s early years of operation. Here’s a timeline of some important events:
- On July 1, 1946, Malaria Control in War Areas, a program within the U.S. Public Health Service, transitions into the Communicable Disease Center (CDC).
- In 1947, CDC acquires the U.S. Public Health Service Plague Suppressive Laboratory which includes an epidemiology division.
- In 1947, CDC offers disaster aid in response to multiple chemical explosions in Texas City, Texas. Subsequently, CDC is designated as the official response agency for future epidemics and disasters.
- In 1947, CDC begins a five-year study on what role flies have in the spread and transmission of poliomyelitis.
- In 1948, Rabies investigation activities are conducted at the Virus & Rickettsia Laboratory in Montgomery, Alabama.
- In 1948, CDC assists the Imperial Iranian Government in planning and establishing a national malaria control program.
- In 1948, CDC conducts first training courses in Laboratory Diagnosis of Tuberculosis and Mycotic Diseases.
- In 1948, CDC investigations expand to include, typhus, dysentery-diarrheal, fly control-poliomyelitis, viral encephalitis, plague, Q fever, brucellosis, creeping eruption, rabies, histoplasmosis, insecticides, and rodenticides.
- In 1949, CDC’s Reference Diagnostic Service Center becomes available to all public health laboratories. Practicing physicians who have hard-to-identify specimens submit through their health departments.
- In 1949, The United States is declared free of malaria as a significant public health problem.
- In 1949, the last case of naturally occurring smallpox is reported in the United States.
Did you know?
- Approximately 5,000 animal rabies cases are reported annually to CDC, and more than 90% of those cases occur in wildlife.
- The number of rabies-related human deaths in the United States declined during the twentieth century, from more than 100 annually in the early 1900’s to just one or two per year since 1960.
- About 2,000 cases of malaria are diagnosed in the U.S. each year, the vast majority of which are in travelers and immigrants returning from countries where malaria transmission occurs.
- In 1980, the World Health Assembly declared smallpox eradicated.
- No cases of naturally occurring smallpox have happened since 1977.
Newsletter Activities
All August/September 2021 Teen Newsletter winners will be announced 9/28/21 during the Zoom – see individual deadlines below, as applicable.
Don’t forget! The CDC Museum Public Health Academy Teen Newsletter has the newsletter activity prize category: Future CDCer
To qualify for Future CDCer, you must participate in all newsletter activities (scavenger hunt—Goosechase, Zoom, social media challenge, Ask a CDCer, and pre-Zoom game—Kahoot). All who qualify will be entered into a prize drawing for a CDC Museum Public Health Academy t-shirt.
*The following newsletter activities: Scavenger Hunt, Zoom, and Social Media Challenge are available for your participation anytime – even after deadlines. To be eligible for prizes, you must complete activities by the deadline.
Want to do a fun digital scavenger hunt?
Time: ~20 min to complete
Complete all missions by 9/27/21 11pm ET, for prize drawing.
See below for more details.
Want to learn more from CDCers who work on polio eradication?
Join us for an exclusive Zoom on 9/28/21 at 8pm ET.
Advance registration is required. All who register by or on 9/28/21 3pm ET will be entered into a prize drawing.
Watch the polio eradication Teen Talk.
Help spread awareness about vaccines! Post your COVID-19 vaccine selfie, or promote any vaccine resource to encourage others to get vaccinated!
Post it on your social media using #CDCTeenNewsletter and tag @cdcmuseum on Insta.
Submit by 9/27/21 11pm ET to be entered into a prize drawing.
Do you have a question for a CDCer who works on polio eradication internationally or in the polio lab?
Submit your question for the polio experts who will be joining the Zoom on 9/28/21 at 8pm ET.
If your question is selected, you will get a shout out on the live Zoom and a prize.
Please do not submit questions that are answered by reading this newsletter.
Click to submit your question(s) by 9/27/21 11pm ET.
CDCM PHA Teen Newsletter Scavenger Hunt
August 2021
Step 1: Download the GooseChase iOS or Android app
Step 2: Choose to play as a guest
Step 3: Enter game code – R3RDGZ
Step 4: Enter password – CDC
Step 5: Enter your email as your player name (this is how we will contact you if you are the prize winner)
Step 6: Start at https://www.cdc.gov/polio/about/index.html to begin the missions.
Tips for Winning:
- All answers are found on the website, see Step 6.
- Open-ended answers and photo submissions are evaluated for accuracy.
- Complete all the missions by 9/27/21 11pm ET, to be entered into a drawing for a prize.
- Make sure to make your player name is your email.
Have fun!