If you have questions about the WTC Health Program, you can get help and information at the WTC Health Program call center at 1-888-982-4748.
The WTC Health Program Member Handbook is available for download below:
English and Spanish version updated as of April 2025. The updated Polish and Chinese language handbooks will be made available as soon as they are ready.
Previous versions of the Member Handbook are available upon request by emailing WTC@cdc.gov
Press Ctrl+F (Command+F on Mac) or use the search bar below to find information on the page quickly.
A Message from the Administrator
In This Section:
It is my pleasure to present you with the World Trade Center (WTC) Health Program Member Handbook. I hope this handbook helps you find Program information quickly and easily, and that it makes Program benefits and policies easier to understand.
We know that you depend on the WTC Health Program for high-quality, compassionate care for your WTC-related health care needs. Your trust, satisfaction, and success in the Program are very important to us.
We are honored to serve you.

Sincerely,

John Howard, M.D.
Administrator, World Trade Center Health Program
About the Administrator
John Howard, MD, MPH, JD, LLM, MBA, is board-certified in internal medicine and occupational medicine. He is admitted to the practice of medicine and law in the State of California and in the District of Columbia. He is a member of the U.S. Supreme Court bar. He has written numerous articles on occupational health law and policy and serves as a professorial lecturer in environmental and occupational health in the Milken Institute School of Public Health at The George Washington University in Washington, D.C.
In addition to serving as the Administrator of the WTC Health Program, he also serves as Director of the National Institute for Occupational Safety and Health (NIOSH).
Learn more about Dr. Howard on the National Institute for Occupational Safety and Health (NIOSH) Leadership page.
About Your Member Handbook
This Handbook will help you better understand the benefits and services available to you as a member of the World Trade Center (WTC) Health Program.
This Handbook has seven sections:
- Important Information for Members
- Benefits and Services
- Covered Conditions and Certifications
- Treatment in the WTC Health Program
- Pharmacy Benefits
- Program Policies, Privacy, and Support
- Glossary
Each one of these sections will explore that area of the Program in more detail.
Throughout the Handbook you will see a few symbols to highlight important information we don’t want you to miss:
Important note
Who to contact for help
More info online
Key Program term
Terms that are highlighted in purple are key terms with definitions in the Glossary.
In this section we've included important information for new members and helpful contact information for various parts of the Program. There is also a handy section for you to write down key details about your membership.
This handbook is not a legal document. It provides general Program information in a way that is easy for you to use and understand.
About the WTC Health Program
In This Section:
On January 2, 2011, President Obama signed the James Zadroga 9/11 Health and Compensation Act of 2010 (Zadroga Act) into law (Public Law 111-347). The Zadroga Act extended and improved protections and services to individuals directly impacted by September 11, 2001 and amended the Public Health Service Act to establish the World Trade Center Health Program.
The Zadroga Act established or reauthorized the following three programs that help those directly affected by the September 11, 2001, attacks:
- The World Trade Center (WTC) Health Program;
- The September 11th Victim Compensation Fund (VCF); and
- The WTC Health Registry
For more information about the laws that authorize the Program visit the Program Laws page.
The WTC Health Program provides WTC-related medical and mental health services at no cost to you. This means high-quality, compassionate care with no copayments, deductibles, or other out-of-pocket expenses for medically necessary treatment of your certified WTC-related health condition(s) or a health condition medically associated with your certified WTC-related health condition.
The WTC Health Program is authorized by the Zadroga Act to provide benefits to these categories of individuals:
-
WTC Responders: workers or volunteers who provided rescue, recovery, debris cleanup, and related support services on or in the aftermath of the September 11, 2001, attacks for certain amounts of time during the period between September 11, 2001, and July 31, 2002.
- There are three types of responders: FDNY Responders, NYC General Responders (including NYPD), and Pentagon and Shanksville, PA, Responders.
- WTC Survivors: individuals who were present in the New York City (NYC) Disaster Area in the dust or dust cloud on September 11, 2001; who worked, resided, or attended school, childcare, or adult daycare in the NYC Disaster Area from September 11, 2001, to July 31, 2002; who were eligible for certain residential grants or whose place of employment was eligible for certain grants following the September 11, 2001, attacks through May 2003.
Program Statistics
Statistics on the WTC Health Program are updated quarterly and available on the Program Statistics webpage. Available statistics include:
- Trends/features of member population,
- Application & New enrollment trends,
- Certification trends,
- Medical utilization trends,
- Pharmacy utilization trends, and
- Member feedback/interactions.
Learn more about the Program and its history on the About Us page.
New to the WTC Health Program
In This Section:
If you are new to the WTC Health Program, welcome. We are dedicated to providing you with compassionate, expert care for WTC-related conditions. There are some important things to remember as you get familiar with the Program.
- We are a limited federal benefits program administered by the National Institute for Occupational Safety and Health (NIOSH) within the U.S. Centers for Disease Control and Prevention (CDC).
- We provide medical monitoring and treatment for certified WTC-related conditions only.
- We do not replace your primary health insurance, and are not a health insurance provider. You must maintain your other health insurance to receive treatment through the Program.
- WTC-related care must be authorized and provided by a WTC Health Program Participating Provider (e.g., doctor, specialist, clinician).
- We are a separate program from the September 11th Victim Compensation Fund (VCF), administered by the U.S. Department of Justice (DOJ), and the WTC Health Registry.
The first step for every new member is getting an initial health evaluation. This is the first medical exam within the Program and looks for potential WTC-related health condition(s). For Responder members, this is also your first monitoring exam. Your Program welcome letter will have more information about your Clinical Center of Excellence or the Nationwide Provider Network and next steps for scheduling this exam.
Here are some helpful tips to prepare for your initial health evaluation:
Review this handbook to learn about your program benefits, rights, and responsibilities.
Complete any paperwork provided by your program clinic prior to your first visit.
Bring your medical records and any workers’ comp or line-of-duty injury paperwork with you.
Write down a list of...
- Any symptoms, even if you think they may not be related to your 9/11 exposures.
- Questions for the provider or doctor.
- Any medications you are currently taking.
Be prepared to talk about your exposure, work history (if applicable), and your current symptoms
Survivors: Present your primary health insurance card at this and every visit.
Important Contact Information
If you are experiencing a medical emergency, call 911. If you are experiencing a mental health crisis or thoughts of self-harm, call or text 988.
WTC Health Program Member Services
Enrollment, Program benefits and policies, appeals, or to update your contact info
Call 888-982-4748 (M-F 9a-5p ET) or email wtc@cdc.gov
Express Scripts, Inc.
Pharmacy benefits, home delivery services, or issues filling a prescription
Call 800-935-7179 or visit the Express Scripts Portal
Clinical Centers of Excellence or Nationwide Provider Network
Scheduling appointments, care and treatment, medications, provider authorizations and denials, case management, clinic transfers, and certifications.
Responder Clinical Centers of Excellence
| CCE | Phone |
|---|---|
| FDNY |
212-570-1693 (Manhattan) 718-999-1858 (All other locations) |
| Mount Sinai | 212-241-1554 |
| New York University | 212-263-7335 |
| Northwell Health | 718-267-2420 |
| Rutgers | 848-445-0123 |
| Stony Brook | 631-855-1200 |
Survivor Clinical Centers of Excellence
| CCE | Phone |
|---|---|
| NYC Health + Hospitals | 877-982-0107 (for all locations) |
| William Street Clinic (Optum Serve) | 800-714-7426 |
Nationwide Provider Network
| CCE | Phone |
|---|---|
| Managed Care Advisors (MCA)-Sedgwick |
800-416-2898 Callers in U.S., U.S. territories, and Canada 614-362-2641 International callers outside U.S., U.S. territories, and Canada (International rates may apply) |
Program Feedback
Submit formal feedback to the Program or write to the Administrator at CDC/NIOSH, WTC Health Program, 400 7th Street SW, Suite 5W, Washington, DC 20024
Fill Out This Page For Your Reference
Print this page and write down your key membership details here for your quick reference.
Membership Details [PDF, 1 page, 46 KB]
Important Information for Members
In This Section:
- Key Facts about the Program
- Member rights and responsibilities
- Billing in the WTC Health Program
- Making Appointments
- Other Program Information
The World Trade Center (WTC) Health Program provides health care for certified WTC-related health conditions and health conditions medically associated with a certified WTC-related health condition at no out-of-pocket cost. In the New York (NY) metropolitan area, care is provided through multiple Clinical Centers of Excellence (CCE) locations. The Nationwide Provider Network (NPN) provides care for members who live outside the NY metropolitan area.
WTC Health Program Participating Providers are 9/11 health experts with special skills in the diagnosis and treatment of WTC-related physical and mental health conditions. These providers are able to offer the expertise, time, and space you need to talk about your conditions, your treatments, and your 9/11 experience.
Learn more about providers who treat members.
Key Facts about the Program
- Administered by the National Institute for Occupational Safety and Health (NIOSH), part of the U.S. Centers for Disease Control and Prevention (CDC) in the U.S. Department of Health and Human Services (HHS).
- Established as a federal program by the James Zadroga 9/11 Health and Compensation Act of 2010 (Zadroga Act). The Program is authorized until 2090.
- Serves over 130,000 currently enrolled 9/11 responders and survivors from the World Trade Center in New York City and related sites, and responders from the Pentagon and Shanksville, Pennsylvania sites. There is no deadline to enroll.
- Is a limited health benefits program that covers initial health evaluations, annual monitoring exams, and medically necessary medical and mental health treatment for certified WTC-related health conditions only.
- Does not replace your primary health insurance, and is not a health insurance provider. You must maintain your other health insurance to receive treatment through the Program.
- Administers monitoring and medically necessary treatment for certified conditions through Clinical Centers of Excellence in the New York metropolitan area and in all 50 U.S. states and territories through a Nationwide Provider Network.
- Is a separate program from the September 11th Victim Compensation Fund (VCF). The VCF provides financial compensation and is administered by the DOJ. The VCF and WTC Health Program have different eligibility criteria and enrollment processes.
James Zadroga 9/11 Health and Compensation Act (Zadroga Act): Public Law 111-347 passed by the U.S. Congress in 2010 that created the WTC Health Program.
Member rights and responsibilities
Your Rights as a WTC Health Program Member
- Be assured of privacy and confidentiality: The Program handles your personal health information in a manner that preserves and protects your privacy and confidentiality. This includes, but is not limited to, the maintenance of medical records in a secure environment and the education of Program staff regarding confidentiality. The Program will not release medical information without authorization, except as required or permitted by law to administer benefits, comply with government requirements, or if you consent to participate in research or education.
- Have access to treatment: You have the right to receive medically necessary treatment for a certified WTC-related health condition(s) if the condition(s) is certified by the Program. In addition, you have the right to be informed about the risks and benefits of treatment and to refuse care.
- Appeal decisions: You have a right to appeal certain decisions by the Program, including an enrollment denial, disenrollment, certification denial, decertification, and treatment denial.
- Voice complaints/grievances related to the Program: You have the right to voice your concerns and receive a prompt and fair review of any complaints you may have about the Program.
- Receive considerate, respectful care: In the Program, we strive to treat all members equally and with respect and dignity, regardless of race, religion, sex, sexual orientation, national origin, age, disability, or income. If you have any concerns about how you are being treated, please contact the Program’s call center at 1-888-982-4748.
Learn more about your rights and Program policies in the Policies section.
Your Responsibilities as a WTC Health Program Member
- Knowing the extent and limitations of the Program’s services: This handbook provides information about the Program to help you better understand the Program’s benefits and services. Contact the Program’s call center or website if you have questions.
- Keeping appointments: You have a responsibility to keep your appointments. If you are unable to keep your appointment, notify your Program CCE or NPN case manager within 24 hours of your appointment so that your appointment time can be given to another member.
- Providing accurate and complete information: You are responsible for providing accurate and complete information about your present and past medical conditions and 9/11 exposures to the Program. You are also responsible for submitting appropriate signed medical release forms so that the Program can obtain medical records as needed. Survivors must share primary insurance information whenever you receive care for certified WTC-related health conditions.
- Active participation in your care: You have a responsibility to participate in your care by asking questions to understand your certified WTC-related health condition(s), following the recommended treatment plan, managing your medications, and making healthy lifestyle choices to try to maintain your health and prevent illness.
- Fulfilling financial obligations: Treatment of your certified WTC-related health conditions will be provided at no cost to you as long as the provider is a WTC Health Program Participating Provider with the Program and the services are appropriately authorized. Depending on the type of treatment services you need, services must be authorized by your WTC Health Program doctor or NPN case manager, your CCE or the NPN Medical Director, or the Program.
- Showing consideration and respect: You have a responsibility to show consideration and respect to Program providers and staff at all times. Disruptive, abusive, or threatening behavior may impact the Program’s ability to provide benefits to you.
WTC Health Program Participating Provider: A Network Provider that has agreed to the Program’s terms and conditions and is able to provide services to WTC Health Program members. These may also be referred to as participating providers, or Program providers.
Disruptive and Abusive Behavior
Everyone has the right to a safe working environment, and all Program members deserve care in a safe environment. Disruptive or abusive behavior by a WTC Health Program applicant, member, or designated representative (including attorneys) at or directed towards other patients, a facility, or personnel affiliated with the Program (e.g., a Clinical Center of Excellence (CCE), the Nationwide Provider Network (NPN), providers, or staff) will not be tolerated.
These types of behavior include, but are not limited to:
- Acts of violence or threats against staff or other patients, including verbal or physical abuse;
- Rude or vulgar language, including cursing or shouting;
- Throwing and striking objects;
- Harassing or stalking;
- Concealing or using a weapon; and
- Engaging in criminal behavior.
Depending on the particular circumstances, members who engage in such behaviors:
- May have their care suspended by their CCE or NPN provider;
- May be required to sign a behavioral agreement outlining what will be expected of them in order to receive care from their provider;
- May be required to transfer to another CCE or NPN provider; or
- May be subject to other appropriate actions, including involvement of law enforcement authorities as necessary.
The Program strives to provide high-quality, compassionate care for members’ WTC-related health needs. Disruptive or abusive behavior, however, may impact the Program’s ability to provide benefits in a timely manner.
Health Insurance Requirement
The WTC Health Program does not replace your primary health insurance. The Zadroga Act requires all Program members to have qualifying health insurance unless they meet one of the exceptions in the Affordable Care Act.
Your primary health insurance must cover the 10 essential health benefits as outlined by the Patient Protection and Affordable Care Act of 2010 (i.e., “minimum essential coverage”). This means you must have both pharmacy and medical coverage. All members must share their primary health insurance information with their CCE or the NPN and any participating provider.
If you do not have health insurance your CCE or the NPN can help you find and apply for public or private health insurance, such as Medicaid, Medicare, health insurance offered through Healthcare.gov , or other options.
For Survivors
As a Survivor in the WTC Health Program, your primary health insurance plays a critical role in providing your benefits at no out-of-pocket cost. This is because of a process called Coordination of Benefits that is required by the Zadroga Act.
Learn more about Coordination of Benefits.
For Responders
As a Responder in the WTC Health Program, your health insurance will not be billed for care for your certified WTC-related health conditions. Please remember, your WTC-related care must be authorized and received through the WTC Health Program and its providers to be covered.
The health insurance requirement ensures that you have minimum essential health coverage for any condition(s) or service(s) received that are not covered by the Program.
For All Members
The Program covers the cost of treatment for certified WTC-related health conditions only. You must use your primary health insurance or pay out-of-pocket for any care related to a health condition not certified by the Program. Your CCE or the NPN can advise you on how to find care for any health conditions not certified by the Program.
Learn more about the health insurance requirement on the Health Insurance Requirement page.
Billing in the WTC Health Program
Your CCE, the NPN, or WTC-provider where you received services will bill medical claims to the Program. Pharmacy claims are billed at the pharmacy at the time they are filled.
If you receive WTC-related health care from a provider that is not located at a CCE or that is a NPN provider, please be prepared since they may not be as familiar with the Program. Please let the provider staff know that the visit is for a certified WTC-related health condition. This will help make sure that the visit is billed properly. Members should also be prepared to present proof of other health insurance at the time of their visit.
For Survivors who get WTC-related medications at a retail pharmacy, please tell your pharmacy to bill your primary insurance first, including any public insurance (such as Medicare or Medicaid), and then the WTC Health Program for any remaining amount. You should not pay any money out of pocket for your WTC-related prescriptions.
What to do if you receive a bill
If you receive a document that looks like you might owe money for a WTC-related service
Contact the WTC Health Program call center, your Clinical Center of Excellence, or the Nationwide Provider Network as soon as you can. We will work with you and the provider on next steps.
If you are asked to pay something (such as a copay, etc.) when at a WTC-related appointment
Tell the provider that as a member of the WTC Health Program, you do not need to pay anything for treatment of your certified WTC-related health condition(s). Have the provider call your Clinical Center of Excellence, the Nationwide Provider Network, or the Program call center. We will work it out with them.
If you are a member of the Nationwide Provider Network, also show the provider your NPN member ID card. It contains important information for them including claim submission and contact details.
Visit the Billing page for more information on what to do if you mistakenly get a bill for WTC-related services.
Why you might receive a bill by mistake
The process of paying claims for care received in the Program is different from other health programs. Because of the complexity of the process, mistakes can happen and you may receive a bill from a participating provider or be asked to pay a co-pay for covered treatment for your certified WTC-related condition.
If the bill or co-pay is for covered treatment, do not pay. Contact the WTC Health Program or your CCE or NPN.
Some examples of why Program billing is so complex are:
- CCEs may refer some members to outside providers for specialized care. These providers and their offices may not have as much experience working with the Program.
- The NPN is made up of WTC Health Program Participating Providers all across the country who may only see Program members occasionally.
-
Survivor claims must follow a Coordination of Benefits process, while Responder claims do not use this process.
- After benefits are coordinated, a Survivor’s primary insurance or provider may send what is called an Explanation of Benefits for care you receive through the Program. This looks like a bill, but it is not. Please be sure to read all materials sent to you from the Program or your insurance carefully to determine the difference.
- Responder claims are only sent to the Program. It is possible that a provider may bill a Responder’s health insurance instead of the Program and then the Responder would receive a bill. Responders should make sure that their claims for treatment of their certified WTC-related health condition are sent to the Program, and not to their health insurance.
We do our best to educate providers and to remind them how to process WTC Health Program claims. However, you may still mistakenly receive a bill for this WTC-related care because of the complicated process or because your participating provider sees Program members infrequently. You might also be mistakenly asked to pay a co-pay at the WTC Health Program Participating Provider's office.
Remember: Do not pay! The Program is not able to reimburse you if you do.
Workers’ Compensation Recoupment
If you have an established workers’ compensation case for a certified WTC-related health condition(s), the WTC Health Program will bill your workers’ compensation insurance carrier for the cost of the treatment of those conditions. This is known as recoupment and applies to both Responders and Survivors. The exception to this recoupment requirement is if your workers’ compensation case is part of a New York City-funded law or plan including, but not limited to, line-of-duty plans.
If you are waiting for your workers’ compensation case to be established, the Program will continue to pay for any medically necessary services needed to treat your certified WTC-related health condition(s) until the case is established. If your workers’ compensation case is denied, then the WTC Health Program will cover the cost for the medically necessary treatment of your certified WTC-related health condition(s).
Workers’ Compensation Settlements
Some workers decide to settle their workers’ compensation claims. The worker enters into a settlement agreement, called a Section 32 Waiver Agreement, with the workers’ compensation insurance carrier. The insurance carrier gives the worker a lump sum of money to close the case forever. Sometimes, Section 32 Waiver Agreements release the insurance carrier from having to pay any future medical costs for the worker’s injury or illness.
Any Section 32 Wavier Agreement entered into between a Program member and an insurance carrier must protect the WTC Health Program’s interests. In some cases, the Program will require that money from a Section 32 Waiver Agreement be set aside to cover future medical expenses that should have been paid by workers’ compensation, like the costs of medical treatment and medications for certified WTC-related health condition(s).
If you consider entering into a Section 32 Waiver Agreement, you must ask the Program to review the proposed settlement. This review determines if the proposed settlement amount is enough to cover future medical costs for your certified WTC-related health condition(s).
For more information about the Program’s recoupment policy, view the Workers’ Compensation FAQs .
Coordination of Benefits (for Survivors only)
Coordination of Benefits is a process that helps determine who pays a medical bill first when there is more than one potential payor (e.g., private insurance, Medicare, the Program). The Zadroga Act, as amended, requires medical and pharmacy claims for Survivor members go through this process.
Coordination of Benefits does not apply to the one-time initial health evaluation, annual monitoring exams, and related diagnostics for Screening-Eligible Survivors. The WTC Health Program covers that cost directly.
Screening-Eligible Survivor: A Survivor member that does not have a certified WTC-related health condition.
How Coordination of Benefits works
The Program is the payor of last resort. All treatment, medication, and other medical monitoring for Certified-Eligible Survivors are billed to all other health insurances first, including your primary health insurance. Once your health insurance(s) have paid, the Program pays any remaining amount.
Payor of last resort: The entity that pays last when there are multiple entities paying a bill.
Certified-Eligible Survivor: A Survivor member that has one or more certified WTC-related health conditions.
This leaves no out-of-pocket cost to you. You are not responsible for paying any co-insurance charges, copayments, or deductibles for care of your certified WTC-related health conditions so long as that care is received from a participating provider and approved by the Program.
Please note: If your certified condition is work-related and you have a workers’ compensation claim for the condition, then workers’ compensation is the primary payor. The Program will pay initially and then seek recoupment from either your workers’ compensation carrier or your settlement, where applicable.
For more information about workers’ compensation and recoupment, see the Workers' Compensation Recoupment section.
Survivors must share their primary health insurance (private and public) information when visiting a CCE, participating provider, or retail pharmacy so that coordination of benefits can occur.
What Survivors need to do to coordinate benefits
You play an important role in helping us coordinate your benefits. All Survivors must follow these steps so the WTC Health Program can make payments for your medical treatment and/or prescriptions for your certified WTC-related health condition(s).
1. Sign up for primary health insurance
2. Share your insurance information with your CCE or the NPN
3. Make sure your program provider is also in your primary health insurance network
4. Show your insurance card when receiving WTC-related care or filling a WTC-related prescription
5. Follow all requirements of your primary health insurance
1.
Sign up for primary health insurance.
2.
Share your insurance information with your CCE or the NPN
3.
Make sure your program provider is also in your primary health insurance network.
4.
Show your insurance card when receiving WTC-related care or filling a WTC-related prescription
5.
Follow all requirements of your primary health insurance
Steps for Survivors
- Sign up for primary health insurance if you are not already covered.
- Share your current primary health insurance information with your CCE or the NPN as soon as possible. Be sure to update your CCE or the NPN whenever this changes.
- Make sure that any WTC Health Program provider you see is also in your primary health insurance plan’s network.
- Show your primary health insurance card and Program pharmacy card at every treatment visit.
- Follow all requirements of your primary health insurance, including prior authorization requirements.
For more information on Coordination of Benefits, visit the Coordination of Benefits page.
Making Appointments
How to Make an Appointment with a CCE
Current CCE Members
Contact your CCE directly for medical appointment scheduling and any questions or issues related to your care. The WTC Health Program call center cannot schedule or change appointments.
New CCE Members
Your Program enrollment welcome letter contains specific information on how to schedule an initial health evaluation at one of the CCEs. If you have questions, please call the WTC Health Program call center at 888-982-4748 or contact your assigned CCE.
For a list of clinics, visit the Clinics page.
How to Make an Appointment with the NPN
Current NPN Members
Appointments can be made directly with your WTC Health Program Participating Provider. If you do not have an NPN provider, you can call Managed Care Advisors (MCA)-Sedgwick at 800-416-2898. More information regarding your appointments and care is available via the NPN Member Portal .
New NPN Members
Shortly after you receive your Program welcome letter, you will receive a new member packet from the NPN, administered by MCA-Sedgwick. This will include information on scheduling your first exam and how to sign up for the NPN Member Portal.
MCA-Sedgwick will schedule your first appointments for you. For questions about how to schedule your NPN appointments, call MCA-Sedgwick NPN Member Services at 800-416-2898 Monday through Friday, 8am to 8pm ET.
Important information about making appointments with the NPN is available on the Sedgwick FAQ page .
Travel Expenses (For NPN Members Only)
Travel expenses are available on a limited basis under the Program for members of the NPN. Transportation and lodging expenses for medically necessary care within the U.S. may be allowed on a case-by-case basis.
For reimbursement to be considered, certain criteria (such as the need to travel over 250 roundtrip miles for necessary medical care) must be met and approved in advance of any travel. Please speak to your NPN case manager for additional information.
Contact MCA-Sedgwick directly at 800-416-2898 for issues related to your care.
Canceling and Rescheduling Appointments
There are times that you may need to cancel or reschedule your appointment at the CCE or with a participating provider in the NPN. If you need to cancel or reschedule an appointment:
- With a CCE, please call your clinic with at least 24 hours notice so that your appointment time can be offered to another member.
- With a WTC Health Program Participating Provider in the NPN, please follow the canceling and rescheduling policies of that provider or practice.
Other Program Information
Transferring Clinics
WTC Health Program members are allowed to change their clinic once a year.
In some limited circumstances, you can transfer your care to a new CCE even if it has been less than a year since you began care at your current CCE.
Responders can transfer between any Responder CCE or the Nationwide Provider Network (NPN); Survivors can only transfer between NYC Health + Hospitals, William Street Clinic, and the NPN.
You can request a transfer by informing your current CCE or NPN by phone or in person that you would like to transfer to a different CCE or another doctor in the NPN.
For more detailed information on the process of transferring clinics and how long it takes, visit the Transferring Clinics page.
Designated Representatives
A designated representative is someone you appoint and authorize to act on your behalf and represent your administrative interests in the WTC Health Program. Members can only have one designated representative at a time. However, you can change your designated representative at any time. The person you designate may not make medical care (e.g., treatment) decisions for you.
For more information about designated representatives, see the Designated Representatives section.
Help Others Impacted by 9/11
Contribute to 9/11 Health Research
World Trade Center Health Program research plays a vital role in the treatment of your condition and the Program’s ability to add a condition to the List of WTC-Related Health Conditions.
For members in the NY metropolitan area, when you come in for an exam you will be asked if the CCE can add your medical information to the data which researchers use to understand 9/11 health effects.
Responders in the NPN are also able to participate in this research by consenting to share their medical information with researchers.
Participation is optional and any information collected is maintained in accordance with strict requirements for privacy and confidentiality. You will receive your exam and continue to receive treatment, even if you do not agree to share medical information for research purposes.
Learn more about the Program's research.
Spread the Word about the Program
It is estimated that more than 400,000 people were directly impacted by 9/11 and its aftermath. With over 130,000 members currently enrolled, there are many more people that may not know they are eligible for health benefits through the WTC Health Program.
Word of mouth is one of the most effective ways to promote the WTC Health Program. We need your help to spread the word!
The WTC Health Program covers:
- WTC general responders (worker or volunteer who provided rescue, recovery, debris cleanup or related support services).
- Active or retired FDNY responders and certain family members.
- WTC survivors (people who were present on 9/11 or who lived, worked, visited, or went to school or daycare in the NYC Disaster Area or those with certain grants from the Lower Manhattan Development Corporation).
- Responders to the Pentagon and Shanksville, PA sites including active or retired members of a fire or police department (fire or emergency personnel), recovery or cleanup contractors, volunteers, employees of the Department of Defense or any other Federal agency, contractors of the Department of Defense or any other Federal agency between September 11, 2001, and September 18, 2001, or members of a regular or reserve component of the uniformed services.
Do you know someone who was there on 9/11 or in the days, weeks, or months after?
Encourage them to visit the Program website or call the Program call center at 1-888-982-4748 to learn more.
Learn more about the Program and how to apply on the Interest page.
Benefits and Services
In This Section:
Through the Zadroga Act and its implementing regulations, the WTC Health Program is able to provide WTC-related medical and mental health services at no out-of-pocket cost.
This means access to high-quality, compassionate care without any copayments, deductibles, or other out-of-pocket expenses for medically necessary treatment of certified WTC-related health conditions.
The services available to you depend on what type of enrolled member you are:
| Initial Health Evaluation | Annual Monitoring Exams | Medical and Mental Health Treatment (condition must be certified) | Select Cancer Screenings (if age and risk guidelines are met) | Benefits Counseling | |
|---|---|---|---|---|---|
| Responders | |||||
| Certified-Eligible Survivors | |||||
| Screening-Eligible Survivors |
* Screening-Eligible Survivors receive select cancer screenings for six months from the date of initial health evaluation.
Where you get care
The Program covers medically necessary healthcare services within the United States and its territories, including the District of Columbia, Guam, the Commonwealth of Puerto Rico, the Northern Mariana Islands, the Virgin Islands, American Samoa, and the Trust Territory of the Pacific Islands.
These benefits and services are provided through Clinical Centers of Excellence for members in the New York (NY) metropolitan area. Members outside of the NY metropolitan area receive care through the Nationwide Provider Network.
The WTC Health Program does not cover medical care, pharmacy products, or supplies received outside of the United States or its territories.
Clinical Centers of Excellence
Care for both Responders and Survivors in the New York (NY) metropolitan area is provided through designated WTC Health Program Clinical Centers of Excellence (CCEs). CCE providers specialize in diagnosing and treating certified WTC-related health conditions.
Even if you reside outside of the NY metropolitan area, you can choose to receive your care at a CCE. However, the Program does not cover travel expenses for you to get to a CCE appointment.
For clinic contact information, see Important Contact Information.
General Responder CCEs
There are five General Responder CCEs in the NY metropolitan area:
| CCE | Locations |
|---|---|
|
Icahn School of Medicine at Mount Sinai Selikoff Centers for Occupational Health WTC Health Program Clinical Center of Excellence at Mount Sinai |
|
|
New York University Grossman School of Medicine NYUGSOM WTC Health Program Clinical Center of Excellence |
|
|
Northwell Health Northwell WTC Clinical Center |
|
|
Rutgers, The State University of New Jersey Environmental & Occupational Health Sciences Institute World Trade Center Health Program at Rutgers |
|
|
State University of New York, Stony Brook Stony Brook WTC Health and Wellness Program; Long Island Clinical Center of Excellence at Stony Brook Medicine |
|
FDNY Responder CCEs
The Fire Department of the City of New York (FDNY) has several clinic locations throughout the NY metropolitan area that serve FDNY Responders:
| FDNY CCE | Location |
|---|---|
| FDNY Headquarters | Brooklyn |
| Brentwood | Suffolk County |
| Commack (physical health services only) | Suffolk County |
| Fort Totten | Queens (Bayside) |
| Manhattan (mental health services only) | NoLita |
| Middletown | Orange County |
| Staten Island | Castleton Corners |
Survivor CCEs
There are two Survivor CCEs in the NY metropolitan area:
| CCE | Location |
|---|---|
|
NYC Health + Hospitals System WTC Environmental Health Center |
Manhattan (32nd Street) Manhattan (Gouverneur) Queens (Elmhurst) |
|
William Street Clinic Operated by Optum Serve (formerly LHI) |
Lower Manhattan |
Nationwide Provider Network
Members who live outside the New York metropolitan area receive their WTC Health Program benefits through the Nationwide Provider Network (NPN). The NPN is a network of WTC Health Program Participating Providers throughout the country who provide WTC-related services. Members in the NPN get the same Program benefits as members who go to the CCEs.
Network: The health care providers, facilities, and pharmacies the Program has contracted with to provide you with health care services covered by the Program.
The NPN is different than the CCEs based in the New York metropolitan area. Unlike the CCEs, the NPN has no central clinic. Instead, a healthcare delivery company provides a network of individual providers or provider groups nationwide. Managed Care Advisors (MCA)-Sedgwick administers the NPN.
MCA-Sedgwick oversees the day-to-day operations of the NPN by:
- Building and expanding the available provider network
- Scheduling initial health evaluations, annual monitoring exams, and diagnostic appointments
- Submitting WTC-related health condition certification requests to the WTC Health Program
- Maintaining medical records for NPN members
- Operating an NPN-specific call center and online member portal
Since individual doctors and clinicians with their own specialties make up the NPN, you may need to go to more than one participating provider to receive care for each of your certified WTC-related health conditions.
If you live in an urban area, the NPN will try to find you care within 30 miles of your residence. If you live in a rural area, the NPN will try to find you care within 75 miles of your residence. If you would like to learn more about the location of local participating providers available to you through the NPN, please contact the NPN directly.
Program Exams
Monitoring, Diagnostic, and Screening Services
Initial Health Evaluations
Initial health evaluations are given to each new member of the World Trade Center (WTC) Health Program at no cost to you.
The purpose of the initial health evaluation is to find out if you have any conditions related to your 9/11 exposures that are covered by the Program. Only doctors who are WTC Health Program Participating Providers may conduct an initial health evaluation.
For more information on covered conditions, see the Covered Conditions section.
An initial health evaluation may include the following services:
- 9/11 exposure assessment;
- Blood tests;
- Medical history and mental health questionnaires;
- Physical examination;
- Urinalysis (urine test);
- Vital signs (blood pressure, pulse);
- Chest X-ray, if medically necessary;
- EKG (heart test), if medically necessary; and
- Spirometry/Pulmonary function testing (breathing test).
9/11 Exposure Assessment: A questionnaire used to gather a comprehensive and medically relevant exposure history that helps physicians determine if 9/11 exposures are substantially likely to be a significant factor in aggravating, contributing to, or causing conditions that may be submitted to the Program for a certification request.
Responders
When you first enroll, the Program provides an initial health evaluation to all members, Responders included. The Program provides Responders yearly follow-up exams called annual monitoring exams, whether you are sick or not.
Survivors
New Survivor enrollees in the Program are called Screening-Eligible Survivors. The Program offers a one-time initial health evaluation to all Screening-Eligible Survivors at no cost. The Zadroga Act allows only one initial health evaluation to be paid for by the Program. Therefore, Survivors should have symptoms of a WTC-related health condition before scheduling their initial health evaluation.
For a Screening-Eligible Survivor, if your initial health evaluation does not result in any certifications, you remain a member of the Program. If you later feel a new health problem may be WTC-related, you can use your primary health insurance or pay out–of–pocket for an additional health evaluation by a WTC Health Program Participating Provider.
Until you have an initial health evaluation, most Program benefits are not available to you. If you receive your initial health evaluation and are not diagnosed with a certified WTC-related condition, you can receive selected cancer screenings covered by the Program for six (6) months.
As a Survivor, if you are certified as having a WTC-related health condition, then your status is changed to a Certified-Eligible Survivor. You are then eligible for Program benefits, such as yearly follow-up exams called annual monitoring exams, medical and mental health treatment for certified WTC-related health conditions, and benefits counseling.
Annual Monitoring Exams
Responders and Certified-Eligible Survivors receive annual monitoring exams in the Program. Annual monitoring exams help track your health over time and allow participating doctors to evaluate any new symptoms to determine if any WTC-related health condition(s) or health condition medically associated to your WTC-related health condition(s) have developed.
Your annual monitoring exam may include:
- Blood tests;
- Medical history and mental health questionnaires;
- Physical examination;
- Urinalysis (urine test);
- Vital signs (blood pressure, pulse);
- Chest X-ray, if medically necessary;
- EKG (heart test), if medically necessary; and
- Spirometry/Pulmonary function testing (breathing test).
Program members should contact their Clinical Center of Excellence (CCE) or Nationwide Provider Network (NPN) participating provider directly to schedule an annual monitoring exam.
For NPN members: If you are scheduling an annual monitoring exam with a WTC Health Program Participating Provider that you have NOT visited before, please call the NPN call center at 800-416-2898 to schedule your appointment.
Cancer Diagnostic and Screening Services
The Program covers diagnostic services, such as blood work, imaging studies, biopsies, and specialty consults that your WTC Health Program Participating Provider needs to determine if you have a cancer that is covered by the Program.
The Program covers cancer screenings for all members (except FDNY family members) who meet the age and risk-factor guidelines set forth by the U.S. Preventive Services Task Force (USPSTF). The criteria for each type of screening are listed below. Cancer screenings for Screening-Eligible Survivors are only covered by the Program from the date of their initial health evaluation until six (6) months after.
Cancer screening benefits may change based on new guidelines issued by USPSTF. The Program may offer additional screening tests in the future based on the recommendations for cancer screenings by the USPSTF.
Breast Cancer Screening/Mammograms
Eligible members between the ages of 40 and 74 can receive a mammogram once every other year. The Program will also cover an additional mammogram if you receive a positive test result from a mammogram.
Cervical Cancer Screening
Most members between the ages of 21 and 65 are eligible to receive cervical cancer screening covered by the Program. Members between the ages of 21 and 65 may receive a Pap smear every three years. Members between the ages of 30 and 65 who wish to lengthen the screening interval may choose to receive a Pap smear in combination with HPV testing every five years.
Colon Cancer Screening
In most cases, the Program provides colon cancer screening for members between the ages of 45 and 75. The frequency and type of screenings can be determined by your Program provider.
Lung Cancer Screening
Lung cancer screening once a year is available to eligible members aged 50 to 80 years who have a 20 pack-year smoking history and currently smoke or have quit within the past 15 years. A pack year is the equivalent of smoking an average of 20 cigarettes, or one full pack, per day for a year.
Get more information on cancer screening in the Program on the Cancer Factsheets page.
Benefits Counseling
As a member of the Program, you may be eligible for benefits counseling from a case manager, social worker, benefits counselor, or other designated staff person at your CCE or the NPN. Benefits counselors can help identify benefits you may be eligible for and explain how you can apply for those benefits. Benefits counselors may also refer you to external benefits experts to help you access benefits available outside the Program, if needed.
As part of each visit, a CCE or NPN Program representative will work with you to complete a short benefits assessment questionnaire. The questionnaire helps the Program representative identify specific benefits for which you might be eligible. Then, you can work with your Program representative to learn more about those benefits, seek assistance applying for benefits, and/or be referred to a benefits expert for help.
Benefits Counseling: A service available to eligible members where a CCE or NPN WTC Health Program representative informs you about various benefits outside of the Program that you might be eligible for and assists you in applying for those benefits.
The WTC Health Program offers various types of benefits counseling, including:
Workers’ Compensation Counseling
Educates you about available workers’ compensation benefits, how to access them, and how they interact with WTC Health Program benefits.
More information on how Workers’ Compensation works with the Program.
September 11th Victim Compensation Fund (VCF) Assistance
Informs you about the September 11th Victim Compensation Fund (VCF), how to register and file a claim, and the relationship between the VCF and the WTC Health Program. Your WTC Health Program provider may conduct a VCF disability evaluation as needed and appropriate.
More information about the VCF is available.
External Work-Related and Disability Benefits Counseling
Helps you identify external (non-WTC Health Program) benefits you might be eligible for and educating you on how to access them.
Social Services Assistance
Helps you access needed social services, such as food, utility, housing, transportation, or other basic needs assistance.
Cancer Care Assistance
Helps members with cancer identify and access Program cancer-related benefits and services, as well as other resources needed for cancer treatment and/or in response to the financial, psychosocial, legal, or occupational impact of cancer on the member and the member’s family. Coordinates with oncology social workers as needed.
Non-Covered Conditions Assistance
Helps you identify appropriate care for medical and mental health conditions or medications not covered by the Program.
For benefits counseling assistance, contact your CCE or the NPN.
Covered Conditions and Certifications
In This Section:
Covered Conditions
WTC-Related Health Conditions Covered by the Program
The WTC Health Program provides medically necessary monitoring and treatment for certified WTC-related health conditions. The Program also covers medically associated health conditions, which are conditions that result from the treatment or progression of a certified condition.
More information on certification.
Medically Associated Health Condition: A health condition that results from treatment of a certified WTC-related health condition or results from the progression of a certified WTC-related health condition.
The following categories are outlined by the Zadroga Act and include examples of conditions within each category.
Please note: The list below is not exhaustive. It has been adapted from the List of WTC-Related Health Conditions in the Zadroga Act and the Program’s regulations for ease of use. The full list of covered conditions can be found on the Regulations page section 88.15.
 Acute Traumatic Injuries
Acute Traumatic Injuries
Acute traumatic injuries are characterized by physical damage to your body caused by hazards or adverse conditions. Examples include:
- Burn
- Complex sprain
- Eye injury
- Fracture
- Head trauma
- Tendon tear
 Airway and Digestive Disorders
Airway and Digestive Disorders
Airway and digestive disorders, also known as aerodigestive disorders, are a group of conditions that affect breathing airways, such as your sinuses or lungs, or upper digestive tract, such as your esophagus. Examples include:
- Asthma
- Chronic laryngitis
- Chronic nasopharyngitis
- Chronic respiratory disorder-fumes and vapors
- Chronic rhinosinusitis
- Gastroesophageal reflux disorder (GERD)
- Interstitial lung disease
- New-onset, and WTC-exacerbated chronic obstructive pulmonary disease (COPD)
- Reactive airway dysfunction syndrome (RADS)
- Sleep apnea
 Cancers
Cancers
Cancer may be defined as the uncontrolled growth and spread of cells. It may occur at any place in the body, and it makes it difficult for the body to function normally. Examples include:
- Blood and lymphoid tissue (including lymphoma, myeloma, and leukemia)
- Breast
- Childhood cancers
- Digestive system (including colon and rectum)
- Eye and orbit
- Ovary
- Head and neck (oropharynx and tonsil)
- Prostate
- Mesothelioma
- Rare cancers
- Respiratory system (including lung and bronchus)
- Skin (melanoma, non-melanoma and carcinoma in situ)
- Soft tissue
- Thyroid
- Urinary system (including kidney and bladder)
- Uterine (including endometrial)
 Mental Health Conditions
Mental Health Conditions
Mental health conditions include a wide range of conditions that affect your mood, thinking, and behavior. Examples include:
- Adjustment disorder
- Anxiety disorders
- Depression
- Dysthymic disorder
- Generalized anxiety disorder
- Major depressive disorder
- Panic disorder
- Post-traumatic stress disorder (PTSD)
- Substance use disorder
 Musculoskeletal Disorders (for WTC Responders ONLY)
Musculoskeletal Disorders (for WTC Responders ONLY)
Musculoskeletal disorders are chronic or recurring disorders of the musculoskeletal system caused by heavy lifting or repetitive strain on the joints. Examples include:
- Carpel tunnel syndrome (CTS)
- Other musculoskeletal disorders
For more information on covered conditions, visit the Covered Conditions page.
How to Add a Condition to the List of WTC-Related Health Conditions
The Program only provides treatment for the specific conditions on the List of WTC-Related Health Conditions established by the Zadroga Act and Program regulations. However, the Administrator may add new health conditions to the List through the rulemaking process.
For example, a condition may be added if the Administrator finds there is enough scientific evidence to link a health condition to 9/11 exposures. This might happen if research shows that a health condition is more likely to occur in individuals with 9/11 exposure than in individuals without 9/11 exposure.
If you believe you have a condition that is the result of your 9/11 exposure but is not included on the List, you may petition the Administrator to add the health condition. To be considered, a petition must be sent in writing to the Administrator, and include the following:
- An explicit statement of an intent to petition the Administrator to add a health condition to the List of WTC-Related Health Conditions;
- Name, contact information, and signature of the interested party submitting the petition;
- Name and description of the health conditions(s) to be added; and
- Reasons for adding the health conditions(s), including the medical basis for the association between 9/11 exposure and the health condition(s) to be added.
The petition form can be found on the Petitions page. For more information on how the Program considers petitions to add health conditions to the List of WTC-Related Health Conditions, you may review the applicable three policies and procedures on the Policies page.
These include:
- Policy and Procedures for Handling Submissions and Petitions to Add a Health Condition to the List of WTC-Related Health Conditions;
- Policy and Procedures for Adding Non-Cancer Conditions to the List of WTC-Related Health Conditions; and
- Policy and Procedures for Adding Types of Cancer to the List of WTC-Related Health Conditions.
Certification of Covered Conditions
The WTC Health Program will pay for medically necessary treatment of certified conditions. Your condition can be certified by the Program if:
- Your health condition is included on the List of WTC-Related Health Conditions;
- Your health condition and 9/11 exposures meet WTC Health Program policies and criteria for certification, such as maximum time intervals, minimum latency requirements, and any additional requirements; and
- Using the 9/11 exposure assessment, your WTC Health Program provider determines your 9/11 exposures are substantially likely to have been a significant factor in aggravating, contributing to, or causing the health condition.
Certified: A certified WTC-related health condition (or medically associated health condition) is one that has been approved for coverage by the Program based on the approval of a certification request for that condition.
If your WTC Health Program Participating Provider determines that you have a health condition that meets all criteria above, your CCE or the NPN will complete paperwork signed by your Program provider and submit the Certification Request that the Program certify your health condition.
The Program will review the Certification Request submitted by your CCE or the NPN to determine if your health condition can be certified. The Program will certify your health condition if it finds that your health condition and exposure meet the above criteria.
The Program will notify you in writing and will also communicate the decision to your CCE or the NPN. You can be certified for more than one condition.
In some rare circumstances, a certified condition may be decertified.
For more information about decertification, see the Decertification section.
Certification Request: Paperwork completed by your WTC Health Program Participating Provider to request certification of your WTC-related health conditions by the Program. It includes information about you, your health condition(s), and your 9/11 work and exposures.
Your WTC Health Program Participating Provider may only submit a request for certification to the Program when all criteria listed above are met. Requests for certification that do not meet these criteria will not be sent to the Program for review and will not be eligible for appeal. In some cases, a secondary medical review may be available.
Learn more about secondary medical reviews.
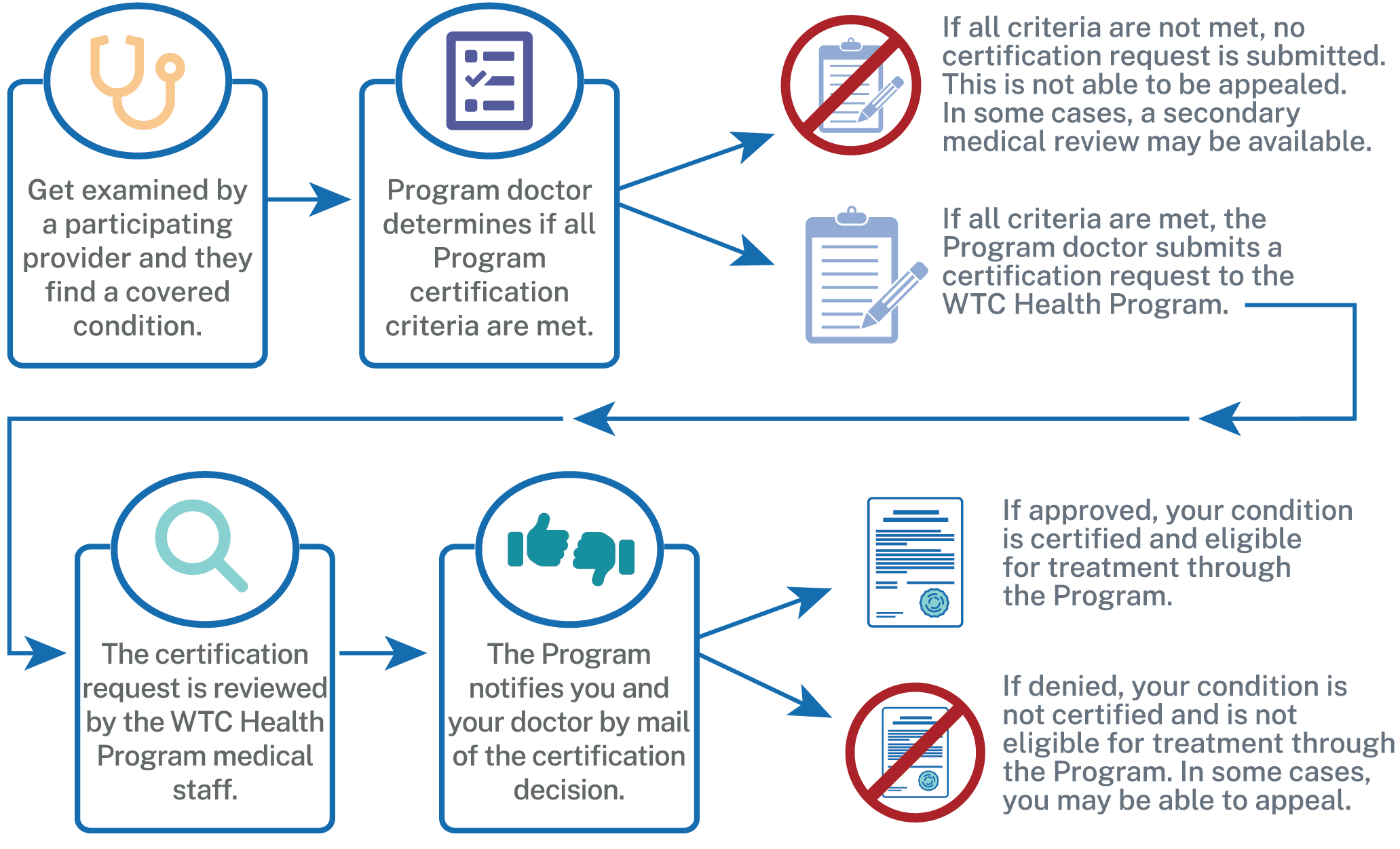
Certification Process
Certification of Medically Associated Health Conditions
In addition to the health conditions on the List of WTC-Related Health Conditions, the Program may also certify health conditions that result from either the treatment of your certified WTC-related health condition or the progression of your certified WTC-related health condition. These conditions are called medically associated health condition(s).
Your medically associated health condition will be eligible for Program treatment if the Program finds and certifies that it is the direct result of the treatment or progression of your certified WTC-related health condition and the relationship between the two conditions is supported in the scientific literature.
For the Program to cover the treatment for a medically associated health condition, your WTC Health Program Participating Provider must explain how the health condition is a direct result from either treatment or progression of the underlying certified WTC-related health condition. The Program will review your participating provider’s explanation and determine whether the relationship linking the medically associated health condition with your certified WTC-related health condition is appropriate for coverage.
Additional Certification Requirements
Maximum Time Intervals for Aerodigestive Disorders
For an aerodigestive disorder, an additional requirement known as maximum time interval must be met for the health condition to be certified by the Program. Your symptoms of an aerodigestive disorder must have started during a specific time frame for it to be certified by the Program.
Maximum time interval: The maximum amount of time that could have gone by between the last date of your 9/11 exposures and the initial onset of symptoms of your aerodigestive disorder.
Aerodigestive disorders are divided into six categories with a maximum time interval for each category (see table below). The time intervals are based on the best available published science and the Program’s clinical expertise.
If you have questions about maximum time interval for your aerodigestive disorder, speak to your Program provider.
The six categories of aerodigestive disorders and the maximum time interval for each are as follows:
| Category | Types of Diseases | Conditions Include | Maximum Time Interval |
|---|---|---|---|
| 1 | Chronic Obstructive Pulmonary Disease (COPD) | COPD (both WTC-exacerbated and new onset) | No maximum time interval |
| 2 | Other Obstructive Airways Diseases (does not include COPD-see above) |
|
5 years |
| 3 | Upper Respiratory Diseases |
|
5 years |
| 4 | Interstitial Lung Diseases | All types of interstitial lung diseases | No maximum time interval |
| 5 | Co-occurring GERD | GERD in combination with a condition in Category 1, 2, 3 or 4 | 5 years |
| 6 | Isolated GERD | GERD with no other diagnosed WTC-related health condition | 1 year |
Cancer Latency
Minimum latency requirements must be met for your cancer to be certified by the Program. In most cases, cancer does not develop until some time has passed after exposure to a cancer-causing agent.
Latency is the amount of time that has passed between your initial 9/11 exposures and the date you were first diagnosed with cancer. Minimum latency requirements have been set based on well-established scientific literature (see table below).
The following table outlines the minimum latency requirements for cancers covered by the Program:
| Type of Cancer | Minimum Latency Requirement |
|---|---|
| Blood Cancer | 0.4 years (146 days) |
| Childhood cancers | 1 year |
| Thyroid cancer | 2.5 years |
| Mesothelioma | 11 years |
| Other types of covered solid cancers | 4 years |
The WTC Health Program will not consider any exceptions to the maximum time interval or minimum latency period. Members may not request a secondary medical review when their conditions do not meet these requirements.
If you have questions about maximum time interval or latency requirements for certification of your cancer, speak to your Program doctor. For more information about these requirements, visit the Policies page.
Acute Traumatic Injury and Musculoskeletal Disorder Criteria
For your Acute Traumatic Injury (ATI) or Musculoskeletal Disorder (MSD) to be certified by the Program, the injury must be directly related to your 9/11 exposures and activities.
The Zadroga Act only allows coverage of MSDs for WTC Responders with a chronic or recurrent disorder of the musculoskeletal system caused by heavy lifting or repetitive strain during rescue or recovery efforts in the New York City Disaster Area. Survivors and Pentagon and Shanksville, PA Responders cannot be certified for an MSD.
However, all categories of Program members (except FDNY family members) can be certified for an ATI. For both ATIs and MSDs, there must be evidence that you received medical treatment for the ATI or MSD injury between September 11, 2001, and September 11, 2003.
If you have questions about ATI or MSD criteria, speak to your Program provider.
Secondary Medical Review
If your WTC Health Program doctor declines to submit a certification request for your health condition to the Program, you may be eligible for a secondary medical review. A secondary medical review is a review of your case by the CCE/NPN Clinical Director or a designee. This designee may be a WTC Health Program doctor at another CCE.
Examples of when you may request a secondary medical review include, but are not limited to, when you disagree with the CCE/NPN doctor regarding the characterization of your exposure, diagnosis, onset of symptoms dates, or intensity of exposure in relation to aggravating, contributing to, or causing your health condition.
Your CCE or the NPN will advise you if you may be eligible for a secondary medical review. To initiate the process, you must send a letter to the CCE/NPN Clinical Director or designee which clearly indicates your request to obtain a secondary medical review.
You may not request a secondary medical review when your health condition does not meet Program certification criteria.
Decertification
The Program may decertify your condition in the following circumstances:
- The Program finds that your 9/11 exposures do not meet the Program requirements;
- The Program finds that your certified health condition was certified in error or mistakenly considered to have been aggravated, contributed to, or caused by exposure to airborne toxins, any other hazard, or any other adverse condition resulting from the September 11, 2001 attacks; or
- The Program finds that your health condition was mistakenly found to be medically associated with a WTC-related health condition.
The Program will notify you in writing if the certification has been withdrawn and your health condition has been decertified. The letter will explain why your condition was decertified and provide you with information about how to appeal the decision.
For more information on how to appeal a decertification, see the Appeals section.
Treatment in the WTC Health Program
In This Section:
The World Trade Center (WTC) Health Program pays for all medically necessary treatment for your certified WTC-related health condition(s), including medically associated health conditions, as long as the treatment aligns with Program policies and is provided by a WTC Health Program provider.
Medically necessary treatment: Medical services that are appropriate to manage, improve, or cure a certified WTC-related or medically associated health condition.
WTC Health Program Providers
To provide WTC-related care to members, the Program’s vendors—such as the Clinical Centers of Excellence (CCEs) and the Nationwide Provider Network (NPN)—contract or partner with health provider networks. Providers in these networks, known as Network Providers, are not always automatically notified about every program the health network covers, including programs like the WTC Health Program. Individual providers in these large networks may not have been educated about the Program, or agreed to provide care to WTC Health Program members.
Network Provider: A provider that is part of a network either contracted with the WTC Health Program or one of the Program’s vendors.
The World Trade Center (WTC) Health Program covers care provided to members for certified WTC-related health conditions received from providers who:
- Are part of a health network contracted with the Program or one of the Program's vendors, and
- Have agreed to provide care to WTC Health Program members.
These are known as WTC Health Program Participating Providers, and are sometimes referred to as Program providers or participating providers.
Network Providers who have not agreed to, or in some cases declined to, treat WTC Health Program members are known as WTC Health Program Non-Participating Providers.
Providers who are not contracted with the Program or one of the Program’s vendors are known as Out-of-Network Providers.
It is important that members visit a WTC Health Program Participating Provider for their WTC-related care. To do this, members who receive their WTC-related care through a CCE will make an appointment through that CCE. Members in the NPN will call MCA-Sedgwick, who administers the NPN, at 1-800-416-2898, 8am to 8pm ET, Monday through Friday, to schedule their appointments.
This allows your clinic or the NPN to connect members with providers who are:
- Appropriate for the member’s certified WTC-related health condition,
- Approved by the Program, and
- Educated about and have agreed to the Program’s unique requirements.
For NPN members: MCA-Sedgwick adds providers to the NPN regularly. Members can nominate providers on the MCA-Sedgwick Nominate a Provider page to join the NPN, and a representative from MCA-Sedgwick will reach out to that provider. This process can take several weeks or months and is not guaranteed.
Medically Necessary Treatment and Authorizations
The Program only provides treatment for your certified WTC-related health condition or medically associated health condition.
All Program treatment services must:
- Be authorized by your WTC Health Program Participating Provider (and in some cases the CCE or NPN Clinical Director) and the Program.
- Follow Program guidelines and be medically necessary to treat your certified WTC-related health condition.
You must receive treatment from a WTC Health Program Participating Provider for the Program to cover the cost. There are no exceptions. The Program also does not cover the cost for care received prior to your condition being certified.
To access treatment services for your certified WTC-related or medically associated health condition(s), you will need your current WTC Health Program member identification (ID) number.
Your Program Member ID number—also sometimes called your 911 number since all member IDs start with ‘911’—is included on:
- Your Program welcome letter received when you were first enrolled,
- Your WTC-related health condition certification letter from the Program,
- On your WTC Health Program Prescription ID card (members with a certified condition only), and/or
- Your NPN Member ID card (NPN members only).
Your participating provider will help coordinate care of your certified WTC-related health condition(s) or associated medical conditions only. Members should always maintain their own primary care provider and primary health insurance for health conditions not covered in the Program.
Find more information on the health insurance requirement for Program members.
Referrals
If your Program provider thinks that you need to see a specialist to diagnose or treat a certified WTC-related health condition, they will refer you to a specialist affiliated with the Program.
For example, if you have asthma, your Program provider might refer you to a pulmonologist who is affiliated with the Program. Your Program provider and the specialist will communicate about medically necessary treatment for your certified WTC-related health condition(s).
You must be referred to a specialist by your CCE or the NPN. This ensures that they are a WTC Health Program Participating Provider and the service can be covered. You should coordinate with your referring NPN provider or CCE to schedule your first appointment.
Authorizations
Most WTC-related treatment services require some level of authorization from the WTC Health Program and/or the Program provider. This ensures that the treatment is medically necessary and eligible for coverage within the Program’s guidelines.
Level 1 Authorization
Your WTC Health Program Participating Provider authorizes your treatment to ensure it is medically necessary for your condition and meets Program policies. This is called a Level 1 Authorization. This level of authorization does not require permission or review by the WTC Health Program.
Level 2 and Level 3 Prior Authorizations
In some cases, your participating provider needs additional authorization from your CCE or NPN Clinical Director (Level 2 Prior Authorization).
Other times both your CCE or NPN Clinical Director and the WTC Health Program administration need to give your participating provider authorization (Level 3 Prior Authorization) before a medically necessary treatment service can be covered by the Program.
If you need treatment services that require a Level 2 or Level 3 Prior Authorization, your Program provider will request the authorization for you. You do not need to request authorization yourself.
Level 2 and Level 3 Prior Authorizations must be obtained before you receive the medical treatment or service. You may also hear it referred to as just ‘prior authorization’ by medical staff or the Program.
Medical Treatment Guidelines
The following treatments are examples of medically necessary treatments you may receive for your certified WTC-related health condition(s). Depending on your situation and the type of treatment, different treatments may require different levels of prior authorizations. Talk with your WTC Health Program Participating Provider to discuss your options.
The WTC Health Program reserves the right not to cover any of the following services at any time if they are determined not to be medically necessary or do not meet Program policies or coverage guidelines.
Medical guidelines may change based on the latest medical research and recommendations. The Program’s current medical policies are available on the Policies page and Administrative Manual.
Acupuncture Services
Acupuncture services available for coverage under the WTC Health Program include traditional acupuncture with needles. They also include other acupuncture services involving heat, pressure, friction, suction, and electromagnetic impulses.
Members with the following health conditions may be eligible for acupuncture services:
- A certified WTC-related cancer when authorized by a participating provider,
- Cancer medically associated with a certified WTC-related health condition, or
-
Chronic pain resulting from:
- Certified WTC-related acute traumatic injury,
- Certified WTC-related muscular skeletal disorder, or
- A condition medically associated with a certified WTC-related acute traumatic injury or muscular skeletal disorder.
Cancer Treatment Services
The Program covers medically necessary cancer treatment for your certified WTC-related cancer. This includes doctor visits, medications, cancer therapies, surgeries, and other services.
The Program will cover these services if both of the following conditions are met:
- Your cancer specialist is a participating provider who has been approved to provide services to Program members; and
- The cancer treatment you receive follows the National Comprehensive Cancer Network (NCCN) guidelines on treatment for your type of cancer.
Cancer care is coordinated by your CCE or the NPN.
Some cancer treatment service may require a prior authorization. Your participating provider will be able to determine this.
Learn more about NCCN guidelines on the NCCN Guidelines for Patients page .
COVID-19
The Program covers limited COVID-19 testing and treatment services that are medically necessary to deal with certain certified WTC-related condition or medically associated health condition.
Treatment for these services is covered when certain criteria are met, including that the member was eligible for COVID-19 testing, the treatment is authorized by the Program, and the treatment is not experimental.
Dental Services
The Program covers limited dental services with specific eligibility criteria. Limited dental services may be covered for members before cancer treatment or an organ transplant. Members with certified head and neck cancer may receive additional dental treatment to fix new dental issues caused by cancer treatment.
Before treatment for WTC-related cancer or an organ transplant, you can receive through the Program:
- A once-per-lifetime dental checkup. This checkup might include a cleaning and x-rays.
- Based on what the checkup finds, you may get medically necessary dental care like deep cleaning, fillings, or tooth removal.
Dental problems because of cancer treatment for head and neck cancer may be covered as part of your Program medical benefits.
Some dental services may be authorized by a WTC Health Program Participating Provider, while other services may need authorization by the Program. In rare situations, medically necessary dental care related to other certified WTC-related health conditions may be considered on a limited case-by-case basis.
Durable Medical Equipment (DME)
Durable Medical Equipment (DME) is medical equipment used in the home, such as hospital beds, wheelchairs, nebulizers, CPAP machines, and other types of equipment.
If DME is medically necessary to treat your certified WTC-related health condition(s), then the rental or purchase of DME is covered by the Program and supplied by a preferred Program provider whenever possible.
Family Therapy and/or Marital Counseling
In certain circumstances, psychotherapy services for a member’s family may be covered as part of the treatment of the member’s certified WTC-related health condition. Marital counseling for a member and their spouse may also be covered in certain circumstances. Talk to your Program provider or case manager.
Home Health Services
Home health services are a wide range of health care services provided in a member’s home to treat a certified WTC-related health condition(s).
Medically necessary home health services may be covered for a limited period for members who are homebound and require these services. Home health services must be authorized by your CCE or the NPN Clinical Director, or by the Program.
Hospice Care
The Program may cover hospice care when treatment for your certified WTC-related health condition is no longer controlling the illness and the member has a life expectancy of six months or less if the illness runs its normal course. Hospice provides medical, psychological, and spiritual support during end-of-life care.
Hospice care may be continued beyond six months if your CCE or the NPN Clinical Director confirms care is needed for a longer period of time. Hospice services may be provided in the member’s home or a hospice facility when it is recommended by your Program provider.
Inpatient Care Services
The Program covers inpatient treatment and services if those services are medically necessary to treat your certified WTC-related health condition(s).
Inpatient care covers hospital services, including semi-private rooms, meals, general nursing, and prescription drugs as part of your inpatient treatment, and other hospital services and supplies. This includes the care you get in acute care hospitals, critical access hospitals, and mental health care in a hospital setting.
For inpatient services to be covered, your CCE or the NPN Clinical Director must authorize the services before you are hospitalized or admitted to an inpatient facility.
It is important to work closely with your CCE or NPN if inpatient care is needed so that the services can be appropriately authorized by your CCE, the NPN Clinical Director, or the Program.
Inpatient Rehabilitation Services
The Program may cover inpatient rehabilitation services for members with intensive physical rehabilitation needs due to their certified WTC-related health condition. Inpatient rehabilitation services may be covered when the member requires a team approach to care that cannot be provided in an outpatient setting. These services must be authorized by the Program.
Long-Term Care Hospital
A long-term care hospital provides care to members with medically complex problems that require an extended stay.
For a stay at a long-term care hospital to be covered, the Program must confirm these services are medically necessary for your certified WTC-related health condition(s) and authorize your treatment before a long-term stay.
Mental Health Services
The Program covers mental health treatment services for certified WTC-related mental health conditions.
Mental health treatment services include:
- Services of psychiatrists and other mental health providers, such as psychologists, social workers, counselors
- Services such as prescription drugs, counseling/psychotherapy, hospitalization, and other services in special circumstances
The Program does not cover residential treatment for mental health care.
Mental Health Service Providers
At some CCEs, the mental health treatment services are provided in-house by a mental health provider employed directly by the CCE. At other CCEs, these services are provided by affiliated external mental health providers who are part of the CCE’s network of credentialed health care providers.
The NPN includes credentialed mental health care providers as part of their provider network. As with physical health care, all mental health providers must be WTC Health Program Participating Providers to be covered by the Program.
FDNY Family Members’ Mental Health Treatment
Family members of deceased FDNY personnel may receive mental health treatment under the following conditions:
- You are a surviving immediate family member of an FDNY Responder who was killed at the WTC site on September 11, 2001; and
- You received treatment for a mental health condition included on the List of WTC-Related Health Conditions on or before September 1, 2008; and
- You are enrolled in the Program and your mental health condition has been certified by the Program.
Non-Emergency General Transportation (NPN only)
Non-emergency general transportation for treatment appointments is only available to NPN members who live a certain distance away from a Program provider and there are no other options for treatment. The Program or the NPN Medical Director must authorize all non-emergency transportation services before using the service.
Non-Emergency Medical Transportation
Non-emergency medical transportation, such as via an ambulance or ambulette, may be available if necessary. You must be receiving medically necessary care for a certified WTC-related health condition. The Program or your CCE or the NPN Medical Director must authorize all non-emergency transportation services before using the service.
Organ Transplants
The Program may cover organ transplants to treat a certified WTC-related health condition if specific circumstances are met. Talk to your Program provider or NPN case manager to learn more about organ transplant coverage.
Outpatient Rehabilitation Services
The Program may cover physical rehabilitative care for a certified WTC-related health condition in a comprehensive outpatient rehabilitation facility. This facility provides outpatient services such as physical therapy, physician services, and social or psychological services.
Your CCE or NPN Clinical Director must review your rehabilitative care plan and authorize your treatment.
Skilled Nursing Facility Services
The Program may cover medically necessary services in a skilled nursing facility that provides around-the-clock nursing or rehabilitation services after a member has been hospitalized for a certified WTC-related health condition(s).
Multiple criteria must be met for these services to be covered, and the services must be authorized by your CCE or the NPN Clinical Director.
Smoking Cessation Therapy
The WTC Health Program provides smoking cessation therapy for:
- Members with at least one certified WTC-related health condition; or
- Eligible members who are current smokers and are referred based on the results of lung cancer screening.
Examples of smoking cessation therapy include non-nicotine medications that reduce cravings and nicotine replacement products such as patches, gum, and lozenges.
Substance Use Disorder Treatment Programs
In certain circumstances, the Program may cover substance use disorder treatment. This may include acute hospitalization services and specialty outpatient treatment to treat certified WTC-related mental health and substance use disorders. Residential treatment for substance use disorder is not covered by the Program. To learn more about available treatment for substance use disorder, speak to your WTC Health Program provider.
Vaccine Coverage
The Program covers certain vaccines for eligible enrolled members (except for FDNY family members). Members may be eligible for vaccines recommended by the CDC Advisory Committee on Immunization Practices (ACIP) when the member meets requirements regarding age, timing of doses, and specific precautions.
Medical Emergencies
If there is a medical emergency, call 911 or go to the nearest emergency room.
The Program defines a medical emergency as a serious medical or mental health condition for which immediate treatment is necessary (it would result in a threat to life, limb or sight, or when a person is at immediate risk to self or others).
Emergency Care Services
The Program may cover emergency care services that are necessary to prevent death or serious impairment to the member as a result of a certified WTC-related health condition(s).
The Program does not cover non-emergency visits to the emergency department. Members should follow up with their CCE or NPN for non-emergency care. If something is not deemed an emergency, or is determined to not be related to your certified WTC-related health condition, the Program will not cover the emergency care services.
You do not have to call your CCE or the NPN before getting emergency care, however you should notify them within 24 hours of receiving such care. This helps coordinate your ongoing care and ensures proper authorization.
Urgent Care (After Hours)
Urgent care services are for medically necessary treatment of an urgent medical condition which is not considered to be an emergency. However, it is an illness or injury that must be addressed within 12 hours to avoid the likely onset of a medical emergency.
The Program covers certain types of urgent care visits for your certified WTC-related health condition(s). The urgent care facility should notify your CCE or the NPN of your visit as soon as possible.
Visit the Administrative Manual for more information on urgent care and the Program.
As a Program member, you can use emergency room services or urgent care for your certified WTC-related health condition(s) in your local area or while traveling. However, the Program only covers emergency care and urgent care services that are related to your certified WTC-related health condition(s).
Case Management
The goal of case management is to share resources that allow you to return to your maximum health and well-being.
Case Management: A collaborative process that facilitates medical care and treatment plans to meet individual healthcare needs, maximize the care goals, and improve the continuity and quality of care.
Case managers can help you understand your available care options while developing a plan of care specific to your individual needs. Case management may assist with:
- Identifying providers,
- Locating healthcare facilities,
- Addressing pharmacy concerns,
- Assisting with billing inquiries, and
- Obtaining authorizations for specialty care.
Depending on your situation, you may be assigned a case manager or case management team for extra help navigating your care. A case management team is made up of the individuals involved in a member’s care. This could include doctors, nurse practitioners, nurses, social workers, care coordinators, and CCE/NPN support staff. This person or team will coordinate with you, your health care providers, and other resources as appropriate.
It is very important that you work closely with the case management team because they will assist in coordinating your care and should be your first level of contact if an issue arises.
For CCE members
If you have questions or concerns about your care and case management, contact your CCE directly.
For NPN members
If you have any questions about case management in the NPN, call 1-800-416-2898.
Pharmacy Benefits
In This Section:
Prescriptions
Prescription Drugs
The Program covers prescription drugs for eligible members. Your WTC Health Program Participating Provider will prescribe medication(s) for you using the Program’s formulary. The formulary is a list of prescription drugs covered by the Program. The CCEs and the NPN are given updated lists periodically.
Prior Authorizations
Some prescriptions may need prior authorizations to be covered by the Program. Your WTC Health Program Participating Provider should complete and submit these for you. In some cases, your participating provider may need to submit a second prior authorization to your primary insurance as well.
If the drug is not authorized for coverage by the Program but you would like to still use it, you will have to use a different form of payment such as your primary insurance or pay out-of-pocket for the drug.
Generic Drugs
The Program requires that WTC-related prescriptions for medications that come in generic form must be filled using the generic medication. The Program requires generic drugs because the cost of a generic drug is significantly lower than brand name drugs.
Generic drugs contain the same active ingredients as brand name drugs, and are the same in dosage, safety, stability, strength, purity, quality, and administration.
For more information on generic drugs, talk to your CCE or NPN provider.
Preferred Medications
For some drugs, there are no approved generics. In these cases, the Program reviews the available medications to compare effectiveness and cost. The Program then decides to cover a specific medication based on whether the drug provides reasonable treatment at the best cost.
This practice is known as preferred medications and is common with government health programs and private insurance companies.
Filling Prescriptions
Your WTC Health Program doctor or specialist will write the prescription for your certified WTC-related health condition(s). Filling prescriptions may look different depending on if you are a Responder or a Survivor.
| Pharmacy Options | Responder | Survivor |
|---|---|---|
| Retail |
Up to a 90-day supply at Walgreens/ Duane Reade Pharmacies Up to a 30-day supply at retail pharmacies in an Express Scripts network |
Up to a 90-day supply at retail pharmacies that are in both an Express Scripts network AND your primary insurance network |
| Home Delivery | 90-day supply through Express Scripts Home Delivery only | 90-day supply through a home delivery pharmacy that is in both an Express Scripts network AND your primary insurance network |
| Specialty | Up to a 30-day supply through Accredo Specialty Pharmacy only | Up to a 30-day supply at any pharmacy that is in both an Express Scripts network AND your primary insurance network |
Specialty Medicines for Responders
Responders who have specialty medications can get these prescriptions covered and filled through Accredo Specialty Pharmacy only. Other pharmacies that provide specialty medications but are not in the Express Scripts network will not be covered by the Program.
Responders with specialty medications can visit the Accredo website or call 1-855-540-1780 with any questions, to fill prescriptions, access plan information, and track online orders.
Prescriptions and Coordination of Benefits (Survivors Only)
For Survivors, Coordination of Benefits is required for the WTC Health Program to cover WTC-related prescriptions, including specialty medications, at no cost to you. Survivors must make sure that the pharmacy they are using is in-network for both the Survivor’s primary health insurance and the Express Scripts network.
How Survivors Fill a WTC-Related Prescription
Step 1: You may fill your prescriptions at any in-network retail pharmacy or through certain home delivery pharmacies in the Express Scripts network as long as the retail pharmacy and home delivery pharmacy are also in network for your primary health insurance’s prescription coverage plan.
Step 2: You must make sure any pharmacy you use has your most up-to-date primary health insurance information as well as your WTC Health Program Prescription ID card. For prescriptions delivered through home delivery, please confirm your mailing address information as well.
Step 3: Tell the pharmacy that the WTC Health Program is the payor of last resort.
Step 4: The pharmacy will bill your primary health insurance first, and then bill any remaining costs to the WTC Health Program. If the pharmacy tries to bill the Program directly, the claim will be rejected with a message for them to bill your primary insurance first.
Please note: Your primary health insurance may have certain requirements that need to be met, such as prior authorizations. Such requirements must be processed to permit your primary health insurance to pay before the WTC Health Program may pay the remaining the amount.
Step 5: Call your pharmacy before going to pick up your prescription to ensure the coordination of benefits process has been followed.
Problem filling a prescription as a Survivor?
If the pharmacy is unable to fill your prescription, it may be due to a problem billing the prescription to your primary health insurance. You or the pharmacy should contact your primary insurance company to resolve the issue.
If the pharmacy is having difficulty processing the WTC Health Program as payor of last resort, they should contact Express Scripts at 1-800-935-7179.
If you pay for a prescription out-of-pocket, before resolving any issues with Express Scripts, the WTC Health Program cannot guarantee reimbursement and does not have the legal authority to reimburse you directly. If you have paid out-of-pocket for a prescription but believe the prescription(s) should be covered by the WTC Health Program, contact Express Scripts for a Claim Reimbursement Form.
More information on coordination of benefits.
For more information, visit the Pharmacy Benefits page.
Pharmacy Benefits Manager
Pharmacy benefits in the World Trade Center (WTC) Health Program are administered by a company known as a Pharmacy Benefit Manager. Express Scripts is the Program’s Pharmacy Benefit Manager.
Pharmacy Benefit Manager: A company that oversees pharmacy benefits on behalf of health programs, contracts with pharmacies, and processes and pays prescription claims. A Pharmacy Benefit Manager may also be referred to as a ‘PBM.’
More about Express Scripts
Express Scripts has a large national retail pharmacy network including major retail pharmacy chains and independent pharmacies. Express Scripts also provides home delivery and specialty pharmacy options for members with a certified WTC-related health condition.
Prescription ID Card
Members with certified WTC-related health conditions will receive a WTC Health Program Prescription ID card provided by Express Scripts. If you are certified and do not receive this ID card, contact Express Scripts directly.
Remember! You will only receive a WTC Health Program Prescription ID card if you have a certified WTC-related health condition.
Express Scripts Member Portal
Members eligible for pharmacy benefits can register online to access the Express Scripts Member Portal. The Express Scripts Member Portal allows you to find your local in-network pharmacy and track your home delivery prescription.
Members can create a new pharmacy benefit account on the Express Scripts website or through the Express Scripts Mobile App available in your app store.
How to contact Express Scripts
All questions related to pharmacy benefits and prescription fills should be directed to Express Scripts. You can reach Express Scripts by phone or online.
Express Scripts Member Service: 1-800-935-7179
Program Policies, Privacy, and Support
In This Section:
- Designated Representatives
- Appeals
-
HIPAA Privacy Practices in the WTC Health Program
- How Do We Use and Share Your Personal Health Information?
- How Else Do We Use and Share Your Personal Health Information?
- What Are Your Rights When It Comes To Your Personal Health Information?
- When Do We Require Your Written Permission?
- What Are the Responsibilities of the WTC Health Program?
- How Can You Contact the WTC Health Program?
- How Can You File a Complaint?
- Complaint Procedure
- Other September 11th Programs
Designated Representatives
A designated representative is someone you appoint and authorize to act on your behalf and represent your administrative interests in the World Trade Center (WTC) Health Program. However, this person may not make medical care (e.g., treatment) decisions for you.
If you need to appoint someone to make decisions regarding your medical care, this is done directly with your CCE or the NPN. Talk to your CCE or the NPN about their process.
When you designate a representative, you must also authorize the WTC Health Program to disclose your personal health information to the representative under the Health Insurance Portability and Accountability Act of 1996 (HIPAA).
Once you designate a representative and complete a HIPAA authorization for them, the designated representative may then:
- Serve as your representative in all matters pertaining to your membership in the WTC Health Program, including enrollment, certification, and any other administrative issues; and
- Receive and/or provide information pertaining to your membership and participation in the WTC Health Program, including copies of factual and medical evidence contained in your records for the Program.
Please note: Any requirement of the WTC Health Program to notify you in writing is fully satisfied if sent to the designated representative.
You may only have one designated representative at a time. You can change your designated representative at any time.
Who Can be a Designated Representative
A designated representative in the WTC Health Program can be someone such as a family member, friend, attorney, or advocate, unless that individual’s service as a representative would violate any applicable provision of law.
Only a single individual may serve as your designated representative. An entire organization or group of people—such as multiple family members or a law firm —is not permitted to be a designated representative.
If a member is a minor, a parent or guardian may act on the member’s behalf. If a member is a mentally incompetent adult, the person authorized under state or other applicable law to act on the member’s behalf may act as their designated representative in the Program.
The WTC Health Program does not generally accept Powers of Attorney for administrative matters. This includes signing and/or submitting an application on an individual’s behalf, signing Designated Representative forms on an individual’s behalf, and otherwise interacting with the WTC Health Program on an individual’s behalf.
How to Designate a Representative
To designate a representative, you must notify the Program in writing using the Designated Representative forms available on the Designated Representative page.
Your Clinical Center of Excellence (CCE) or the Nationwide Provider Network (NPN) may have additional requirements and forms for medical records to be released to your designated representative.
Appeals
An appeal in the WTC Health Program is a formal process requesting reconsideration of certain Program decisions.
What Can Be Appealed
You or your designated representative may appeal the following three types of decisions made by the Program:
- Enrollment denial – includes denial of enrollment in the Program or disenrollment.
- Certification denial – includes denial of certification of a health condition as a WTC-related health condition, denial of certification of a health condition as medically associated health condition, or decertification of a WTC-related health condition.
- Treatment denial - includes denial of treatment authorization for a certified WTC-related health condition based on a finding that the treatment is not medically necessary.
An appeal can be submitted when you believe the Program incorrectly determined you don’t meet Program criteria as described above. For example, an appeal request could argue that the Program incorrectly determined the number of hours the individual worked or volunteered during a covered time period.
What Cannot Be Appealed
Not all appeal requests can be considered. An appeal is invalid if it challenges:
- Enrollment criteria established by the James Zadroga 9/11 Health and Compensation Act of 2010 (Zadroga Act) or WTC Health Program regulations;
- Certification requirements established by the Zadroga Act and WTC Health Program regulations;
- A determination by a WTC Health Program Participating Provider that a condition does not meet the criteria for certification;
- A WTC Health Program policy that has been established by the Administrator and is applicable to all Program applicants and/or members;
- The exclusion or absence of a health condition from the List of WTC-Related Health Conditions (List);
Criteria and requirements in the Zadroga Act are established by law and may only be changed by the U.S. Congress amending the Act.
Criteria within the WTC Health Program’s regulations are established through rulemaking and may only be changed by the Program revising the regulations.
Health conditions may only be added to the List through a petition process. See the How to Add a Condition section of this handbook for more information.
More information on what may and may not be appealed is available on the Appeals page.
Valid Appeals in a Nutshell
You may appeal:
- The Program’s application of enrollment, certification, or treatment authorization criteria to your individual enrollment, certification, or treatment decision
You may not appeal:
- Zadroga Act criteria or Program regulations
- Program policies applicable to all members
- WTC Health Program Participating Provider determination that a condition does not meet certification criteria
- A condition not being on the list of WTC-Related Health Conditions
Appeals that are determined to be invalid are not reviewed. An appeal that is invalid is not a denied appeal.
Requesting an Appeal
To request an appeal, you must mail or fax a written letter requesting an appeal to the Program’s appeals coordinator postmarked within 120 calendar days from the date of your denial, disenrollment, or decertification letter from the Administrator.
Your appeal letter must:
- Be made in writing and signed;
- Identify the name, address, and contact information of the member and designated representative (if applicable);
- Describe the decision being appealed and state the reasons why you believe the decision was incorrect and should be reversed; and
- Provide a basis for the appeal that is sufficiently detailed and supported by information to permit a review of the appeal. An appeal request may include relevant new information not previously considered by the WTC Health Program.
The description may include:
- Scientific or medical information correcting factual errors that may have been submitted to the Program by the CCE or NPN;
- Information showing that the Program did not correctly follow or apply relevant Program policies or procedures;
- Any information showing that the Program’s decision was not reasonable given the facts of the case; and/or
- A request to designate a representative.
| By Mail | By Fax |
|---|---|
|
Appeals Coordinator WTC Health Program P.O. Box 7000 Rensselaer, NY 12144 |
1-877-646-5308 |
|
If using a shipping service that does not permit a P.O. Box and allows tracking: Appeal Coordinator WTC Health Program 327 Columbia Turnpike Rensselaer, NY 12144 |
For certification denial, decertification, or treatment authorization denial appeals, your appeal request may also include a request for you or your designated representative to make a 15-minute oral statement by telephone.
Appeal Process
When the Program receives your appeal, the Administrator will appoint a federal official independent of the Program to review your appeal.
The federal official will review all available records, including any oral statement made by you or your designated representative, that are relevant to the Program’s decision to assess whether your appeal should be granted. This review would include any relevant new information submitted by you.
Oral statements are not accepted for enrollment denial or disenrollment appeals.
For certification and treatment denial appeals, the federal official may also consult one or more qualified experts to review the Program’s decision and any additional information provided by you.
Based on the review, the federal official makes a recommendation to the Administrator regarding whether or not your appeal should be granted.
More information on the appeal process is available on the Appeals page.
Final Appeal Decision and Notification of the Outcome
The Administrator reviews the federal official’s recommendation and any relevant information and makes a final decision on your appeal. You will be notified in writing of the following:
- The recommendation and findings made by the federal official;
- The Administrator’s final decision on your appeal;
- An explanation of the Administrator’s final decision; and
- Any actions taken by the Program in response to the Administrator’s final decision.
Once the Administrator has made a decision on your appeal, it is final. The Administrator’s decision may not be appealed further.
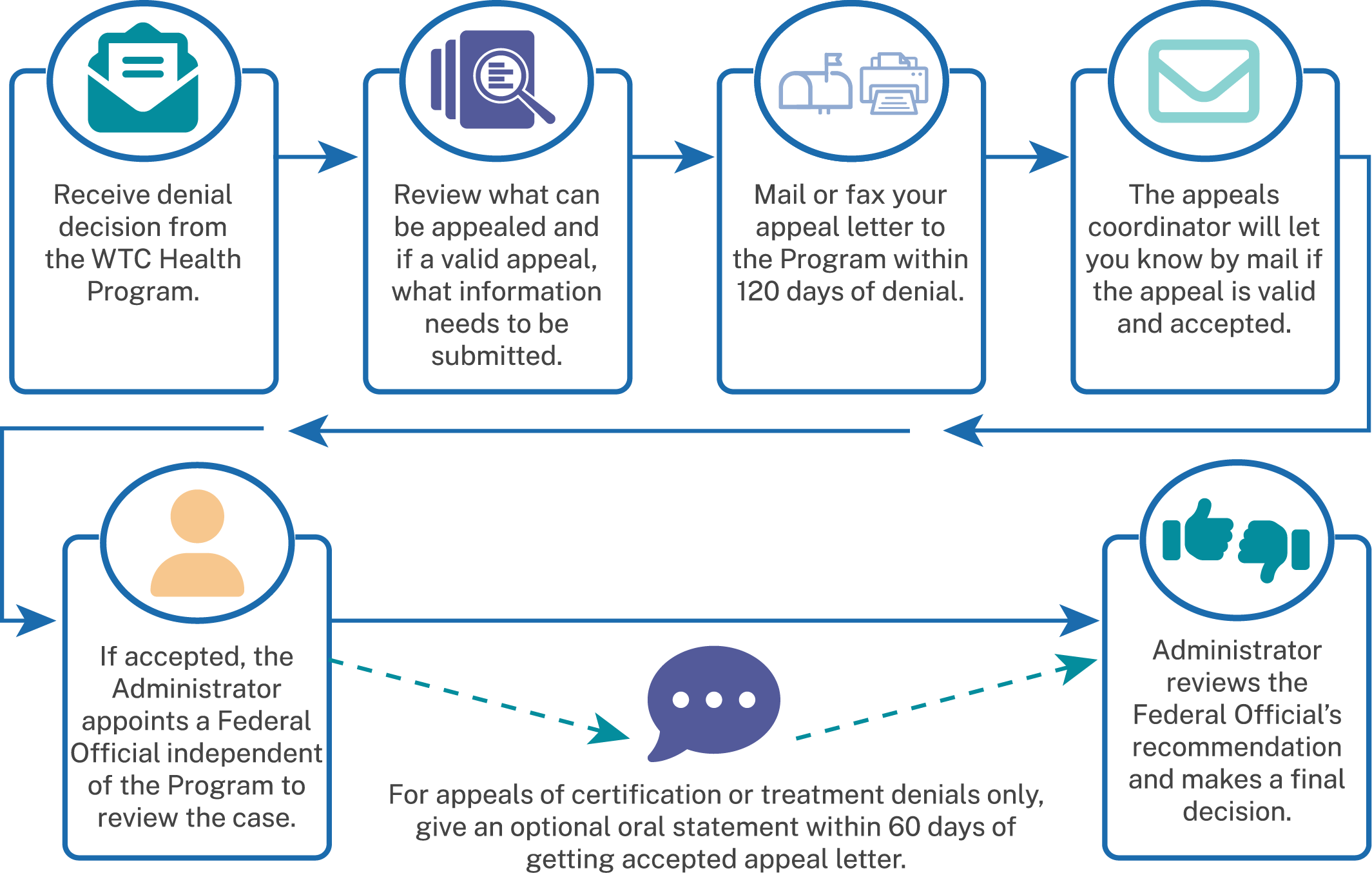
HIPAA Privacy Practices in the WTC Health Program
This notice describes how medical information about you may be used and disclosed and how you can get access to this information. Please review carefully.
The Health Insurance Portability and Accountability Act of 1996 (HIPAA) requires the World Trade Center (WTC) Health Program to maintain the privacy and security of your personal health information and to provide you with notice of its legal duties and privacy practices with respect to how your personal health information is held, used, and disclosed by the WTC Health Program.
How Do We Use and Share Your Personal Health Information?
The WTC Health Program must use and share your personal health information to provide information:
- To you, someone you name to receive your personal health information, or someone who has the legal right to act for you (the WTC Health Program will make sure that the person has the proper authority before taking any action);
- To the Secretary of the Department of Health and Human Services (HHS), if necessary, to make sure your privacy is protected and that the HIPAA requirements are being followed; and
- Where required by law.
How Else Do We Use and Share Your Personal Health Information?
The WTC Health Program may use and share your personal health information to provide you with treatment, to pay for your health care, and to operate the WTC Health Program. For example, the WTC Health Program may use or share your personal health information in the following ways:
- The WTC Health Program will collect and use your personal health information to decide if you meet the necessary requirements for coverage of your health condition(s) under the WTC Health Program. Conditions which meet these requirements are then “certified” by the WTC Health Program.
- The WTC Health Program will collect and use your personal health information to determine your diagnosis and any medically necessary treatment for your “certified” health conditions.
- The WTC Health Program will disclose your personal health information to the Centers for Medicare and Medicaid Services (CMS) Office of Financial Management to pay providers for eligible health care services you received.
- The WTC Health Program will review and use your personal health information to make sure you are receiving quality healthcare.
Under limited circumstances, the WTC Health Program may use or share your personal health information for the following purposes:
- To other federal and state agencies, where allowed by federal law, that need WTC Health Program health data for their program operations;
- For public health activities conducted by public health authorities (such as reporting disease outbreaks);
- For health care oversight activities (such as fraud and abuse investigations);
- For judicial and administrative proceedings (such as in response to a court order);
- For law enforcement purposes;
- To avoid a serious and imminent threat to health or safety;
- For purposes of reporting information to a government authority about victims of abuse, neglect, or domestic violence;
- To report information about deceased individuals to a coroner, medical examiner, or funeral director;
- To organ procurement organizations for organ or tissue donation and transplantation purposes;
- For research purposes, under certain conditions;
- For worker’s compensation purposes; or
- To contact you about new or changed coverage under the WTC Health Program.
What Are Your Rights When It Comes To Your Personal Health Information?
When it comes to your personal health information, you have certain rights. By law, you have the right to:
- Receive a paper copy of this privacy notice. You can ask for a paper copy of this notice even if you have already received an electronic copy (for example, by email). We will provide you with a paper copy promptly upon request.
- Receive a list that shows with whom we have shared your personal health information. You can ask for a list (accounting) of the times we have shared your personal health information for six years prior to the date you ask. The list shows whom we shared it with, when, and why. The list does not include information about treatment, payment, health care operations, and certain other disclosures (such as any you asked us to make). We will provide one free accounting a year but will charge a reasonable, cost-based fee if you ask for another one within 12 months.
- Receive a copy your personal health information. You can ask to see or get a copy of your health and claims records and other health information that we have about you. You can contact us by using the information included in the How Can You Contact the WTC Health Program? section. We will provide a copy or a summary of your health and claims records, usually within 30 days of your request. We may charge a reasonable, cost-based fee to send your health and claims records.
- Ask us to change (“amend”) your personal health information. You can request to change your records if you believe that your personal health information is wrong or that information is missing. Please note that we may deny your request to change your personal health information if we believe the information in your records is accurate and complete. If your request is denied, we will provide you with a written explanation of the denial within 60 days of the date we received your request. You may have a statement added to your personal health records to reflect your disagreement.
- Request confidential communications. You may request that we communicate your personal health information in a private (“confidential”) way. You may ask that we contact you in a specific way (for example, home or office phone) or to send mail to a different address.
- Ask us to limit how we use and share your personal health information. You can ask us not to use or share certain health information. We are not required to agree to the limits you request, except under certain circumstances.
- Choose someone to act for you. If you have given someone medical power of attorney or if someone is your legal guardian, that person can exercise your rights and make choices about your personal health information. We will make sure the person has this authority and can act for you before we take any action.
- Receive breach notification. You can expect to be informed of and receive notification if a breach occurs that may have compromised the privacy or security of your information.
When Do We Require Your Written Permission?
By law, the WTC Health Program must have your written permission (authorization) to use or share your personal health information for any purpose that is not set out in this notice, including certain uses or disclosures of psychotherapy notes. In addition, the WTC Health Program will not sell or market your personal health information without your written permission.
You may take back (revoke) your written permission anytime, except in cases where the WTC Health Program has already acted on your permission. If you take back your written permission, please provide that to the WTC Health Program in writing.
The WTC Health Program is prohibited from using or sharing your personal genetic health information (i.e., your genetic tests, the genetic tests of your family members, and your family medical history) to determine your eligibility and enrollment into the WTC Health Program (i.e., underwriting).
What Are the Responsibilities of the WTC Health Program?
The WTC Health Program is required by law to abide by the terms of this privacy notice. The WTC Health Program has the right to change this privacy notice and the changes will apply to all the information that we have about you. If we make any significant changes to this notice, a copy of the revised notice will be made electronically available on the WTC Health Program website and you will receive the new notice by mail or email within 60 days. You may also request to receive a copy of the notice at any time.
How Can You Contact the WTC Health Program?
You can call 1-888-982-4748 to get further information about matters covered by this notice. Ask to speak to a member of the WTC Health Program’s HIPAA Team. To view an electronic copy of the WTC Health Program’s HIPAA privacy notice, you can visit the WTC Health Program’s website.
How Can You File a Complaint?
If you believe that your privacy rights have been violated, you may file a complaint with the WTC Health Program by calling 1-888-982-4748 or by sending a letter to P.O. Box 7000 Rensselaer, NY 12144 ATTN: WTC Health Program, HIPAA Complaint. Filing a complaint will not affect your coverage under the Program.
You may also file a complaint with the HHS Office for Civil Rights by sending a letter to
200 Independence Avenue, SW, Washington, DC 20201, calling 1-800-368-1019, or visiting the HHS Filing a Complaint page . TTY users should call 1-800-537-7697.
The Notice of Privacy Practices for the WTC Health Program is effective January 23, 2024.
Complaint Procedure
All Program health care providers and staff share responsibility for ensuring member satisfaction. If you have a problem or concern about the services you receive, please ask for help. Each CCE and the NPN has an administrator who is able to assist you with your concerns and complaints.
If you have a problem with any aspect of the service you have received at your CCE, call or visit the administrative office at that facility.
If you have a problem with the service you have received through the NPN, you may call MCA-Sedgwick, who administers the NPN, at 1-800-416-2898. The NPN has an administrator or director who is responsible for addressing concerns involving the provider network.
If you are not satisfied with the way your complaint was handled, Member Services Representatives who work directly for the Program are available to address your concerns. Be sure to provide complete information regarding the nature of your complaint, including names, dates, and any other specific information. We will make every effort to respond to your request as quickly and effectively as possible. You can contact the Program’s call center at 1-888-982-4748.
If you have comments and feedback for the WTC Health Program about our performance, you can use our online feedback form.
Fraud and Abuse
Fraud is the intentional deception or misrepresentation that an individual or entity makes knowing that the misrepresentation could result in some unauthorized benefit to the individual, or the entity, or to some other third party.
The Program will closely monitor any fraudulent activity including the submission of fraudulent information in support of a claim of eligibility or for necessary and covered services, fraudulent misuse of the Program by health care providers participating in the Program, and submission of claims for services not provided or needed as claimed.
The Program will report fraudulent conduct to Federal law enforcement agencies and violators may be subject to criminal, civil, or administrative penalties.
Information concerning suspected fraud related to the Program by contractors, grantees, health care providers, or individual recipients should be reported to the U.S. Department of Health and Human Services, Office of Inspector General by phone at 1-800-HHS-TIPS (1-800-447-8477), online at oig.hhs.gov/fraud/report-fraud/, or in writing to the following address:
U.S. Department of Health and Human Services
Office of Inspector General
ATTN: OIG HOTLINE OPERATIONS
P.O. Box 23489 Washington, DC 20026
Other September 11th Programs
The following programs are not part of the WTC Health Program. However, a Program member may also be eligible for these programs.
September 11th Victim Compensation Fund
The September 11th Victim Compensation Fund (VCF) is a separate program from the WTC Health Program and is administered by the U.S. Department of Justice. The VCF provides financial compensation for physical injuries, illnesses, or deaths that happened as the result of the 9/11 attacks. The VCF does not compensate for mental health conditions and does not distinguish between responders and survivors.
The VCF has a different process to sign up than the WTC Health Program. You need to register with them before filing a claim. You do not have to be sick or injured to register. Registration preserves your right to file a VCF claim in the future.
Enrollment in the WTC Health Program does not automatically register you or file a claim with the VCF.
For more information about the VCF, including everything needed to register, file, and monitor the status of a claim, visit the VCF's website or contact the VCF at 1-855-885-1555. Do not contact the WTC Health Program call center or your Program clinic for VCF questions or issues.
WTC Health Registry
The Zadroga Act also extended the WTC Health Registry. The Registry was developed to document and evaluate the long-term physical and mental health effects of the 9/11 attacks. To date, the Registry is the largest effort in the U.S. to monitor the health of people exposed to a large-scale disaster.
This is done through regular surveys of the enrolled participants. Enrollment in the Registry occurred in 2003-2004 through voluntary responses to an initial survey and is now closed.
For more information about the WTC Health Registry, please contact them directly at wtchr@health.nyc.gov. You can also visit the WTC Health Registry website or call 1-866-692-9827.
Workers’ Compensation Benefits
WTC Health Program members whose certified WTC-related health condition(s) are also work-related may be eligible to file for workers’ compensation benefits. Even if you are a Program member and receiving medical treatment for your certified WTC-related health condition(s) through the Program, it can be beneficial to file a workers’ compensation claim if eligible. It may also provide a financial award for lost wages related to your WTC-related health condition(s).
New York State Workers’ Compensation Law
Workers and volunteers who performed rescue, recovery, and clean-up of the World Trade Center and other impacted sites can register with the New York State (NYS) Workers’ Compensation Board. This registration preserves the right to file for workers’ compensation benefits through the State of New York should you need them in the future.
NYS passed legislation (Senate Bill S9294A) on September 9, 2022, extending the deadline until September 11, 2026, for filing the Registration of Participation in World Trade Center Rescue, Recovery and/or Clean-up Operations form (Form WTC-12).
For information on eligibility, how to download Form WTC-12, and how to file a claim with the NYS Workers’ Compensation Board, call 1-877-632-4996.
Workers can also pick up Form WTC-12 in-person from any New York State Workers’ Compensation Board office.
Glossary
- 9/11 Exposure Assessment
- A questionnaire used to gather a comprehensive and medically relevant exposure history that helps physicians determine if 9/11 exposures are substantially likely to be a significant factor in aggravating, contributing to, or causing conditions that may be submitted to the Program for a certification request.
- Administrator (the Administrator of the WTC Health Program):
- The Director of the National Institute for Occupational Safety and Health (NIOSH), part of the Centers for Disease Control and Prevention (CDC) in the Department of Health and Human Services (HHS), or his or her designee. The Administrator is the person responsible for overseeing and administering the Program.
- Annual Monitoring Exam:
- Also called Medical Monitoring Exam; Detailed yearly health exam of a WTC Responder or Certified-Eligible Survivor that looks for WTC-related physical and mental health conditions. Findings help determine whether a member has a condition that can be certified (approved) for treatment in the WTC Health Program.
- Appeal:
- To formally challenge a decision made by the Program to not enroll an applicant or to disenroll a member, to not certify a health condition or to decertify a health condition, or to not cover a treatment.
- Benefits Counseling:
- A service available to members where a WTC Health Program staff person informs you about various benefits outside of the Program that you might be eligible for and assists you to apply for those benefits.
- Case Management:
- A collaborative process that facilitates medical care and treatment plans to meet individual healthcare needs, maximize the care goals, and improve the continuity and quality of care.
- Centers for Medicare and Medicaid Services (CMS):
- The Federal agency that administers the Medicare and Medicaid programs; CMS assists the WTC Health Program with payment functions.
- Certification:
- A decision by the WTC Health Program that your health condition is included on the List of WTC-Related Health Conditions, that your health condition and 9/11 exposures meet Program policies, and that your 9/11 exposures are substantially likely to have been a significant factor in aggravating, contributing to, or causing the health condition.
- Certification Request:
- Paperwork completed by your WTC Health Program Participating Provider to request certification of your WTC-related health conditions by the Program. It includes information about you, your health condition(s), and your 9/11 work and exposures.
- Certified:
- A certified WTC-related health condition (or medically associated health condition) is one that has been approved for coverage by the Program based on the approval of a certification request for that condition.
- Certified-Eligible Survivor:
- A Survivor with a certified WTC-related health condition(s). These members are eligible for annual monitoring exams and treatment for certified WTC-related and medically associated health condition(s).
- Clinical Center of Excellence (CCE):
- A medical center under contract with the WTC Health Program to provide WTC-related health services to members.
- Coordination of Benefits:
- A process that helps determine who pays a medical bill first when there is more than one potential payor.
- Designated Representative:
- A person that you choose to represent your interests in the Program. They can represent your interests in Program administrative processes, including during an appeal.
- Durable Medical Equipment (DME):
- Medical equipment used in a member’s home, such as CPAP machines and wheelchairs.
- EKG:
- Abbreviation for electrocardiogram. An electrocardiogram is a medical test used to look at and record the electrical activity of your heart.
- Formulary:
- A list of prescription drugs covered by the Program. The CCEs and the NPN are given updated lists periodically.
- Fraud:
- Intentional deception or misrepresentation by an individual or entity with knowledge that the misrepresentation could result in an unauthorized benefit to the individual, the entity, or some other third party.
- Health Insurance Portability and Accountability Act of 1996 (HIPAA):
- A federal law that established national privacy standards for the protection of personal health information (called “protected health information” or PHI under HIPAA) given to and used by health care entities such as health plans, hospitals, clinics, and doctors. The law outlines how your PHI can be disclosed to other entities and when your consent is required. Learn more about your rights under HIPAA on the HHS HIPAA page.
- Home Health Services:
- Healthcare services you receive in your home. These services are delivered according to a plan written by your healthcare provider.
- Hospice Care:
- Special services provided to an individual with a terminal illness. Hospice care addresses the medical, physical, social, emotional, and spiritual needs of a terminally ill person. Hospice also provides care and rest services to caregivers and family members.
- Initial Health Evaluation:
- Also called a baseline monitoring exam for Responders; Assessment of one or more symptoms that may be associated with a WTC-related health condition to evaluate whether a new member has a WTC-related health condition and is eligible for treatment under the Program. This exam includes a medical and exposure history, a physical examination, and additional medical testing as needed.
- Inpatient:
- A patient who is admitted to a healthcare facility, like a hospital or skilled nursing facility, for treatment that requires at least one overnight stay.
- Inpatient Care:
- Healthcare you get when you are admitted to a health care facility, like a hospital or skilled nursing facility.
- James Zadroga 9/11 Health and Compensation Act of 2010 (Zadroga Act):
- Public Law 111-347 passed by the U.S. Congress in 2010 that created the WTC Health Program. The Zadroga Act provided funding for monitoring, medical and mental health treatment, and research for WTC Responders and Survivors. The Zadroga Act also reopened the September 11th Victim Compensation Fund (VCF).
- Latency:
- The amount of time that has passed between your earliest 9/11 exposures and the date you were first diagnosed with a health condition.
- Level 1 Authorization:
- When your WTC Health Program provider can decide that your needed treatment or medical service can be covered by the Program without having to seek permission from anyone else in the Program.
- Level 2 Prior Authorization:
- When your WTC Health Program provider must request permission from your CCE or the NPN Medical Director for your needed treatment or medical services to be covered by the Program.
- Level 3 Prior Authorization:
- When your WTC Health Program provider must request permission from the WTC Health Program administration for your needed treatment or medical services to be covered by the Program.
- List of WTC-Related Health Conditions (List):
- Mental and physical health conditions eligible for coverage in the WTC Health Program identified in the Zadroga Act and Program regulations at 42 C.F.R. § 88.15.
- Mammogram:
- An X-ray of the breast.
- Managed Care Advisors (MCA)-Sedgwick:
- The two organizations that together administer the Nationwide Provider Network (August 2022 to present) and manage Program health care for members who live outside of the NY metropolitan area. Sedgwick is MCA's parent company.
- Maximum Time Interval:
- For certain aerodigestive health conditions, the maximum amount of time that could have gone by between your last 9/11 exposure and the onset of symptoms of your WTC-related health condition.
- Medicaid:
- A joint Federal/state program that covers medical costs for some people with low incomes and/or disabilities.
- Medical Benefits Team:
- The WTC Health Program staff who oversee medical benefits for Program members and make initial decisions about treatment authorizations for members.
- Medical Emergency:
- A serious physical or mental health condition for which immediate treatment is necessary (it would result in a threat to life, limb, or sight, or when a person is at immediate risk to self or others).
- Medically Associated Health Condition:
- A health condition that results from treatment of a certified WTC-related health condition or results from the progression of a certified WTC-related health condition. A medically associated health condition must be certified as WTC-related by the Program in order to be eligible for coverage.
- Medically Necessary Treatment:
- Services by physicians and other health care providers, including diagnostic and laboratory tests, prescription drugs, inpatient and outpatient hospital services, and other care that is appropriate to manage, improve, or cure a certified WTC-related health condition or a medically associated health condition.
- Medicare:
- A Federal health insurance program for people who are 65 or older, certain younger people with disabilities, and people with end stage renal disease.
- Member:
- A WTC Responder or WTC Survivor who has been found eligible for the Program and enrolled.
- Minimum Latency Requirement:
- The shortest amount of time that could have passed between your earliest 9/11 exposure and the date you were first diagnosed with a cancer in order for your cancer to be covered by the Program.
- National Institute for Occupational Safety and Health (NIOSH):
- The federal agency that administers the WTC Health Program. NIOSH is part of the Centers for Disease Control and Prevention (CDC), in the U.S. Department of Health and Human Services (HHS).
- Nationwide Provider Network (NPN):
- A nationwide network of health care providers across the country under contract with the Program to provide WTC-related health care for Program members who live outside the NY metropolitan area and want to receive their WTC-related health care locally.
- Network:
- The health care providers, facilities, and pharmacies the Program has contracted with to provide you with health care services covered by the Program.
- Network Provider:
- A provider that is part of a network contracted with the Program or one of the WTC Health Program’s vendors.
- New York City (NYC) Disaster Area:
- The area within New York City that is the area of Manhattan south of Houston Street, and any block in Brooklyn wholly or partially contained within a 1.5 mile radius of the former WTC complex.
- New York (NY) Metropolitan Area:
- An area specified by the Administrator to include portions of New York, New Jersey, Connecticut, and Pennsylvania; Program members residing within the area may access CCEs for their WTC-related health care.
- Out-of-Network Provider:
- A provider that is not part of a network contracted with the Program or one of the WTC Health Program’s vendors.
- Payor of Last Resort:
- The entity that pays last when there are multiple entities paying a bill.
- Petition:
- A formal written request to the Administrator to add a health condition to the List of WTC-Related Health Conditions.
- Pharmacy Benefit Manager:
- A third-party administrator that oversees pharmacy benefits on behalf of health programs, contracts with pharmacies, and processes and pays prescription claims. A pharmacy benefit manager may also be referred to as a ‘PBM.’
- Preferred Medication:
- An available brand name drug chosen by healthcare experts to be most effective in treating a condition at the lowest cost. Preferred medications are used when a generic version of a drug is unavailable.
- Primary Health Insurance:
- Whatever private or public health insurance you have. Private insurance may include employer-sponsored health insurance or insurance purchased from the health insurance marketplace. Public insurance may include Medicare or Medicaid coverage. Some individuals may have a mix of both private and public insurance. The WTC Health Program is a limited health care benefits program that provides monitoring and treatment for certified WTC-related health conditions only. The Zadroga Act requires all members to maintain minimum essential health insurance coverage outside of the Program.
- Screening-Eligible Survivor:
- An individual who meets the WTC Survivor eligibility criteria and has symptoms of a WTC-related health condition. Upon enrollment in the Program, a Screening-Eligible Survivor is eligible for a one-time, initial health evaluation paid for by the Program.
- September 11th Victim Compensation Fund (VCF):
- A Program administered by the U.S. Department of Justice that provides compensation for economic and non-economic loss to individuals who were physically injured, or made physically ill, or relatives of deceased individuals who were killed, as a result of the terrorist-related aircraft crashes on September 11, 2001. Learn more at VCF's website or call 1-855-885-1555.
- Skilled Nursing Facility:
- A nursing facility with the staff and equipment needed to provide skilled nursing care.
- Urgent Care:
- Medically necessary services required for an illness or injury that would not result in further disability or death if not treated immediately but requires professional attention within 24 hours.
- U.S. Preventive Services Task Force (USPSTF):
- An independent, volunteer panel of national experts in disease prevention and evidence-based medicine. The USPSTF works to improve the health of all Americans by making evidence-based recommendations about clinical preventive services. Learn more at USPSTF's website .
- Workers’ Compensation:
- An insurance plan that employers are required to have to cover workers who get sick or injured on the job. It can provide injured or ill workers with medical and compensation benefits.
- World Trade Center (WTC) Health Program (Program):
- The Program established by Title XXXIII of the Public Health Service Act as amended, 42 U.S.C. §§ 300mm through 300mm– 61 (codifying Title I of the James Zadroga 9/11 Health and Compensation Act of 2010 (Pub. L. 111–347, as amended by Pub. L. 114-113)), to provide medical monitoring and treatment benefits for eligible responders and survivors of the September 11, 2001, terrorist attacks.
- WTC-3 Certification Package:
- Paperwork completed by your Program doctor to request certification of your WTC-related health conditions by the Program. It includes information about you, your health condition(s), and your 9/11 work and exposures.
- WTC Health Program Non-Participating Provider:
- A Network Provider that has not agreed to the WTC Health Program’s terms and conditions or is not able to provide services to WTC Health Program members.
- WTC Health Program Participating Provider:
- Also called a participating provider or Program provider; A Network Provider that has agreed to the Program’s terms and conditions and is able to provide services to WTC Health Program members.
- WTC Health Registry:
- A study run by the New York City Department of Health and Mental Hygiene to document and evaluate the long-term physical and mental health effects of 9/11. Learn more at www1.nyc.gov/site/911health/about/wtc-health-registry.page
- An illness or health condition for which exposure to airborne toxins, any other hazard, or any other adverse condition resulting from the September 11, 2001, attacks, based on an examination by a medical professional with expertise in treating or diagnosing the health conditions in the List of WTC-Related Health Conditions, is substantially likely to be a significant factor in aggravating, contributing to, or causing the illness or health condition or mental health condition. Only those conditions on the List of WTC-Related Health Conditions codified in 42 C.F.R. § 88.15 may be considered WTC-related health conditions and a health condition must be certified by the Program to be eligible for coverage.
- WTC Responder:
- Workers or volunteers who provided rescue, recovery, debris cleanup, and related support services on or in the aftermath of the September 11, 2001 attacks for certain amounts of time during the period between September 11, 2001 and July 31, 2002. There are three groups of Responders in the WTC Health Program: FDNY Responders (and surviving FDNY family members); WTC General Responders (including NYPD); and Pentagon and Shanksville, PA Responders. Learn more on the Eligible Groups page.
- WTC Survivor:
- Also known as NYC Survivors; Includes individuals who were present in NYC Disaster Area in the dust or dust cloud on September 11, 2001; individuals who lived, worked or went to school or childcare, or adult child care in the NYC Disaster area for a certain amount of time during the period between September 11, 2001 and July 31, 2002; certain cleanup and maintenance workers; and certain individuals eligible (or whose place of employment was eligible) to receive certain grants from the Lower Manhattan Development Corporation. Learn more on the Eligible Groups page.
