Chapter 1—Overview of the WTC Health Program
TABLE OF CONTENTS
Last Revised – January, 2025
1.0 Purpose and Scope
The purpose of the World Trade Center Health Program (WTC Health Program or the Program) Administrative Manual is to document the policies and procedures that provide the comprehensive framework for administering the Program.
The audience of the Administrative Manual includes Program staff, the Health Program Support (HPS)/Third-Party Administrator (TPA) Contractor, and the Clinical Centers of Excellence (CCEs) and Nationwide Provider Network (NPN) that provide medical care to members. The Administrative Manual is a public document that can also provide information to Program members, outreach partners, and the general public. The Administrative Manual is updated as needed to reflect revised Program policies, procedures, and operations.
This chapter provides a general overview of the WTC Health Program, including a brief description of its history and origins, a summary of the guiding legislation, and a description of the Program and its organization developed to carry out the provisions of the legislation.
1.1 Statutory and Regulatory References
The WTC Health Program was established by Title I of Public Law 111-347, the James Zadroga 9/11 Health and Compensation Act of 2010 (the Zadroga Act), as amended by Pub. L. 114-113, Pub. L. 116-59, Pub. L. 117-328, and Pub. L. 118-31. Title I of the Zadroga Act amended the Public Health Service Act and is codified at 42 U.S.C. §§ 300mm to 300mm-64. Portions of the Zadroga Act found in Titles II, III, and IV do not pertain to the WTC Health Program and are codified elsewhere. Program regulations are published in Title 42, Part 88 of the Code of Federal Regulations (C.F.R.). Descriptions of the major provisions of the Zadroga Act and the Part 88 regulations are outlined in Section 3 below.
2.0 History of the WTC Health Program
Since the terrorist attacks of September 11, 2001, the U.S. Department of Health and Human Services (HHS), the Centers for Disease Control and Prevention (CDC), and the National Institute for Occupational Safety and Health (NIOSH) have facilitated health evaluations and screenings for individuals who responded to, or were survivors of, the attacks to identify and treat any health issues resulting from their exposures in the aftermath of the attacks.
- The first such program began in 2002 with grants funded through discretionary appropriations and awarded to the Mount Sinai School of Medicine (Mt. Sinai) and the Fire Department of the City of New York (FDNY) to provide health screenings to 9/11 responders only. Mt. Sinai worked with specialized occupational health clinics in the New York (NY) metropolitan area, developing a standardized health screening protocol.
- Bellevue Hospital also documented symptoms among downtown residents and worked with the community to establish a self-funded treatment program.
- In 2004, the health screenings program at Mt. Sinai and FDNY were expanded to include periodic monitoring examinations in addition to the initial health screenings. The individual clinics that provided the screening and monitoring examinations were funded through cooperative agreements between NIOSH, Mt. Sinai, and FDNY.
- In Fiscal Year 2006, diagnostic and treatment services were added to provide medical care for WTC-related occupational health conditions. The program was called the WTC Medical Monitoring and Treatment Program (MMTP), and its medical providers were individually funded as CCEs. They included Mt. Sinai, New York University School of Medicine-Bellevue Hospital Center, Queens College, Richmond University Medical Center, State University of New York (SUNY)-Stony Brook, and University of Medicine and Dentistry of New Jersey. Services were provided outside the NY metropolitan area by a network of providers through a contract with Logistics Health, Inc. (LHI), now known as OptumServe Health Services, Inc.
- Also in 2006, NYC funded the WTC Environmental Health Center (EHC) Community Program at Bellevue Hospital.
- In 2008, for the first time, federal funds were appropriated to provide screening, diagnostic, and treatment services to residents, students, and others who were affected by the September 11, 2001, attacks in NYC, under the WTC EHC Community Program, operated under a CDC-sponsored grant to the NYC Health and Hospitals Corporation (H+H).
- On January 2, 2011, the President signed the James Zadroga 9/11 Health and Compensation Act (the Zadroga Act) into law, establishing the WTC Health Program within HHS.
- On December 18, 2015, the President signed the Consolidated Appropriations Act, 2016 (Public Law 114-113), which included the James Zadroga 9/11 Health and Compensation Reauthorization Act, amending the Public Health Service Act to reauthorize the WTC Health Program for 75 years, ending in 2090.
- On September 27, 2019, the President signed the Continuing Appropriations Act, 2020, and Health Extenders Act of 2019 (Public Law 116-59), which further amended provisions regarding the WTC Health Program in the Public Health Service Act to increase numerical limitations on the enrollment of 9/11 newly enrolled responders and certified-eligible survivors in the WTC Health Program.
- On December 22, 2023, the President signed the National Defense Authorization Act for Fiscal Year 2024 (Public Law 118-31), which further amended provisions regarding the WTC Health Program in the Public Health Service Act to expand eligibility requirements for responders at the Shanksville, Pennsylvania and the Pentagon sites.
3.0 Summary of the Zadroga Act
-
The Zadroga Act established the WTC Health Program within HHS and mandated that the Program begin providing services on July 1, 2011.1 The Program only covers services provided on and after July 1, 2011.2 The Program is required to provide:
- Medical monitoring and treatment benefits to eligible emergency responders and recovery and cleanup workers who responded to the September 11, 2001, terrorist attacks in NYC, Shanksville, PA, and the Pentagon;3 and
- Initial health evaluation, monitoring, and treatment benefits to eligible residents and other building occupants and area workers in NYC who were directly impacted by the attacks.4
- Monitoring and treatment benefits and initial health evaluation benefits are provided at no cost to enrolled responders and certified-eligible survivors; screening-eligible survivors receive an initial health evaluation at no cost.5
-
Administrator of the WTC Health Program (Administrator): The PHS Act directs the Secretary of HHS to designate an HHS Department official to be the Administrator.6 Certain activities of the Administrator are reserved to the Secretary to delegate at their discretion; other duties not explicitly reserved to the Secretary are specifically assigned to the Director of NIOSH or their designee. The Secretary has designated the Director of NIOSH to serve as the Administrator for the discretionary activities; the Secretary delegated responsibilities for disbursing payments to providers to the Centers for Medicare & Medicaid Services (CMS).7
Specific duties of the Administrator include:
- Establish an enrollment process for eligible responders and screening-eligible survivors;8
- Establish end-dates for Pentagon and Shanksville responder eligibility;9
- Establish a process for the certification of health conditions;10
- Add new health conditions to the List of WTC-Related Health Conditions through rulemaking;11
- Establish a medical necessity standard;12
- Establish a quality assurance program to ensure adherence to monitoring and treatment protocols, appropriate diagnostic and treatment referrals, prompt communication of test results to participants, and other programmatic elements the Administrator finds necessary;13
- Submit an annual report to Congress, including statistics on eligible individuals; costs of monitoring, screening, and treatment; administrative costs; administrative experience; summary of new scientific reports or studies that address WTC-related exposures; and WTC Health Program Scientific/Technical Advisory Committee (STAC) recommendations and the Administrator’s actions on those recommendations.14
- Establish a process for appeals of denial of enrollment, denial of certification of health conditions, and denial of medically necessary treatment.15
- WTC Responder Enrollment and Eligibility: The PHS Act establishes eligibility criteria for NYC responders,16 Pentagon responders,17 and Shanksville responders.18 The total number of newly enrolled responders is limited to 75,000 individuals at any time;19 individuals included on the terrorist watchlist may not be enrolled in the Program.20
- WTC Survivor Enrollment and Eligibility: The PHS Act establishes eligibility criteria for NYC screening-eligible survivors21 and certified-eligible survivors.22 The PHS Act requires that a CCE/NPN provides initial health evaluations at no charge to determine if the screening-eligible survivor has a WTC-related health condition.23 The total number of newly enrolled certified-eligible survivors is limited to 75,000 individuals at any time;24 individuals included on the terrorist watch list may not be enrolled in the Program.25
- WTC Health Program Scientific/Technical Advisory Committee (STAC): The STAC is established by the Administrator of the WTC Health Program, with a specified, diverse membership.26 The frequency of the STAC meetings is discretionary.27 Reports of the STAC are to be published on the WTC Health Program website.28
- WTC Health Program Steering Committees: The PHS Act establishes two steering committees: one for WTC responders and another for WTC survivors.29 Each of these committees establishes a forum for providing input from affected stakeholders and facilitating the coordination of services for eligible individuals.30 Each has specific requirements for membership and was initially composed of members of steering committees that existed when the Zadroga Act was signed into law.31 The steering committees appoint their members, and the Administrator consults with the two committees.
- Certification of Health Conditions: The PHS Act establishes an initial List of WTC-Related Health Conditions.32 The WTC Health Program is required to certify WTC-related health conditions for treatment and monitoring33 after a Program physician determines that exposure to airborne toxins, any other hazard, or any other adverse condition resulting from the September 11, 2001, terrorist attacks is substantially likely to be a significant factor in aggravating, contributing to, or causing the illness or health condition, or is a mental health condition for which a Program physician finds that the terrorist attacks are substantially likely to be a significant factor in aggravating, contributing to, or causing.34 The health condition must be included on the List of WTC-Related Health Conditions35 or identified as a health condition medically associated with a WTC-related health condition.36 Denials of certification may be appealed.37
- Medical Benefits: The PHS Act establishes that the scope of treatment covered by the Program includes services of physicians and other healthcare providers, diagnostic and laboratory tests, prescription drugs, inpatient and outpatient hospital services, and other medically necessary treatment.38 In certain situations, the Program may approve medical treatment in advance of a decision to certify the health condition as a WTC-related health condition.39
- Claims Processing and Billing: Benefits under the WTC Health Program for work-related health conditions are offset by workers’ compensation benefits, except for those plans to which NYC is obligated to make payments.40 WTC Health Program benefits do not absolve other workers’ compensation or health insurance plans of their obligations regarding payment of claims for medical treatment of Program members.41 Initial health evaluation, monitoring, and treatment payments are to be made using the rates applicable under the Federal Employees’ Compensation Act (FECA) regulations in 20 C.F.R. Part 20.42 If no FECA rate is available, the WTC Health Program will reimburse providers for treatment pursuant to the applicable Medicare fee for service rate, as determined appropriate by the Administrator; if neither FECA nor Medicare fee for service rates have been established, reimbursement will be made at rates as determined appropriate by the Administrator.43 Payment rates may not exceed the rate the Office of Workers’ Compensation Programs in the Department of Labor would pay for such products or services at the time they were provided.44
- Data Centers: The PHS Act requires the Administrator to enter into contracts with the Data Centers to receive, analyze, and report data from a CCE/NPN to the WTC Health Program Administrator; develop Program monitoring, treatment, and initial health evaluation protocols; coordinate outreach and retention activities with the CCEs; establish criteria to credential medical providers participating in the Program; coordinate and administer the activities of the WTC Health Program Steering Committees; and meet with the CCEs for input on data collection and analysis and medical protocols.45
- Clinical Centers of Excellence (CCEs): The PHS Act requires the Administrator to enter into contracts with the CCEs to provide monitoring, treatment, and initial health evaluation benefits; conduct outreach to eligible and enrolled individuals; provide counseling regarding benefits available under the WTC Health Program and other programs; provide translational and interpretive services for non-English-proficient participants; and collect and report data.46 The definition of and contract requirements for CCEs and transition requirements for continuity of care are also provided.47
- Nationwide Provider Network (NPN): The PHS Act requires the Administrator to establish a nationwide network of healthcare providers to provide monitoring and treatment benefits and initial health evaluation near such individuals’ areas of residence in such states.48 Any healthcare provider participating in the network must meet the criteria for credentialing established by the Data Centers, follow Program treatment protocols, collect and report data, and meet fraud, quality assurance, and other Program requirements.49
- Member Services: The PHS Act requires the development of an outreach program to provide information to potentially eligible individuals regarding benefits, clinical data collection and analysis, and research on health conditions resulting from the terrorist attacks.50 Outreach must include a public website, meetings with potentially eligible persons, development and distribution of outreach materials, and telephone information services. The services must be carried out in such a way as to reach all affected populations and include materials for culturally and linguistically diverse populations.51
- Governmental Affairs: The HHS Inspector General must conduct reviews of the healthcare and administrative expenditures under the Program to detect potential fraudulent or duplicate billing, payment for inappropriate services, or unreasonable administrative costs.52
- Pharmacy Benefits: Pharmacy prescription benefits are paid through contracts with outside vendors using a competitive bidding process. A separate contract may be used for FDNY participants.53
4.0 Organization
The WTC Health Program is administered by the National Institute for Occupational Safety and Health (NIOSH), which is part of the Centers for Disease Control and Prevention (CDC) within the Department of Health and Human Services (HHS).
The WTC Health Program is a division within NIOSH composed of an Office of the Director and three administrative branches that support the Program’s operations.54 The Research and Evaluation Branch establishes and manages the Program’s research agenda to increase understanding of the health effects of 9/11 and to improve member health and well-being. The Healthcare Benefits Branch oversees member eligibility for medically necessary treatment and monitoring of WTC-related health conditions. The Business Operations Branch provides business and management solutions for the Program, including strategic acquisition planning and procurement for contract awards. These branches are managed by the Office of the Director, which provides central management and strategic oversight of the Program through the Zadroga Act.
The work of the WTC Health Program is carried out through teams consisting of NIOSH employees aided in specific tasks by contract vendors. Key contractor functions for health plan operations are listed below, as well as the vendors currently assigned these tasks (note, vendors may change as part of routine acquisition and procurement award schedules):
- CCEs: Fire Department of the City of New York (FDNY); Icahn School of Medicine at Mount Sinai (ISMMS); New York City Health and Hospitals Corporation (H+H); New York University (NYU); Northwell Health, Inc.; Research Foundation for the State University of New York Stony Brook (SUNY); Rutgers, the State University of New Jersey; and OptumServe Health Services, Inc. William Street Clinic (WSC)
- NPN: Managed Care Advisors (MCA)-Sedgwick
- Health Program Support (HPS)/Third-Party Administrator (TPA): Karna, LLC (with General Dynamics Information Technology serving as the primary subcontractor)
- Pharmacy Benefit Manager (PBM): Express Scripts, Inc.
- DCs: FDNY; H+H; and ISMMS
- Outreach and Education contractors: FealGood Foundation; Hispanic Federation, Inc.; New York Committee for Occupational Safety and Health (NYCOSH); and 9/11 Environmental Action Inc.
- Health Program Evaluation (HPE): Health Research and Analysis, LLC (HRA)
- Research: The RAND Corporation
- Comprehensive Cost Avoidance (CCA) Contractor: Gainwell Technologies, LLC
The CCEs deliver healthcare services to members living in the NY metropolitan area, while the NPN delivers healthcare services to members who live outside the NY metropolitan area. The CCEs/NPN provide direct assistance and services to enrolled and potential members. They provide medical monitoring, screening, treatment services, and make referrals to affiliated medical providers for some medical services. They also oversee medical treatment, submit medical claims for reimbursement, and provide input on Program guidelines.
The HPS/TPA contractor provides administrative support for the Program in the areas of medical benefits and member services, including, but not limited to, member enrollment, health condition certification, affiliated provider credentialing and enrollment, claims processing, and coordination of benefits. The HPS/TPA contractor also maintains a call center and mailroom to respond to inquiries from potential enrollees, members, and providers.
Medical providers must be enrolled as WTC Health Program-affiliated providers to provide care to WTC Health Program members through a network assigned to the CCEs or the NPN. The HPS/TPA contractor manages the CCE provider network in the NY metropolitan area, while the NPN contractor manages the provider network serving members outside the NY metropolitan area. A list of the CCE/NPN clinics and their contact information is found at https://www.cdc.gov/wtc/clinics.html.
Chapter 2—Eligibility and Enrollment
TABLE OF CONTENTS
Last Revised – October 2025
1.0 Purpose and Scope
This chapter provides an overview of the eligibility requirements for enrolling in the World Trade Center (WTC) Health Program. It also explains how the enrollment process works and how to appeal enrollment decisions. Eligibility requirements, enrollment instructions, and applications can be found on the WTC Health Program "How to Apply" webpage.
2.0 Statutory and Regulatory References
The following sections of the James Zadroga 9/11 Health and Compensation Act of 2010, as amended (Zadroga Act),1 are applicable to this chapter:
- Section 3311 (42 U.S.C § 300mm-21), Identification of WTC Responders and Provision of WTC-Related Monitoring Services; and
- Section 3321 (42 U.S.C § 300mm-31), Identification and Initial Health Evaluation of Screening-Eligible and Certified-Eligible WTC Survivors.
Program regulations relating to eligibility and enrollment are established in the following sections of 42 C.F.R. Part 88:
- Section 88.1, Definitions;
- Section 88.3, Eligibility—currently identified2 responders;
- Section 88.4, Eligibility criteria—WTC responders;
- Section 88.5, Application process—WTC responders;
- Section 88.6, Enrollment decision—WTC responders;
- Section 88.7, Eligibility—currently identified survivors;
- Section 88.8, Eligibility criteria—WTC survivors;
- Section 88.9, Application process—WTC survivors;
- Section 88.10, Enrollment decision—screening-eligible survivors;
- Section 88.11, Initial health evaluation for screening-eligible survivors;
- Section 88.12, Enrollment decision—certified-eligible survivors;
- Section 88.13, Disenrollment;
- Section 88.14, Appeal of enrollment or disenrollment decision; and
- Section 88.25, Reopening of WTC Health Program final decisions.
3.0 Roles and Responsibilities
Responsibilities for eligibility and enrollment in the Program are distributed among various entities within the WTC Health Program. Below is a list of these entities along with a description of their specific roles concerning member eligibility and enrollment.
- Clinical Centers of Excellence (CCEs) support the enrollment of new members in the Program through outreach programs, education, and assistance with enrollment application forms. When the Program was established in 2011, CCEs provided information on responders and survivors who were enrolled in predecessor programs [the WTC Medical Monitoring and Treatment Program (MMTP) and the WTC Environmental Health Center (EHC) Community Program] to help ensure those members’ enrollment in the WTC Health Program to achieve continuity of care.
- Health Program Support (HPS)/Third-Party Administrator (TPA) Contractor receives new enrollment applications, examines the enrollment packages for completeness, and enters information in the claims processing system. If necessary, the HPS/TPA contractor may request additional information from the applicant before forwarding the application to the Program for a decision. When an application is approved, the HPS/TPA contractor notifies the applicant and sends approval notification to the Data Center (see item E below). The HPS/TPA contractor sends welcome packages to new members. The welcome package provides the member with information on their clinic assignment. For members who live outside the NY metropolitan area (NYMA), the HPS/TPA contractor sends notification to the Nationwide Provider Network (NPN) (see item F below).
- The WTC Health Program makes the final enrollment determination and is responsible for adjudicating any appeals.
- Federal Bureau of Investigation (FBI) screens Program applicants against the terrorist watch list3 and notifies the Program of applicants’ clearance.
- Data Centers (DCs) process all new members into the appropriate cohort (responder or survivor), enter their information into its database, and ensure they are assigned to the correct CCE after enrollment.
- The Nationwide Provider Network (NPN) receives weekly updates on new NPN enrollees from the HPS/TPA contractor and enters them into its system. The NPN provides new members residing outside the NYMA with information on how to access covered benefits through the NPN.
- Outreach and Education Contractors are organizations that partner with the National Institute for Occupational Safety and Health (NIOSH) through contracts to support the diverse needs of various WTC Health Program populations. These contractors provide outreach and education services on behalf of the Program, including developing and implementing approaches to raise awareness of the Program among specific underrepresented populations and assisting applicants with enrollment application forms. For more information about these contractors, please visit the WTC Health Program Outreach webpage.
4.0 Overview—Eligibility and Enrollment
The Zadroga Act identifies multiple member groups eligible to enroll in the WTC Health Program. Membership groups include:
- FDNY responders (responders from the Fire Department of New York City (FDNY) and surviving immediate family members of the 343 FDNY responders who perished on September 11, 2001);
- WTC general responders;
- WTC survivors; and
- Pentagon and Shanksville, Pennsylvania responders.
Some responders and survivors were enrolled in predecessor programs prior to the July 11, 2011, start date of the WTC Health Program. Responders who were enrolled with FDNY or the MMTP prior to July 1, 2011, and survivors who were enrolled in the EHC Community Program prior to January 2, 2011, were automatically enrolled in the WTC Health Program upon its inception (following terrorist watch list screening).
All applicants for the WTC Health Program must use the Program’s application forms. FDNY responders, WTC general responders, WTC survivors, and Pentagon and Shanksville, Pennsylvania responders each have a distinct application form that is unique to the eligibility requirements for each member group. These application forms can be found on the WTC Health Program “Application” webpage.
4.1 Applications: Completion and Submission
Information for WTC Health Program applicants, including online application forms, can be found on the WTC Health Program’s “Application” webpage. Applications can be completed online or by downloading and printing the forms to send by mail or fax. Individuals can call the WTC Health Program at 1-888-982-4748 and request that a paper application be mailed to them.
Please note that all online applicants must hand-sign, scan, and upload the WTC Health Program Online Application Signature Form for their application to be processed. The form can be found on the Program website: WTC Health Program Online Application Signature Form [PDF, 7 pages, 208 KB] .
Applicants who have questions about the application process or their individual application can contact the WTC Health Program at 1-888-982-4748 or WTC@cdc.gov. Trained customer service representatives are available to answer questions about the enrollment process. Help in languages other than English is available. Additionally, free enrollment assistance is provided by the CCE outreach teams and the Outreach and Education contractors.
Completed responder and survivor paper application forms and supporting documents must be mailed to the WTC Health Program at either of the following addresses:
WTC Enrollment
P.O. Box 7000
Rensselaer, NY 12144
OR
WTC Enrollment
327 Columbia Turnpike
Rensselaer, NY 12144
Alternatively, applications may be faxed to 1-877-646-5308.
4.1.1 Designated Representative
If desired, an applicant or enrolled member can appoint a designated representative. A designated representative is an individual appointed by an applicant, WTC responder, screening-eligible survivor, or certified-eligible survivor who is authorized to act on the applicant’s or member’s behalf and to represent their administrative interests to the WTC Health Program.4
The appointment of a designated representative must be made in writing and follow relevant federal laws and regulations. Appointment of only one designated representative per applicant or member is permitted at any given time, and a new representative can only be recognized if the previous designated representative's appointment is revoked in writing. An applicant or member may authorize any individual as their designated representative unless it violates applicable laws or is prohibited by WTC Health Program policies, procedures, or contract provisions. Federal employees can only act as representatives within the limits set by statute at 18 U.S.C. §§ 203 and 205.
A properly appointed designated representative recognized by the WTC Health Program may make requests or provide direction about eligibility, certification, administrative issues, and appeals on behalf of the applicant or member. A designated representative does not have authority to make medical decisions for a member. Any notice requirement under the Zadroga Act is fully satisfied if sent to the designated representative. If a member or applicant has an approved DR in the system, mail will be sent to both individuals.
To appoint a designated representative, an applicant or member must complete and submit both a Designated Representative form and a HIPAA Authorization for Designated Representative form. More information and the forms are available at the Program’s Designated Representative webpage or by calling 1-888-982-4748.
If an applicant or member has appointed an individual to be their healthcare proxy or assigned a healthcare power of attorney, that individual may act as the member’s designated representative. In this circumstance, a copy of the legally accepted and executed documentation granting this authority (e.g., a Power of Attorney document) must be submitted along with the Designated Representative form and the HIPAA Authorization for Designated Representative form for the selection to be reviewed and verified.
4.2 Enrollment Determination
Applications go through several stages of assessment. Upon receipt, the Program scans the enrollment form and any attachments to convert to electronic format and assigns a Document Control Number. The scanned applications are delivered to the HPS/TPA contractor via a Secure File Transport Protocol server.
The HPS/TPA contractor receives the application forms and attachments, assigns them to enrollment processors, and creates an enrollment record in the system to facilitate status tracking.
The application is reviewed by the HPS/TPA contractor for sufficient documentation. The HPS/TPA contractor contacts the applicant if more documentation is needed to process the application. When all necessary documentation is collected and entered into the system, the HPS/TPA contractor sends the application to the Program to make a final enrollment decision.
Prior to final approval of an applicant’s enrollment, the Program transmits the applicant’s information to the FBI to ensure that the applicant is not on the terrorist watch list, in compliance with the requirements of the Zadroga Act and 42 C.F.R. §§ 88.6(c)(3), 88.7, 88.10(b)(3), and 88.12. Once the enrollment record is updated with the date of the terrorist watch list screening clearance, the new member is enrolled. On a weekly basis, the HPS/TPA contractor sends the DCs a list of all new enrollees and notifies the NPN of any new NPN enrollees.
4.3 Notification to Applicants
All applicants receive notification of their membership status once a final enrollment decision is made.
When enrollment is approved, notification is made based on membership group:
- General responders who live within the NYMA receive a letter from the WTC Health Program confirming their acceptance into the Program and a postcard listing the available CCE options. General Responders may select their CCE by returning the postcard by mail or calling the Program. If they do not respond within 30 days, the Program automatically assigns the member to a responder CCE.
- FDNY responders receive a letter from the WTC Health Program confirming their acceptance into the Program and assignment to the FDNY CCE. This letter includes a phone number the member may call to initiate their health benefit services.
- Survivors who live within the NYMA receive a letter from the WTC Health Program confirming their acceptance into the Program and assignment to a survivor CCE. The letter also provides a phone number to call to initiate their health benefit services.
- Responders and survivors who live outside the NYMA receive a letter from the WTC Health Program confirming their acceptance into the Program and assignment to the NPN. The letter includes a phone number the member may call to initiate their health benefit services.
- Reasons for Denial—The letter explains why enrollment is denied, for example:
- Application or supporting documents do not meet statutory or Program policy requirements regarding time, location, activity, or exposure.
- Failure to provide adequate supporting documentation or failure to sign attestation statement affirming that all information provided is truthful.
- Right to Appeal—The letter informs applicants about their right to appeal the enrollment denial and provides instructions on how to file an appeal.
When enrollment is denied, applicants receive a notification letter that includes:
4.4 Disenrollment
The Program may disenroll a member if the member was mistakenly enrolled or the enrollment was based on incorrect or fraudulent information. Sections 6 and 7 below provide more detail on enrollment and disenrollment, respectively.
Both enrollment denials and disenrollments can be appealed to the Administrator. Information about the appeal process is found in Section 8 below.
5.0 Eligibility Groups
Eligibility criteria for the WTC Health Program are defined by the Zadroga Act, Secs. 3311 and 3321 (42 U.S.C. §§ 300mm-21 and 300mm-31) and found in 42 C.F.R. Part 88. These criteria are summarized below.
5.1 FDNY Responders
Program eligibility for this cohort of responders is defined by the Zadroga Act, Secs. 3311(a)(1)(A) and 3311(a)(2)(A) (42 U.S.C. §§ 300mm-21(a)(1)(A) and 300mm-21(a)(2)(A)) and found at 42 C.F.R. §§ 88.3 or 88.4(a)(1). Eligibility is limited by inclusion on the terrorist watch list. Eligibility criteria are described below.
- A member of the FDNY (whether fire or emergency personnel, active or retired) who participated at least one day in the rescue and recovery effort at any of the former World Trade Center sites (including Ground Zero, the Staten Island Landfill, or the NYC Chief Medical Examiner’s Office), during the period beginning on September 11, 2001, and ending on July 31, 2002; or
- A surviving immediate family member 5 of an individual who was an active or retired member of the FDNY (whether firefighter or emergency personnel) who was killed at the World Trade Center site on September 11, 2001, and received any treatment for a WTC-related mental health condition on or before September 1, 2008.
FDNY responders who were identified as eligible for monitoring and treatment under the arrangements in effect on January 2, 2011, between NIOSH and the MMTP or FDNY were enrolled in the WTC Health Program upon its establishment in July 2011, without being required to submit a new application (subject to terrorist watch list screening).
5.2 WTC General Responders
Eligibility criteria for WTC general responders are defined by the Zadroga Act, Secs. 3311(a)(1) and 3311(a)(2)(B) (42 U.S.C. §§ 300mm-21(a)(1) and 300mm-21(a)(2)(B)) and 42 C.F.R. §§ 88.3 and 88.4. Eligibility is limited by the number of responders already enrolled in the Program6 and by inclusion on the terrorist watch list. Eligibility criteria are summarized below.
Responders may apply for enrollment in the WTC Health Program if they meet the criteria in one of the following categories:
- Law enforcement officers and WTC rescue, recovery, and cleanup workers:
-
The individual worked or volunteered onsite in rescue, recovery, debris cleanup, or related support services in lower Manhattan (south of Canal Street), the Staten Island Landfill, or the barge loading piers, for at least:
- Four hours during the period beginning on September 11, 2001, and ending on September 14, 2001; or
- Twenty-four hours during the period beginning on September 11, 2001, and ending on September 30, 2001; or
- Eighty hours during the period beginning on September 11, 2001, and ending on July 31, 2002.
-
The individual was an active or retired member of the NYC Police Department or an active or retired member of the Port Authority Police of the Port Authority of New York and New Jersey who participated onsite in rescue, recovery, debris cleanup, or related support services, for at least:
- Four hours during the period beginning September 11, 2001, and ending on September 14, 2001, in lower Manhattan (south of Canal Street), including Ground Zero, the Staten Island Landfill, or the barge loading piers; or
- One day during the period beginning on September 11, 2001, and ending on July 31, 2002, at Ground Zero, the Staten Island Landfill, or the barge loading piers; or
- Twenty-four hours during the period beginning on September 11, 2001, and ending on September 30, 2001, in lower Manhattan (south of Canal Street); or
- Eighty hours during the period beginning on September 11, 2001, and ending on July 31, 2002, in lower Manhattan (south of Canal Street).
-
The individual worked or volunteered onsite in rescue, recovery, debris cleanup, or related support services in lower Manhattan (south of Canal Street), the Staten Island Landfill, or the barge loading piers, for at least:
- Office of the Chief Medical Examiner of NYC employee: The individual was an employee of the Office of the Chief Medical Examiner of NYC involved in the examination and handling of human remains from the WTC attacks, or other morgue worker who performed similar post-September 11 functions for such Office staff, during the period beginning on September 11, 2001, and ending on July 31, 2002.
- Port Authority Trans-Hudson Corporation Tunnel worker: The individual was a worker in the Port Authority Trans-Hudson Corporation Tunnel for at least 24 hours during the period beginning on February 1, 2002, and ending on July 1, 2002.
- Vehicle-maintenance worker: The individual was a vehicle-maintenance worker who was exposed to debris from the former WTC while retrieving, driving, cleaning, repairing, and maintaining vehicles contaminated by airborne toxins from the September 11, 2001, terrorist attacks; and conducted such work for at least one day during the period beginning on September 11, 2001, and ending on July 31, 2002.
Responders who were identified as eligible for monitoring and treatment under the arrangements in effect on January 2, 2011, between NIOSH and the MMTP (a predecessor program) were enrolled in the WTC Health Program upon its establishment in July 2011, without being required to submit a new application (subject to terrorist watch list screening).
5.3 Pentagon and Shanksville, Pennsylvania Responders
Eligibility criteria for Pentagon responders are defined by the Zadroga Act, Sec. 3311(a)(2)(C) (42 U.S.C. § 300mm-21(a)(2)(C)) and 42 C.F.R. § 88.4(b) and for Shanksville, Pennsylvania responders at Zadroga Act, Sec. 3311(a)(2)(C) (42 U.S.C. § 300mm-21(a)(2)(C)) and 42 C.F.R. § 88.4(c). Eligibility is limited by the number of responders already enrolled in the Program7 and by inclusion on the terrorist watch list. The criteria are summarized below.
Pentagon responders:
Individuals who responded to the Pentagon site must meet each of the three criteria below to be considered eligible for enrollment:
- The individual was one of the following:
- An active or retired member of a fire or police department (fire or emergency personnel);
- Worked for a recovery or cleanup contractor;
- A volunteer;
- An employee of the Department of Defense or any other Federal agency;
- Worked for a contractor of the Department of Defense or any other Federal agency during the period beginning on September 11, 2001, and ending on September 18, 2001; or
- A member of a regular or reserve component of the uniformed services.
- The individual performed rescue, recovery, demolition, debris cleanup, or other related services at the Pentagon site of the September 11, 2001, terrorist attacks; and
- The individual performed the activities listed in item B for at least one day beginning September 11, 2001, and ending on November 19, 2001.
Shanksville, Pennsylvania responders:
Individuals who responded to the Shanksville, Pennsylvania site must meet each of the three criteria below to be considered eligible for enrollment:
-
The individual was one of the following:
- An active or retired member of a fire or police department (fire or emergency personnel);
- Worked for a recovery or cleanup contractor;
- A volunteer;
- An employee of the Department of Defense or any other Federal agency;
- Worked for a contractor of the Department of Defense or any other Federal agency during the period beginning on September 11, 2001, and ending on September 18, 2001; or
- A member of a regular or reserve component of the uniformed services;
- The individual performed rescue, recovery, demolition, debris cleanup, or other related services at the Shanksville, Pennsylvania site of the September 11, 2001, terrorist attacks; and
- The individual performed the activities described in item B for at least one day beginning September 11, 2001, and ending on October 3, 2001.
5.4 WTC Survivors
WTC survivors are those who lived, worked, went to school, or attended child or adult day care in the NYC Disaster Area on September 11, 2001, or in the days, weeks, or months after, including those who were present in the dust or dust cloud within the NYC Disaster Area on that date. The NYC Disaster Area is the area of Manhattan south of Houston Street and any block in Brooklyn wholly or partially contained within a 1.5-mile radius of the former WTC site.8 A map of the NYC Disaster Area can be found on the Program's website. The Zadroga Act establishes eligibility criteria for two groups of survivors: screening-eligible survivors9 and certified-eligible survivors.10 Eligibility is limited by the number of certified-eligible survivors already enrolled in the program11 and by inclusion on the terrorist watch list.
5.4.1 Criteria for Status as a Screening-Eligible Survivor
Screening-eligible survivors are those individuals who meet the WTC survivor eligibility criteria and claim symptoms of a WTC-related health condition. Upon enrollment in the Program, a screening-eligible survivor is eligible for a one-time initial health evaluation paid for by the Program. WTC Survivors may apply for enrollment in the WTC Health Program as a screening-eligible survivor if they meet the criteria in one of the following categories:
- The screening applicant was present in the dust or dust cloud in the NYC disaster area on September 11, 2001;
-
The screening applicant worked, resided, or attended school, childcare, or adult daycare in the NYC disaster area, for at least:
- Four days during the 4-month period beginning on September 11, 2001, and ending on January 10, 2002; or
- Thirty days during the period beginning on September 11, 2001, and ending on July 31, 2002;
- The screening applicant worked as a cleanup worker or performed maintenance work in the NYC disaster area during the 4-month period beginning on September 11, 2001, and ending on January 10, 2002, and had extensive exposure to WTC dust as a result of such work;
-
The screening applicant:
- Was deemed eligible to receive a grant from the Lower Manhattan Development Corporation Residential Grant Program;
- Possessed a lease for a residence or purchased a residence in the NYC disaster area; and
- Resided in such residence during the period beginning on September 11, 2001, and ending on May 31, 2003; or
-
The screening applicant is an individual whose place of employment:
- At any time during the period beginning on September 11, 2001, and ending on May 31, 2003, was in the NYC disaster area; and
- Was deemed eligible to receive a grant from the Lower Manhattan Development Corporation WTC Small Firms Attraction and Retention Act Program or other government incentive programs designed to revitalize the lower Manhattan economy after the September 11, 2001, terrorist attacks.
5.4.2 Criteria for Status as a Certified-Eligible Survivor
Certified-eligible survivors survivors are screening-eligible survivors who have a certified WTC-related health condition(s). Certified-eligible survivors are eligible for annual monitoring exams and treatment for certified WTC-related and medically associated health condition(s). Status as a certified-eligible survivor is based on a certification by the WTC Health Program that, pursuant to an initial health evaluation,12 the screening-eligible survivor has a WTC-related health condition and is eligible for follow-up monitoring and treatment.
Survivors who were identified as eligible for medical treatment and monitoring within the WTC EHC Community Program as of January 2, 2011, were considered certified-eligible upon establishment of the WTC Health Program and were not required to submit a new application (subject to terrorist watch list screening).13
6.0 Enrollment
6.1 Acknowledgment
The HPS/TPA enrollment processors send a letter to each applicant acknowledging receipt of their application. There are two types of acknowledgment letters:
- Acknowledgment of Receipt of Application: This letter is sent when the information included on the application appears to be complete and no further information is needed by the enrollment processor to process the application.
- Acknowledgment of Receipt + Information Needed: This letter is sent when the enrollment processor needs additional information to process the application. The letter explains what information is needed and provides instructions on how to submit the additional information. When the additional information is received, the enrollment processor resumes processing of the application.
6.2 Application Processing and Evaluation
The HPS/TPA enrollment processors review all enrollment information received, including the information provided in the enrollment application and any supporting documentation included in the enrollment record, such as documentation that verifies presence at the site. This information is evaluated following the guidance, protocols, and procedures of the WTC Health Program to summarize the applicant’s experience on and after September 11, 2001. Factors considered in the enrollment process include:
- Presence at a covered location;
- Presence during the eligible days, weeks, or months;
- Presence for minimum hour requirements;
- For survivor applicants, symptoms of a WTC-related health condition; and
- For responder applicants, work duties performed.
The enrollment processor’s evaluation and enrollment recommendation reflects the processor’s assessment of whether eligibility criteria is met and serves to orient the Program enrollment reviewer to the contents of the application. The enrollment processor makes one of the following recommendations:
- Enroll: Applicant is eligible for enrollment.
- Deny: Applicant is not eligible for enrollment.
- Defer: Survivor applicant meets eligibility criteria but does not claim symptoms of a WTC-related health condition in application.
- Recategorize: Applicant’s experiences on or after September 11, 2001, are more appropriately captured by a different member type than the one they applied for (e.g., the individual applied as a responder but meets the survivor eligibility criteria instead of the responder eligibility criteria and therefore should be enrolled as a survivor).
- Administrative Closure: A decision on enrollment eligibility is not required because the application process is ending for administrative reasons, typically due to the applicant withdrawing their application or upon the death of the applicant.
- Duplicate: Multiple applications were submitted for the same individual. A decision on enrollment eligibility is unnecessary because it has been or will be assessed through a separate application package.
The enrollment record and the processor’s evaluation and recommendation are sent to Program enrollment reviewers for a final enrollment decision.
6.3 Program Administrator's Determination
The Program makes one of two enrollment determinations for each applicant:
- Enroll: Sufficient evidence exists that the applicant meets Program eligibility criteria and can be enrolled. This includes recategorization (see Section 6.2 above) and reclassification decisions (see below).
- Deny: Sufficient evidence exists that the applicant does not meet one or more of the eligibility criteria established in the Zadroga Act and cannot be enrolled. Denied applications can be appealed; appeals must be submitted within 120 days of denial to be considered (see Section 8).
- Reconsideration: A denied applicant may reapply or provide new documentation for review at any time after the Program’s decision to deny enrollment. If the new information is qualifying, the initial decision is reopened and a new “Enroll” decision can be made.
- Classification Review Request: An enrolled member may request a review of their classification as a responder or survivor, typically supported by new documentation and additional details or context surrounding their experience. If the Program agrees that the member’s experiences on or after September 11, 2001 more accurately reflect a different membership group (as described above in Section 4.3) than the group in which they were enrolled, the Program will reclassify the member (e.g., survivor member meets responder eligibility criteria and therefore is reclassified to a responder).
If an application is incomplete or does not provide sufficient evidence that the applicant meets Program eligibility criteria, the application is placed in “Suspend” status. Suspended applications are sent back to the HPS/TPA enrollment processor to obtain additional information from the applicant (See Section 6.4.).
In some cases, the Program may reopen and review an application record after the initial decision:
6.4 Notification to Applicants
There are circumstances when an application cannot be enrolled or denied, as described in Section 4.3. In those instances, the Program notifies the applicant of the status of their application with the appropriate letter sent by the HPS/TPA contractor, as follows:
- Defer: If sufficient evidence exists that an individual who applied as a survivor—or who may be classified as a survivor—meets all Program eligibility criteria except for the requirement to claim symptoms of a WTC-related health condition, the applicant will receive a letter explaining their application is deferred. The letter further explains how the application process can be resumed when the applicant claims symptoms of a WTC-related health condition.
- Suspend: If an application is incomplete or has insufficient documentation, the applicant will receive a letter explaining why their application has been suspended and what is needed to resume the application process.
- Inactive: When an applicant fails to respond to multiple “Suspend” letters for 90 consecutive days, they are informed that their application is still on file but has been marked as “Inactive.” Following this notification, an annual reminder letter is sent to the applicant, which includes contact information for the Program to facilitate re-engagement in the application process.
7.0 Disenrollment
7.1 WTC Health Program Disenrollment Decision
The WTC Health Program has the authority to disenroll a member, as outlined in 42 C.F.R. § 88.13, under the following circumstances:
- Mistaken Enrollment—If an individual was mistakenly enrolled without providing sufficient documentation that aligns with the required eligibility criteria.
- Incorrect or Fraudulent Information—If a member’s enrollment in the WTC Health Program was based on incorrect or fraudulent information.
7.2 Notification to Disenrolled Member
A disenrolled WTC Health Program member receives a written notification from the Administrator explaining the disenrollment decision, any resulting administrative actions, and the effective date of the disenrollment. The letter also informs the disenrolled member about their right to appeal the disenrollment decision and provides instructions on how to file an appeal.
8.0 Appeal of Enrollment Denial or Disenrollment Decision
All applicants have the right to appeal an enrollment denial or disenrollment decision, as outlined in 42 C.F.R. § 88.14.
8.1 Appeal Requests
An appeal request meeting the following requirements must be sent to the Program within 120 calendar days from the date of the notification letter issued by the Administrator:
- The appeal request must identify the denied applicant or disenrolled member, along with their designated representative (if applicable). For details on appointing a designated representative, refer to Section 4.1.1.
- The appeal request should outline the specific decision being appealed and provide reasons why the denial or disenrollment is incorrect and should be overturned. The appeal request may also include relevant new information not previously considered by the WTC Health Program.
- The appeal request must be submitted in writing and signed.
- Send the appeal request via mail or fax to the address or fax number specified in the notice of denial or disenrollment.
Any appeal that solely challenges existing laws, regulations, or Program policies will be deemed invalid and outside the scope of the administrative appeal process; those matters can only be changed through broader legal actions. Regulations or policies set forth by the Administrator apply universally to all Program applicants and/or members and therefore cannot be challenged through an individual appeal.
Any concerns about Program policies or requests for changes to Program regulations can be directed to the Administrator in writing. This process is separate from individual appeals. Changes to the Zadroga Act require congressional action.
An appeal may, however, challenge how the Program has applied the eligibility criteria established by law or regulation. For example, an appeal could argue that the Program incorrectly determined the number of hours the individual worked or volunteered during a covered period.
8.1.1 Submitting an Appeal Request
Appeal requests (along with required forms to request a designated representative, if any) must be sent via mail or fax to the Appeal Coordinator at:
Appeal Coordinator
WTC Health Program
P.O. Box 7000
Rensselaer, NY 12144
OR
Appeal Coordinator
WTC Health Program
327 Columbia Turnpike
Rensselaer, NY 12144
Fax: 1-877-646-5308
8.2 Review by Federal Official
In compliance with the Program regulations, the Administrator appoints a Federal Official to review appeal requests and provide a recommendation to the Administrator. This Federal Official operates independently of the WTC Health Program and does not participate in enrollment, eligibility, or disenrollment decisions; their sole responsibility is to review appeals. This ensures each appeal receives an objective and impartial third-party evaluation of the facts.
8.3 Appeal Procedure
The appeal procedure consists of the following steps:
- A denied applicant or disenrolled member submits an appeal request following the steps detailed in Section 8.1.
- The WTC Health Program Appeal Coordinator reviews the appeal of enrollment denial or disenrollment and determines its validity (i.e., the request meets all of the requirements in Section 8.1, above). Valid appeals are sent to the appointed Federal Official for review and recommendation.
- The Federal Official conducts a comprehensive review of all available records, including any relevant new information submitted, and assesses whether the appeal should be granted. After careful review, the Federal Official provides a recommendation regarding the outcome of the appeal to the Administrator.
- After reviewing the appeal file and recommendation from the Federal Official, the Administrator makes a final decision on the appeal.
- The applicant or member receives a letter from the Program detailing the appeal’s outcome and any actions taken by the WTC Health Program based on that decision.
- In accordance with 42 C.F.R. § 88.25, the Administrator has the authority to reopen a final determination at any time and may affirm, vacate, or modify decisions as deemed appropriate.
For more information about appeals of enrollment denials or disenrollments, see the WTC Health Program’s “Appeals” webpage.
Chapter 3—Certification of Health Conditions
TABLE OF CONTENTS
Last Revised – August, 2025
- Purpose and Scope
- Statutory and Regulatory References
- Responsibilities
- Covered Conditions
- CCE/NPN Physician Determination and Request for Certification of Health Conditions
- Overview of the Certification Process
- Authorization of Treatment Pending Certification
- Certification Decisions
- Linking Member Health Benefits to Certified Health Conditions
- Appeals of Certification Denials and/or Decertifications
-
Appendices
Appendix 3-A WTC-3 Form
Appendix 3-B WTC-3 Instructions for Cancer
Appendix 3-E Making a Determination about Exposure Aggravating Pre-Existing Aerodigestive Disorders
Appendix 3-F Time Intervals for New Onset Aerodigestive Disorders
Appendix 3-G Policy and Procedures for Certification of Physician Determinations for Aerodigestive and Cancer Health Conditions
Appendix 3-H Minimum Latency & Types or Categories of Cancer
Appendix 3-I Malignant Neuroendocrine Neoplasms
Appendix 3-J Myeloid Malignancies
Appendix 3-K Rare Cancers
Appendix 3-L Policy and Procedures for Handling Submissions and Petitions to Add a Health Condition to the List of WTC-Related Health Conditions
Appendix 3-M Policy and Procedures for Adding Non-Cancer Conditions To the List of WTC-Related Health Conditions
Appendix 3-N Policy and Procedures for Adding Types of Cancer To the List of WTC-Related Health Conditions
1. Purpose and Scope
The purpose of this chapter is to describe the circumstances in which a health condition may be certified under Title XXXIII of the PHS Act, the certification process, responsibilities in the certification process, conditions that may be certified, communications regarding certifications, and appeals of certification decisions. Further detail on the certification process is provided in the WTC Health Program Member Services Operations Manual, found in the Program’s file of record.
2. Statutory and Regulatory References
The following sections of Title XXXIII of the PHS Act are applicable to this Chapter:
-
Section 3312(a)(1)(A) defines a WTC-related health condition as:
- “[A]n illness or health condition for which exposure to airborne toxins, any other hazard, or any other adverse condition resulting from the September 11, 2001, terrorist attacks, based on an examination by a medical professional with experience in treating or diagnosing the health conditions included in the applicable list of WTC-related health conditions, is substantially likely to be a significant factor in aggravating, contributing to, or causing the illness or health condition…;” or
- “[A] mental health condition for which such attacks, based on an examination by a medical professional with experience in treating or diagnosing the health conditions included in the applicable list of WTC-related health conditions, is substantially likely to be a significant factor in aggravating, contributing to, or causing the condition….”
- Section 3312(b)(1) states that if a physician at a Clinical Center of Excellence (CCE) makes a determination that a WTC responder has a WTC-related health condition included in the List of WTC-Related Health Conditions (List) and that exposure to airborne toxins, other hazards, or adverse conditions resulting from the September 11, 2001, terrorist attacks is substantially likely to be a significant factor in aggravating, contributing to, or causing the condition, then the physician is to transmit that determination and the medical facts supporting the determination to the WTC Health Program. After review of the CCE physician’s determination, the WTC Health Program will certify the health condition if he finds that it is on the List of WTC-Related Health Conditions and that exposure to airborne toxins, other hazards, or adverse conditions resulting from the September 11, 2001, terrorist attacks is substantially likely to be a significant factor in aggravating, contributing to, or causing the health condition. The WTC Health Program will pay for medically necessary treatment of certified WTC-related health conditions (see § 3312(c)(1)). In addition, the Administrator must establish a process to appeal certification decisions.
- Section 3312(b)(5) authorizes treatment pending certification for responders, and section 3322(a) extends the same benefits to survivors.
- Section 3321(a)(2)(B) requires the Administrator of the WTC Health Program to establish a certification process for screening-eligible WTC survivors who are eligible for further monitoring and treatment after their initial screening exam.
The following provisions in the WTC Health Program regulations in 42 C.F.R. Part 88 are also applicable to this Chapter:
- Section 88.1 includes definitions of the following relevant terms: Aggravating, Certification; Health condition medically associated with a WTC-related health condition; List of WTC-Related Health Conditions; Medically necessary treatment; WTC-related acute traumatic injury; WTC-related health condition; and WTC-related musculoskeletal disorder.
- Section 88.15, List of WTC-Related Health Conditions.
- Section 88.16, Addition of health conditions to the List of WTC-Related Health Conditions.
- Section 88.17, Physician’s determination of WTC-related health conditions.
- Section 88.18, Certification.
- Section 88.19, Decertification.
- Section 88.20, Authorization of treatment.
- Section 88.21, Appeal of certification, decertification, or treatment authorization decision.
- Section 88.25, Reopening of WTC Health Program final decisions.
3. Responsibilities
The parties involved in certifying health conditions and their responsibilities are detailed below.
- The Clinical Centers of Excellence/Nationwide Provider Network (CCEs)/(NPN) provide monitoring and screening examinations for eligible responders and survivors. The CCE/NPN ensures that requests for certification of a member’s health condition are completed using the appropriate forms and procedures. The CCE/NPN transmits the completed health condition certification request in a secure manner to the Program’s Health Program Support (HPS) contractor for processing (see Section 6, below for more information regarding secure data transfer). The WTC Health Program’s certification decision is sent to the member and CCE/NPN via letter. Upon receipt of a decision by the Program to certify a health condition, the CCE/NPN is authorized to provide medically necessary treatment to the member for that condition and shall be responsible for providing adequate treatment services or referrals, which will be scheduled by the CCE/NPN.
- The Program’s Medical Benefit Manager (MBM) has been designated by the Administrator to determine whether a health condition meets the requirements for certification. The MBM reviews an official request by the CCE/NPN to certify a member’s health condition for treatment to be covered by the Program and leads the Certification Team that conducts this function. The MBM consults with the Administrator regarding certifications as necessary.
- The Program’s HPS contractor is responsible for receiving and processing certification requests from the CCE/NPN for the Program’s Certification Team to evaluate. The HPS contractor also receives the Program’s decisions, updates the system of records, and supports the communication process with the CCE/NPN and member.
4. Covered Conditions
-
The following WTC-related health conditions covered by the WTC Health Program are established in 42 C.F.R. § 88.15:
-
Aerodigestive disorders:
- Interstitial lung diseases;
- Chronic respiratory disorders – fumes/vapors;
- Asthma;
- Reactive airways dysfunction syndrome (RADS);
- WTC-exacerbated or new-onset chronic obstructive pulmonary disease (COPD);
- Chronic cough syndrome;
- Upper airway hyperreactivity;
- Chronic rhinosinusitis;
- Chronic nasopharyngitis;
- Chronic laryngitis;
- Gastroesophageal reflux disorder (GERD);
- Sleep apnea exacerbated by or related to a condition described in i-xii.
-
Mental Health Conditions:
- Posttraumatic stress disorder (PTSD);
- Major depressive disorder;
- Panic disorder;
- Generalized anxiety disorder;
- Anxiety disorder (not otherwise specified);
- Depression (not otherwise specified);
- Acute stress disorder;
- Dysthymic disorder;
- Adjustment disorder;
- Substance abuse.
-
Musculoskeletal Disorders (only for WTC responders to the New York City disaster area)::
- Low back pain;
- Carpal tunnel syndrome(CTS);
- Other musculoskeletal disorders.
-
Cancers
:
- Malignant neoplasms of the lip, tongue, salivary gland, floor of mouth, gum and other mouth, tonsil, oropharynx, hypopharynx, and other oral cavity and pharynx.
- Malignant neoplasm of the nasopharynx.
- Malignant neoplasms of the nose, nasal cavity, middle ear, and accessory sinuses.
- Malignant neoplasm of the larynx.
- Malignant neoplasm of the esophagus.
- Malignant neoplasm of the stomach.
- Malignant neoplasm of the colon and rectum.
- Malignant neoplasm of the liver and intrahepatic bile duct.
- Malignant neoplasms of the retroperitoneum and peritoneum, omentum, and mesentery.
- Malignant neoplasms of the trachea; bronchus and lung; heart, mediastinum and pleura; and other ill-defined sites in the respiratory system and intrathoracic organs.
- Mesothelioma.
- Malignant neoplasms of the peripheral nerves and autonomic nervous system, and other connective and soft tissue.
- Malignant neoplasms of the skin (melanoma and non-melanoma), including scrotal cancer.
- Malignant neoplasm of the female breast.
- Malignant neoplasms of the corpus uteri and uterus, part unspecified.
- Malignant neoplasm of the prostate.
- Malignant neoplasm of the urinary bladder.
- Malignant neoplasm of the kidney.
- Malignant neoplasms of the renal pelvis, ureter and other urinary organs.
- Malignant neoplasms of the eye and orbit.
- Malignant neoplasm of the thyroid.
- Malignant neoplasms of the blood and lymphoid tissues (including, but not limited to, lymphoma, leukemia, and myeloma).
- Childhood cancers: Any type of cancer diagnosed in a person less than 20 years of age.
- Rare cancers: any type of cancer that occurs in less than 15 cases per 100,000 persons per year in the United States (based on 2005–2009 average annual data age-adjusted to the 2000 U.S. population).
-
Acute Traumatic injuries:
- Eye injury.
- Burn.
- Head trauma.
- Fracture.
- Tendon tear.
- Complex sprain.
- Other similar acute traumatic injuries.
-
Aerodigestive disorders:
-
Special Note on Malignancy for Cancers
-
Solid Neoplasms
-
To qualify as a malignant neoplasm, a solid neoplasm must:
- Have been diagnosed after September 11, 2001 and meet the WTC Health Program’s minimum latency criteria for the specific cancer see Minimum Latency & Types or Categories of Cancer); [12 pages, 517 KB] and
- Be characterized histopathologically as malignant and “invasive,” i.e., having evidence of growth or spread beyond the layer of tissue in which it first developed or in which it was first diagnosed.
-
To qualify as a malignant neoplasm, non-invasive neoplasms including carcinomas in situ must:
- Have been diagnosed after September 11, 2001 and meet the WTC Health Program’s minimum latency criteria for the specific cancer.
- Be characterized histologically as malignant and be regarded in the peer-reviewed scientific literature as having an increased risk of developing into an invasive neoplasm. Non-invasive neoplasms, including carcinomas in situ, will be evaluated on a case-by-case basis. The review will include consideration of the treatment recommendations made by the National Comprehensive Cancer Network (NCCN). Such reviews will be documented and included in the member file where relevant to a specific cancer certification evaluation.
-
Non-invasive neoplasms ineligible for certification:
-
A non-invasive neoplasm that is completely removed surgically during an excisional biopsy or resection of an organ or body part containing the lesion may be curative (i.e., NCCN Guidelines recommend no further treatment). The following carcinomas in situ have been determined to be examples of such types of non-invasive neoplasms and are, therefore, ineligible for certification:
- Breast: Lobular carcinoma in situ (CIS) [except pleomorphic lobular CIS]
- Colon and rectum: CIS [including high grade intraepithelial and intramucosal neoplasia]
- Gallbladder: CIS
-
Non-invasive neoplasms of the cervix uteri are ineligible for certification but may be eligible for medical benefits related to surveillance, management, and/or treatment. The following lesions have been determined to be examples of such types of non-invasive neoplasms and are, therefore, ineligible for certification:
- Cervical intraepithelial neoplasia (CIN): CIN grade I, CIN grade II, and CIN grade III
- Carcinoma in situ of the cervix uteri
-
A non-invasive neoplasm that is completely removed surgically during an excisional biopsy or resection of an organ or body part containing the lesion may be curative (i.e., NCCN Guidelines recommend no further treatment). The following carcinomas in situ have been determined to be examples of such types of non-invasive neoplasms and are, therefore, ineligible for certification:
- Histologically benign neoplasms are ineligible for certification.
-
To qualify as a malignant neoplasm, a solid neoplasm must:
-
Liquid neoplasms
To qualify as a malignant neoplasm, a liquid neoplasm must:- Have been diagnosed after September 11, 2001 and meet the WTC Health Program’s minimum latency criteria for the specific cancer see Minimum Latency & Types or Categories of Cancer); [12 pages, 517 KB] and
- Exhibit uncontrolled clonal growth of a specific type of hematopoietic cell.
-
Cancers of Unknown Primary Origin (CUPs)
These are histologically-proven, metastatic, malignant neoplasms the primary origin of which cannot be identified during pre-treatment evaluation. The date of diagnosis of the metastatic disease will be used to evaluate eligibility for certification of CUPs.
-
Metastasis or recurrence of a pre-existing malignant neoplasm
For malignant neoplasms diagnosed before September 11, 2001, and those diagnosed after September 11, 2001 but with insufficient latency, any recurrence or metastasis from such malignant neoplasms will not be considered for certification regardless of the amount of time that passes between remission of the pre-existing neoplasm and its recurrence or metastatic spread. An exhaustive search of the scientific literature has failed to identify evidence that toxic exposures aggravate, cause, or contribute to a pre-existing cancer resulting in a recurrence or metastasis that requires a change in treatment.
-
Second primary cancers
A second primary cancer is a histologically-proven, new primary malignant neoplasm developing in a person with a history of cancer. The term applies to malignant neoplasms that have arisen independently and not as a result of recurrence or metastasis of the original primary malignant neoplasm. A second primary cancer is considered eligible for certification if it was diagnosed after September 11, 2001 and meets the WTC Health Program’s minimum latency criteria for the specific cancer. Alleged cases of second primary cancers originating from the same tissue and/or of the same histological type as a malignant neoplasm that is certified, certifiable, or ineligible for certification will be evaluated on a case-by-case basis. The review will include consideration of the peer-reviewed scientific literature and Surveillance, Epidemiology, and End Results (SEER) Program Multiple Primary and Histology Coding Rules. Such reviews will be documented and included in the member file where relevant to a specific cancer certification evaluation.
-
Solid Neoplasms
-
Special Note on Documentation of Symptoms, Diagnosis, and/or Treatment of ATIs, MSDs, and Aerodigestive Disorders
-
Acute Traumatic Injuries
A WTC-related acute traumatic injury (ATI) is physical damage to the body caused by and occurring immediately after a one-time exposure to energy, such as heat, electricity, or impact from a crash or fall, resulting from a specific event or incident. Such health conditions include eye injuries, burns, head trauma, fractures, tendon tears, complex sprains, and other similar acute traumatic injuries.
In order for an ATI to be certified by the Program, the injury must be directly related to a member’s 9/11 exposures and activities and must have occurred during one of the following time periods: September 11, 2001 – July 31, 2002 for acute traumatic injuries occurring at one of the New York City Area Sites; September 11, 2001 – November 19, 2001 for acute traumatic injuries occurring at the Pentagon Site; or September 11, 2001 – October 3, 2001 for acute traumatic injuries occurring at the Shanksville, Pennsylvania Site. In addition, the WTC responder or screening-eligible or certified-eligible survivor must have received medical treatment for the acute traumatic injury on or before September 11, 2003. -
Musculoskeletal Disorders
A WTC-related musculoskeletal disorder (MSD) is a chronic or recurrent disorder of the musculoskeletal system caused by heavy lifting or repetitive strain on the joints or musculoskeletal system occurring during rescue or recovery efforts in the New York City disaster area in the aftermath of the September 11, 2001, terrorist attacks. Such health conditions include low back pain, carpal tunnel syndrome (CTS), and other musculoskeletal disorders.
In order for an MSD to be certified by the Program, the injury must be directly related to a member’s 9/11 exposures and activities and must have occurred during the following time period: September 11, 2001 – July 31, 2002. The Zadroga Act only allows coverage of MSDs for WTC Responders; therefore, Survivors and Pentagon and Shanksville, PA Responders cannot be certified for an MSD. In addition, the WTC responder must have received medical treatment for a WTC-related musculoskeletal disorder on or before September 11, 2003. -
Aerodigestive Disorders
To certify a WTC-related aerodigestive disorder through the Program, the disorder must be directly related to a member’s 9/11 exposures. To certify some WTC-related aerodigestive disorders, the member’s condition must have begun (or was aggravated) after their initial 9/11 exposure but within a specific timeframe after those exposures ended. This timeframe is known as the maximum time interval (MTI). The WTC-related aerodigestive disorders for which MTIs pertain are referred to as “MTI-restricted.” A list of these MTI-restricted aerodigestive disorders and their corresponding MTIs can be found in the Program Policy and Procedure document titled “Time Intervals for New-Onset Aerodigestive Disorders [PDF, 15 pages, 342 KB] .”
Certification requests for MTI-restricted aerodigestive disorders can be submitted to the WTC Health Program by the CCEs/NPN for a decision when at least one of the following documentation requirements is met:
The member provides the CCE/NPN with medical records from a provider that documents the diagnosis of the MTI-restricted aerodigestive disorder or related symptoms, including dates. These medical records must show that the new MTI-restricted aerodigestive disorder or related symptoms began after the member’s initial 9/11 exposure but before the MTI for that aerodigestive disorder ended. If the condition or symptoms were present before 9/11, the medical records must document that symptoms were aggravated by the member’s 9/11 exposures within the same timeframe (after their initial 9/11 exposure but before the MTI ended). The dates these medical records were created must be contemporaneous with the symptoms or diagnosis.
If contemporaneous medical records are unavailable, the member may provide the CCE/NPN with a signed letter from their current treating physician (or from their most recent treating physician if the aerodigestive disorder no longer requires treatment) that confirms that the member’s condition or symptoms began (or were aggravated) after their initial 9/11 exposure but before the MTI for that aerodigestive disorder ended. The letter must explain how the treating physician determined the date of the condition/symptom onset/aggravation. Additionally, the letter must state how long the member has been under the physician’s care and explain why the original medical records from that time period are not available.
Furthermore, if the condition or symptoms were present before 9/11, the treating physician must document that there was an aggravation of the condition/symptoms after the member’s initial 9/11 exposure but before the MTI for their aerodigestive disorder ended. The letter must clearly explain any changes in medical treatment that resulted from the 9/11 exposure and document that such changes were initiated after the member’s initial 9/11 exposure and before the MTI for their aerodigestive disorder ended (e.g., the member received medical treatment that was in addition to, more frequent than, and/or of longer duration than the medical treatment that was provided before the member’s 9/11 exposure); the letter must also explain whether those changes in medical treatment were a result of any expected progression of the aerodigestive disorder which may have occurred in the absence of the member’s 9/11 exposure. As noted in Time Intervals for New-Onset Aerodigestive Disorders [PDF, 15 pages, 342 KB] , aggravation of an aerodigestive disorder is governed by the same time intervals as any new-onset aerodigestive disorder.
-
If the documentation described in sections 4.C.3.a. or 4.C.3.b. is unavailable, then the records from the initial monitoring exam (IME) for responders or initial health evaluation (IHE) for survivors must document that at the time of the IME/IHE, the member either had the MTI-restricted aerodigestive disorder or related symptoms or previously had the disorder or symptoms with subsequent resolution. These records must specify that the condition or symptoms began or were aggravated between the date of the member’s initial 9/11 exposure and the expiration of the MTI for their aerodigestive disorder. If the IME/IHE occurred more than two years after the MTI ended, the CCE/NPN must describe on the WTC-3 form their efforts to obtain the documents specified in sections 4.C.3.a. and 4.C.3.b. and explain why those efforts failed.
If the documentation described in sections 4.C.3.a., 4.C.3.b., and 4.C.3.c. cannot be provided, but the member had more than one monitoring exam prior to the expiration of the MTI for their aerodigestive disorder, at least one of those monitoring exams must document the onset or aggravation of the aerodigestive disorder or symptoms that occurred between the date of the member’s initial 9/11 exposure and the end of the MTI for their aerodigestive disorder.
-
Acute Traumatic Injuries
-
Health Conditions Medically Associated with WTC-Related Health Conditions
A condition that is medically associated with a WTC-related health condition is also eligible for certification and treatment within the WTC Health Program. In order for a medically associated health condition to be certified, the condition must result from the treatment or progression of a WTC-related health condition. The underlying WTC-related health condition must first be certified by the WTC Health Program before any conditions may be certified as medically associated with the underlying condition. Medically associated conditions are evaluated and certified on a case-by-case basis
The WTC Health Program requires that the CCE or NPN physician provide a detailed explanation in the WTC-3 Certification Request form (Appendix 3-A), and medical records as appropriate, that the health condition under consideration as medically associated resulted from either treatment or progression of the underlying certified WTC-related health condition. See Health Conditions Medically Associated with World Trade Center-Related Health Conditions. [5 pages, 484 KB]
-
Establishing that the Medically Associated Health Condition “Results from” Treatment of a Certified WTC-Related Health Condition.
The WTC Health Program will review the CCE or NPN’s explanation to determine if: (i) the relationship linking the medically associated health condition the WTC-related health condition occurs without the influence of an intermediary health condition or event; and (ii) the linkage between the certified WTC-related health condition and the medically associated health condition resulting from treatment of the certified WTC-related health condition has been well-established by published peer-reviewed scientific literature.-
“Results from” Treatment. The CCE or NPN physician must demonstrate by means of a detailed narrative (including medical records when appropriate) that the health condition “results from” medical treatment of the underlying certified WTC-related health condition without the influence of an intermediary health condition or event. The WTC Health Program will certify as medically associated only those conditions which directly result from treatment of a WTC-related health condition, i.e., that the medically associated condition occurred in absence of intervening medical events.
Note: CCE and NPN physicians are encouraged to consult with the Director, WTC Health Program Medical Benefits, about medically associated health conditions that result from treatment of a certified WTC-related health condition as certification will depend on the particular medical facts of each case.
- Previously Published in Peer-Reviewed Literature. The CCE or NPN physician must demonstrate that the medical association between the underlying [certified WTC-related] health condition and the medically associated health condition resulting from treatment of the underlying [certified WTC-related] health condition has been established in previously published peer-reviewed medical literature. The establishment of this medical association in the literature must be documented in the member file, whether included as part of the physician’s narrative or otherwise captured by Program staff.
-
“Results from” Treatment. The CCE or NPN physician must demonstrate by means of a detailed narrative (including medical records when appropriate) that the health condition “results from” medical treatment of the underlying certified WTC-related health condition without the influence of an intermediary health condition or event. The WTC Health Program will certify as medically associated only those conditions which directly result from treatment of a WTC-related health condition, i.e., that the medically associated condition occurred in absence of intervening medical events.
-
Establishing that the Medically Associated Health Condition “Results from” Progression of a Certified WTC-Related Health Condition.
The WTC Health Program will review the CCE or NPN physician’s explanation to determine if: (i) the relationship linking the medically associated condition with the WTC-related health condition occurs without the influence of an intermediary health condition or event; and (ii) the linkage between the certified WTC-related health condition and the medically associated condition resulting from progression of the certified WTC-related health condition has been well-established in published, peer-reviewed scientific literature.
-
“Result from” Progression. The CCE or NPN physician must demonstrate by means of a detailed narrative (including medical records when appropriate) that the health condition ”results from” progression of the underlying certified WTC-related health condition without the influence of an intermediary health condition or event.
Note: CCE and NPN physicians are encouraged to consult with the Director, WTC Health Program Medical Benefits, about medically associated health conditions that are the result of progression of a certified WTC-related health condition as certification will depend on the particular medical facts of each case.
- Previously Published in Peer-Reviewed Literature. The CCE or NPN physician must demonstrate that the medical association between the underlying [certified WTC-related] health condition and the medically associated health condition resulting from progression of the underlying [certified WTC-related] health condition has been established in previously published peer-reviewed medical literature. The establishment of this medical association in the literature must be documented in the member file, whether included as part of the physician’s narrative or otherwise captured by Program staff.
-
“Result from” Progression. The CCE or NPN physician must demonstrate by means of a detailed narrative (including medical records when appropriate) that the health condition ”results from” progression of the underlying certified WTC-related health condition without the influence of an intermediary health condition or event.
-
Establishing that the Medically Associated Health Condition “Results from” Treatment of a Certified WTC-Related Health Condition.
5. CCE/NPN Physician Determination and Request for Certification of Health Conditions
When a member is diagnosed with a health condition that the provider believes is related to a 9/11 exposure, the member may be eligible for medical treatment for that condition under the Program.
-
CCE/NPN Physician Determination
If, following an initial health evaluation or monitoring or treatment exam, the treating CCE or NPN physician determines that the member has a health condition which is a qualifying condition covered by the Program, as described in Section 4, and that member’s exposure to airborne toxins, any other hazard, or any other adverse condition resulting from the September 11, 2001, terrorist attacks, is substantially likely to be a significant factor in aggravating, contributing to, or causing the illness or health condition or mental health condition, then the physician must submit this determination to the Program and request certification of the health condition in order to provide treatment under the Program.
-
Secondary Review of Negative Physician Determination
Where a member’s CCE/NPN makes a negative determination (a finding that exposure to airborne toxins, any other hazard, or any other adverse condition resulting from the September 11, 2001, terrorist attacks, is not substantially likely to be a significant factor in aggravating, contributing to, or causing the health condition or mental health condition) and declines to request certification of the health condition by the WTC Health Program, the member may request a secondary review of this decision by writing the Clinical Director of the CCE or NPN. However, a request for a secondary medical review for a health condition that does not meet WTC Health Program policy is not permitted. Disagreement with Program policy is not a valid reason for secondary review. The procedure for a secondary review is as follows:
- The member is informed by the CCE/NPN of the decision to not request certification in a timely manner and is informed of his/her right to obtain secondary review; this should occur ideally through a Clinic visit.
- If the member disagrees with the decision to not request certification, s/he shall be given counsel regarding the secondary review process and provided a brochure detailing his/her rights in terms of obtaining a secondary review. To initiate the secondary review process, the member must send a letter to the CCE/NPN Clinical Director, or designee, which clearly indicates his/her request to obtain secondary medical review.
- The CCE/NPN Clinical Director or designee then performs a review of the case. This designee can be a CCE physician at another CCE.
- If the secondary review upholds the original decision to not request certification, then the CCE /NPN Clinical Director must send a written letter to the member (within 4 weeks) which summarizes the decision and provides an explanation of how this decision was made. A copy of this letter should be sent to the Administrator of the WTC Health Program.
- If the secondary review finds that WTC-relatedness is supported, the CCE/NPN Clinical Director must send a written letter to the member informing him/her of this decision. This letter should state that a WTC-3 request for certification will now be sent to the WTC Health Program, with an attestation coming from the physician who performed the secondary review.
- The CCE/NPN shall track all secondary review decisions and may make recommendations to the Administrator of the WTC Health Program, as appropriate, when such decisions point to a need for an evaluation or change to Program policies and procedures.
-
CCE/NPN Requests Certification from the Program Using the WTC-3 Form
The WTC-3 Certification Package is the standard documentation completed by a CCE/NPN physician to request certification for a member’s health condition; it provides the medical rationale linking the exposure to the stated health condition. A sample of the form is provided in Appendix 3-A. This form must be used for any condition which a physician has determined to be WTC-related since the Program CCE contracts were implemented [i.e., as of July 1, 2011 for enrolled responders; as of September 29, 2011 for enrolled survivors; and as of October, 2013 for enrolled members assigned to the Nationwide Provider Network (NPN)]. The Clinical Director of the CCE or the NPN reviews, approves and securely submits the completed WTC-3 Certification Package signed by the examining or responsible physician to the Program. Such forms are also used to request certification of health conditions as medically associated with a WTC-related health condition.
The WTC-3 Certification Package contains identifying information for the member and examiner, diagnostic codes for the condition(s) for which the member is requesting certification, and either a medical rationale linking 9/11 exposure to the health condition or the medical rationale linking the medically associated health condition to an existing WTC-related health condition. For a health condition medically associated with a WTC-related health condition, the physician’s determination shall contain information on how the health condition has resulted from treatment of a previously certified WTC-related health condition, or how it has resulted from progression of the certified WTC-related health condition. All cancer certification requests require a pathology report to be submitted with the WTC-3 Certification Package. Specific guidance regarding how to complete the WTC-3 Certification Package, including reasonable practice examples using Program-approved templates, is provided below.
When providing a rationale for the certification, requesters use an explanatory narrative that may be combined with Program-approved template within the WTC-3 form. The rationale should contain pertinent information about 9/11 exposure and time-linked emergence of symptoms. Facts available from the standardized monitoring or screening examination, including exposure assessment, presenting symptoms and temporal relationship of these symptoms relative to 9/11 exposure, should be included. Medical findings should be documented in the institutional medical record, which include the screening or monitoring exams and any additional medical testing or imaging studies required to establish the diagnosis. By procedure, the member’s institutional medical record is incorporated by reference when the CCE provider or NPN Clinical Director requests certification using the WTC-3 Certification Package. This process provides the Program with all relevant information required to make an informed decision regarding the member’s certification. See Appendix 3-B for instructions specific to completing the WTC-3 form for cancer.
The WTC-3 submission must include a signed affirmative statement by the physician that the member’s exposure to airborne toxins, any other hazard, or any other adverse condition resulting from the September 11, 2001, terrorist attacks, is substantially likely to be a significant factor in aggravating, contributing to, or causing the illness or health condition or mental health condition. If the physician is unable to make such and affirmative finding, then the WTC-3 cannot be submitted or considered.
-
Previous Program Members Certified Using WTC-2 Batch Process
The WTC-2 batch certification process was used for a subset of program members who had treatment initiated for qualifying conditions as part of the previous federally-sponsored programs (the Medical Monitoring and Treatment Program (MMTP) for responders and/or the Environmental Health Clinic (EHC) for community members). This process was implemented to ensure treatment continuity for members already receiving care under predecessor programs and is no longer being used.
If the certifications for qualified conditions were supported by documentation in the members’ medical records, the Clinical Director of the CCE or the NPN submitted an attestation for all members and their associated conditions via electronic spreadsheet. The spreadsheet contained identifying member information and diagnostic codes for each qualifying WTC-related or medically associated condition that required certification. The CCE/NPN then transmitted the WTC-2 batch certification request to the Program in a secure manner (as described in Section 6, below). The Program verified the requested conditions against the Codebook (described further in Section 9, below) and returned any discrepant data to the submitter for rectification. Periodic summary reports of certified conditions by member were then sent to the CCE/NPN by the HPS contractor.
The CCE/NPN is responsible for maintaining a record of a member’s certifications to enable appropriate service authorization decisions. As part of their Quality Assurance Program the CCE/NPN conducts internal audits of their contracted part of the WTC Health Program at a minimum of every quarter. These data are made available to the Administrator of the WTC Health Program or designee. Where data is obtained, through a quality assurance audit or otherwise, that indicates that the certification issued through the WTC-2 process was incorrect, the Administrator of the WTC Health Program may de-certify a condition as appropriate.
6. Overview of the Certification Process
Certification is the lynchpin by which the Program ensures members receive appropriate services and that all services are provided in accordance with statutory and regulatory requirements. A CCE/NPN is responsible for submitting requests for health condition certification using the WTC-3 form. The WTC Health Program then reviews and evaluates the request (WTC-3) and makes one of three possible decisions for each health condition contained within the request:
- The health condition is certified, enabling the member to receive treatment for the certified health condition;
- The health condition is denied certification, which gives the member the right to request an appeal of the denial decision; or
- The request is suspended and categorized by the WTC Health Program as a “re-do” pending receipt of additional information about the request from the CCE or NPN physician submitting the request.
- The certification process begins when the CCE/NPN examines the member and makes a determination regarding whether the member has an illness which is covered in the WTC Health Program and that the member’s 9/11 exposure is related to his or her illness.
-
The CCE/NPN completes and submits the WTC-3 package (including supporting documents) to the Program in one of three ways:
- By mail to the WTC Health Program mailroom;
- By fax to the secure WTC Health Program fax number; or
- By placing a PDF version of the WTC-3 package on the Program’s secure file transfer protocol (SFTP) server.
- For paper and fax submissions, the mailroom scans the package, assigns a document control number (DCN), uploads the scanned document to the SFTP server for the HPS Member Services Team (MST) to access, and notifies the MST that certification requests are available for review. In this way, the MST accesses all submitted packages from one consolidated location – the SFTP server.
-
The MST reviews the submitted WTC-3 package to determine whether it is complete and can be processed. A WTC-3 package is considered to be complete if:
- The WTC-3 form is legible and fully filled out;
- A supporting narrative/assessment is provided;
- The WTC-3 form is signed and dated by the member’s health provider and includes the required physician determination and attestation that the member’s exposure to airborne toxins, any other hazard, or any other adverse condition resulting from the September 11, 2001, terrorist attacks, is substantially likely to be a significant factor in aggravating, contributing to, or causing the illness or health condition or mental health condition; and
- The member for whom certification is being requested is enrolled as a member in the Program.
- If the CCE/NPN request for certification is found to be incomplete, the request will be categorized as a “re-do” (neither certified nor denied), and held in a suspended status until specific facts are either supplied (when missing) or clarified (when too vague or misleading) by the CCE or NPN submitting the request for certification. As a result of the request for certification being suspended, the member is not eligible to receive medical or pharmacy benefits for the health condition subject to request for certification (see section below regarding the request for a time-limited authorization of treatment pending certification). If a certification is made via a follow up submission, the effective date of the certification will always be assigned as the signature date of the original submission.
- If the MST determines that the WTC-3 package is complete and the member is properly enrolled, the package is forwarded to the NIOSH MBM for review and approval. Certifications are forwarded to the MBM on a weekly basis.
- The NIOSH MBM reviews the certification requests and makes determinations to approve or deny the certification or to request a “redo,” when necessary (e.g., due to missing information). The MBM also determines the effective date for medical benefits, and notifies the MST of the decisions.
- Upon approval by the MBM, the MST updates the claims processing system, assigns benefit plans as appropriate, and notifies the CCE/NPN of the decisions.
7. Authorization of Treatment Pending Certification
Authorization of Treatment Pending Certification is permitted pursuant to Sections 3312(b)(5) (responders) and 3322(a) (survivors) of the PHS Act and 42 C.F.R. § 88.20(c). Treatment pending certification is offered, where specifically requested by a CCE/NPN physician, in order to provide timely institution of therapy or continuity of care while a certification request is being reviewed.
- In the past, the WTC-1 Form was used to request this authorization as a means of providing “continuity of care” for the subgroup of members receiving treatment in the previous federally sponsored programs (MMTP and EHC) until the new certification process was implemented. This process expired in November 2011, and the form was retired.
- Under the current WTC-3 certification process, while certification is pending, authorization for time-limited treatment of a WTC-related health condition or a health condition medically associated with a WTC-related health condition may be requested at the CCE/NPN physician’s discretion through the WTC-3 Form. Such authorization must be obtained from the WTC Health Program before treatment is provided, except for the provision of treatment for a medical emergency.
- Treatment rendered after WTC-3 submission but prior to certification will only be covered if the request for treatment pending certification was included in the WTC-3 submittal, the care delivered does not require a Level 3 Prior Authorization, the request for certification is ultimately granted, the treatment provided is medically necessary and follows Program guidelines, and the care is rendered by a CCE/NPN-affiliated provider. In the event that the condition is denied certification, any care provided for the condition that is outside the parameters of the Diagnostic Plan will not be covered and the CCE or NPN providing the care will be responsible for the costs of such care.
- If the certification request is determined to be unsatisfactory, then the authorization for treatment pending certification is discontinued immediately and related claims are pended for up to three weeks, during which time the CCE or NPN will work with the MST to rectify any deficiencies in the request, if possible. After 3 weeks, unsatisfactory certification requests will convert to a denial of certification and appropriate Program actions (see Sections 8 and 10, below).
8. Certification Decisions
-
Potential Outcomes Following a Request for Certification
A CCE or NPN physician is responsible for submitting requests for certification of a health condition using the WTC-3 form. The WTC Health Program then reviews and evaluates the request (WTC-3) and makes one of the three following decisions for each health condition contained within the request:
- The member’s health condition is certified, enabling the member to receive treatment for the certified health condition;
- The member’s health condition is denied certification, which gives the member the right to request an appeal of the denial decision; or
- The request for certification is “suspended” pending receipt of additional or clarifying information regarding the certification request submitted by the CCE or NPN.
-
Communicating Certification Request Outcomes to Members
The Program makes every effort to make informed decisions regarding WTC-related health condition certifications in a timely manner and to communicate those decisions to the member efficiently. For certification requests of health conditions medically associated with a WTC-related health condition, the Program will render a decision and notify the member in writing of the decision and the reason for the decision within 60 calendar days after the date the physician’s determination was received. To that end, the Program has developed decision letters addressing the range of decisions that could be made in the certification process (e.g., approval or denial of certification request, the need for additional information to inform the certification decision, etc.). When a member’s health condition is approved for certification as either a WTC-related health condition or a medically associated health condition, the Program sends the member a letter informing him/her of the certification and provides electronic notification to the CCE/NPN that requested the certification. When a member’s requested health condition is denied certification, the Program sends the member letter informing him/her of the denial and provides an electronic copy of the letter to the requesting CCE/NPN. The denial letter discusses the condition requested, the reason for the denial, and the information submitted to the Program for review from the CCE or NPN. The letter also answers frequently asked questions and provides instructions about how appeal the denial decision.
-
Suspended Requests for Certification
A suspended request for certification is neither certified nor denied, but has been placed in an administratively pended status until specific facts are either supplied (when missing) or clarified (when too vague or misleading) by the CCE or NPN submitting the request for certification.
-
Time to Provide Information to Resolve a Suspended Request for Certification
The WTC Health Program will notify the CCE or NPN that submitted the request for certification when more information is required to complete processing of the request for certification. This notification will be made in writing by electronic message (via secure portal). The CCE or NPN has 60 days from the date of the written notification from the WTC Health Program to provide the Program with the requested additional information. The WTC Health Program will provide weekly updates to each CCE or NPN regarding any outstanding requests for certification that have been suspended pending additional information and the number of days that have elapsed since the notification and request for additional information for each case was sent to the CCE or NPN.
-
Effect of Suspended Request for Certification on Authorization of Treatment Pending Certification
As a result of the request for certification being suspended, the WTC Health Program member is generally not eligible to receive medical or pharmacy benefits for the health condition subject to request for certification. However, if the original submission requesting certification of a given condition included a time-limited authorization of treatment pending certification, the requesting CCE or NPN may choose to continue providing benefits to the member at their own expense. In the event that the suspended request for certification is subsequently approved through timely rectification of the record, reimbursement of treatment services will be permitted with an effective date of the signature date of the original WTC-3 submission. In the event that the condition is denied certification, any care provided outside the parameters of the Diagnostic Plan will not be covered and the CCE or NPN providing the care will be responsible for the costs of such care. If the concerns resulting in the suspended request are not resolved after 60 days as outlined above, then any authorization for treatment pending certification is terminated and the member is notified as per protocol.
-
Resolution of a Suspended Request for Certification
There are five potential outcomes for a request for certification that has been placed in a suspended status; those outcomes are as follows:
-
Certification After Receipt of Additional Information from the CCE or NPN
The CCE or NPN responds to the notification of a suspended request for certification with additional or clarifying information. Based on this information, the Program is able to certify the health condition.
-
Denial of Certification After Receipt of Additional Information from the CCE or NPN
The CCE or NPN responds to the notification of a suspended request for certification with additional or clarifying information. This additional information does not satisfy the requirements for certification, however, and results in a denial of certification for the health condition. The member has the right to appeal the denial decision.
-
Administrative Closure Following a Request by the CCE or NPN to Withdraw the Certification Request
The CCE or NPN responds to the notification of a suspended request for certification by indicating in writing that they would like to withdraw the original request for certification. If a withdrawal is requested, the WTC Health Program will no longer evaluate the request for certification and will administratively close the request file. Reasons for withdrawal may include the CCE/NPN determining that the requested information cannot be supplied in a timely manner or newly recognizing that the request for certification cannot be supported based on established WTC Health Program criteria. The CCE/NPN will inform the member of the withdrawal of the request for certification, and advise the member of their right to a secondary review.
-
Denial of Certification Following an Insufficient Response from the CCE or NPN After Request for Additional Information
If the CCE or NPN responds to the WTC Health Program’s notification of suspended request for certification but is unable to provide the requested information necessary to resolve the suspended certification request within the 60 day time limit allowed for final resolution of the request, then the WTC Health Program will take the following actions. The WTC Health Program will send a written communication to the CCE/NPN (via electronic message) asking for confirmation that they cannot provide additional information but that they still wish to request certification for the health condition. If the CCE/NPN responds in writing (via electronic message) that this is the case, then the WTC Health Program will deny the request for certification of the health condition due to lack of sufficient information to make a definitive evaluation of the link between 9/11 exposure and the requested health condition or between the WTC-related health condition and the requested medically associated health condition. The WTC Health Program will inform the member of the denial and his or her right to request an appeal of the denial decision.
-
Administrative Closure Following No Response from the CCE or NPN After Request for Additional Information
If the CCE or NPN does not respond at all to the notification of a suspended request for certification within the 60 day time limit allowed for final resolution of the request, then the WTC Health Program will administratively close the request for certification of the health condition due to lack of sufficient information to support a physician’s determination (upon which a certification decision could be based). Similarly, if the WTC Health Program asks the CCE/NPN for a confirmation that they cannot provide additional information but that they still wish to request certification for the health condition (as outlined above) and the response from the CCE/NPN is unclear or equivocal as to the intent to request certification, then the WTC Health Program will administratively close the request for certification of the health condition due to lack of sufficient information to support the physician’s determination. In either case, the WTC Health Program will notify the CCE or NPN in writing via electronic message that the request for certification has been administratively closed. The CCE/NPN will inform the member of the administrative closure of the request for certification, and advise the member of his or her right to a secondary review. The CCE/NPN may submit a new WTC-3 at a later date should additional or clarifying information becomes available.
-
Certification After Receipt of Additional Information from the CCE or NPN
-
Time to Provide Information to Resolve a Suspended Request for Certification
-
Certification of Deceased Members
The WTC Health Program does not certify health conditions for deceased members. The WTC Health Program may cover medically necessary treatment for certified health conditions from the effective date of the certification (or from the effective date of the certification request in cases of appropriately requested treatment pending certification). The WTC Health Program will not review certification requests dated after a member’s death.
9. Linking Member Health Benefits to Certified Health Conditions
WTC-related health conditions identified in 42 C.F.R. § 88.15 have been grouped into certification categories to align the limited coverage intent of the Program with standards of care and principles of medical necessity. The WTC Health Program defined the business rules used in the processing (adjudication) of healthcare claims to ensure compliance with the limited coverage intent of the Program. Each member category – General Responder, Screening-eligible Survivor, Certified-eligible Survivor, FDNY Responder, and FDNY Family Member – is associated with one or more designated benefit plans. The WTC Health Program Codebook contains the covered diagnosis codes (ICD-9, or if after October 1, 2015, ICD-10), procedural codes (CPT-4 and HCPCS), and pharmaceutical codes (Rx) for the Program. Providers are responsible for working with the CCE/NPN to determine allowable services. A more complete description of these categories and benefit plans may be found in Chapter 4.
-
The Program Codebook describes the diagnoses and services covered under the Program and consists of accepted medical coding for the following:
- Health condition diagnoses – defined by the current World Health Organization’s (WHO’s) International Classification of Disease, 10th edition and Clinical Modification (ICD10-CM) and the World Health Organization’s International Classification of Diseases for Oncology, 3rd edition (ICD-O-3);
- Health services – defined as procedures by the American Medical Association’s Current Procedural Terminology (CPT®);
- Provider-administered pharmaceutical products or durable medical equipment (DME) by the Centers for Medicare & Medicaid Services’ (CMS’s) Healthcare Common Procedural Coding System (HCPCS); and
- WTC Health Program Formulary – medications by therapeutic class, brand name, and generic name.
- Medical coding is regularly updated as per source coding references (ICD, CPT, and HCPCS) and as per requirements published by HHS (e.g., transition to WHO’s International Classification of Diseases, 10th edition [ICD-10] on October 1, 2015). The Codebook is updated through a systems change management process (see Chapter 4), and version control is maintained through regular electronic dissemination and posting on a centralized Program website. The official version of the Codebook is found in the Program’s file of record.
- Care Suites have been developed by the Program to link the adjudication of healthcare claims with a member’s health benefits, including the care required to manage certified health condition(s). Care Suites are defined by the medical coding that comprises both the allowable conditions within a certification category, and the medical care required to manage these conditions via allowable procedures and products. The Care Suites guide the processing of healthcare claims. Further discussion of Care Suites can be found in Chapter 4, and a full discussion of the claims processing system is found in Chapter 5.
- D. The System of Records for the WTC Health Program is housed within the claims processing system, which contains file links to scanned images of source member enrollment and certification paperwork. The System of Records Notice may be found at: https://www.cdc.gov/SORNnotice/09-20-0147.htm and was last updated in June 2011 (76 Fed. Reg. 34706 (June 14, 2011)).
10. Appeals of Certification Denials and/or Decertifications
Requests to appeal a denial of certification of a health condition as a WTC-related health condition or as a health condition medically associated with a WTC-related health condition, a decertification of a health condition, or a denial of authorization for treatment must be postmarked within 120 calendar days of the date of the letter from the Administrator notifying the member of the adverse decision. A valid request for an appeal must (1) be made in writing and signed; (2) identify the WTC Health Program member and designated representative (if applicable); (3) describe the decision being appealed and the reasons why the member or designated representative believes the decision is incorrect and should be reversed; and (4) be sent to the WTC Health Program at the address specified in the notice of denial.1
The description in the request may include scientific or medical information correcting factual errors that may have been submitted to the WTC Health Program by the CCE or NPN; information demonstrating that the WTC Health Program did not correctly follow or apply relevant WTC Health Program policies or procedures; or any information demonstrating that the WTC Health Program’s decision was not reasonable given the facts of the case. The basis provided in the appeal request must be sufficiently detailed and supported by information to permit a review of the appeal. Any new information not previously considered by the WTC Health Program must be included with the appeal request, unless later requested by the WTC Health Program.2 For more detailed information about what may or may not be considered during the appeal process, please see Chapter 4, Section 3.6 of this Administrative Manual.
An appeal request that meets the above requirements, however, will still be considered invalid and outside the scope of the WTC Health Program’s administrative appeal process if its sole argument is a challenge to existing law, regulations, or Program policies. In other words, if the issues raised in the appeal have already been determined by law, regulation, or Program policy, then the appeal may not move forward because there are no outstanding issues for the Program to resolve with respect to the individual appellant. For example, an appeal request may not challenge a denial of certification of a health condition where the denial was based on certification requirements established in the Zadroga Act or the health condition not being included on the List of WTC-Related Health Conditions (List) in the Program’s regulation at 42 C.F.R. § 88.15 because those criteria are established by law and may only be changed by an act of Congress amending the law or the Program publishing an amendment to the regulation, respectively. Similarly, an appeal request may not challenge a denial of certification based on a Program policy that has been established by the Administrator and is applicable to all Program members, such as the latency requirements in the Program’s Minimum Latency & Types or Categories of Cancer. Any challenge to criteria established by law, regulation, or Program policy through the appeal process would be ineffectual because revisions to such criteria require a broader legal, regulatory, or policy action that would be applicable to all Program members; therefore, the challenge cannot be addressed in the appeal of an individual member. An appeal request may, however, challenge the Program’s application of the certification criteria (e.g., the member could argue that the Program incorrectly determined the amount of time that elapsed between the member’s initial 9/11 exposure and the date of his/her initial cancer diagnosis).
An individual wishing to voice concerns or request that the Administrator change a Program regulation or policy may write to the Administrator. An individual may also petition the Administrator to add a health condition to the List of WTC-Related Health Conditions (List); for more information on the petition process, see https://www.cdc.gov/wtc/petitions.html. The petition process can only be used to request the addition of a WTC-related health condition to the List. It cannot be used to request that the Program cover a specific health condition medically associated with a certified WTC-related health condition, cover a certain type of treatment, or amend Program regulations or policies. Changes to the Zadroga Act require an act of Congress.
When a denial of health condition certification or a decision to decertify a health condition is issued by the Program, the member may appeal the decision. An appeal must be made in writing within 120 calendars days from the date of the WTC Health Program’s letter notifying the member of the denial or decertification decision. The written, signed appeal request should include a full explanation of why the member (or the member’s designated representative) believes that the denial decision is incorrect. See Overview of the Appeal Process for Denial of Health Condition [PDF, 9 pages, 684 KB] The following mailing address or fax number should be used to submit a request for appeal:
Appeal Coordinator
WTC Health Program
Po Box 7000
Rensselaer, NY 12144
Fax: 1-404-471-8338
- Within 14 days of receiving an appeal request, the appeals coordinator will notify the individual by letter whether the appeal request is accepted or not. If the appeal request is accepted, the letter will provide the individual with the name of the Federal Official who will review the appeal. If the appeal request is not accepted, the letter will inform the individual and provide the reason(s) the appeal was not accepted.
- An individual may request the opportunity to make an oral statement to the Federal Official during the appeal review within the appeal request letter to the appeals coordinator. The individual may also request to make an oral statement within 14 calendar days of receiving the letter from the appeals coordinator notifying him/her that the appeal request was accepted.
- The Federal Official will review the appeal. If the appeal review is going to take longer than 60 calendar days from the date of the letter notifying the individual that his/her appeal request was accepted, the appeals coordinator will send a letter to the individual providing a written explanation of the delay and the estimated date the review is expected to be completed.
- The Federal Official will review all available records and assess whether the appeal should be granted. The Federal Official may consider additional relevant new information and will provide a recommendation to the Administrator of the WTC Health Program. After receipt of the Federal Official’s recommendation, the Administrator will make a final decision on the appeal. The Administrator will notify the member and/or designated representative in writing of the decision and an explanation of the reason(s) for the decision, as well as any actions taken by the WTC Health Program resulting from the decision.
- Pursuant to 42 C.F.R. § 88.15(c), the WTC Program Administrator is permitted to reopen a final determination at any time and to affirm, vacate, or modify that determination in any manner he or she deems appropriate.
142 C.F.R. § 88.21(b).
242 C.F.R. § 88.21(b)(2)(iii).
Appendices
3-A WTC-3 Form [PDF, 3 pages, 391 KB]3-B WTC-3 Instructions for Cancer [PDF, 5 pages, 594 KB]
3-E Making a Determination about Exposure Aggravating Pre-Existing Aerodigestive Disorders
3-F Time Intervals for New Onset Aerodigestive Disorders
3-G Policy and Procedures for Certification of Physician Determinations for Aerodigestive and Cancer Health Conditions
3-H Minimum Latency & Types or Categories of Cancer
3-I Malignant Neuroendocrine Neoplasms
3-J Myeloid Malignancies
3-K Rare Cancers
3-L Policy and Procedures for Handling Submissions and Petitions to Add a Health Condition to the List of WTC-Related Health Conditions
3-M Policy and Procedures for Adding Non-Cancer Conditions To the List of WTC-Related Health Conditions
3-N Policy and Procedures for Adding Types of Cancer To the List of WTC-Related Health Conditions
Chapter 4—Medical Benefits
TABLE OF CONTENTS
Last Revised – January, 2026
- Administration of Medical Benefits and Services
- Approved Benefit Plans
- Authorization of Services
-
Guidelines for Covered Services
- Acupuncture Services
- Chimeric Antigen Receptor T-cell (CAR-T) Therapy
- Coverage of Conditions Outside the United States
- COVID-19
- Dental Services
- Durable Medical Equipment, Prosthetics, Orthotics and Supplies (DMEPOS)
- Hospitalizations
- Medical Marijuana
- Mental Healthcare
- Monoclonal Gammopathy of Undetermined Significance (MGUS)
- Non-Invasive Neoplasms of the Cervix Uteri
- Post-Acute Care Services
- Preventive Care
- Repetitive Transcranial Magnetic Stimulation (rTMS)
- Routine Medical Care
- Second Opinions
- Sleep Apnea
- Solid Organ Transplants
- Surgeries
- Transportation Services
- Urgent Care
- Uterine Cancer
- Appendices
1.0 Administration of Medical Benefits and Services
1.1 Purpose and Scope
This chapter describes the medical benefits that are available through the World Trade Center (WTC) Health Program under the James Zadroga 9/11 Health and Compensation Act of 2010 (the Zadroga Act),1 as amended, including: (1) the Program’s responsibilities regarding the provision of medical benefits and the roles of various parties; (2) the types of medical benefits and treatment provided; (3) communications regarding medical benefits; (4) appeals of treatment authorization decisions; (5) the process for requesting changes to medical treatment that is permitted under the WTC Health Program; and (6) unique considerations relative to certain permitted services.
1.2 Statutory and Regulatory References
The following Sections of the Zadroga Act are applicable to this chapter:
- Section 3311(b) of the Zadroga Act authorizes monitoring benefits for WTC responders;
- Section 3312(b)(1)(A)(ii) provides that the WTC Health Program shall pay for medically necessary treatment for certified WTC-related health conditions, assuming certain conditions are met;
- Section 3312(b)(3)-(5) explains the requirement of medical necessity for treatment, the need to use rulemaking to specify a standard for determining medical necessity and for appealing such determinations, the scope of treatment, and the provision of treatment pending certification;
- Section 3321(b) provides for initial health evaluations (screening) for screening-eligible WTC survivors; and
- Section 3322 allows for follow-up monitoring and treatment of certified-eligible WTC survivors.
Program regulations relating to medical benefits are established in the following sections of 42 C.F.R. Part 88:
- Section 88.11 regarding initial health evaluation for screening-eligible survivors;
- Section 88.17 regarding physician’s determination of WTC-related health conditions;
- Section 88.20 regarding authorization of treatment;
- Section 88.21 regarding appeal of certification, decertification, or treatment authorization decision; and
- Section 88.22 regarding reimbursement for medical treatment and services.
1.3 Roles and Responsibilities
The parties involved in providing WTC Health Program medical benefits and their roles are detailed below:
- The Administrator of the WTC Health Program or Designee (e.g., WTC Health Program medical benefits manager (MBM)) establishes medical and pharmaceutical policy for the WTC Health Program, certifies health conditions for treatment, establishes a process for members’ appeals of medical denials, designates a Federal Official independent of the WTC Health Program to review member appeals, issues final decisions on appeals regarding medical treatment, considers additions of health conditions to the List of WTC-Related Health Conditions (List), and conducts any necessary rulemaking. The Administrator of the WTC Health Program or Designee also authorizes requests for certain levels of prior authorization (PA), as discussed in Section 3.4, Prior Authorizations.
- The Clinical Centers of Excellence (CCEs) and the Nationwide Provider Network (NPN) provide monitoring and initial health evaluations for eligible responders and survivors. The CCEs/NPN also provide treatment for certified WTC-related and medically associated health conditions, and make referrals for treatment to other medical experts (external network providers) that work with the CCEs/NPN as part of their WTC Health Program-affiliated provider networks. The CCEs/NPN provide medical services to WTC Health Program members including treatment, writing and approving prescriptions, and providing prior authorizations when necessary. The CCEs/NPN authorize medical treatment that is consistent with established treatment protocols and review claims for payment from external network providers to ensure adherence to coding requirements and WTC Health Program guidelines. The CCEs/NPN document decisions requiring prior authorization from their respective CCE/NPN Clinical Directors and submit information to the Program for services that require prior authorization from the WTC Health Program MBM. For pharmacy benefits, the CCEs/NPN provide prior authorization or perform overrides for certain medications (see Chapter 14 for further details). Further information regarding CCE/NPN responsibilities, including provider enrollment, may be found in Chapter 6 of this manual.
- The Health Program Support (HPS) Contractor is responsible for receiving and processing claims for medical benefits, enrolling providers in the WTC Health Program-affiliated provider networks, processing requests for prior authorization from the WTC Health Program MBM, providing technical assistance with any changes to medical benefits, providing expert research and recommendations to inform policy decisions, providing communication support regarding Program medical policy and appeals arising from denials of treatment due to medical necessity, ensuring that medical claims are processed in accordance with WTC Health Program policy, and, unless specific exemptions apply, standard American Medical Association (AMA) and Centers for Medicare and Medicaid Services (CMS) billing practices.
1.4 Scope of Treatment Services
The WTC Health Program provides medical treatment services for the conditions specified in the Zadroga Act and 42 C.F.R. § 88.15, as well as any other condition added to the List through the rulemaking procedures specified by the Zadroga Act.
Pursuant to Section 3312(b)(4) of the Zadroga Act, the scope of treatment covered includes services of physicians and other health care providers, diagnostic and laboratory tests, prescription drugs, inpatient and outpatient hospital services, and other medically necessary treatment. Transportation expenses to secure medically necessary treatment through the NPN, involving travel of more than 250 miles, are also authorized under Section 3312(b)(4)(C). 2
1.5 Medically Necessary Treatment
Section 3312(b)(3)(A) requires physicians and other providers to provide medically necessary treatment that is in accordance with medical treatment protocols when providing treatment for a WTC-related health condition. Medical treatment protocols, also referred to as “medical guidelines,” are developed by the Data Centers (DCs) in accordance with accepted medical practice and recommendations from professional organizations, such as the American Medical Association, American College of Chest Physicians, and the like. The protocols are subsequently approved by the Administrator of the WTC Health Program or Designee for use with WTC Health Program members. Protocols are maintained by the DCs/CCEs as well as in NIOSH’s official file of record.
Section 3312(b)(3)(B) requires that the Administrator of the WTC Health Program issue regulations specifying a standard for determining medical necessity, a process for determining whether the standard is being met, and an appeals process for medical necessity determinations. 3
2.0 Approved Benefit Plans
The WTC Health Program uses benefit plans to determine the type of medical procedures or treatment a member is eligible to receive. “Benefit plans” are groupings developed by the WTC Health Program that define the acceptable ranges of care for specific categories of covered health conditions. The WTC Health Program offers multiple benefit plans, which are open to members based on their status as defined in the Zadroga Act (e.g., Responder or Survivor) and their certified health condition(s). The WTC Health Program Codebook also lists approved medical procedures and treatment by benefit plan (For further information, see Section 3.2 WTC Health Program Codebooks).
The benefit plans include procedures for the initial health evaluation for survivors, annual medical monitoring for responders and certified-eligible survivors, diagnostic evaluation to enable a nonspecific symptom or abnormal finding to be properly diagnosed for the purpose of certification, and treatment benefit plans organized by the category of certified health condition(s).
Screening-eligible Survivor
WTC Health Program Benefit Plan: Survivor Screening (during initial health evaluation period); Diagnostics (during initial health evaluation period); Cancer Diagnostics (during initial health evaluation period 4)
Certified-eligible Survivor
WTC Health Program Benefit Plan: Monitoring; Diagnostics; Cancer Diagnostics; Treatment; Cancer Treatment if certified for WTC-related cancer condition.
General & FDNY Responder
WTC Health Program Benefit Plan: Monitoring; Diagnostics; Cancer Diagnostics; Treatment; Cancer Treatment if certified for WTC-related cancer condition.
FDNY Family
WTC Health Program Benefit Plan: Diagnostics (coverage limited to mental health conditions); Treatment (coverage limited to certified mental health conditions)
Shanksville Responder
WTC Health Program Benefit Plan: Monitoring; Diagnostics; Cancer Diagnostics; Treatment; Cancer Treatment if certified for WTC-related cancer condition.
Pentagon Responder
WTC Health Program Benefit Plan: Monitoring; Diagnostics; Cancer Diagnostics; Treatment; Cancer Treatment if certified for WTC-related cancer condition.
2.1 Survivor Screening Benefit Plan (Initial Health Evaluations)
Section 3321(b)(1) of the Zadroga Act provides for an initial health evaluation (screening) for screening-eligible WTC survivors. The purpose of the screening is to determine whether the member has a WTC-related health condition and is eligible for follow-up monitoring and treatment benefits under the WTC Health Program. Unlike annual monitoring exams, the screening is a one-time evaluation. However, the member may seek additional screenings at his or her own expense. 5
Upon enrollment in the WTC Health Program, survivors are classified as screening-eligible survivors without a certified health condition and are eligible for the Survivor Screening Benefit Plan. As screening-eligible survivors, they have access to all of the services in the Survivor Screening Benefit Plan and the services in the Cancer Screening Benefit Plan. The initial health evaluation for screening-eligible survivors is listed in the WTC Health Program Codebook, Volume B, under the Survivor Screening Benefit Plan. Use of codes included under the Survivor Screening Benefit Plan indicates to the claims processing system that a given procedure is part of the survivor’s initial health evaluation. The initial health evaluation includes all of the following elements:
- Initial Health Evaluation: Included at no cost to member once per lifetime. Includes completion of a set of detailed questionnaires evaluating 9/11 exposure, health complaints, and medical history, using age-appropriate codes.
- Laboratory analyses of blood: Includes comprehensive metabolic panel or basic metabolic panel, lipid panel, and complete blood count when clinically indicated.
- Urinalysis: May be conducted when clinically indicated.
- Spirometry/Chest Radiography: Includes spirometry with or without bronchodilation. Chest radiography may also be conducted when clinically indicated. Separate billings for technical and professional components may be submitted for these medical tests.
- Electrocardiogram (EKG): May be performed once per year but only for members aged 40 years or older when clinically indicated. 6
Once a health condition is certified, the screening-eligible survivor’s status changes to certified-eligible survivor and they are authorized to receive annual medical monitoring and medically necessary treatment to manage that condition following the medical protocols approved by the Program. 7 Under rare circumstances, a survivor may obtain certification prior to completion of the full initial health evaluation exam if specific requirements, including medical record documentation and other certification requirements are met.8 The member is still required to receive the appropriate initial health evaluation to identify other health conditions that may be a result of exposure.9
2.2 Monitoring Benefit Plan
Sections 3311(b) and 3321(b)(1) authorize monitoring benefits for enrolled WTC responders and certified-eligible survivors, respectively. These monitoring benefits consist of yearly medical examinations and long-term health monitoring and analysis. Monitoring benefits are provided through the CCEs, or the NPN for enrolled members who live outside of the New York metropolitan area.10 The purpose of medical monitoring is to identify health concerns for early intervention, characterize the health of Program members over time, facilitate efforts for continuous quality improvement in the healthcare rendered by the Program, and inform emergency preparedness efforts for future disasters.
Monitoring benefits for WTC responders and certified-eligible survivors are listed in the WTC Health Program Codebook, Volume B, under the Monitoring Benefit Plan. Use of procedure codes included under the Monitoring Benefit Plan indicates to the claims processing system that a given procedure is part of the standard monitoring exam. The monitoring exam includes the following elements:
- Initial monitoring examination: Included at no cost to member once per lifetime. Includes completion of a set of detailed questionnaires evaluating 9/11 exposure, health complaints, and medical history along with health education counseling by a registered nurse.
- Follow-up monitoring examinations: Conducted once per year. The follow-up exam reassesses for health complaints and the intervening medical history occurring since the prior monitoring exam or initial health evaluation. Both the initial and follow-up examinations include items C-E below.
- Laboratory analyses of blood: May be conducted once per year. Includes comprehensive metabolic panel or basic metabolic panel, complete blood count, and lipid panel.
- Urinalysis: May be conducted once per year and/or when clinically indicated.
- Spirometry/Chest Radiography: Spirometry may be performed, once per year. Spirometry with bronchodilation is to be performed on the initial visit only unless the monitoring exam indicates otherwise. Chest radiography may be conducted when clinically indicated and/or once every 2 years. Separate billings for technical and professional components may be submitted for these medical tests.
- Electrocardiogram (EKG): May be performed once per year but only for members aged 40 years or older when clinically indicated.11
2.3 Diagnostics Benefit Plan
All members are eligible for the Diagnostics Benefit Plan, including members who have a certified health condition(s) and members who do not have a certified health condition(s). Screening-eligible survivors who do not have a certified health condition(s) have access to the Diagnostics Benefit Plan only during the initial health evaluation period. Codes in this benefit plan should be used when evaluating a member’s symptoms to determine whether a member has a WTC-related health condition, including both cancer and non-cancer conditions. Mental health conditions under the Diagnostics Benefit Plan are also available to FDNY family members.
All diagnostic claims should be coded using an approved ICD-10 code in the Diagnostics Benefit Plan. Following certification of the WTC-related health condition (as appropriate), the ICD-10 codes available for that condition can be used as part of the Treatment Benefit Plan.
2.4 Treatment Benefit Plan
Under the Treatment Benefit Plan, the WTC Health Program provides coverage for medical diagnoses and procedures related to a member’s certified WTC-related health condition, or health condition medically associated with a certified WTC-related health condition. The Treatment Benefit Plan should be used for all non-cancer certifications, while the Cancer Treatment Benefit Plan should be used for all cancer certifications. FDNY family members are eligible for treatment of mental health conditions under the Treatment Benefit Plan.
For responders and certified-eligible survivors, providers may use any of the procedure codes located in the Treatment Benefit Plan, as long as the codes correspond with the condition-specific Care Suite. Care Suites are used in the Treatment Benefit Plan to further group medical diagnosis codes (ICD-10) into specific treatment categories. When a member is certified for a WTC-related health condition, the member is assigned to a Care Suite that correlates with their certified health condition(s). The medical services associated with each covered condition arise from standard coding references, including the American Medical Association’s (AMA’s) Current Procedural Terminology (CPT®) codes, and the Centers for Medicare and Medicaid Services’ (CMS’) Healthcare Common Procedural Coding System (HCPCS) Level II codes.
The table below provides an example of ICD-10 diagnosis codes that are in the Gastroesophageal Reflux Disorder (GERD) Care Suite. Certification of any of the following WTC-related ICD-10 diagnosis codes opens up the GERD Care Suite, so that the member has access to all the medical services within the GERD Care Suite.
GERD Care Suite
WTC-Related ICD-10 Code: J39.2
ICD-10 Code Description: Diseases of Pharynx- Other
WTC-Related ICD-10 Code: K20.0
ICD-10 Code Description: Esophagitis- Eosinophilic
WTC-Related ICD-10 Code: K20.8
ICD-10 Code Description: Esophagitis- Other
WTC-Related ICD-10 Code: K21.0
ICD-10 Code Description: Gastro-esophageal reflux with esophagitis
WTC-Related ICD-10 Code: K21.9
ICD-10 Code Description: Gastro-esophageal reflux without esophagitis
WTC-Related ICD-10 Code: K29.30
ICD-10 Code Description: Chronic superficial gastritis without bleeding
WTC-Related ICD-10 Code: K29.31
ICD-10 Code Description: Chronic superficial gastritis with bleeding
WTC-Related ICD-10 Code: K29.40
ICD-10 Code Description: Chronic atrophic gastritis without bleeding
WTC-Related ICD-10 Code: K29.41
ICD-10 Code Description: Chronic atrophic gastritis with bleeding
WTC-Related ICD-10 Code: K29.50
ICD-10 Code Description: Chronic gastritis without bleeding – Unspecified
WTC-Related ICD-10 Code: K29.51
ICD-10 Code Description: Chronic gastritis with bleeding—Unspecified
WTC-Related ICD-10 Code: K29.60
ICD-10 Code Description: Other gastritis without bleeding
WTC-Related ICD-10 Code: K29.61
ICD-10 Code Description: Other gastritis with bleeding
WTC-Related ICD-10 Code: K29.90
ICD-10 Code Description: Gastroduodenitis without bleeding—Unspecified
The Care Suites provide an important fiscal control for the Program by defining additional business rules guiding the adjudication of healthcare claims for payment. The examining physician submits information about a specific health condition to the WTC Health Program to review for certification (see Chapter 3, Certification of Health Conditions). The Codebooks provide the medical coding for all medically necessary care to manage the certified health condition under a specific Care Suite. The Care Suites enable the claims adjudication process to approve the appropriate care for that health condition, but withstand the variability that may occur between providers or referral specialists using different specific diagnosis codes when billing for procedures. The conditions listed within a given Care Suite either share target symptoms (like cough), or share a mechanism of injury (like inflammation) within a given organ system.
The Program uses the following Care Suites in the Treatment Benefit Plan:
- Adjustment Disorder (ADJ)
- Anxiety (ANX)
- Depression (DEP)
- Post-Traumatic Stress Disorder (PTSD)
- Substance Abuse (SA)
- Extremity (EXT)
- Head Trauma (HT)
- Spine (SP)
- Gastroesophageal Reflux Disorder (GERD)
- Interstitial Lung Disease (ILD)
- Obstructive Airway Disease (OAD)
- Sarcoid (SRC)
- Upper Respiratory Disease (URD)
- Sleep Apnea (SLP)
Once a member receives certification for a new non-cancer health condition, the condition is assigned to a specific Care Suite listed above. The claims processing system compares the billed diagnosis code on a claim against the Care Suite for the member’s health condition, and verifies that the diagnosis on a claim is among the accepted diagnoses within that Care Suite. This process provides important checks and balances to ensure only approved care for the member’s certified condition is delivered under the WTC Health Program.
Health conditions medically associated to the WTC-related health condition due to the progression or treatment of the certified WTC-related health condition are also treated through the Care Suite model and require certification.
“Ancillary condition” refers to a health condition that does not meet the requirements for certification under the Program, but must be treated in order to manage, ameliorate or cure a certified WTC-related health condition or health condition medically associated with a certified WTC-related health condition. Ancillary conditions are typically within the same organ system as the certified-WTC related health condition or certified health condition medically associated with a certified-WTC related health condition. This includes the acute complications of WTC-related health conditions or common treatment side effects that are generally inexpensive to manage (ex. cough, nausea).
2.5 Cancer Diagnostics Benefit Plan
When a CCE or NPN health provider determines that a member has an abnormality which merits diagnostic evaluation for a possible WTC-related cancer, the provider uses codes in the Cancer Diagnostic Benefit Plan. The Cancer Diagnostic Benefit Plan is assigned to all enrolled responders (except FDNY family members), and is also available to enrolled survivors during the initial health evaluation period. If the survivor has a certified WTC-related health condition, the Cancer Diagnostic Benefit Plan is available on a continuous basis along with the Monitoring Benefit Plan. CCE and NPN providers should use their clinical judgment to determine when clinical, laboratory, or imaging findings merit further evaluation for a possible WTC-related cancer, while considering the exposure history of the member and the likelihood of finding a form of cancer that is covered by the WTC Health Program.
The services (procedure codes) that are permitted for cancer under the Cancer Diagnostic Benefit Plan are found in the WTC Health Program Codebook, Volume A. In addition, numerous ICD-10 condition codes (some that correlate with various signs and symptoms that could be indicative of cancer) may be used for services billed under the Cancer Diagnostic Benefit Plan. These allowable condition codes (ICD-10) are listed in the WTC Health Program Codebook, Volume B.
2.6 Cancer Treatment Benefit Plan
When a CCE or NPN physician determines that a member’s 9/11 exposures are substantially likely to have been a significant factor in aggravating, contributing to, or causing a cancer condition, the physician may request certification of the member’s condition with the submission of a WTC-3 certification request. To assist the CCE or NPN provider with certification requests for cancer conditions, a supplemental information packet has been developed entitled “Instructions for Completing WTC-3 Package Requesting Certification for Types of Cancer.”12
Once a member has been certified for a WTC-related cancer, the member is assigned to the Cancer Treatment Benefit Plan. The Cancer Treatment Benefit Plan contains the medical services (procedure codes) necessary to treat certified cancer conditions, medically associated conditions, and ancillary conditions.13 The procedure codes for these services are found in the WTC Health Program Codebook, Volume A. The cancer diagnosis (ICD-10) codes are found in the WTC Health Program Codebook, Volume B. The National Comprehensive Cancer Network has developed “Clinical Practice Guidelines in Oncology” (NCCN Guidelines14) for cancer treatment. To the extent practical and possible, these guidelines will be used to guide cancer treatment under the Program.
3.0 Authorization of Services
3.1 Authorized Services
The Medical Coverage Determination (MCD) and coverage guidelines for this section are under development. This section will be updated once finalized.
3.2 WTC Health Program Codebooks
The WTC Health Program Codebook lists approved medical procedures and diagnosis codes that may be used for members, depending on the members’ Member Category (Responder or Survivor) and their certified health condition(s). The WTC Health Program Codebook is divided into two volumes, which are further organized by benefit plans that define the acceptable ranges of care for specific categories of health conditions. The treatment benefit plan is further organized by care suites. (For further information, see Approved Benefit Plans, Section 2.0).
The Codebook should be consulted by the CCE/NPN providers to determine payable services and to review applicable guidelines and authorization requirements. Limitations and authorization requirements are further described in Guidelines for Covered Services, Section 4.0 .
-
The WTC Health Program Codebook, Volume A lists the medical procedure codes approved for use within the Program, organized by benefit plan. The WTC Health Program Codebook, Volume A includes codes for office visits for evaluation and management, diagnostic and surgical procedures, laboratory and other medical testing and imaging studies, and durable medical equipment, prosthetics, orthotics, and supplies (DMEPOS). The procedure codes arise from standard coding references, including CPT,15 HCPCS,16 and dental codes.
The Codebook lists the available procedure/service code, code description, mapping to the respective benefit plan, relevant effective dates, prior authorization levels (if applicable), guidelines (if applicable), service limitations (if applicable), and code history. The WTC Health Program Codebook, Volume A is reviewed and updated on a regular basis, and is provided to the CCEs and NPN.
-
The WTC Health Program Codebook, Volume B lists the diagnosis codes approved for use within the Program, organized by benefit plan and treatment Care Suite. (For more information on Care Suites, see Section 2.4 Treatment Benefit Plan).
The diagnosis codes arise from standard coding references, including the International Classification of Diseases, Revision 10 (ICD-10). The WTC Health Program Codebook, Volume B lists the available diagnosis code, code description, mapping to the respective benefit plan or Care Suite, relevant effective dates, guidelines (if applicable), and code history. The WTC Health Program Codebook, Volume B is reviewed and updated on a regular basis, and is provided to the CCEs and NPN.
3.3 Medical Code Change Management
To ensure members receive ongoing high-quality, WTC Health Program-approved care, the Program maintains a mechanism for making necessary changes to the WTC Health Program Codebook. WTC Health Program-initiated changes in covered health condition diagnostic and treatment codes are made on an ongoing basis. These changes may be enacted to refine treatment protocols, align code coverage with WTC Health Program approved coverage, or bring codes in line with updates made by organizations that oversee the codes (such as the American Medical Association or the Centers for Medicare and Medicaid Services).
The CCE/NPN may determine 17 that a diagnosis, procedure, or medical product is necessary for quality patient care, but is not currently covered by the WTC Health Program. The CCE/NPN may also need to request changes to covered health condition diagnostic and treatment codes. In both of these scenarios, the CCE/NPN Clinical Director may request coverage for the diagnosis, procedure, or medical product, or a change to the code, by properly completing and submitting a WTC-5 Medical Code Request Form (Appendix 5.2) to the WTC Health Program MBM via the Medical Code Request Process. The submission of this form triggers the process, which begins with a review of the request and a subsequent decision by the WTC Health Program MBM through the HPS.
The WTC Health Program MBM will review the CCE/NPN-completed WTC-5 Medical Code Request Form (Appendix 5.2) and render one of the following decisions:
-
If the request is approved,
- The WTC Health Program Codebook is updated to reflect the changes;
- The claims processing system is updated to capture the changes; and
- The changes to the WTC Health Program Codebook are communicated to the requester and the other CCEs/NPN.
- The WTC Health Program will communicate the reasons for the denial decision to the CCE/NPN.
- The denial decision may be challenged by the CCE/NPN by submitting a letter to the WTC Health Program within 120 calendar days from the date of denial.
- The WTC Health Program will communicate the needed additional information to the CCE/NPN.
- The CCE/NPN will have 60 calendar days to submit the requested information. If the CCE/NPN does not submit the requested information, the request will be administratively closed.
- The WTC Health Program will notify the CCE/NPN of the closure.
The CCE/NPN and Program staff are required to use the most current version of the Codebook. Because the Codebook undergoes frequent revisions, the CCE/NPN and Program staff should always consult the most current version of the Codebooks when referencing any procedure or diagnosis codes cited in this manual to determine if the code is still valid. Codebooks are updated and posted monthly in the SAMS Portal for the CCEs/NPN to access.
3.4 Prior Authorizations
Certain medical services, devices, and drugs have limited use guidelines and/or require Prior Authorization (PA). Brief guidelines, including those related to PAs, are listed in the Codebook and direct the treating provider to use services in limited or specific clinical situations that align with the Program’s limited health plan model. More information on coverage limitations and service specific coverage decisions can be viewed in Section 4.0 “Guidelines for Covered Services.” The Codebook will list the code, definition, authorization requirement, and guideline (if applicable).
The CCE/NPN Clinical Director may designate individuals to serve as designees for Level 2 Prior Authorization (PA2) and Level 3 Prior Authorization (PA3) requests. The CCE/NPN Clinical Director is liable for all PA2/PA3 decisions. The CCE/NPN Clinical Director may designate a limited number of staff members to sign PA2/PA3 requests on the CCE/NPN Clinical Director’s behalf only if they have the appropriate training and expertise. The name and credentials of the designee must be sent to the WTC Health Program for approval as a selected “treatment authorization designee.”
-
Level 2 Prior Authorization (PA2) Requests require authorization by the CCE/NPN Clinical Director. For services that require a PA2 (e.g. surgeries, DME, etc.), documentation of medical necessity and approval by the CCE/NPN Clinical Director must be maintained either in the member’s medical record or other CCE/NPN tracking system, and be easily retrievable. Certain services may also have a Medical Coverage Determination (MCD) with specific authorization criteria that the member must meet (See MCDs in Section 4.0 “Guidelines for Covered Services”). The CCE/NPN Clinical Director must attest that the member meets relevant MCD criteria and maintain a copy of the attestation in the member’s medical record or other CCE/NPN tracking system. Documentation related to PA2 Requests is subject to audit, as the Program performs periodic utilization reviews to ensure compliance with Codebook guidelines and limitations.
Medical necessity documentation must clearly state the justification for use of the service, drug, or device. If the member is certified, documentation must clearly state how the service/drug/device manages, ameliorates, or cures the certified WTC-related health condition or health condition medically associated with a certified WTC-related condition. Some services are for diagnostic and evaluation purposes and should have clear documentation in the member medical record or other CCE/NPN tracking system as to why the service, drug, or device is necessary to diagnose and evaluate a suspected WTC-related health condition.
No further notification to the WTC Health Program is required for PA2s, since the CCE/NPN stamp on a paper-based or electronically-submitted medical claim (described in Chapter 5) reflects the CCE/NPN acknowledgement that the claim is valid in accordance with all WTC Health Program requirements, including those related to PAs.
If the CCE/NPN Clinical Director denies the PA2, the members may request a secondary review. Each CCE/NPN must have an established secondary review process. Please contact the CCE/NPN for instructions on the secondary review process.
-
Level 3 Prior Authorization (PA3) Requests require authorization by the WTC Health Program.
Some services which require a PA3 (e.g. home health aide, hospice inpatient respite care, etc.) have a Medical Coverage Determination (MCD) with specific guidance on use and limitations (see MCDs in Section 4.0 “Guidelines for Covered Services”). The CCE/NPN Clinical Director must submit a PA3 Request to the WTC Health Program for any service, drug, or device that requires a PA3.
Prior to performing or authorizing a service that requires a PA3, the CCE/NPN Clinical Director must submit a PA3 Request to the WTC Health Program and receive authorization from the Program. If the PA3 Request is not received, the WTC Health Program will not provide payment for the service. The WTC Health Program will either approve, deny, or administratively close the PA3 Request and will return the form, along with the decision, to the Health Program Support (HPS) contractor for distribution to the requesting CCE/NPN. In the event there is an urgent need for the medical service, the CCE/NPN Clinical Director may submit a PA3 Request for the medically necessary, urgent services retrospectively. This retrospective PA3 Request must be submitted within the timeframe parameters stated within the MCD. For those services which do not currently have an MCD, the retrospective PA3 should be submitted within 14 calendar days of the start date of services. Each medical service will generally be authorized as a single service unless otherwise requested by the CCE/NPN in the PA3 Request. The rationale for additional services must be included in the medical justification. For PA3 Requests extending beyond a single service, the CCE/NPN must specify an authorization date range and intended quantity (or unit) of service.
The HPS contractor coordinates with the MBM to process the authorization request. The HPS contractor will notify the CCE/NPN Clinical Director of the approval, denial, or administrative closure.
- If the PA3 Request is approved, the PA3 information is entered into the claims processing system by the HPS contractor, linking the request and any supplemental information to the member record to permit payment.
- If the PA3 Request is incomplete, the associated claims are pended for 14 calendar days and the HPS contractor requests the missing information from the originating CCE/NPN. Incomplete PA3 Requests will be administratively closed if the originating CCE/NPN does not provide the additional information needed to complete the PA3 Request within 14 calendar days of notification.
- If the PA3 Request is denied, the HPS contractor will notify the originating CCE/NPN as soon as possible. Claims for the denied services will not be paid. Appeals for denied PA3 services may be submitted to the Program through the formal appeals process.18 (Please see Section 3.6 “Decisions and Appeals”).
3.5 Authorization of Treatment Pending Certification
While certification is pending, authorization for time-limited treatment of a WTC-related health condition or health condition medically associated with a WTC-related health condition may be requested at the CCE/NPN physician’s discretion through the WTC-3 Form. The purpose of this authorization is to ensure continuity of appropriate medical care that is time sensitive and consistent with Program policy. Such authorization must be obtained from the WTC Health Program before treatment is provided, except for the provision of treatment for a medical emergency.19 Treatment rendered after WTC-3 submission, but prior to certification, will only be covered if the request for treatment pending certification was included in the WTC-3 submittal, the request for certification is ultimately granted, and the treatment provided is medically necessary, does not require a Level 3 Prior Authorization, follows Program guidelines, and is rendered by a CCE/NPN-affiliated provider. In the event that the condition is denied certification, any care provided for the condition that is outside the parameters of the Diagnostic Plan or Cancer Diagnostics Benefit Plan shall be discontinued immediately and the CCE or NPN providing the care will be responsible for the costs of such care.20
3.6 Decisions and Appeals
Requests to appeal a denial of authorization for treatment must be postmarked within 120 calendar days of the date of the letter from the Administrator notifying the member of the adverse decision. A valid request for an appeal must (1) be made in writing and signed; (2) identify the WTC Health Program member and designated representative (if applicable); (3) describe the decision being appealed and the reasons why the member or designated representative believes the decision is incorrect and should be reversed; and (4) be sent to the WTC Health Program at the address specified in the notice of denial.21
The description in the request may include scientific or medical information correcting factual errors that may have been submitted to the WTC Health Program by the CCE or NPN; information demonstrating that the WTC Health Program did not correctly follow or apply relevant WTC Health Program policies or procedures; or any information demonstrating that the WTC Health Program’s decision was not reasonable given the facts of the case. The basis provided in the appeal request must be sufficiently detailed and supported by information to permit a review of the appeal. Any new information not previously considered by the WTC Health Program must be included with the appeal request, unless later requested by the WTC Health Program.22
An appeal request that meets the above requirements, however, will still be considered invalid and outside the scope of the WTC Health Program’s administrative appeal process if its sole argument is a challenge to existing law, regulations, or Program policies. In other words, if the issues raised in the appeal have already been determined by law, regulation, or Program policy, then the appeal may not move forward because there are no outstanding issues for the Program to resolve with respect to the individual appellant. For example, an appeal request may not challenge a denial of certification of a health condition where the denial was based on certification requirements established in the Zadroga Act or the health condition not being included on the List of WTC-Related Health Conditions (List) in the Program’s regulation at 42 C.F.R. § 88.15 because those criteria are established by law and may only be changed by an act of Congress amending the law or the Program publishing an amendment to the regulation, respectively.
An individual wishing to voice concerns or request that the Administrator change a Program regulation or policy may write to the Administrator. An individual may also petition the Administrator to add a health condition to the List of WTC-Related Health Conditions (List); for more information on the petition process, see https://www.cdc.gov/wtc/petitions.html. The petition process can only be used to request the addition of a WTC-related health condition to the List. It cannot be used to request that the Program cover a specific health condition medically associated with a certified WTC-related health condition, cover a certain type of treatment, or amend Program regulations or policies. Changes to the Zadroga Act require an act of Congress.
When a denial of authorization for treatment is issued by the Program, the member may appeal the decision. An appeal must be made in writing within 120 calendars days from the date of the WTC Health Program’s letter notifying the member of the denial or decertification decision. The written, signed appeal request should include a full explanation of why the member (or the member’s designated representative) believes that the denial decision is incorrect. See Overview of the Appeal Process for Denial of Health Condition [PDF, 10 pages, 591KB] . The following mailing address or fax number should be used to submit a request for appeal:
Appeal Coordinator
WTC Health Program
P.O. Box 7000
Rensselaer, NY 12144
Fax: 1-404-471-8338
- Within 14 days of receiving an appeal request, the appeals coordinator will notify the individual by letter whether the appeal request is accepted or not. If the appeal request is accepted, the letter will provide the individual with the name of the Federal Official who will review the appeal. If the appeal request is not accepted, the letter will inform the individual and provide the reason(s) the appeal was not accepted.
- An individual may request the opportunity to make an oral statement to the Federal Official during the appeal review within the appeal request letter to the appeals coordinator. The individual may also request to make an oral statement within 14 calendar days of receiving the letter from the appeals coordinator notifying him/her that the appeal request was accepted.
- The Federal Official will review the appeal. If the appeal review is going to take longer than 60 calendar days from the date of the letter notifying the individual that his/her appeal request was accepted, the appeals coordinator will send a letter to the individual providing a written explanation of the delay and the estimated date the review is expected to be completed.
- The Federal Official will review all available records and assess whether the appeal should be granted. The Federal Official may consider additional relevant new information and will provide a recommendation to the Administrator of the WTC Health Program. After receipt of the Federal Official’s recommendation, the Administrator will make a final decision on the appeal. The Administrator will notify the member and/or designated representative in writing of the decision and an explanation of the reason(s) for the decision, as well as any actions taken by the WTC Health Program resulting from the decision.
- Pursuant to 42 C.F.R. § 88.25, the Administrator is permitted to reopen a final determination at any time and to affirm, vacate, or modify that determination in any manner he or she deems appropriate.
4.0 Guidelines for Covered Services
Covered services, procedures, and devices are given codes and listed in the Program Codebooks for use by CCE/NPN and network providers. Some codes include additional guidelines for use, which are listed in the Codebook. Certain subsets of services have exceptions, limitations, and/or authorization criteria, which are described in the section below.
For those services, procedures, and devices with more detailed exceptions and limitations, the Program has created Policy and Procedure (P&P) documents that broadly delineate the Program’s stance on benefit or pharmaceutical coverage, outline high-level Program procedure, or clarify current law and regulation. Some P&Ps generate more comprehensive coverage information contained in documents called Medical Coverage Determinations (MCDs). MCDs are an administrative tool which provide coverage information for specific services, along with qualifying criteria for coverage and instructions for authorization. Certain MCDs may also have applicable forms, such as prior authorization forms or reimbursement forms, intended for use by WTC Health Program providers.
The below section outlines Program guidelines for certain covered services, procedures, and devices. The content in this section undergoes regular programmatic evaluation, as the Program revises its policies and procedures to reflect the latest administrative regulations. As a result, this section may have frequent program updates or new language in development.
4.1 Acupuncture Services
Acupuncture involves the manipulation of a bodily system by inserting small needles into identified anatomical points. Acupuncture methods may also include the use of heat, pressure, friction, suction, and electromagnetic impulses. The WTC Health Program provides coverage of such acupuncture services in certain instances.
The WTC Health Program will cover medically necessary acupuncture services for members with certified WTC-related cancer when authorized by a WTC Health Program provider. The WTC Health Program follows the National Comprehensive Cancer Network (NCCN) guidelines which recommend the use of acupuncture for cancer-related pain, fatigue, nausea, and/or vomiting.
The WTC Health Program will also cover acupuncture services for members with chronic pain resulting from certified WTC-related acute traumatic injuries (ATI), musculoskeletal disorders (MSD), and health conditions causing chronic pain that are medically associated with the ATI or MSD condition. The WTC Health Program must authorize acupuncture services for ATI and MSD conditions.
Members may receive up to 12 acupuncture visits in 90 days if they meet certain criteria for authorization. Members showing improvement may receive subsequent authorization for an additional eight acupuncture visits for a total of 20 acupuncture visits during the 12-month period from the date of their first treatment.
Authorization Required – Medical Coverage Determination [PDF, 6 pages, 208 KB]
4.2 Chimeric Antigen Receptor T-cell (CAR-T) Therapy
CAR-T therapy is a type of cancer treatment that is used when standard cancer treatments have failed or cancer has relapsed. In CAR-T therapy, a type of immune system cell called a T-cell is taken from a patient’s blood and altered in the laboratory so it will attack cancer cells. Large numbers of CAR-T cells are grown in the laboratory and given to the patient by infusion. CAR-T therapy may be covered by the WTC Health Program when the services are medically necessary for the member’s certified WTC-related cancer, or health condition medically associated with a certified WTC-related cancer.
Members may receive medically necessary CAR-T therapy when they meet certain criteria for authorization. CAR-T therapy must be administered at a healthcare facility enrolled in the FDA Risk Evaluation and Mitigation Strategies (REMS) compliance program; the therapy must be used for either an FDA-approved indication or for other uses when the product has been FDA-approved and the use is supported in one or more CMS-approved compendia. Coverage of CAR-T therapy services is permitted only when in accordance with other Program guidelines.
Authorization Required – Medical Coverage Determination [PDF, 187 KB, 5 pages, September 2024]
4.3 Coverage of Conditions Outside the United States
The WTC Health Program will only cover medically necessary healthcare services within the United States and its territories, including the District of Columbia, Guam, the Commonwealth of Puerto Rico, the Northern Mariana Islands, the Virgin Islands, American Samoa, and the Trust Territory of the Pacific Islands. The WTC Health Program will not cover medical care, pharmacy products, or supplies received outside of the United States or its territories.
4.4 COVID-19
COVID-19 is a systemic respiratory disease caused by the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2 or SARS-CoV-2 infection). The virus spreads through respiratory droplets or very small particulates produced when an infected person coughs, sneezes, or talks. Some people infected may be asymptomatic. For those who are symptomatic, illness may range from mild to severe. Adults 65 years and older and people with certain underlying medical conditions are at higher risk for severe COVID-19.
The WTC Health Program may provide coverage of acute COVID-19 diagnostic and treatment services that are medically necessary to manage, ameliorate, or cure a certified WTC-related health condition or medically associated health condition and which meet relevant prior authorization criteria. The CCE/NPN Clinical Director may authorize acute COVID-19-related services only when the member meets all of the applicable requirements described in this medical coverage determination (MCD).
Authorization Required – Medical Coverage Determination – COVID-19 [PDF, 221 KB, 10 pages, July 2021]
4.5 Dental Services
The WTC Health Program provides limited coverage of medically necessary dental services for members undergoing certain cancer treatments or organ transplantation for a certified WTC-related health condition. Members receiving either a solid organ or hematopoietic stem cell transplant or cancer treatment involving radiation and chemotherapy for a certified WTC-related health condition may receive a dental exam and medically necessary dental treatment prior to undergoing the transplant or treatment. In addition, members with certified WTC-related head or neck cancers may receive additional dental services that are medically necessary to address dental trauma or other adverse effects resulting from cancer treatment.
The WTC Health Program provides coverage of medically necessary dental services only when certain criteria for authorization are met. Some dental services may be authorized by a WTC Health Program provider.
Authorization Required – Medical Coverage Determination [PDF, 158 KB, 7 pages, January 2026]
4.6 Durable Medical Equipment, Prosthetics, Orthotics and Supplies (DMEPOS)
Durable medical equipment, prosthetics, orthotics, and supplies (DMEPOS) rental or purchase is a covered health service by the WTC Health Program. The CCE/NPN Clinical Director must provide a Level 2 Prior Authorization (PA), when indicated in the WTC Health Program Codebook, Volume A, and the DMEPOS must be ordered via prescription 23 by a WTC Health Program provider or a WTC Health Program-affiliated provider to treat a certified WTC-related health condition or health condition medically associated with a certified WTC-related health condition.
-
Requirements for DMEPOS Coverage
DMEPOS is a covered health service when the member is under the care of a CCE/NPN provider or a CCE/NPN-affiliated provider; the DMEPOS is ordered by the provider via prescription; the CCE/NPN Clinical Director provides a Level 2 PA Request, when indicated in the WTC Health Program Codebook, Volume A; and the DMEPOS is to be used primarily at home to treat a certified WTC-related health condition or a health condition medically associated with a certified WTC-related health condition.
Suppliers of DMEPOS must be enrolled in Medicare and have a Medicare supplier number. The WTC Health Program will not pay a claim for equipment that is provided by a supplier that does not have a Medicare supplier number.
The following three (3) requirements must be met and documented by the CCE/NPN in order for the WTC Health Program to provide payment for the DMEPOS: 24
- The equipment meets the Medicare definition of DMEPOS; 25
- The equipment is necessary and reasonable for the treatment of the member’s certified health condition; and
- The equipment appropriate for use in the member’s home.
- Can withstand repeated use;
- Has an life expectancy of at least 3 years;
- Is primarily and customarily used to serve a medical purpose related to a certified WTC-related health condition or health condition medically associated with a certified WTC-related health condition;
- Generally is not useful to an individual in the absence of an illness or injury; and
- Is not otherwise excluded.
-
Repair, Maintenance, Replacement, and Delivery of DMEPOS
Payment may also be made for repair, maintenance, replacement, and/or delivery of medically required DMEPOS and for expendable and non-reusable items essential to the effective use of the equipment. However, payments for repair and maintenance will not include payment for parts and labor covered under a manufacturer’s or supplier’s warranty and will not exceed the cost of replacing the equipment. Replacement or repair of DMEPOS damaged as a result of misuse, abuse, and/or neglect will not be covered and is the responsibility of the member. -
Special Requirements for Power Mobility Devices
Power wheelchairs and Power Operated Vehicles (POVs)–also known as scooters–are collectively classified as Power Mobility Devices (PMDs). PMDs are defined by CMS as a covered DMEPOS item that a patient uses in the home. In order for the WTC Health Program to cover the cost of a PMD, the member must meet all three of the following criteria:26- The member has a mobility limitation that significantly impairs his or her ability to participate in one or more Mobility-Related Activities of Daily Living (MRADLs) such as toileting, feeding, dressing, grooming, or bathing in customary locations in the home; 27
- The member’s mobility limitation cannot be resolved sufficiently and safely by using an appropriately-fitted cane or walker; and
- The member does not have sufficient upper extremity function 28 to self-propel an optimally configured manual wheelchair 29 in the home to perform MRADLs during a typical day
-
Devices and Equipment Not Considered DMEPOS 30
Equipment which is primarily and customarily used for non-medical purposes may not be considered “medical” equipment for which payment can be made under the WTC Health Program. This is true even though the item has some remote medically-related use. For example, in the case of a member with lung cancer, an air conditioner might possibly be used to lower room temperature to reduce fluid loss in the patient and to restore an environment conducive to maintenance of the proper fluid balance. Nevertheless, because the primary and customary use of an air conditioner is a non-medical one, the air conditioner may not be deemed to be DMEPOS for which payment can be made.31
Other devices and equipment used for environmental control or to enhance the environmental setting in which the beneficiary is placed are not considered covered DMEPOS. These include, for example, room heaters, humidifiers, dehumidifiers, and electric air cleaners. Equipment which basically serves comfort or convenience functions, or is primarily for the convenience of a person caring for the member, such as elevators, stairway elevators, and posture chairs, do not constitute DMEPOS. Similarly, physical fitness equipment (such as an exer-cycle), first-aid or precautionary-type equipment (such as preset portable oxygen units), self-help devices (such as safety grab bars), and training equipment (such as Braille training texts) are considered nonmedical in nature. 32
The following DMEPOS are excluded from coverage under the WTC Health Program:
- DMEPOS for a member who is a patient in a type of facility that ordinarily provides the same type of DMEPOS to its patients at no additional charge in the usual course of providing its services is excluded; and
- DMEPOS with deluxe, luxury, or immaterial features which increase the cost of the item to the WTC Health Program relative to a similar item without those features.
-
Claims Submission and Processing
The CCE/NPN Clinical Director must provide a Level 2 PA Request when indicated in the WTC Health Program Codebook, Volume A. The CCE/NPN is responsible for ensuring that the DMEPOS supplier is enrolled in the WTC Health Program. The WTC Health Program will pay for a member to receive DMEPOS if all established conditions are met.
Reimbursement rates for DMEPOS are in accordance with the FECA fee schedule. Payment for DMEPOS is either on a rental or lump-sum purchase basis. In the case of rental, the item(s) are to be paid monthly.33 Separate maintenance and servicing payments are not made for any rented DMEPOS, nor are delivery and service charges for rental or purchased DMEPOS. Such costs are assumed to have been taken into account by suppliers (along with all other overhead expenses) in setting the prices they charge for covered items and services.
The WTC Health Program will continue to review available DMEPOS codes and add them to the WTC Health Program Codebook, as appropriate. DMEPOS items, with established CPT/HCPCS codes, that are prescribed and considered to be medically necessary for treatment of a member’s certified condition(s), may be requested for addition to the WTC Health Program Codebook by the CCE/NPN through the usual change request process using a WTC-5 Medical Code Request Form. If there is no established CPT/HCPCS code for a necessary DMEPOS item, the CCE/NPN should contact the HPS Contractor for guidance.
4.7 Hospitalizations
4.7.1 Emergency Room Treatment
The WTC Health Program follows the definition of emergency medical condition established in the Medicare regulations implementing the Emergency Medical Treatment and Active Labor Act (EMTALA) which define an emergency medical condition as “a medical condition manifesting itself by acute symptoms of sufficient severity (including severe pain, psychiatric disturbances and/or symptoms of substance abuse) such that the absence of immediate medical attention [via emergency care services] could reasonably be expected to result in: placing the health of the individual… in serious jeopardy; serious impairment to bodily functions; or serious dysfunction of any bodily organ or part….”34
The WTC Health Program follows the Centers for Medicare & Medicaid Services (CMS) definition of emergency care services, which are defined as “inpatient or outpatient hospital services that are necessary to prevent death or serious impairment of health and, because of the danger to life or health, require use of the most accessible hospital available and equipped to furnish those services.”35
-
CCE/NPN Authorization of Emergency Care & Claims Submission and Processing
The WTC Health Program will only cover emergency care services rendered by provider-based emergency departments (EDs) that meet state licensing requirements.36 The ED is not required to be a WTC Health Program-affiliated provider on the date of service to the member and no prior authorization is required for emergency care services. To ensure proper receipt and payment of claims, the member should inform the treating hospital/ED that the CCE/NPN should be notified of the member’s visit to the ED. When the CCE/NPN has been notified of the ED visit, or when the bill and medical records are sent from the external ED provider to the member’s CCE/NPN, the CCE/NPN will retrospectively review the ED medical records and ensure that either:-
The presenting symptom(s) for which the member appears at the ED are reasonably related to a WTC-related health condition, or health condition medically associated with a certified WTC-related health condition;
OR
- The presenting symptom(s) can be reasonably assumed to be related to the member’s 9/11 exposure history as documented in his/her medical files. This means that the symptom(s) is/are being assessed as either the initial or emergency presentation of a WTC-related health condition, or a health condition medically associated with a certified WTC-related health condition, or a health condition likely to be certified as a WTC health condition due to exposure.
Payment for treatment that is not related to a certified WTC-related health condition, or health condition medically associated with a certified WTC-related health condition, or a health condition likely to be certified as a WTC health condition due to exposure, will be denied.
Claims submitted directly to the WTC Health Program by external providers will be returned to the CCE/NPN for review and authorization.
When the CCE/NPN submits the ED claim to the WTC Health Program, the CCE/NPN is responsible for ensuring that the medical facility providing emergency services is enrolled as a provider with the WTC Health Program, through either a Single Case Agreement (SCA) or a full contract. The standard review stamp or submission through Electronic Data Interchange (EDI) represents the CCE/NPN’s acknowledgement that the CCE/NPN has an authorization on file. ED claims must be accompanied by any available medical documents/reports to facilitate the medical review. Whenever possible, ED claims should contain valid codes found in the WTC Health Program Codebook for the date of service. If after medical review, the WTC Health Program finds that codes other than those found in the WTC Health Program Codebook are acceptable for the claim, the additional charges will be paid and the Codebook will be updated accordingly. All coding and reimbursement is subject to the requirements of coding rules and guidelines in the WTC Health Program Codebook located on the Secure Access Managements services (SAMs) portal.
As with other CCE/NPN documentation, all authorizations are subject to audit and utilization reviews.
-
The presenting symptom(s) for which the member appears at the ED are reasonably related to a WTC-related health condition, or health condition medically associated with a certified WTC-related health condition;
-
Exclusions
Non-emergency visits to the ED compromise the continuity and coordination of care for individual WTC Health Program members; therefore, they are not covered by the WTC Health Program. Members should be referred back to their CCE/NPN for appropriate follow-up care.The Program will not pay for the following services provided by an emergency care provider:
- Occupational medicine;37
- routine mental health services, including counseling;
- monitoring;
- survivor screening;
- routine medical care;
- follow-up visits;
- prescription refills;
- sports and school physicals;
- travel medicine services;
- routine immunizations;
- extended pain management;
- physical and occupational therapy;
- case management and evaluation;
- routine labs and diagnostics; and
- other services as determined by the Program.
-
Claims Submission and Processing
As with other external provider bills, ER claims must be submitted through the member’s CCE/NPN. The CCE/NPN is responsible for ensuring that the medical facility providing emergency services is enrolled as a provider in the WTC Health Program. Claims submitted directly to the WTC Health Program by external providers will be returned to the CCE/NPN for review and authorization. When the ER claim is submitted to the WTC Health Program via the CCE/NPN, the standard review stamp or submission through Electronic Data Interchange (EDI) represents the CCE’s/NPN’s acknowledgement that the CCE/NPN has an ER-A on file. As with other CCE/NPN documentation, ER-As are subject to audit and utilization reviews.
ER claims must be accompanied by any available medical reports to facilitate the medical review.
Whenever possible, ER claims should contain valid codes found in the WTC Health Program Codebook for the date of service. If after medical review the WTC Health Program finds that codes other than those found in the WTC Health Program Codebook are acceptable for the claim, the additional charges will be paid and the Codebook will be updated accordingly. All coding and reimbursement is subject to requirements of coding rules and guidelines.
All ER treatment will be evaluated during the processing of the claim to ensure that treatment beyond screening and stabilization was directly related to the care of a certified WTC-related health condition, or health condition medically associated with a certified WTC-related health condition, or to an initial or emergency presentation of a condition that is likely to be certified as a WTC-related health condition (based on the exposure history on file). Payment for treatment beyond screening and stabilization that is not related to a certified WTC-related health condition or health condition medically associated with a certified WTC-related health condition, or a WTC exposure, will be denied.
-
Hospital Registration Procedures
The hospital providing emergency services may follow reasonable registration procedures once the member has been screened and stabilized. EMTALA does not prohibit an inquiry into availability of medical insurance, but it does provide that neither examination nor treatment may be delayed to make the inquiry.38 A pre-authorization requirement imposed by the WTC Health Program should not prevent or delay the performance of a medical screening evaluation or the institution of necessary stabilizing treatment once it is determined that an emergency medical condition exists. Hospitals may ask members to complete financial responsibility forms upon registration. Such forms are common practice and are standard consent forms that are signed at the time of hospital registration. These forms may result in the member being responsible for payment for services not covered by WTC Health Program.
-
Use of Emergency Facilities for Routine Care Prohibited
An ER or ED is not the appropriate medical environment for a WTC Health Program member to seek care for a routine illness. Where the member’s medical condition never was, or never appeared to be, an emergency, a physician’s office or CCE/NPN clinic, for example, would be a more appropriate and adequate medical environment for providing such non-emergency care. Non-emergency visits to the ER or ED compromise the coordination and continuity of care for individual WTC Health Program members; therefore, they are not covered by the WTC Health Program. Members should be referred back to their CCE/NPN for appropriate follow-up care. To ensure proper receipt and payment of claims, the member should inform the treating hospital/ED that the CCE/NPN should be notified of the member’s visit to the ER or ED.
Members should follow-up with their respective CCE/NPN for further treatment and monitoring following their ED visit within 14 calendar days.
4.7.2. Inpatient Hospitalization
WTC Health Program members may require hospitalization in the treatment of their covered conditions. Such treatment is covered by the WTC Health Program, in accordance with the provisions below.
-
Basis for Hospital Admission and Authorization
Only claims that relate to certified WTC-related health conditions, or health conditions medically associated with certified WTC-related health conditions, should be submitted to the WTC Health Program.
All inpatient hospitalizations require a Level 2 PA by the CCE/NPN Clinical Director, unless Level 3 PA by the WTC Health Program is required (e.g., transplants, some surgeries). (See Section 3.4, “Prior Authorizations” above for further information regarding PA requirements).
The CCE/NPN Clinical Director may authorize admission for inpatient services when the admitting diagnosis (primary diagnosis-related group [DRG] ) is directly related to the member’s certified WTC-related health condition, or directly related to a health condition medically associated with a certified WTC-related health condition. The CCE/NPN Clinical Director may also authorize admission for inpatient services when the admitting diagnosis is documented as consistent with WTC Health Program policy pertaining to diagnostic evaluation services for WTC-related conditions.39
If the hospitalization also involves a procedure that requires prior authorization by the WTC Health Program (Level 3 PA) and the CCE/NPN is aware prior to hospitalization that a Level 3 PA procedure will be performed, then the admission must be authorized by both the CCE/NPN Clinical Directorand the WTC Health Program, in accordance with established procedures for a Level 3 PA. If the need for a Level 3 PA40 procedure arises during the hospitalization, authorization will be handled on a case-by-case basis.
-
Claims Submission Requirements
Claims for inpatient hospitalizations must be submitted using standard UB-04 (CMS-1450) format or electronically using the 837 5010 ANSI standard format. Hospital-based inpatient services should be billed on the UB-04 showing revenue center charges, ICD-10 diagnosis codes, procedure codes, and the hospital's Medicare number. Inaccurate coding may cause inappropriate reimbursement, erroneous reductions in allowable amounts, and/or delays in bill processing. The physician's professional services should be coded and billed on Form CMS-1500 or the electronic equivalent.
The WTC Health Program may request detailed inpatient hospital claims, notes, and discharge summaries for some claims after submission. Failure to respond to requests for additional information related to claims for inpatient hospitalizations may result in delay in processing or denial of the claim.
The CCE/NPN is responsible for ensuring that the hospital is enrolled as a provider in the WTC Health Program. See Chapter 6 of this manual for more information regarding enrolling providers.
All acute inpatient hospital claims processed by the WTC Health Program will be priced using diagnosis-related group (DRG)-based pricing, as modified by the FECA Program. The amount paid will be the lesser of the DRG-based price or the amount billed. (See Chapter 5 for more information regarding billing of claims).
4.8 Medical Marijuana
The WTC Health Program does not cover costs associated with medical marijuana.41 Although WTC Health Program members may be able to access and purchase medical marijuana in their state of residence, its use is not approved by the FDA42 and is considered an illegal substance (Schedule 1)43 by the federal government.
4.9 Mental Healthcare
4.9.1 Inpatient Psychiatric Facilities
The Medical Coverage Determination (MCD) and coverage guidelines for this section are under development. This section will be updated once finalized.
4.9.2 Partial Hospitalizations
The Medical Coverage Determination (MCD) and coverage guidelines for this section are under development. This section will be updated once finalized.
4.9.3 Crisis Observation
The Medical Coverage Determination (MCD) and coverage guidelines for this section are under development. This section will be updated once finalized.
4.9.4 Intensive Outpatient Services
The Medical Coverage Determination (MCD) and coverage guidelines for this section are under development. This section will be updated once finalized.
4.9.5 Family Psychotherapy With and Without the Member
In certain circumstances, psychotherapy services for a member’s family may be covered as part of the treatment of the member’s certified WTC-related health condition. Family members include a parent, spouse, or child who lives in the same household as the member.
-
Diagnostic Interview
As part of a comprehensive mental health assessment with a qualified provider, a diagnostic interview session with other family members may be needed to assess the family context contributing to or being impacted by the member’s mental health related to the attacks on September 11th.
When conducted with the explicit verbal and written consent of a WTC Health Program member, a single diagnostic interview session may be billed (CPT 90791) to the WTC Health Program as part of the member’s benefit under the Diagnostics Benefit Plan in order to evaluate whether the member’s situation meets the Program’s criteria for certification. This single session may involve more than one family member, if clinically desirable.
-
Marriage or Family Counseling as Treatment
In addition, marriage or family counseling may be medically indicated to treat a WTC Health Program member’s certified mental health condition. During the course of such therapy, the non-member may require an individual therapeutic evaluation/intervention to manage traumatic reactions or trust issues emerging from the family treatment. The WTC Health Program Codebook, Volume A identifies the appropriate codes for use when marriage or family counseling is needed to treat the member’s certified mental health condition.
The WTC Health Program may provide a maximum of two family therapy sessions without the member present (CPT 90846) every 3 months for up to eight sessions in total with the expressed consent of the member for this specific reason. Use of the member’s treatment plan benefit for this purpose must be documented as medically necessary in the treatment record and a Level 2 PA by the CCE/NPN Clinical Director is required. The CMS-1500 form (or EDI equivalent) should be completed using the member’s ID number, the member’s name as the “Insured’s Name” (box 4), and the member’s name as the “Patient’s Name” (box 2). The remittance advice will reflect the member name only.
Mental health conditions detected or emerging in the non-member during the course of family therapy, including ongoing trust issues, should be referred to community resources for treatment. The WTC Health Program does not cover the cost of such treatment for non-members.
-
Treatment Providers and Claims 44
To the extent permitted under State law, mental health services can be delivered by a:
- Clinical psychologist (holds a Doctoral degree in psychology and is licensed or certified, on the basis of the Doctoral degree in psychology, in the State of practice);
- Physician (is an MD or DO, licensed in the State of practice and currently practicing within the scope of this license);
- Licensed clinical social worker (holds a Master’s level or Doctoral degree in social work, and is licensed or certified as a clinical social worker in the State of practice);
- Clinical nurse specialist (is a registered nurse, licensed in the State of practice, authorized by State law to furnish the services of a clinical nurse specialist in accordance with State law, holds a Doctor of Nursing Practice or Master’s degree in a defined clinical area of nursing from an accredited educational institution, and is certified as a clinical nurse specialist by a recognized national certifying body with established standards for clinical nurse specialists);
-
Nurse practitioner (is a registered professional nurse, licensed in the State of practice, authorized by State law to furnish the services of a nurse practitioner in accordance with State law, holds a Doctor of Nursing Practice or Master’s degree in nursing, and is certified as a nurse practitioner by a recognized national certifying body with established standards for nurse practitioners);
OR - Physician assistant (has graduated from a physician assistant educational program accredited by the Accreditation Review Commission on Education for the Physician Assistant or has passed the national certification examination administered by the National Commission on Certification of Physician Assistants, and is licensed in the State of practice).
4.10 Monoclonal Gammopathy of Undetermined Significance (MGUS)
MGUS is a condition in which abnormal levels of certain proteins are found in the blood. These abnormal levels of protein must be monitored by regular blood tests to check for any signs of cancer that could develop over time. The WTC Health Program may provide coverage of medically necessary MGUS services (i.e., initial diagnostic studies and, after diagnosis, further monitoring) when there are symptoms of a plasma cell neoplasm or clinical findings suggestive of MGUS. WTC Health Program providers may authorize a follow-up evaluation and ongoing monitoring of MGUS when the member meets all the applicable requirements. MGUS is NOT eligible for certification.
Authorization Required – Medical Coverage Determination [PDF, 6 pages, 259 KB]
4.11 Non-Invasive Neoplasms of the Cervix Uteri
Non-invasive neoplasms of the cervix uteri are ineligible for certification but further surveillance, management, and/or treatment of these conditions may be covered under the diagnostic benefit plan. Initial diagnostic studies of abnormal cervical screening results will be covered only if being used to evaluate for potential WTC-related invasive cervical cancer.
After initial diagnosis, further surveillance, management, and/or treatment may be covered for identification of potential WTC-related cervical cancer following the guidelines established by the American Society for Colposcopy and Cervical Pathology (ASCCP). These services are available under the cancer diagnostic plan for all Responders and Certified-eligible survivors. These services are available for Screening-eligible survivors during the initial health evaluation period only.
Any medically associated nonmalignant condition resulting from surveillance or management/treatment of non-invasive neoplasms of the cervix uteri is not eligible for certification or treatment. This includes any medically associated conditions that affect fertility or pregnancy outcomes. Types of non-invasive neoplasms that are ineligible for certification include cervical intraepithelial neoplasia (CIN) grades I-III and carcinoma in situ of the cervix uteri.
4.12 Post-Acute Care Services
4.12.1 Home Health Care Services
Home Health Care services are personal care and related support services that enable WTC Health Program members to live at home while receiving medically necessary care for a certified WTC-related health condition or health condition medically associated with a certified WTC-related health conditions certified by the Administrator of the WTC Health Program or Designee. Under certain circumstances, care received at home may be a substitute for receiving medically necessary care in a hospital or skilled nursing facility for members who are homebound.45
-
Homebound Defined
The Administrator of the WTC Health Program has elected to follow the definition of “confined to his home” used by CMS to determine whether a WTC Health Program member is “homebound.” In establishing conditions required for payment of services, CMS defines an individual as being “confined to his home” when:
- The individual has a condition, due to an illness or injury, that restricts the ability of the individual to leave his or her home except with the use of special transportation, the assistance of another individual, the aid of a supportive device (such as crutches, a cane, a wheelchair, or a walker), or if the individual has a condition such that leaving his or her home is medically contraindicated. While an individual does not have to be bedridden to be considered “confined to his home,” the condition of the individual should be such that there exists a normal inability to leave home and that leaving home requires a considerable and taxing effort by the individual.46
- The services are required because the individual is confined to his home and needs services or intermittent skilled nursing care;
- A plan for services has been established;
- The services are furnished while the individual is under the physician’s care; and
- Prior to the initial episode of home health care, the physician, or a nurse practitioner or clinical nurse specialist under the physician’s supervision, has had a face-to-face encounter with the individual in the past 6 months. For reauthorization of subsequent episodes, there must be a physician or physician-supervised encounter within 30 days of the beginning of the authorized episode to evaluate the need for continued home health care.
-
Requirements for Coverage of Home Health Care – Prior Authorization Level 2 PA (Level 3 PA for Home Health Aide Services)
Home health care is intended to provide treatment for an illness or injury with the goal of maintaining health. In order for a member’s home health care to be eligible for payment by the WTC Health Program, the following requirements must be met and documented by the CCE or NPN:
- The member must be under the care of a physician affiliated with a CCE or the NPN.
- The Home Health Agency (HHA) provider caring for the member must be Medicare-certified and enrolled in the WTC Health Program’s claims processing system.48
-
The CCE or NPN-affiliated network physician must provide a “plan of care” to the CCE/NPN Clinical Director for a Level 2 PA for home health services.49
-
Separate PAs Required for Each Episode of Care
The CCE or NPN Clinical Director shall provide authorizations in 60-day episodes of care. The HHA will be required to obtain additional authorization if there is a need for subsequent episodes of care. If the member still requires home health care at the end of the initial 60-day episode of care, a new authorization will be required to justify a new episode of care on day 61. Re-authorization continues to be required (the next episode would start on day 121, the next on day 181, etc.) as long as the member is receiving services under the HHA’s plan of care. More than one episode may be authorized for the same or different dates of service when there is a transfer to another HHA, or discharge with readmission to the same HHA. Authorization for service extending beyond 120 days may be subject to audit by the WTC Health Program for medical necessity.
-
Separate PAs Required for Each Episode of Care
-
The member requires the skilled services of at least one of the following:
-
Part-time or intermittent skilled nursing care50 provided by or under the supervision of a registered professional nurse (RN). To qualify as skilled nursing service, all of the following criteria must be met:
- Requires the skills of a nurse based on the inherent complexity of the service, the condition of the member and accepted standards of medical and nursing practice;
- Is performed by an RN or licensed practical nurse (LPN) under the supervision of an RN;
- Is medically necessary for the treatment of the member’s certified health condition; and
- Is either intermittent or part-time. The member has a medically predictable recurring need for skilled nursing services. This definition will be met if the member requires a skilled nursing service at least once every 60 days;
- Part-time or intermittent services of a home health aide. In general, a member is not eligible for home health aide care, including homemaker services and personal care services, if these services are not related to the member’s plan of care. However, extenuating situations may be presented in a plan of care and the required Level 3 PA for home health aide services. The reason for the visits must be to provide hands-on personal care of the member or services needed to maintain the member’s health or to facilitate treatment of the member's certified WTC-related health condition, or health condition medically associated with a certified WTC-related health condition. The information submitted should indicate the frequency of the home health aide services required. (See section D below for more information)
- Physical therapy, occupational therapy, or speech-language pathology services;
- Medical social services under the direction of a physician;
- Routine and non-routine medical supplies;
- Part-time or intermittent services of a home health aide. In general, a member is not eligible for home health aide care, including homemaker services and personal care services, if these services are not related to the member’s plan of care. However, extenuating situations may be presented in a plan of care and the required Level 3 PA for home health aide services. The reason for the visits must be to provide hands-on personal care of the member or services needed to maintain the member’s health or to facilitate treatment of the member's certified WTC-related health condition, or health condition medically associated with a certified WTC-related health condition. The information submitted should indicate the frequency of the home health aide services required. (See section D below for more information)
-
Part-time or intermittent skilled nursing care50 provided by or under the supervision of a registered professional nurse (RN). To qualify as skilled nursing service, all of the following criteria must be met:
CMS further clarifies that the individual may leave home for medical treatment or short, infrequent absences for non-medical reasons, such as attending religious services, and may still receive home health care if he/she attends adult day care. In order for a qualified service provider to be eligible for payment for home health services, CMS requires that the individual submit a written request and that an enrolled physician certify the below requirements:47
Medical social services that are provided by a qualified medical social worker or a social work assistant under the supervision of a qualified medical social worker may be covered as home health care services where the beneficiary meets the qualifying criteria specified below:
- The services of these professionals are necessary to resolve social or emotional problems that are or are expected to be an impediment to the effective treatment or rate of recovery of the member's certified WTC-related health condition or health condition medically associated with a certified WTC-related health condition; and
- The plan of care indicates how the required services necessitate the skills of a qualified social worker or a social work assistant under the supervision of a qualified medical social worker to be performed safely and effectively.
-
In general, a member is not eligible for home health aide care including personal care services. However, extenuating situations may be presented in a plan of care for a Level 3 PA review by the WTC Health Program Medical Benefits Manager. For home health aide services to be considered and covered:
- The member must meet the qualifying criteria as specified in 22B (Requirements for Coverage of Home Health Care); and
- The services provided by the home health aide must be part-time or intermittent; and
- The services must meet the definition of home health aide services in this section; and
- The services must be reasonable and necessary for the treatment of the member’s certified WTC-related health condition or health condition medically associated with a certified WTC-related health condition; and
- The reason for the visits must be to provide
-
Home Health Aide: Provision of Services Incidental to Personal Care Services (e.g. homemaker services)
When a home health aide visits a member to provide a health related service as discussed above, the home health aide may also perform some incidental services which do not meet the definition of a home health aide service (e.g., light cleaning, preparation of a meal, taking out the trash, shopping, etc.). However, the main purpose of a home health aide visit may not be to provide these incidental services as they are not health related services.
4.12.2 Hospice Care Services
Hospice provides medical, psychological, and spiritual support during end-of-life care. Hospice care53 allows the member to remain at home in a personal, comfortable setting, or in special in-patient facilities, hospitals, or nursing homes. It also supports caregivers and families with bereavement counseling. The WTC Health Program will pay for hospice services when therapies for a covered condition are no longer controlling the illness and, if the illness runs its normal course, the member’s life expectancy is 6 months or less54. If the member’s condition improves or the illness goes into remission, hospice care can be discontinued and active treatment may resume.55
-
Requirements for Coverage of Hospice Care
Acceptance into hospice care requires a Level 2 Prior Authorization (PA2) by the CCE or NPN Clinical Director specifying that the member has a life expectancy of 6 months or less if the illness runs its normal course. The member also signs a statement saying that he or she is choosing hospice care. (Hospice care can be continued if the member lives longer than 6 months, as long as the CCE or NPN Clinical Director reconfirms the member’s terminal illness and provides a new PA2 for continuity of hospice care.)
In order for a member’s hospice care to be eligible for payment by the WTC Health Program, the CCE/NPN must meet and document the following requirements:
- The member must be under the care of a CCE/NPN-affiliated physician. The hospice care must be provided from a Medicare-certified hospice program and the CCE/NPN is responsible for ensuring that the hospice program is enrolled as a provider in the WTC Health Program;
- The CCE/NPN network physician must provide a Plan of Care 56 to the CCE or NPN Clinical Director for a Level 2 PA for hospice care, which is given in benefit periods;
- The CCE or NPN Clinical Director shall initially provide a Level 2 PA for a 90-day benefit period. Additional authorization(s) are required if there is a need for subsequent hospice care (in 60-day increments); 57
- Reauthorizations of Level 2 PAs may be completed up to 15 days before the start of the next benefit period; and
- Clinical case management, including a detailed Plan of Care, for hospice members is required to ensure continuity of care during both the initial and any subsequent benefits periods.
-
Covered Services
- The following hospice services can be provided when they’re needed to care for a member’s terminal illness and related condition(s):
- Physician services
- Nursing services
- Medical equipment (such as wheelchairs or walkers)
- Medical supplies (such as bandages and catheters)
- Drugs for symptom control or pain relief
- Hospice aide and homemaker services
- Physical and occupational therapy
- Speech-language pathology services
- Medical social services
- Dietary counseling
- Grief and loss counseling for member and family
- Short-term inpatient care (for pain and symptom management)
- Short-term respite care
- Other services needed to manage pain and other symptoms related to the member’s terminal illness, as recommended by the hospice
- If receiving at-home hospice care, a member may receive inpatient respite care in a Medicare- certified facility (such as a hospice inpatient facility, hospital, or nursing home) if their usual caregiver (such as a family member) needs a rest. Members can stay up to 5 days each time they receive respite care; the member may be provided respite care up to two times per six-month coverage period.
4.12.1 Skilled Nursing/Extended Care Facilities
Extended care services are provided to WTC Health Program members who require skilled nursing or rehabilitation staff to manage, observe, and evaluate their care for a condition or conditions certified by the Administrator of the WTC Health Program or Designee. Inpatient skilled nursing facility (SNF) care, including room and board, skilled nursing care, and other customarily provided services in a Medicare-certified skilled nursing facility, are covered by the WTC Health Program when certain factors are met.58 The Administrator of the WTC Health Program has elected to follow factors similar to those used by CMS. 59
-
Requirements for Coverage of SNF/Extended Care Coverage
-
Member Need for SNF or Extended Care
All of the following conditions must be established and documented by the CCE/NPN in order for the WTC Health Program to provide payment for services:60
- The member requires daily skilled nursing services or skilled rehabilitation services that must be performed by or under the supervision of professional or technical personnel; 61
- As a practical matter, considering economy and efficiency, the daily skilled services can only be provided on an inpatient basis in a SNF; 62 and
- The services must be reasonable and necessary for the treatment of a member’s illness or injury (i.e., consistent with the nature and severity of the member’s illness or injury, the member’s particular medical needs, and accepted standards of medical practice). The service must also be reasonable in terms of duration and quality. 63
-
Additional Requirements CCE/NPN Must Establish in Order for the SNF to Qualify as a Provider
- The SNF caring for the member must be Medicare-certified, and the CCE/NPN is responsible for ensuring that the SNF admitting the member is enrolled as a provider in the WTC Health Program.
-
The CCE or NPN must also confirm that the SNF meets both of the following basic requirements:
-
The SNF must be primarily engaged in providing either:
- Skilled nursing care and related services for members who require medical or nursing care; or
- Skilled rehabilitation services for the rehabilitation of injured, disabled, or sick persons and is not primarily for the care and treatment of mental diseases.
- Skilled services must be rendered under physician orders, require the skills of qualified technical or professional health personnel such as RNs, LPNs, and/or therapists (physical, occupational, speech–language pathologists or audiologists), and must be provided directly by or under the supervision of these skilled nursing or skilled rehabilitation personnel.
-
The SNF must be primarily engaged in providing either:
-
In order for a member’s SNF care to be eligible for payment by the WTC Health Program, the CCE or NPN must meet and document each of the following requirements:
- The member must be under the care of a physician affiliated with a CCE or the NPN
-
The CCE or NPN network physician must provide a “plan of care” to the CCE/NPN Clinical Director for a level 2 PA for SNF services.64
The CCE/NPN Clinical Director shall provide an initial Level 2 PA for a 30-day SNF episode of care. The SNF will be required to obtain additional authorization(s) if there is need for subsequent episodes of care (in 30-day increments). Level 2 PA continues to be required (in 30 day increments) as long as the member is receiving SNF services.
If any one of these factors is not met, a stay in a SNF, even though it might include the delivery of some skilled services, will not be covered by the WTC Health Program.
-
Member Need for SNF or Extended Care
Extended care services are considered post-hospital if initiated within 30 days following discharge. In order to be eligible for coverage of post-hospital extended care services, the member must be receiving inpatient hospital care for a WTC Health Program certified condition for not less than 3 consecutive days of medically necessary services before discharge, and must also require a skilled level of care.
The member must also require at least one of the following: 65
- Nursing care provided by or under the supervision of a registered professional nurse;
- Physical therapy, occupational therapy, and/or speech-language pathology services;
- Medical social services;
- Drugs, biologicals, supplies, appliances, and equipment;
- Services furnished by a hospital with which the SNF has a transfer agreement in effect; 66 or
- Other services that are generally provided by (or under arrangements made by) SNFs.
The following are excluded from the SNF benefit:
- The WTC Health Program will not pay for the services of a private duty nurse or attendant. 67 An individual is not considered to be a private duty nurse or attendant if he or she is a SNF employee at the time the services are furnished.
-
Private accommodations, except in circumstances where: 68
- The member’s condition requires isolation;
- The SNF has no semiprivate or ward accommodations; or
- The SNF semiprivate and ward accommodations are fully occupied by other patients, or were so occupied at the time the member was admitted to the SNF for treatment of a condition that required immediate inpatient SNF care, and have been so occupied during the interval.
- Personal convenience items such as television, radio, or telephone in the room; 69 or
- Custodial Care. 70
- The WTC Health Program may provide coverage of medically necessary treatment for skilled nursing/extended care for a certified WTC-related health condition, or a health condition medically associated with a certified WTC-related health condition. Member must require daily skilled nursing services or skilled rehabilitation services that must be performed by or under the supervision of professional or technical personnel.
4.12.3 Long-Term Care Hospital Services
The Medical Coverage Determination (MCD) and coverage guidelines for this section are under development. This section will be updated once finalized.
4.12.4 Inpatient Rehabilitation
The Medical Coverage Determination (MCD) and coverage guidelines for this section are under development. This section will be updated once finalized.
4.12.5 Outpatient Rehabilitation
The Medical Coverage Determination (MCD) and coverage guidelines for this section are under development. This section will be updated once finalized.
4.13 Preventive Care
4.13.1 Cancer Screening
WTC Health Program cancer screening benefits are based upon guidelines recommended by the U.S. Preventive Services Task Force (USPSTF). The Program only covers cancer screening services with a USPSTF Grade A or Grade B recommendation.71 Cancer screening is currently limited to breast, cervical, colorectal, and lung cancers.
Cancer screening is available to all WTC Health Program members72 (except FDNY family members) who meet the age and risk guidelines set forth by the USPSTF. The timing and frequency of cancer screening are based on the following guidelines:
- Breast cancer screening, for eligible female members ages 40 to 74 years, once every other year via mammography.73
- Cervical cancer screening, for eligible female members ages 21 to 65 years, once every 3 years via cytology (Pap smear), OR for female members ages 30 to 65 years who want to lengthen the screening interval, once every 5 years with high-risk human papillomavirus (HPV) testing alone, or once every 5 years via a combination of cytology (Pap smear) and HPV testing.74
- Colorectal cancer screening, for all eligible members ages 45 to 75 years, with limitations on the frequency of the screening according to the specific procedure performed, which may include high sensitivity guaiac fecal occult blood test, fecal immunochemical test (FIT), stool test (DNA-FIT), CT colonography, flexible sigmoidoscopy, or colonoscopy.75 Eligible members include adults 45 years and older who do not have signs or symptoms of colorectal cancer and who are at average risk for colorectal cancer (i.e., no prior diagnosis of colorectal cancer, adenomatous polyps, or inflammatory bowel disease; no personal diagnosis or family history of known genetic disorders that predispose them to a high lifetime risk of colorectal cancer [such as Lynch syndrome or familial adenomatous polyposis]).
- Lung cancer screening, for eligible members ages 50 to 80 years with a 20 pack-year or greater smoking history who are current smokers or quit smoking in the last 15 years, once every year via low-dose chest computed tomography (CT). Screening should be discontinued once the member has not smoked for 15 years or develops a health problem that substantially limits life expectancy or the ability or willingness to have curative lung surgery.76
Exclusion criteria for all forms of cancer screening covered by the WTC Health Program are based on best medically accepted guidelines and include:
- Recent testing (diagnostic or screening) for the same cancer type being considered for screening that has been performed within the minimum recommended cancer screening interval (e.g., mammography performed within the past 24 months, colonoscopy performed within the past 10 years, etc.). A member would only be excluded from receiving the cancer screening for the duration of the minimum recommended cancer screening interval (i.e., if the screening is recommended every 12 months and the member last had a screening 6 months ago, they would be eligible for the screening in 6 months' time — 12 months from their last screening).
- Acute symptoms suggestive of the same cancer type for which screening is being considered. (Screening is for members who do not have symptoms suggestive of a possible cancer. If such symptoms are present, members need a diagnostic work-up, not screening. Diagnostic testing based on new symptoms is available to members at any time.)
- Diagnosis of advanced stage cancer, regardless of cancer type, and life expectancy of less than six months.
- Professional judgment on the part of the clinical provider that the member is unable to undergo evaluation (e.g., serious co-morbidities, estimated life expectancy of less than 5 years).
4.13.2 Immunizations
-
Vaccine Coverage Generally
The WTC Health Program may cover vaccines in limited circumstances if the condition prevented by the vaccine could worsen a WTC-related condition. If the Program determines that coverage is appropriate for a WTC-related condition, the Program benefits are based on the Centers for Disease Control and Prevention (CDC)’s Advisory Committee on Immunization Practices (ACIP) recommendations for members certified for that condition. For the immunizations described in this section, the WTC Health Program will cover both the vaccine product and the procedure to administer the vaccine when clinically indicated and advised by CDC ACIP recommendations.
-
Vaccines Covered by the WTC Health Program
The WTC Health Program provides vaccine coverage based on the member’s benefit plan. The benefit plan determines what type of medical treatment or services a member is eligible to receive, according to their member category and certification status. The table below shows what vaccines are payable under the WTC Health Program for eligible members of each benefit plan (except for FDNY family members). (For more information on benefit plans, see Section 2.0 “Approved Benefit Plans”).
| Vaccine | Survivor Screening | Diagnostics | Monitoring | Treatment | Cancer Diagnostics | Cancer Treatments |
|---|---|---|---|---|---|---|
| Influenza | Yes | Yes | Yes | Yes | Yes | Yes |
| Hepatitis A | No | No | No | No | No | Yes |
| Hepatitis B | No | No | No | Yes | No | Yes |
| Hep A & Hep B | No | No | No | No | No | Yes |
| HPV | No | No | No | No | Yes | Yes |
| Meningococcal | No | No | No | No | No | Yes |
| MMR | No | No | No | No | No | Yes |
| Prevnar13 (pneumococcal) | No | No | Yes | Yes | Yes | Yes |
| PPSV23 (pneumococcal) | No | Yes | Yes | Yes | Yes | Yes |
| Poliovirus | No | No | No | No | No | Yes |
| TD | No | No | No | No | No | Yes |
| Tdap | No | No | No | Yes | Yes | Yes |
| Varicella | No | No | No | No | No | Yes |
| Zoster | No | No | No | Yes | No | Yes |
4.13.3 Smoking Cessation Program
The WTC Health Program provides smoking cessation therapy for (1) those members with at least one certified WTC-related health condition or (2) eligible members who are current smokers and are referred as part of the lung cancer screening program. For members with at least one certified WTC-related health condition, smoking cessation therapy services will be available for use in the benefit plan for the certified condition.
For those members who are eligible though a referral from the lung cancer screening program, smoking cessation services will be accessible through the benefit plan being used at the time of the lung cancer screening. Service limitations and/or prior authorization requirements may apply if the member is not certified for at least one WTC-related health condition.
The available pharmaceutical formulary will include medications for use in conjunction with smoking cessation therapy (See Chapter 12 Pharmacy Benefits). When a member is referred for smoking cessation therapy, this information should be documented in the member’s medical record. This medical record documentation is subject to audit by the WTC Health Program.
4.14 Repetitive Transcranial Magnetic Stimulation (rTMS)
Repetitive Transcranial Magnetic Stimulation (rTMS) is a non-invasive, non-systemic treatment using an FDA-approved device to generate brief magnetic pulses that induce an electrical field in a localized region of the brain for the purpose of treating major depressive disorder (MDD) without psychosis. The technique involves placing a small electromagnetic coil over the scalp and passing a rapidly alternating current through the coil wire to produce a magnetic field that passes unimpeded through the brain.
Depending on stimulation parameters (frequency, intensity, pulse duration, stimulation site), rTMS applied to specific cortical regions can change the excitability of the affected brain structures. The procedure is usually carried out in an outpatient setting and does not require anesthesia or analgesia. When used as antidepressant therapy, rTMS produces a clinical benefit without the systemic side effects of standard oral medications and without adverse effects on cognition. Unlike electroconvulsive therapy (ECT), rTMS does not induce amnesia or intentionally induce seizures.
The WTC Health Program may provide coverage of medically necessary rTMS services which meet relevant Level 2 Prior Authorization (PA2) criteria. The CCE/NPN Clinical Director or Designee may authorize rTMS services only when there is clinical documentation that the member has MDD that is a certified WTC-related health condition or medically associated health condition, or the MDD is ancillary to another certified WTC-related health condition. Members with certain medical or psychiatric conditions may not be a candidate for rTMS treatment. Coverage of rTMS services must be in accordance with Program guidelines.
Authorization Required – Medical Coverage Determination [PDF, 582 KB, 7 pages, August 2023]
rTMS PA2 Request Form for Providers [PDF, 1140 KB, 6 pages, September 2023]
4.15 Routine Medical Care
The WTC Health Program only covers medically necessary treatment for certified WTC-related health conditions or medically associated conditions that result from treatment or progression of a certified condition. The Program does not cover routine medical care. Members should always maintain their own primary care provider for health conditions not covered by the Program.
4.16 Second Opinions
Member-initiated second opinions by a CCE/NPN-affiliated provider may be covered by the WTC Health Program only when assessing the medical need for a covered surgery or for major nonsurgical diagnostic and therapeutic procedures (e.g., invasive diagnostic techniques such as biopsy or differing therapeutic options for a covered cancer). Second opinions may be covered to address the appropriate approach to evaluating allowable clinical findings, as consistent with policies for managing (treating) a member’s certified health condition(s).
In the event that the recommendation of the first and second physician differs regarding the need for surgery (or other major procedure), a third opinion may also be covered. Second and third opinions are covered even if a therapeutic modality under consideration is not covered by the WTC Health Program. Payment may be made for the history and examination of the member, and for other covered diagnostic services required to properly evaluate the member’s need for a procedure and to render a professional opinion.
4.17 Sleep Apnea
Sleep apnea is a common sleep disorder characterized by brief interruptions of breathing during sleep. The most common type of sleep apnea is obstructive sleep apnea (OSA). OSA occurs when the upper airway collapses or becomes blocked during sleep, thus reducing or stopping airflow. Central sleep apnea (CSA) is caused by irregularities in the brain’s normal signals to breathe. Most people with sleep apnea will have a combination of both types.
Sleep apnea may be covered by the WTC Health Program in three different ways: as a certified WTC-related health condition included on the List of WTC-Related Health Conditions (List), as a health condition medically associated with a certified WTC-related condition, or where medically necessary to treat certain certified WTC-related health conditions.
Medical Coverage Determination – Sleep Apnea [PDF, 309 KB, 12 pages, December 2021]
4.18 Solid Organ Transplants
WTC Health Program policies regarding solid organ transplants are consistent with best clinical practices and nationally recognized guidelines.
The WTC Health Program may cover solid organ transplants if specific requirements are met and a Level 3 PA is in place. The transplant must be non-experimental and non-investigational. The specific medical condition(s) being treated by the solid organ transplant must be certified by the WTC Health Program and must be a contributory cause to the deterioration of the organ being transplanted. The specific medical condition(s) being treated with the solid organ transplant must be shown to be chronic and severe/end-stage despite maximal treatment with other known standard treatment options. The solid organ transplant should be considered to have a high likelihood of a positive health outcome, with potential benefits effectively outweighing any potential harms. All appropriate indications and absolute and relative contraindications must be considered. All pre-transplant and transplant services must be non-experimental, non-investigational procedures, and all other WTC Health Program requirements must be met. All pre-transplant and transplant authorizations and services are subject to WTC Health Program utilization review and/or audit. The CCE/NPN Clinical Director should consult with the WTC Health Program Medical Benefits Team regarding additional requirements related to specific solid organ transplant requests.
-
Transplant Request Denials
Denials of requests for transplants are subject to appeal by the member, pursuant to regulation, as a denial of medically necessary treatment. Appeal rights will be provided when the outcome of the WTC Health Program evaluation is a denial decision (See Section 3.6 for additional information on appeals).
4.19 Surgeries
Diagnostic and reparative surgeries requiring inpatient hospitalization are covered by the Program for a certified WTC-related health condition or a health condition medically associated with a certified WTC-related health condition. Surgeries requiring inpatient hospitalization are generally subject to a PA2 by the CCE/NPN Clinical Director in accordance with medical protocols and Program policy.
Surgical procedures related to transplants, dental surgeries, or cancer treatment may require a higher level of authorization. Transplants and certain head and neck surgeries require a PA3 from the Program. The WTC Health Program Codebook, Volume A should be consulted to determine the PA level for any surgery.
4.20 Transportation Services
4.20.1 Emergency Transportation
The Medical Coverage Determination (MCD) and coverage guidelines for this section are under development. This section will be updated once finalized.
4.20.2 Non-Emergency General Transportation Services for NPN Members
The WTC Health Program may provide members assigned to the Nationwide Provider Network (NPN) coverage of expenses for necessary and reasonable, non-emergency general transportation services, and those expenses that are incident to the necessary and reasonable, non-emergency general transportation. This transportation must be for the purpose of the member securing medically necessary treatment for a certified WTC-related health condition, or a health condition medically associated with a certified WTC-related health condition. In addition, the travel must exceed 250 miles roundtrip from the member’s place of residence or a WTC Health Program-affiliated healthcare facility or office to a WTC Health Program-affiliated healthcare facility or office. Travel is reimbursed according to General Services Administration (GSA) rates and practices.
Authorization Required – Medical Coverage Determination [6 pages, 531 KB]
4.20.3 Non-Emergency Medical Transportation Services for All Members
The WTC Health Program only provides coverage of medically necessary, non-emergency medical transportation services by ambulette or ambulance for members when it is determined that no other means of transportation could be used without posing a threat to the member’s survival or seriously endangering the member’s health.
Any expenses must be for the purpose of the member accessing medically necessary treatment from a CCE- or NPN-affiliated provider for a certified WTC-related health condition, or a health condition medically associated with a certified WTC-related health condition.
The WTC Health Program does not pay for expenses incident to medically necessary, non-emergency medical transportation services for a CCE- or NPN-assigned member.
Authorization Required – Medical Coverage Determination [6 pages, 632 KB]
Applicable Forms
- Non-Emergency Medical Transportation PA3 Request Form [3 pages, 207 KB]
- Non-Emergency Medical Transportation PA3 Reimbursement Form Policy and Procedure [1 pages, 165 KB]
4.21 Urgent Care
An urgent medical condition is not considered an emergency, but requires medical services to be furnished within 12 hours to avoid the likely onset of an emergency medical condition. In contrast, emergency services are immediately necessary to prevent serious health impairment or death.77
-
Urgent Care Facilities
Urgent care facilities are facilities outside of a traditional hospital or a freestanding emergency department that includes freestanding, walk-in ambulatory clinics generally open seven days per week with extended hours. Urgent care facilities provide immediate medical treatment and unscheduled, episodic care to individuals who require care within a 12-hour period, but whose condition requires immediate treatment to avoid the onset of an emergency condition.78 Members who visit an urgent care center who need a higher level of service will be referred to a specialist or an Emergency Department (ED). Acutely ill members may be transferred by ambulance through activation of the 911 system because most urgent care centers are not equipped or staffed to handle life-threatening emergencies.
-
CCE/NPN Authorization of Urgent Care & Claims Submission and Processing
The urgent care facility rendering urgent care services is not required to be a WTC Health Program-affiliated provider on the date of service to the member. No prior authorization is required for urgent care services. To ensure proper receipt and payment of claims, the member should have the urgent care facility notify the CCE/NPN of their visit. NPN members should present their WTC Health Program membership card to the urgent care facility to ensure proper billing. The CCE/NPN should remind members of their responsibility in directing urgent care providers to the CCE/NPN to coordinate payment for allowable care. Claims submitted directly to the WTC Health Program by external providers will be directed to the CCE/NPN for medical necessity review.
When the CCE/NPN has been notified of the urgent care visit, or when the bill and medical records are sent from the external urgent care provider to the Program, the CCE/NPN will retrospectively review the urgent care medical records and ensure that the treatment was related to a certified WTC-related health condition or a health condition medically associated with a certified WTC-related health condition. Payment for treatment determined not to be medically necessary for the member's certified condition(s) will be denied.
When the CCE/NPN submits an urgent care claim to the WTC Health Program, the CCE/NPN shall make all attempts to recruit the medical facility into providing urgent care services through a full provider agreement. If the provider is unwilling to fully enroll with the WTC Health Program under the Program Terms and Conditions, the provider may be considered for a Single Case Agreement (SCA) or Letter of Agreement (LOA). All outreach efforts must be documented. The standard review stamp or submission through Electronic Data Interchange (EDI) represents the CCE’s/NPN’s acknowledgement that the urgent care services were medically necessary for the member’s covered condition(s). Urgent care claims must be accompanied by any available medical documents/reports to facilitate the medical review. Whenever possible, urgent care claims should contain valid codes found in the WTC Health Program Codebook for the date of service. If the codes are not in the WTC Health Program Codebook, the claim will auto-deny. In such cases, CCE/NPN providers may request coverage for claims they determine are medically necessary following the medical code change request process outlined in Section 3.3 of this Chapter. All coding and reimbursements are subject to the requirements of coding rules and guidelines in the WTC Health Program Codebook located on the Program’s Centralized Accessible Real-Time Enterprise (CARE) Portal.
All documentation for completed urgent care services is subject to audit and utilization reviews by the Program.
-
Urgent Care Services
Where determined to be related to a certified WTC-related health condition or a health condition medically associated with a certified WTC-related health condition, WTC Health Program coverage of urgent care services may include orthopedic-related services, onsite laboratory and diagnostic testing, pharmacy services, and other treatments and services (e.g., intravenous (IV) fluids). Coverage of urgent care services is permitted only when in accordance with the WTC Health Program Pharmacy Formulary and other Program guidelines.79
Some examples of urgent medical conditions may include, but are not limited to:
- Breathing difficulties, such as mild to moderate asthma
- Severe sore throat
- Severe cough
-
On-Site Laboratory and Diagnostic Tests
A range of laboratory and diagnostic tests may be provided to a member during an urgent care visit. A laboratory test is a medical procedure that involves testing a sample of blood, urine, or other substance from the body. Laboratory tests can help make a diagnosis, plan treatment, verify treatment success, or monitor the disease course.80 A diagnostic test is a type of test used to diagnose a disease or condition.81 Examples include endoscopy, biopsy, and imaging tests such as CT scans, mammography, x-rays, and ultrasounds. In general, when an urgent care provider orders a laboratory or diagnostic test for a member, this test is used to make a diagnosis and create a treatment plan. Members should follow-up with their CCE/NPN for further treatment and monitoring within 14 calendar days of their urgent care visit.
-
Orthopedic Services
Orthopedic services focus on injuries and diseases of the body’s musculoskeletal system.82 Examples of orthopedic services that may be provided at an urgent care center include treatment of musculoskeletal injuries that occur as a result of a WTC-related health condition, or a health condition medically associated with a certified WTC-related health condition.
-
Pharmacy Services
Pharmacy services (including prepackaged pharmaceuticals and limited pain management) may be covered in an urgent care when an urgent care provider prescribes medication to treat an urgent medical problem, to manage, ameliorate, or cure a certified WTC-related health condition or health condition medically associated with a certified WTC-related health condition. Only drugs included in the WTC Health Program Pharmacy Formulary are eligible for coverage in the Program. In some cases, the CCE/NPN may need to approve the prescriptions due to providers not being in-network.
-
Other Treatments and Services
Other urgent care treatments and services which may be provided to a member include but are not limited to intravenous fluids.
-
Exclusions
Non-urgent visits to an urgent care center are generally not covered by the WTC Health Program. Non-urgent visits to an urgent care center can compromise the coordination and continuity of care for individual WTC Health Program members and are not cost-effective. If the services provided at an urgent care center visit are determined not to be covered, the member will be responsible for covering the cost through other means (i.e., other health insurance).
The Program will generally not pay for the following services provided at an urgent care facility:
- occupational medicine;83
- routine mental health services, including counseling;
- monitoring exams;
- initial health evaluations (survivor screening);
- routine medical care;
- follow-up visits;
- routine prescription refills;
- routine immunizations;
- extended pain management;
- physical and occupational therapy;
- case management and evaluation;
- routine labs and diagnostics; and
- others as determined by the Program.
In limited situations, urgent care centers may offer non-urgent, routine services, such as survivor screenings, monitoring exams, and routine blood work in addition to the urgent and emergent services described above. When appropriate, members will be referred for these services directly by their CCE/NPN only when the urgent care facility fees are billed according to Program requirements as standard treatment.
Members should follow-up with their CCE/NPN for further treatment and/or monitoring within 14 calendar days following their urgent care visit.
4.22 Uterine Cancer
Uterine cancer is a common term for cancer of the female reproductive tract. Uterine cancer is also referred to as endometrial cancer since it occurs in the inner lining of the uterine body called the endometrium.
The WTC Health Program covers medically necessary treatment of certified endometrial cancer following the clinical practice guidelines set forth by the National Comprehensive Cancer Network (NCCN).
The WTC Health Program also covers medically necessary treatment of atypical endometrial hyperplasia, also known as EIN. EIN is an abnormal change in the uterine lining that can lead to cancer of the uterus.
The WTC Health Program may authorize fertility-sparing treatment via hormone-based therapy when requested by a WTC Health Program provider for members with certified low-grade endometrial cancer or EIN. Coverage of fertility-sparing treatment is limited to those services related to endometrial disease only. Coverage includes appropriate clinical counseling, additional diagnostics as needed, medically necessary hormonal therapy, and follow-up disease surveillance per NCCN guidelines. Certain criteria must be met for the Program to authorize coverage of fertility-sparing treatment.
Authorization Required – Medical Coverage Determination [PDF, 6 pages, 223 KB]
5. Appendices
4-B WTC-5 Medical Code Request Form
4-C Home Health Care CMS Form 485
4-D Policy and Procedures for Cancer Screening
Chapter 5—Claims Processing and Billing
TABLE OF CONTENTS
Last Revised – August 2014
- Purpose and Scope
- Statutory and Regulatory References
- Responsibilities
- Overview
- EDI Claims
- Pharmacy
- Fee Schedule
- Billing
- Unlisted and Miscellaneous Procedure Codes
- Payments and Remittance Advice
- Payment Reporting
- Payment Reconciliation and Auditing
- Appeal of Reimbursement Denial
-
Appendices
Appendix 5-A—CMS-1500
Appendix 5-B—UB-04
Appendix 5-C Policy and Procedures for Coordination of Benefits for Treatment Costs for Non-Work-Related, Certified WTC-Related Health Conditions: Coordination with Health Insurance
Appendix 5-D Policy and Procedures for Recoupment: Lump-Sum Workers' Compensation Settlements
Appendix 5-E Policy and Procedures for Recoupment & Coordination of Benefits: Workers’ Compensation Payment
1. Purpose and Scope
This Chapter provides a high level overview of the process for submitting and processing claims for medical benefits under the WTC Health Program. This process is managed by the Health Program Support (HPS) contractor. A more complete description of the claims processing function is found in the WTC Health Program Claims Processing Procedure Manual, found in the WTC Health Program file of record.
2. Statutory and Regulatory References
The sections of the Public Health Service (PHS) Act applicable to this Chapter include Section 3312(c), Payment for Initial Health Evaluation, Monitoring, and Treatment of WTC-Related Health Conditions, and Section 3331, Payment of Claims. The sections of the WTC Health Program regulations applicable to this Chapter include 42 C.F.R. §§ 88.20, 88.22, 88.23.
3. Responsibilities
The parties involved in developing, submitting, processing, and paying claims are described below.
- The Clinical Centers of Excellence (CCEs) and Nationwide Provider Network (NPN) develop and submit claims for medical benefits to the WTC Health Program HPS contractor and ensure that they are submitted in accordance with established requirements and guidelines, described further in Chapter 4. The CCEs/NPN provide and make referrals to affiliated external medical providers to provide treatment, monitoring, and screening services. They authorize medical treatment, monitoring, and screening services. Additionally, they provide information to the HPS contractor to enable it to enroll external medical providers in the WTC Health Program, and validate the professional qualifications of those providers. Some of the CCE/NPN functions may be performed by a third party administrator (TPA), if engaged by the CCEs/NPN.
- The HPS contractor receives and processes claims for medical benefits, resolves claims that pend due to system edits (for example, when a claim requires review by the Medical Benefits Manager (MBM) or requires follow up for missing information), prices claims, generates the data used to make payments to medical providers, submits a weekly payment file to the payment contractor using a standard format, and maintains the provider file for the WTC Health Program. The HPS contractor works with the submitting CCE/NPN, when necessary, to resolve any issues preventing successful processing of the claim and works with the payment contractor to resolve any issues identified with the payment file. The HPS contractor also creates and provides special reports regarding claims outcomes to the CCEs/NPN, and notifies the CCEs/NPN of any issues encountered by the payment contractor that might impact payments.
- The Centers for Medicare & Medicaid Services (CMS) payment contractor receives the payment file from the HPS contractor and issues payments via Electronic File Transfer (EFT) to providers. The payment contractor also issues Remittance Advices (RAs), documents that provide notice of and reasons for payment, adjustment, denial and/or uncovered charges of a claim, to the medical providers. The payment contractor then communicates payment information back to the HPS contractor, notifying the HPS contractor if there are any problems with the payment data. To ensure compliance with requirements in the Zadroga Act (Section 3306(14)(B)), the payment contractor is engaged via an inter-agency agreement with CMS.
- The MBM reviews and takes actions on medical claims appeals and is in the process of establishing a more formal process for appeals of reimbursement denials (see section 13 of this chapter).
- The electronic data interchange (EDI) clearing house provides a mechanism for medical claims to be transmitted electronically between CCEs/NPN and the HPS contractor.
- The pharmacy benefits manager (PBM) receives claims from the pharmacies, applies adjudication rules according to standards developed by the WTC Health Program, and compiles and communicates payment and denial data.
4. Overview
The Program uses Plexis Healthcare System’s Quantum Choice claims processing software to manage enrollee and provider information and to process claims. The claims processing function is scaled to the relatively small size of the WTC Health Program and is designed to quickly, efficiently, and accurately process claims submitted for payment, in accordance with the provisions of the Act.
- The various functions in the payment process are separated both physically and functionally, in accordance with industry best practices. The HPS contractor maintains separation of functions by having different teams for mail handling and imaging, enrollment, eligibility, claims processing, provider enrollment, and auditing. In this way, the risk of fraud is minimized, since no one individual/team can both submit and approve or pay a claim.
- Medical monitoring and treatment claims are submitted to the HPS contractor either by or through the CCEs/NPN or subcontractors, such as a TPA, working on behalf of the CCEs/NPN.
- Claims are submitted in a variety of ways, depending on the CCEs’ preferences and technical infrastructure. They are accepted when submitted using one of the following methods: (1) on paper using the appropriate forms (i.e., CMS-1500 or UB-04); (2) on spreadsheets that have been structured to capture the data required by the CMS-1500 or UB-04 form; or (3) electronically through EDI.
- The CMS-1500 form (seen in Appendix 5-A) is used by outpatient healthcare professionals and suppliers and the UB-04 (seen in Appendix 5-B) is used by healthcare institutions (such as hospitals, rehabilitation centers, and skilled nursing facilities). Both are standard forms developed by CMS and used regularly in other federal programs such as Medicare. The WTC Provider Manual provides guidance on how the forms are to be completed for claims under the Program.
- Paper claims are first created or, in the case of claims coming from affiliated external providers, reviewed by the CCEs/NPN, then approved for submission. The CCEs/NPN indicate their authorization of a claim by affixing a special authorization stamp or by attaching a notice of authorization. The claims are then mailed or faxed to the HPS contactor, which scans the paper claim and uploads the images to a secure server so that the claims processing staff can access and enter the data into the claims processing system.
- Claims submitted using structured spreadsheets are sent directly to the claims processing team by the CCE/NPN, along with its authorization, using a secure server. The claims processing team is notified of the transmission by the data management team, and processes the data in the same manner as paper claims.
- EDI claims are sent to the HPS contractor electronically using the 837 5010 American National Standards Institute (ANSI) standard format, and are uploaded into the claims processing system. When a CCE submits EDI claims using the approved process, it acknowledges that the claims are authorized to be paid. EDI claims received from external providers are pended, and a report is forwarded to the providers’ associated CCE/NPN to obtain their authorization so that the claims can be processed.
- All claims are processed by the HPS contractor using the system configurations and processes developed for use by the Program. Data from the enrollment and certification processes are used along with other industry-standard and WTC Health Program-specific parameters to determine whether the claim is payable. Certain types of claims, such as inpatient care, emergency room visits, and cancer treatment, are reviewed by the MBM for approval before they are paid. Claims may also pend for review for other reasons, such as when additional information is needed to complete the claim. Payable claims are priced according to the fee schedule, described in section 8 below. Additional information concerning the claims process may be found in the WTC Health Program Claims Operations Manual, located in the WTC Health Program file of record.
- The HPS contractor compiles data from the claims processing system for both approved and denied claims, which are transmitted to the payment contractor on a weekly basis. Payments to providers are issued weekly via EFT. The payment contractor also issues the RAs for claims. Section 10 below provides more detail.
- Pharmacy claims are submitted electronically by the pharmacies to the PBM and are then sent to the HPS contractor weekly for further processing. After the HPS contractor forwards a payment file to the payment contractor, the payment contractor issues payments to the PBM, which then forwards the payments to the pharmacies.
- Payment reconciliation, payment adjustments, and audits are performed by the HPS contractor, as further described in section 10 below.
5. EDI Claims
Approximately 90 percent of all claims are submitted to the HPS contractor via EDI using the 837 5010 ANSI standard format. The Program encourages use of EDI as it improves the efficiency and effectiveness of claims processing, reduces the potential for error, and speeds transaction times. CCEs/NPN, their TPAs, and approved external providers submit claims to the EDI clearing house using the 837 format. The clearing house then delivers the claims to the HPS contractor for claims processing.
6. Pharmacy
Prescriptions covered under the Program are issued in accordance with the WTC Health Program-approved pharmaceutical guidelines and the Program’s formulary. The formulary and guidelines are aligned with the Program’s pharmacy benefit plans, which are described in WTC Health Program Bulletin No. 13-2, “Implementing Pharmacy Benefit Plans by Health Condition Certification Status.” These plans, implemented to improve programmatic oversight and minimize fraud, waste and abuse, are documented in the WTC Health Program file of record.
- Prescription drugs are approved at the point of sale (POS). Members provide their WTC Health Program coverage information to the pharmacy, which validates their enrollment through the PBM. The PBM also checks to ensure that the prescribing provider is authorized to prescribe under the Program and that the prescribed drug is covered under the WTC Health Program formulary. After filling the prescription, the pharmacy submits claims electronically to the PBM. Pharmacy claims data are accumulated on a weekly basis and transmitted by the PBM to the HPS contractor which processes the claims and sends them to the payment contractor. The payment contractor pays the PBM, which then issues payments to the pharmacies.
- If the prescription is rejected at the POS, the rejection may be overridden, when necessary, by the CCEs/NPN or by the HPS contractor’s pharmacy team after consultation with the CCE/NPN. CCEs/NPN have access to an online program offered by the PBM which allows online adjudication of pharmacy transactions. Inquiries regarding rejected prescriptions are received via the Program’s Call Center, which either resolves the reason for the rejection (e.g., the pharmacy has an incorrect enrollee number) or routes the issue to the HPS’ Member Services team for resolution.
- The WTC Health Program’s pharmacy network is open, and any pharmacy may submit a claim to the WTC Health Program.
- The physicians who are permitted to prescribe under the WTC Health Program are limited to those providers who have been authorized by the CCEs. Weekly updates of permitted prescribers are sent by the CCEs to the PBM, which shares this information with the HPS contractor. If a provider is permitted to prescribe medications under the WTC Health Program, the provider’s prescriber status is recorded in the claims processing system’s Provider Module.
- Prescription drugs may also be provided through mail-order. Mail-order is encouraged, when feasible, as it adds efficiency to the Program. The member must register and can do soat the mail-order provider’s Website online, via telephone, or through the CCE/NPN. Once the member is registered, the prescribing physician can e-prescribe, fax, or mail the prescription to the mail-order provider. Mail-order is generally used for maintenance medications only, and they are provided in a 90-day supply. Once a prescription is filled through the mail-order service, the member receives a form for refill. Refills may also be obtained online or by phone, and members may elect to auto-refill. To ensure accuracy and prevent fraud, prescribers cannot call in an initial mail-order prescription.
- In response to concerns about significant barriers to care for members with systemic cancers that are likely to receive their care through extended care networks (affiliated with but separate from the CCE/NPN), the WTC Health Program broadly expanded the therapeutic classes available in the Cancer Treatment Pharmacy Plan, opened the prescriber network, and removed prior authorization restrictions. To assist in the alignment of certification activities justifying drug coverage or member counseling about the pharmacy benefit, the CCEs and the NPN conduct weekly retrospective drug utilization reviews for these members as part of their quality assurance activities.
- Pharmacy claims must be submitted within 180 days of the fill date. Older claims must have prior authorization, in order to help prevent untimely filing of claims.
- Prescription medications are available according to the pharmacy benefit plan to which the member is assigned. Medications that are covered under the WTC Health Program are listed in the formulary (Part C of the WTC Health Program Codebook).
7. Fee Schedule
- The Zadroga Act requires that the payment rate for an initial health evaluation, medical monitoring, and/or medically necessary treatment or services for a WTC-related or medically associated health condition be in accordance with the rates paid under the Federal Employees’ Compensation Act (FECA), administered by the U.S. Department of Labor (DOL). Pursuant to 42 C.F.R. § 88.22(b), treatment for which FECA rates have not been established will be reimbursed at the applicable Medicare fee for service rate, as determined appropriate by the Administrator. Treatment for which neither FECA nor Medicare fee for service rates have been established will be reimbursed at rates determined appropriate by the Administrator. More information about FECA, including the methodologies used to calculate FECA rates, can be found at https://www.dol.gov/agencies/owcp/regs/feeschedule/fee . Maximum payments under the WTC Health Program are the lesser of the calculated fee schedule amount or the billed amount.
- The WTC Health Program also follows DOL’s medical fee schedule used by the FECA program for covering inpatient hospital services. These services are subject to a reimbursement schedule based on the Medicare Inpatient Prospective Payment System (IPPS). That system assigns services to Diagnosis-Related Groups (DRGs) and adjusts rates for individual hospitals according to their specific cost index. Inpatient services not covered under the Medicare IPPS are reimbursed under a formula that is based on the cost-to-charge ratio (CCR) data tables published by CMS for rural and urban hospitals in each state. The full explanation of how fees are calculated under FECA may be found at: https://www.dol.gov/owcp/regs/feeschedule/fee/fee12/READ_ME_FIRST_fs12_instructions.htm .
8. Billing
As noted in the Overview above and in Chapter 4, Medical Benefits, billing for covered services under the program is consistent with industry best practices and uses standard procedures and forms. The categories of health conditions are defined by ICD-10 diagnosis codes. The medical services associated with each covered condition/diagnosis code are defined by Current Procedural Terminology (CPT), Healthcare Common Procedure Coding System (HCPCS), DRG, and Revenue Coding Center (RCC) codes. These codes, documented appropriately on standard CMS-1500, UB-04, and EDI claims, are the basis by which member claims are paid. The codes acceptable for submission of claims for healthcare services for covered conditions under the Program have been defined and are documented in the Codebook, found in the WTC Health Program file of record.
9. Unlisted and Miscellaneous Procedure Codes
Special circumstances apply when considering the use of a procedure or service code that is not currently listed in the Codebook.
- Unlisted codes are CPT or HCPCS codes that are not associated with a specific procedure or service. Miscellaneous codes are used for procedures, devices or supplies, and services that have not been assigned a unique CPT code. Because both of these types of codes are not usually associated with a single service, they are typically not priced and reimbursement must be determined on a case-by-case basis. Providers should only use these codes when a more specific code is not available. The unlisted codes provide the means of reporting and tracking services and procedures until a more specific code is established, and are not typically used for reimbursement purposes. When these codes are used, they should be accompanied by documentation to support medical necessity. The MBM will determine on a case-by-case basis whether a particular code will be covered and, if covered, the Program price the code depending on the procedure or service performed.
- If a CCE/NPN requests that an unlisted code or miscellaneous code be added to the WTC Health Program Codebook through the medical change request process, the Program’s Medical Benefits Team will determine if there is a more appropriate procedure or service code available that closely approximates the service or procedures needed to be performed.
- Since unlisted codes and miscellaneous codes lack definition, they will be reviewed by the WTC Health Program for proper code use. All unlisted and miscellaneous codes require supporting documentation, which must be submitted with the claim to facilitate review as to code use justification. If use of the code is justified, the claim will be approved, and a reimbursement amount will be calculated. In the course of the medical review process, the WTC Health Program may ask for additional documentation.
-
When submitting supporting documentation, the medical provider or CCE/NPN should underline or highlight the portion of the note or report that identifies the test or procedure associated with the unlisted or miscellaneous procedure code. Required information must be legible and clearly marked. Documentation must clearly describe a condition and the medical need for the procedure or service. It should also include an explanation of the following:
- Whether the service was performed alone or in conjunction with other services;
- Whether the procedure was performed at the same surgical site or through the same surgical opening as another procedure;
- Any extenuating circumstances which may have complicated the service or procedure;
- The time, effort, and equipment necessary to provide the service;
- The number of times the service was provided; and
- Evidence of cost or charges expected for the procedure.
- No fee schedule amount has been established for unlisted and miscellaneous codes, and they are carried in the system as having a zero dollar amount. If use of the code is approved, the amount payable for the service will be determined on a case-by-case basis, using the documentation provided by the submitter. Therefore, it is important for the submitter to provide enough detail on the cost and charges for the unlisted or miscellaneous procedure so that the Program is able to arrive at a reasonable decision regarding the reimbursable amount.
- No additional reimbursement is provided for special techniques/equipment submitted with an approved unlisted procedure code.
- Unlisted CPT-4 procedure codes should not be billed with a modifier or they will be denied. However, unlisted codes for DME, orthotics, and prosthetics require appropriate NU (for new equipment), RR (for rental equipment) or MS (for maintenance and servicing) modifiers.
- When performing two or more procedures that require the use of the same unlisted CPT code, the unlisted code should only be reported once to identify the services provided (excludes unlisted HCPCS codes—for example, DME/unlisted drugs). If the procedures or services are the same, then the code would be listed once and the units used to describe how many times the service or procedure was performed or rendered. If the procedures or services are different, but require the use of the same unlisted code, then the additional instance of the code must be billed in a separate claim.
- If claims with unlisted or miscellaneous procedure codes are submitted without supporting documentation, a reasonable attempt will be made by the Program to obtain supporting documentation. If no documentation is forthcoming, or documentation is insufficient, the claim will be denied.
- The Program will not routinely accept retrospectively amended medical records or physician queries beyond 60 days from the service date. The Program determines the extent of medical documentation required to support use of the code as a basis for coverage or reimbursement upon review or physician query.
- Clinical documentation or physician queries amended over 60 days from the service will not be accepted to defend reimbursement, increase reimbursement, or consider a previously denied claim. If there are extenuating circumstances, the CCE/NPN must contact the Program to present their circumstances, and the Program will consider each situation on a case by case basis.
-
The following chart shows the type of documentation required for different codes (in addition to the list found in item d above):
Procedure Code Documentation 10021–69990:
Surgical ProceduresOperative or Procedure Report 70010–79999:
Radiology/Imaging ProceduresImaging Report 80048–89356:
Laboratory & Pathology ProceduresLaboratory or Pathology Report 90281–99602:
Medical ProceduresOffice Notes and Report Unlisted DME HCPCS Codes:
Equipment/SupplyProvide Narrative on the Claim
10. Payments and Remittance Advice
On a weekly basis, claim lines are gathered into a claim payment run (or file) which is transmitted to the payment contractor. The process is outlined in the below graphic.
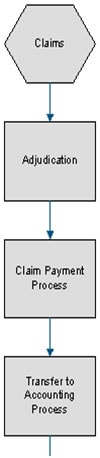
Claims are adjudicated to determine net pay amounts. Claim lines are pulled into Claim Payment Runs to be transferred to accounting.
The Transfer to Accounting Process (TAP) pulls in Claim Payment Runs and creates an AP Accounting Transaction for each amount. Accounts are assigned to transactions based on the user-defined account assignments. All available transactions created by TAP are bundled into payments ready to be paid. Manual payments and transactions may also be created.
- The HPS contractor forwards two files to the payment contractor—a file that generates payments and a file to generate RAs.
- The payment contractor runs the data through a series of edits to ensure 1) format compliance and 2) correct calculations for payments. It also conducts a “pre-note” process, in which it sends a $0 payment to each provider’s bank account to verify all banking information. If any errors are found, the payment contractor notifies the HPS contractor so that their Member Services team can be engaged to correct the information.
- The payment contractor then processes the data through established channels at CMS to send a payment file to the Treasury Department, which issues EFT payments to the providers. The payment contractor issues RAs detailing the claims processing outcomes to providers in either an electronic or paper format, or both, depending on the provider’s preference.
- The payment contractor sends a confirmation file back to the HPS contractor after each week’s payment run which documents what was paid and whether any payments were rejected. The HPS contractor then updates the claims processing software with this data so that the status of all claims can be tracked.
- Payments for pharmaceuticals are sent to the PBM, which forwards them to the dispensing pharmacies.
11. Payment Reporting
Using MicroStrategy’s business intelligence reporting tool, Microstrategy 9, and Quantum Choice, a variety of reports are generated to provide the WTC Health Program insight into the claims and payments processed, and to ensure quality assurance of the claims processing function.
- Claims and payment reports for the WTC Health Program’s and providers’ use include a breakdown of medical claims, claim metrics report, medical claim dollars, denied/returned claims, and so forth.
- Reports for use by the HPS contractor to ensure quality assurance and allow resolution of unique claims include reports of pended claims by age and institutional claims with National Correct Coding Initiative (NCCI) edits.
- In addition to standardized reports, ad hoc reports may be generated, as necessary, to provide the Program with detailed insight into the characteristics of Program enrollees, providers, and claims.
12. Payment Reconciliation and Auditing
Accurate payments and timely payment corrections, when necessary, are important to maintain the integrity of the WTC Health Program. The Program has an established process to ensure payments are accurate.
- The HPS contractor reconciles payment data with the payment contractor on a monthly basis to ensure accuracy and alignment of records.
- If a discrepancy or imbalance is found, the HPS contractor researches and resolves the issue.
- Over payments are recovered by withholding from future payments. Checks and cash are not to be sent to the HPS contractor to correct over payments.
- Under payments are rectified by payment adjustments, i.e., making an additional payment.
- Processed claims are regularly audited to ensure accuracy of payments under the Program. Prior to the implementation of auto-adjudication, 100 percent of processed claims were audited for accuracy. With the implementation of auto-adjudication in September 2012, audits are performed on 2 percent of the claims that are not auto-adjudicated, and focuses on both ensuring processors are resolving edits correctly and on keying accuracy, in accordance with industry standards. Processes for measuring the quality of auto-adjudicated claims and post-payment utilization review are currently in development.
13. Appeal of Reimbursement Denial
After exhausting procedural and/or contractual administrative remedies, a CCE or NPN Clinical Director or affiliated provider may submit a written appeal of a WTC Health Program decision to withhold reimbursement or payment for treatment found to be not medically necessary or not in accordance with approved Program medical treatment protocols. Appeal procedures will be published on the WTC Health Program website.
Appendices
5-A—CMS-15005-B—UB-04
5-C 5-D
Policy and Procedures for Recoupment: Lump-Sum Workers' Compensation Settlements
5-EPolicy and Procedures for Recoupment & Coordination of Benefits: Workers’ Compensation Payment
Chapter 6—CCEs and Providers
Table of Contents
Last Revised – April 20231. Purpose and Scope
The purpose of this chapter is to provide a high-level overview of the Clinical Centers of Excellence's (CCEs') roles, responsibilities and processes for the WTC Health Program. In addition to this procedure manual, further details regarding CCE operations can be referenced in the CCE Clinical Guide and the CCE Operations Manual developed by each CCE, both found in the Program's file of record. Of note, the Nationwide Provider Network (NPN) is discussed separately in Chapter 7 of this manual.
2. Statutory and Regulatory References
This chapter is guided by Sections 3305(a)(1) and 3305(b)(1) of the PHS Act, which describe requirements for the contracts put in place with the CCEs, as well as various sections of 42 C.F.R. Part 88. In addition, the CCEs play a pivotal role in implementing the general provisions of the Act, as described below.
3. Roles and Responsibilities
The roles and responsibilities associated with the CCEs and providers in the WTC Health Program are detailed below.
-
CCEs are the NY metropolitan area-based medical facilities that, in accordance with the Act, operate under individual contractual relationships with NIOSH to provide medical monitoring examinations, diagnosis, and treatment services for eligible persons in the NY metropolitan area. Members are each assigned a CCE which is responsible for coordinating their care under the WTC Health Program. CCE responsibilities include, but are not limited to:
- Using an integrated, centralized health care provider approach to create a comprehensive suite of health services that are accessible to enrolled WTC responders, screening-eligible survivors, or certified-eligible survivors;
- Having experience in caring for WTC responders and screening-eligible survivors, or includes health care providers who have received WTC Health Program training
- Employing health care provider staff with expertise that includes, at a minimum, occupational medicine, environmental medicine, trauma-related psychiatry and psychology, and social services counseling; and
-
Meeting such other requirements as specified by the Administrator of the WTC Health Program. For example, each CCE must:
- Manage a provider network to ensure members have access to the necessary expertise required to treat their certified covered conditions;
- Submit periodic reports to the Program regarding its compliance with WTC Health Program regulations, guidelines, and contract requirements; and
- Coordinate with the WTC Health Program Data Centers (DCs) in collecting and analyzing programmatic data.
- With regard to the CCEs, the Program has the responsibility to certify conditions submitted by the CCEs, informing members of the acceptance or denial of coverage and ensuring WTC Health Program claims submitted by the CCEs and their external providers are paid. The Program also communicates regularly with the CCEs to clarify, modify, or establish WTC Health Program policies and procedures, and is responsible for oversight of CCE operations to determine if the CCEs are operating within the WTC Health Program regulations, guidelines, and contract requirements.
- The Health Program Support (HPS) Contractor, under the direction of the WTC Health Program leadership, provides the information technology and program management support that are essential to WTC Health Program CCE operations. The HPS contractor processes claims submitted by the CCEs and their associated providers, coordinates member enrollment and eligibility, supports the authorization of CCE providers, provides call center support, and coordinates with CCEs to provide requested reports and data analysis.
4. CCE Experience and Personnel
The WTC Health Program CCEs offer unique expertise in the provision of healthcare services to NY metropolitan area-based members. Currently, there are seven CCEs that provide WTC Health Program services:
-
Five CCEs serving general responders:
- Northwell Health (Northwell)
- Mount Sinai School of Medicine (MSSM)
- New York University School of Medicine (NYU)
- State University of New York, Stony Brook (SUNY)
- Rutgers University (RU)
- One CCE devoted specifically to Fire Department of New York (FDNY) Responders (FDNY)
- One CCE devoted specifically to survivors of the WTC attacks in NYC – NYC Health + Hospitals System (H+H) WTC Environmental Health Center
-
CCE Experience
Each CCE is experienced in providing healthcare services of a type similar or greater in scope, size, and complexity to those required under the WTC Health Program. Relevant experience includes providing initial and medical monitoring evaluations, diagnostic and treatment services, member services, and administrative services. The current CCEs demonstrated this experience through participation in the predecessor programs described in the “History of the WTC Health Program” section of Chapter 1. -
Personnel
Each CCE must provide personnel necessary to accomplish all activities within the scope of the CCE contract (e.g., physicians, nurses, and support staff), including healthcare provider staff with expertise that includes, at a minimum, occupational medicine, environmental medicine, trauma-related psychiatry and psychology, and social services and benefits counseling.
Each CCE employs a Clinic Director and a Clinic Administrator to oversee medical and administrative aspects of the CCE’s participation in the WTC Health Program. The Clinic Administrator is responsible for all operational aspects of the WTC Health Program at the CCE.
5. CCE Operations Overview
Each CCE operates under contract with the federal government to administer healthcare (within the limited care model defined by Title XXXIII of the PHS Act) to the responders or survivors of the September 11, 2001, terrorist attacks. (The NPN, discussed in Chapter 8, provides care for enrolled members residing outside the NY metropolitan area, including responders to the plane crashes in Shanksville, PA, and Arlington, VA – the site of the Pentagon.) Each CCE is responsible for all aspects of WTC Health Program-related care for each member they serve. In addition to services provided directly by the CCEs, services are also provided through the CCEs by external providers who have expertise in the diagnosis and treatment of 9/11-related health conditions and have been approved by the CCEs and the Program to provide WTC Health Program benefits. Section 6 below provides more detail regarding external providers.
Each CCE educates its staff and network providers in WTC Health Program policies and procedures such as the proper completion of paperwork, limitations of coverage, protocol changes, and benefits counseling, and maintaining a complete Operations Manual to document them. CCE representatives participate in periodic meetings with the Program leadership, their associated data center, the HPS contractor, and other vendors, as required, to coordinate activities, address and resolve issues, and share information.
The work performed by CCEs is grouped into the following four categories and is discussed in detail, below:
- Monitoring and Initial Health Evaluations
- Treatment Services
- Member Services
- Administrative Services
As provided by the PHS Act, the WTC Health Program reimburses providers for healthcare expenses for health conditions that have been certified by the Administrator of the WTC Health Program as WTC-related or as medically associated to a certified WTC-related health condition. Health condition certification is required for treatment services to be paid by the Program. The certification of a WTC-related or medically associated condition is based on a review of a CCE physician’s clinical assessment of the relationship between a given Program member’s WTC exposure and the type and temporal sequence of symptoms, or diagnosis, of a qualifying health condition. This review must find that the member’s exposure to airborne toxins, any other hazard, or any other adverse condition resulting from the September 11, 2001, terrorist attacks is substantially likely to be a significant factor in aggravating, contributing to, or causing the health condition.
A list of the ICD-10 diagnosis codes that correlate with the List of WTC-Related Health Conditions and medically associated health conditions covered by the Program is found in the WTC Health Program Codebook. CCEs provide guidance to external providers on allowable benefits, including proper use of the WTC Health Program Codebook if disseminated.
A member’s health benefit profile is comprised of all Care Suites and certification gates that reflect the conditions that have been certified for that member (Care Suites are discussed in section 9 of Chapter 3 of this manual). The member benefit profile continues to be updated to reflect any new conditions that are certified over time. The claims processing system verifies that each health care service claim line maps a medical procedure to a diagnosis contained within the Care Suites and certification gates comprising a member’s benefit profile.
A. Monitoring and Initial Health Evaluations
Each CCE schedules and provides a baseline exam for new enrollees and follow-up monitoring examinations to WTC responder and certified-eligible survivor members as applicable. The purpose of the monitoring exams is to: (1) provide periodic physical and mental health assessment designed to identify acute and latent health effects that are WTC-related; (2) serve as an avenue for clinical data collection, analysis and reporting to ensure that all services provided adhere to the appropriate protocols; and (3) inform the diagnosis of WTC-related diseases that could lead to a referral for treatment. The table below describes the extent of these exams.
| Exam Component | Baseline Exam | Annual Follow-up Exam |
|---|---|---|
| Medical History Questionnaire | Yes | Yes |
| Exposure Assessment | Yes | No |
| Vital Signs | Yes | Yes |
| Spirometry/Pulmonary Function Testing | Yes | Yes |
| Urinalysis | Yes | Yes |
| Blood Tests | Yes | Yes |
| Physical Examination | Yes | Yes |
| Chest X-ray | Yes | Every 2 years |
If a test result indicates the presence of a WTC-related condition, or is inconclusive, the monitoring physician will refer the member for additional diagnostic testing and/or treatment.
-
Monitoring Exam Process and Protocols
Monitoring services performed by the CCE must addhere to the following processes
and protocols:
- The CCE must use a form such as a Medical History Questionnaire (MHQ), which comprises standardized assessment instruments for multiple physical and mental health conditions.
- The MHQ must be administered by a Registered Nurse (RN) who has received training in the proper completion of the MHQ.
- To ensure quality assurance, all spirometry results are reviewed by appropriate CCE/NPN staff to determine if they meet quality criteria.
- When all exam inventories and tests are completed, the RN prepares a summary report for the monitoring physician. The summary report contains information from the MHQ and results from the laboratory tests, chest X-ray, and spirometry, as well as a summary of the member’s past medical records on file at the CCE.
- The monitoring physician reviews the summary report, conducts a clinical interview and a physical examination, and synthesizes the clinical information for discussion of findings and any needed treatment referrals with the program member. The clinical interview must be conducted by a qualified physician, preferably one specializing in occupational medicine.
-
Medical Monitoring Evaluation Process
The CCE medical monitoring evaluation process consists of the following tasks:
- Scheduling the exam for the member with a provider in the CCE.
- Summarizing prior medical records (including prior claims information) and ensuring that the medical monitoring exam physician has a copy of the summary report prior to the scheduled physical exam appointment.
- Conducting the Medical History Questionnaire interview using RNs.
- Performing the required lab work, chest radiograph, and spirometry test.
- Ensuring that the medical monitoring physician has a summary of the Medical History Questionnaire interview, a summary of the prior treatment records, if available, and the prior medical monitoring exam records in time for the scheduled physical exam.
- Issuing a letter which reports the results of the medical monitoring examination to the member.
- The CCE is required to ensure that medical monitoring examinations are coded correctly, using appropriate formats as described in Chapter 5, and that claims are submitted promptly to the HPS contractor for claims processing.
- The monitoring exam provider coordinates with the CCE Clinic Director to obtain additional testing or subspecialty evaluation, when necessary, for further diagnosis of suspected WTC-related conditions.
- If a physician determines that a member has a WTC-related health condition, the CCE completes the WTC-3 package and submits it to the WTC Health Program MBM for certification, following the procedure outlined in Chapter 3.
- The CCE must follow appropriate authorization channels for treatment services and prescriptions issued under the program, as described in Chapter 4, as well as for coordinating referrals for treatment of covered conditions.
- Each CCE must explain to the members it serves what monitoring and treatment benefits are provided under the WTC Health Program, and that no treatment benefits are provided under the Program for non-covered conditions.
- CCEs provide social services to its members that are applicable to their coverage under the Program. For example, the CCE may offer case management services or assistance with locating community support for members who need it.
- In order to ensure quality assurance, CCEs conduct regular checks on their implementation of the medical monitoring process, as well as the appropriateness and completeness of the medical records maintained by the CCE, and the Program conducts quarterly audits
- CCEs prepare and submit claims for processing and payment to the PM&A contractor after reviewing and approving each for accuracy.
- Working with its associated DC, each CCE reviews and transmits treatment data to the DC for use in WTC Health Program-related research.
-
The CCE must develop protocols or procedures for the following medical monitoring exam-related issues, working in conjunction with their respective DC. These protocols or procedures are approved by the Administrator of the WTC Health Program or designee and communicated by the CCE to its staff, as appropriate. The protocols and procedures include:
- Obtaining relevant CCE medical records for individuals previously served by another CCE
- Quality assurance protocols which are built upon accepted practice guidelines
- Scheduling medical monitoring exams
- Determining the methodology by which monitoring examination services are delivered
- Ensuring that proper data from the exams are sent to the DC for research and analysis purposes
- Ensuring that a letter is sent to the member informing him or her of the exam results within two weeks of the completion of the monitoring exam
- Preparing and submitting claims for all medical monitoring exam-related services
- Collecting and maintaining all records required for project management and reporting
- Handling emergency situations or managing crises that may arise during monitoring, treatment, case management, or other member interaction
-
Diagnosis
- Non WTC-Related Health Condition. If the medical monitoring exam does not lead to the diagnosis of a WTC-related covered health condition, or if no treatment is required, the member will be scheduled for the next medical monitoring exam in 12 months.
- WTC-Related Health Condition. If the medical monitoring exam reveals a health condition that is on the List of WTC-Related Health Conditions and the physician determines it relates to exposure from the September 11, 2001, terrorist attacks, the CCE prepares a WTC-3 certification package as described in Chapter 3, and promptly transmits it to the Program for certification of the member’s health condition.
-
Additional Medical Testing Required
In order to ensure adherence to monitoring protocols, the CCE Clinic Director must approve any additional medical testing proposed by the examining physician to confirm a diagnosis of a WTC-related health condition. Once the CCE Clinic Director’s authorization has been obtained, CCE staff assists the member in scheduling appointments to obtain the additional medical testing.
-
Records, Member Notification and Claims
- Records. After a medical monitoring exam has been completed, the CCE ensures that all completed medical monitoring records are maintained by the CCE in accordance with best-practice medical records storage and privacy standards.
- Member Notifications. The CCE provides a letter to each member informing him or her of the results of the medical monitoring exam within 2 weeks of the completion of the exam.
- Claims. In accordance with the processes described in Chapter 5, the CCE submits a claim for the monitoring exam and services to the HPS contractor for claims processing, using the codes identified in the WTC Health Program Codebook for monitoring.
-
Treatment Services
Once a member has been diagnosed with a WTC-related health condition and that condition is certified by the Program, the member is eligible to receive treatment for that condition when treatment is indicated. Diagnostic and treatment services for members are delivered through an assigned provider at the member’s CCE or its referral network of authorized external providers.
-
Treatment Covered By Codebook. Treatment is provided in accordance with the procedures and services authorized for the care of each certified condition, as established in the WTC Health Program Codebook. Care must meet the medically necessary criteria of the WTC Health Program, guided by the Program’s treatment protocols and outlined in multiple source documents, including the WTC Health Program Codebook, WTC Health Program policy bulletins, and in the Clinical Center and Provider Guides, all maintained in the WTC Health Program file of record.
It is incumbent upon CCE providers to understand the logic of the Codebook, and to be familiar with the codes that are covered by the Program so they can assign them properly for data analysis, reporting, and billing purposes.
-
Treatment Not Covered by Codebook. When a CCE determines that a treatment or prescription medication that is not covered by the Program is a legitimate, medically necessary requirement for treatment of an enrolled member’s certified condition, the CCE may submit a request to add the service to the Codebook via the Change Management Process described in Chapter 4.
The CCE is responsible for ensuring that all treatment providers are knowledgeable about the specific health conditions, procedures, and medications covered by the Program, including the appropriate procedures for handling non-covered health conditions, medical emergencies and appeals.
-
Treatment Covered By Codebook. Treatment is provided in accordance with the procedures and services authorized for the care of each certified condition, as established in the WTC Health Program Codebook. Care must meet the medically necessary criteria of the WTC Health Program, guided by the Program’s treatment protocols and outlined in multiple source documents, including the WTC Health Program Codebook, WTC Health Program policy bulletins, and in the Clinical Center and Provider Guides, all maintained in the WTC Health Program file of record.
-
Claims
Providers may submit claims as an individual provider or as part of a provider group. If medical treatment services are provided in a group setting, the group must be enrolled in the WTC Health Program as a group provider. Each of the CCEs has established methods for claims submission with the WTC Health Program. For specific guidance between an external provider and a CCE, it is always best to consult with the respective CCE directly. In general:
- Claims submitted through a third party administrator (TPA) are considered to be authorized by the CCE which has engaged the TPA.
- Claims submitted from external providers directly to the WTC Health Program are not considered to be authorized, unless other arrangements have been made with the Program.
For services provided by a clinician in his or her offices, claims submitted on paper rather than Electronic Data Interchange (EDI) must use a Professional claim form (CMS-1500). For inpatient or outpatient hospitalizations, claims submitted on paper rather than EDI should use an Institutional claim form (UB-04). Professional services provided in a hospital setting that are not included in the institutional billing should be billed on the CMS-1500 form.
Paper claims originating with external providers must first be submitted to the appropriate CCE. The CCE is responsible for authorizing treatment for the member. Therefore, the CCE must review and authorize claims to be processed. A stamp provided to the CCE by the WTC Health Program is used for this purpose, along with initialing by an authorized CCE approver. Once approved by the CCE, paper claims should be submitted to the WTC Health Program for processing and disposition (i.e., payment, partial payment, or denial). The information entered on the claim form is captured through an automated data collection process; therefore, all paper claim submissions must be legible and of sufficient quality for imaging. Information must be completed in the appropriate field on the billing form in order to expedite claims processing.
-
Pharmacy Benefit
Pharmacy benefit plans have been implemented to improve oversight and minimize fraud, waste, and abuse.
- The CCE is expected to follow the WTC Health Program-approved Routine Diagnostic Plan and the four treatment plans that govern the pharmacy benefits to which members are entitled. Further details regarding the specifics of the pharmacy benefit may be found in Chapter 4, as well as in the Program’s Codebook and bulletins, specifically WTC Health Program Bulletin 13-2 titled, “Implementing Pharmacy Benefit Plans by Health Condition Certification Status,” both located in the Program’s file of record.
- Should a prescription be denied, the CCE has the opportunity to override the denial using the PBM’s online adjudication tool. Chapter 5 provides more detail.
- The physicians who are permitted to prescribe under the WTC Health Program are limited to those providers who have been authorized by the CCEs. Weekly updates of permitted prescribers are sent by the CCEs to the PBM, which shares this information with the HPS contractor. If a provider is permitted to prescribe medications under the WTC Health Program, the provider’s prescriber status is recorded in the claims processing system’s Provider Module.
-
Member Services
Each CCE develops and implements procedures for providing services to its members.
-
Member Retention
Each CCE is responsible for conducting activities that enable the CCE to maintain contact with enrolled members and promote their continued participation in the Program. Each CCE must attempt to update contact information for all members assigned to that CCE on an annual basis. Contact methods include mailings, telephone calls, or emails and contact attempts should continue until the member is contacted or until three attempts have been made using at least two methods of contact.
-
Outreach and Education
CCEs conduct outreach and education to ensure that those persons who are eligible for care through the WTC Health Program are made aware of their eligibility and know how to enroll in the Program. Outreach is specifically not intended to advertise one CCE over another, but rather to advertise the existence of the WTC Health Program and to ensure the Program’s benefits are communicated to all eligible participants. CCE outreach and education activities are undertaken in coordination with Program leadership and the HPS contractor, which operates the Program’s call center. Types of outreach and education services include:
- Answering general questions in regard to program eligibility processes
- Collaborating with the Program leadership, appropriate DC, and other CCEs in standing up and maintaining a Section 508-compliant Website to provide WTC Health Program information for the members being served. Explaining members’ rights and responsibilities under the Program
- Collaborating with the Program leadership, appropriate DC, and other CCEs in providing program information updates to members and providers (e.g., newsletters, letters, brochures, email)
- Explaining the process for obtaining WTC Health Program services
- Providing information on the providers from whom WTC Health Program members may obtain services
- Fielding and responding to member questions and complaints received regarding the WTC Health Program benefits and/or services (i.e., captured from member satisfaction survey, a resource line, or Case Managers)
- Advising members of the available appeals process and the member’s rights to a fair review
- Providing program benefits counseling, which includes explaining the benefits and covered services offered under the WTC Health Program, including WTC-related health conditions and medically associated WTC-related health conditions and limitations, and any conditions associated with the receipt or use of benefits
-
Case Management
Each CCE provides case management services to all members in treatment. The role of the Case Manager is to address the unique healthcare needs of individual members and improve client satisfaction with the program. Case Managers assist in scheduling visits, coordinating care between providers, and facilitating appeal requests. -
Social Services Support
CCEs must provide social service evaluations and assistance to Program members, when needed. These services include assistance with identifying and completing applications to access social programs outside the WTC Health Program when assistance is needed with housing, transportation, food, or medical services that are not covered by the Program.
-
Medical Reviews
If a member's CCE physician is unable to make the necessary findings regarding WTC-relatedness of a condition and/or refuses to submit a request for certification to the WTC Health Program, or refuses to provide or seek authorization for a particular treatment for a covered condition, the member may request a review of that physician decision by the CCE Clinic Director. The member is instructed to send a letter to the CCE Clinic Director describing why he or she believes the physician's decision was incorrect. The CCE Clinic Director reviews the request and provides the member with the final decision and the rationale for it. The CCE furnishes a copy of the letter to the Program and keeps records of the review process in its files for audit purposes. The CCE also tracks such decisions and makes recommendations to the Administrator of the WTC Health Program, as appropriate, when such decisions may require adjustments to program treatment protocols.
-
Workers’ Compensation Assistance
WTC Health Program members who experienced a health condition resulting from work they performed as part of their job duties when responding to the WTC attacks may be eligible to apply for workers’ compensation benefits. Upon request, CCEs must provide assistance to members who are applying for workers’ compensation benefits due to a WTC-related health condition, such as helping to document the member’s health condition and treatment needed. CCEs must also provide requested assistance to providers in completing required workers’ compensation paperwork. Because there may be an extended period of time between the time a claim is filed and when benefits are awarded, the CCE’s provision of care and submission of claims must not be influenced by or changed due to expected workers’ compensation benefits.
In general, the overall order of payors for responders in the WTC Health Program is as follows: Workers’ compensation (for a WTC-related or medically associated health condition that is work-related),* followed, in order, by the WTC Health Program, private health insurance, Medicare, and Medicaid. In most cases involving WTC-related health conditions that are work-related, however, only Workers’ Compensation and the WTC Health Program will be called upon to make payments for Program members’ care.
The exception to the order of payors provided above is where a Program member’s WTC-related or medically associated health condition is eligible for workers’ compensation or another illness or injury benefit plan to which New York City is obligated to pay. In this case, the WTC Health Program is the primary payer.
The WTC Health Program follows the provisions in Title XXXIII of the PHS Act regarding Coordination of Benefits (COB) for survivors. Workers’ compensation is a required part of COB for responders and, in certain limited situations, survivors.
The overall order of payors for survivors in the WTC Health Program is as follows: Workers’ compensation (applicable only if WTC-related condition is a work-related illness for which a claim has been established),* private health insurance, followed by Medicare, then Medicaid, and finally the WTC Health Program. Requirements for billing under the COB policy for survivors provide that, where applicable, payment for services must first be sought from:
- Private Health Insurance: Where the WTC- related or medically associated health condition is not work-related, and where the member has private health insurance coverage, the private health insurance must be billed prior to billing the WTC Health Program.
- Public Health Insurance (Medicare/Medicaid): Where the WTC-related or medically associated health condition is not work-related, and where the member does not have private health insurance but is covered by Medicare or Medicaid, those entities must be billed (in that order) prior to billing the WTC Health Program.
The total payment, including any amounts paid by other entities and by the WTC Health Program, will not exceed the fee schedule used by the WTC Health Program. If the primary payor already paid up to the fee schedule amount, no additional payment is made under the WTC Health Program.
If prior payments were made by another entity, those payments should be shown when the claim is submitted to the WTC Health Program.
*Note: The WTC Health Program established a process to recoup from workers’ compensation after payment of claims to the CCEs. Therefore, the CCEs are not responsible for billing workers’ compensation for WTC Health Program claims prior to either submission to the Program in the case of responders or private/public insurance in the case of survivors. -
Member Transfers
In the event that a member requires transfer from one CCE to another, the CCEs follow their established procedures for assisting with the transfer by coordinating with each other. The “sending” CCE will share appropriate medical records and other data and provide any information the member and “receiving” CCE may need to ensure seamless care. Transfers between the NY metropolitan area CCEs are available to any non-FDNY responder. FDNY responders who are active members of FDNY are not eligible for transfer to another CCE as care is provided through the FDNY at its Bureau of Health Services. All NY metropolitan area survivors are initially assigned to HHC; all non-NY metropolitan area members are initially assigned to the NPN. Additional information on member transfers can be found in Chapter 8, Member Services.
-
Member Retention
-
Administrative Services
Each CCE must develop and implement certain procedures for providing administrative services to support the WTC Health Program. These procedures are documented in each CCE’s Operations Manual.
-
Healthcare Provider Network
Each CCE has established and maintains an adequate healthcare provider network to serve all members who are assigned to the CCE. This network may include, but is not limited to, hospitals, specialty clinics, trauma centers, specialists, and primary care physicians. The CCEs are responsible for providing healthcare expertise in sufficient numbers and at convenient locations for the members. Providers may be either internal or external to the CCE establishment. An example of an internal provider is a respiratory therapist on the CCE’s staff; an example of an external provider is a psychiatrist in private practice who has been authorized to provide WTC Health Program services on behalf of the CCE. Each CCE is responsible for ensuring that all healthcare providers serving the WTC Health Program meet all requirements of the CCE’s contract, including that they comply with all workers’ compensation requirements and are properly licensed and insured. The physicians who conduct the medical monitoring assessments and physicals must be experienced in practicing occupational medicine (e.g., conducting occupational health screening and medical surveillance)—preferably credentialed as occupational medicine specialists. Additional information on the Provider Network is found in Section 6 below. -
Credentialing
Each CCE has established and implements a credentialing process for its provider network to ensure all providers are qualified to provide care under the WTC Health Program. Each CCE submits key information on each provider to the HPS contractor so the providers can be entered into the claims processing system. The credentialing process is documented in each CCE’s Operations Manual.
-
Training
Each CCE ensures that all providers and other personnel who perform work for the WTC Health Program are properly trained – both initially and on an ongoing basis – to perform their assigned functions. This training includes:
- Potential exposures and health outcomes that have been associated with the WTC terrorist attacks
- The conditions and services covered by the WTC Health Program
- Proper coding of and billing for WTC Health Program services
- How to ensure compliance with the WTC Health Program policies and procedures
- Avenues for problem-solving, escalation of concerns, etc.
Training processes and procedures are further described in each CCE’s Operations Manual. -
Pharmacy Benefit Management (PBM)
Each CCE works with the WTC Health Program PBM to provide pharmacy benefits to its members, as described in Chapters 4 and 5. By providing names of and pertinent data on authorized prescribers to the PBM, each CCE validates to the Program that those writing prescriptions under the WTC Health Program are authorized to do so. CCEs also play a role in the management of pharmacy benefits when overrides or prior authorizations are needed to ensure members receive needed medications. These processes are described further in Chapter 5.
-
Quality Assurance and Internal Audits
Each CCE has established a quality assurance function to ensure high-quality care of WTC Health Program members in accordance with all Program policies and procedures. Responsibilities for quality assurance include:- Ensuring adherence to monitoring and treatment protocols
- Providing benefits counseling for workers’ compensation and other insurance programs, as necessary
- Appropriately billing for only WTC-related health conditions and medically associated health conditions
- Ensuring appropriate diagnostic and treatment referrals for members, when necessary
- Verifying prompt communication of test results to members
- Reviewing all claim forms and other contract deliverables for completeness and accuracy
- Measuring, monitoring, and increasing member satisfaction
- Improving overall program success
- Ensuring early identification and resolution of problems, issues, and risks
- Monitoring of adherence to established policies and procedures
- Continuous process improvement and implementation of lessons learned
-
Quality Assurance Program (QAP)
Each CCE is responsible for developing, implementing, and documenting its approach to quality assurance. CCEs each have developed a WTC Health Program-specific Quality Assurance Program (QAP) which describes the procedures used to monitor and improve all Program activities, including reporting. To ensure consistency among CCEs and alignment with WTC Health Program goals and objectives, each CCE’s QAP must be approved by the Administrator of the WTC Health Program or designee. -
Customer Satisfaction Survey Program (CSSP)
A Customer Satisfaction Survey Program (CSSP) is part of every CCE’s QAP. In this program, members are given the opportunity on an annual basis to complete a customer satisfaction survey.
Each CCE must report findings from its customer satisfaction survey to the Administrator of the WTC Health Program or designee. These findings include frequency and method of surveys, survey results, and corrective actions to be taken based on survey results -
Internal Audits
As a part of its QAP, each CCE conducts an internal audit at least once a quarter. These audits include:
- Targeted Health Care Compliance – The Targeted Health Care Compliance audit focuses on evaluating the adequacy of the procedures used by the CCE to ensure that only approved WTC health conditions and approved health care services (including provider visits, procedures, medication and durable medical equipment) are reimbursed by the Program. This includes a review of documentation justifying payment history for medically associated health conditions.
- Medical Management Review – The Medical Management Review audit looks to ensure that medical practice guidelines developed for the Program are being followed.
- Claims History – The Claims History audit focuses on irregularities in the claims history of any particular provider or member.
- Medical Records Review – The Medical Records Review audit focuses on determining if appropriate procedures are being followed related to the collection, review, and storage of medical records.
- Personnel Training – The Personnel Training audit focuses on ensuring that all personnel performing work on the Program are properly trained.
-
Records Management
Each CCE is responsible for administering a comprehensive records management program which ensures that all Program records, including medical records, are maintained in such a manner that the information is secure and readily accessible to authorized parties. For all protected health information (PHI), this includes compliance with all Health Insurance Portability and Accountability Act (HIPAA) requirements. The CCEs must provide the Administrator of the WTC Health Program with a copy of their Notice of Use and Disclosures of Protected Health Information required by the HIPAA privacy rule and ensure in that notice that the members are aware that the Administrator of the WTC Health Program and/or his designee will have access to the members’ protected health information for the purposes of the treatment provided by and administration of the WTC Health Program. The records management program includes providing assistance to members in obtaining medical records and processing member requests to release protected information. In addition, each CCE has the capability for a medical records locator to facilitate the retrieval of all medical records from any provider for any member within the CCE or their referral network. -
Other Administrative Responsibilities
Additional responsibilities of the CCE include:- Attending administrative, steering, benefits, and clinical WTC Health Program meetings
- Writing reports and Institutional Review Board (IRB) submissions
- Entering data for claims submission and to meet reporting requirements
- Entering data of healthcare information into the DC’s data system
- Providing intellectual input on the refinement of medical guidance and protocols as needed by the program (and coordinated by the DC), or in support of member treatment needs
- Providing administrative personnel and facilities to support the CCE’s contract
- Providing translational and interpretive services for non-English-speaking members, as appropriate to the CCE’s member population
-
Healthcare Provider Network
6. Provider Networks
The establishment and management of the internal and external provider network are coordinated through the respective CCEs. In order for a provider to have a claim for WTC Health Program services paid, the CCE must have enrolled the provider as a participating provider in the WTC Health Program. Provider enrollment into the WTC Health Program and the management of a reliable provider network are critical to efficient claims processing. The complete and accurate enrollment of providers ensures that claims are not suspended for review of provider validity issues, and that claims may be promptly adjudicated.
Each CCE is responsible for submitting provider enrollment requests to the HPS contractor and updating provider details when necessary. All medical providers, including physicians, group practices, hospitals, Durable Medical Equipment (DME) suppliers, nursing facilities, hospice services, and others, must enroll as participating providers in the WTC Health Program for claims to be adjudicated through the Program’s claims processing system. Each CCE determines the nature of its provider relationships (i.e., internal or external) and is also responsible for providing the appropriate level of education and information regarding the Program to external providers so that they may provide an approved level of care for WTC Health Program-certified conditions.
The HPS contractor uses the information provided by the CCEs to add providers to the claims system.
-
Internal Provider
The internal provider network is comprised of healthcare providers (both individuals and groups) that have established relationships as internal medical providers with the medical institutions that are managed by each respective CCE. For example, the Mount Sinai School of Medicine (MSSM) is a medical facility within the purview of the MSSM CCE; most, if not all, of the physicians and groups who practice at the MSSM are enrolled as internal MSSM providers. The designation of “internal” provider is relevant during claims processing, as a claim received by an internal provider is considered to be already authorized by the managing CCE through the nature of the provider’s relationship to that CCE’s affiliated institution(s).
-
External Provider
The majority of the enrolled WTC Health Program providers are external to a CCE. The external provider network comprises healthcare providers (both individuals and groups) that have contractual relationships to provide medical services for members assigned to a particular CCE. External providers may be affiliated with more than one CCE. The designation of “external” provider is relevant during claims processing, as a claim received by an external provider is not considered to be authorized by the managing CCE unless the claim shows an official stamp indicating CCE authorization is submitted by EDI. Claims submitted by the TPA are assumed authorized because of procedures established by the CCEs and the TPA ensuring claims are authorized before they are submitted to the program for payment. The process for authorizing claims is described in Chapter 5.
After a CCE has established either an internal or external relationship with a provider, the CCE must submit a provider enrollment request to the HPS contractor for processing. CCEs must provide the following data:
- Provider/Practice Name
- Provider/Practice Address (must not be a PO Box)
- Provider/Practice Telephone/Fax Number
- Provider/Practice National Provider Identifier (NPI) Number
- Provider/Practice Social Security Number (SSN)/Employer Identification Number (EIN)
- Provider Medicare Number (if provider will be submitting institutional claims)
- Billing Provider/Practice Name
- Billing Provider/Practice Address (can be a PO Box) where Remittance Advice (RA) may be sent
- Billing Provider/Practice NPI Number
- Billing Provider/Practice EIN
-
Financial Information (can be submitted on an Electronic Funds Transfer [EFT] Form), including:
- Financial Institution Name
- Financial Institution Address
- Financial Institution Routing Transfer Number
- Depositor Account Number
Financial information is also provided using an EFT Form or other document provided by the Program so that providers may receive payment for their claims.
Before submitting the provider enrollment, the CCE confirms: 1) that all data are complete and accurate; 2) that the provider’s status as either an internal or external provider is documented; and 3) whether the provider should also be enrolled with the following specialties:
- Rx Prescriber—this is not a required data element, but if this information is not provided, the record will default to “Not an Rx prescriber” and the provider will not be able to write prescriptions for members.
- Cancer Care Provider—this is not a required data element, but if this information is not provided, the record will default to "Not a cancer provider." As of April 26, 2013, an open prescriber network for members assigned to the Cancer Treatment Plan became effective, permitting cancer care providers to prescribe certain drugs for cancer care. For all other non-cancer formulary drugs, a provider must be flagged as "Rx prescriber" in order to authorize prescriptions.
Once a provider enrollment has been received and validated by the CCE, the CCE submits the enrollment to the HPS contractor for processing. If incomplete information is received, the enrollment form will be returned to the CCE for completion. provides more detail regarding the steps taken to complete the enrollment process.
The management and maintenance of the information in a provider record are the CCEs’ responsibility. Changes to provider information may be necessary over time (e.g., an address or financial information changes, or a provider ceases her association with the WTC Health Program). Any changes to provider information that are received by the CCEs are processed in the same way as for an initial enrollment. Changes to provider information that are not first identified by the CCE must be routed to the CCE for validation and to ensure consistency among, and accuracy of, Program records. This could occur, for example, when a claim being processed for payment reveals that the provider’s EFT information has changed
-
Annual Confirmation of Authorized Providers
Enrollment and management of a reliable provider network is critical to ensure that claims will efficiently and accurately adjudicate. In the interest of supporting the CCEs’ responsibility to manage their provider and prescriber enrollees, the HPS contractor annually distributes to each CCE a list of all its providers enrolled in the Program. The CCE must review the list and make any updates or note any discrepancies between the providers held on record by the Program and those held on record by the CCE. The HPS contractor is responsible for working with the CCE to resolve any discrepancies in a timely fashion.
7. Reporting Requirements
CCEs have a number of reporting requirements regarding activities undertaken on behalf of the WTC Health Program.
-
Monthly Reports
Each CCE submits to the Program monthly status reports on member and administrative services activities to allow Program leadership to track the CCE’s program activities and progress. In addition to summarizing the activities and accomplishments of the past month, the report identifies any potential risks to continued program success and communicates the CCE’s plans to mitigate those risks. A variety of reports are required, as detailed below.
-
Member Services Monthly Report. The content of the Member Services Monthly Report is reflected in the following table.
Member Service Function
Information to Be Reported
Member Retention
A complete listing of activities, descriptions of activities, number of actions, and evaluation of effectiveness of all Member Retention services performed during the period and the associated cost for these services invoiced to the government.
Member Outreach and Education
A complete listing of activities, descriptions of activities, number of actions, and evaluation of effectiveness of all Member Outreach and Education services performed during the period and the associated cost for these services invoiced to the government.
Program Benefits Counseling
A complete listing of activities, descriptions of activities, number of actions, and evaluation of effectiveness of all Program Benefits Counseling services performed during the period and the associated cost for these services invoiced to the government.
Case Management
A complete listing of activities, descriptions of activities, number of actions, and evaluation of effectiveness of all Case Management services performed during the period and the associated cost for these services invoiced to the government.
Social Services Functions
A complete listing of activities, descriptions of activities, number of actions, and evaluation of effectiveness of all Social Services Functions performed during the period and the associated cost for these services invoiced to the government.
Member Transfers
A complete listing of activities, descriptions of activities, number of actions, and evaluation of effectiveness of all Member Transfer services performed during the period (including the status of all outstanding requests for medical records) and the associated cost for these services invoiced to the government.
Medical Reviews
A complete listing of activities, descriptions of activities, number of actions, and evaluation of effectiveness of all Administrative Services related to Medical Reviews that were performed during the period and the associated cost for these services invoiced to the government.
Workers’ Compensation Assistance
A complete listing of activities, descriptions of activities, number of actions, and evaluation of effectiveness of all Workers’ Compensation Assistance performed during the period and the associated cost for these services invoiced to the government.
Other Member Services
A complete listing of activities, descriptions of activities, number of actions, and evaluation of effectiveness of all Other Member services performed during the period and the associated cost for these services invoiced to the government.
-
Administrative Services Monthly Report. The content of the Administrative Services Monthly Report is reflected in the following table.
Administrative Service Function
Information to Be Reported
Healthcare Provider Network
A complete listing of activities, descriptions of activities, number of actions, and evaluation of effectiveness of all Healthcare Provider Network services performed during the period and the associated cost for these services invoiced to the government.
Pharmacy Benefit Management
A complete listing of activities, descriptions of activities, number of actions, and evaluation of effectiveness of all Pharmacy Benefit Management services performed during the period and the associated cost for these services invoiced to the government.
Quality Assurance and Internal Audits
A complete listing of activities, descriptions of activities, number of actions, and evaluation of effectiveness of all Quality Assurance and Internal Audits performed during the period and the associated cost for these services invoiced to the government.
Records Management
A complete listing of activities, descriptions of activities, number of actions, and evaluation of effectiveness of all Records Management services performed during the period and the associated cost for these services invoiced to the government.
Transfer of Data and Information (at the end of the contract)
A complete listing of activities, descriptions of activities, number of actions, and evaluation of effectiveness of all Transfer of Data and Information services performed during the period and the associated cost for these services invoiced to the government.
Attending administrative, steering, benefits, and clinical WTC meetings
A complete listing of activities, descriptions of activities, number of actions, and evaluation of effectiveness of all attendance at administrative, steering, benefits, and clinical WTC meetings during the period and the associated cost for these services invoiced to the government.
Report Writing and IRB Submissions
A complete listing of activities, descriptions of activities, number of actions, and evaluation of effectiveness of all Report Writing and IRB Submissions that were performed during the period and the associated cost for these services invoiced to the government.
Data Entry for Claims Submission and to Meet Reporting Requirements
A complete listing of activities, descriptions of activities, number of actions, and evaluation of effectiveness of all Data Entry services performed during the period and the associated cost for these services invoiced to the government.
Data Entry of Healthcare Information into the DC’s Data System
A complete listing of activities, descriptions of activities, number of actions, and evaluation of effectiveness of all Case Management services performed during the period and the associated cost for these services invoiced to the government.
Healthcare Protocol Development—provide intellectual input on the refinement of medical guidance and protocols as needed by the program (and coordinated by the DC), or in support of member treatment needs
A complete listing of activities, descriptions of activities, number of actions, and evaluation of effectiveness of all Healthcare Protocol Development services performed during the period and the associated cost for these services invoiced to the government.
Providing Translational and Interpretive Services
A complete listing of activities, descriptions of activities, number of actions, and evaluation of effectiveness of all Providing Translational and Interpretive Services performed during the period and the associated cost for these services invoiced to the government. General and Administrative Charges
General and Administrative Charges
A complete listing of activities, descriptions of activities, number of actions, and evaluation of effectiveness of all General and Administrative Charges during the period and the associated cost for these services invoiced to the government.
Other Administrative Services
A complete listing of activities, descriptions of activities, number of actions, and evaluation of effectiveness of all Other Administrative Services performed during the period and the associated cost for these services invoiced to the government.
-
Other sections of the Monthly Report are reflected in the below table.
Operations Manual
Difficulties encountered and proposed updates to the Operations Manual. Updates shall be approved by the Administrator of the WTC Health Program after review and discussion of the issues, as needed.
Complaints
A summary of all complaints received by the CCE during the preceding month and the status of their resolutions.
Fraud and Abuse Report
A) The CCE shall submit monthly the number of complaints of fraud or abuse made to the CCE related to covered services that warrant preliminary investigation by the CCE. B) The CCE shall also submit to the Administrator of the WTC Health Program the following on an ongoing basis for each confirmed case of fraud or abuse it identifies through complaints, organizational monitoring, contractors, subcontractors, providers, and members, etc. related to covered services: 1) The name of the individual or entity that committed the fraud or abuse; 2) The source that identified the fraud or abuse; 3) The type of provider, entity, or organization that committed the fraud or abuse; 4) A description of the fraud or abuse; 5) The approximate dollar amount of the fraud or abuse; 6) The legal and administrative disposition of the case including actions taken by law enforcement officials to whom the case has been referred; and 7) Other data/information as prescribed by the Administrator of the WTC Health Program. Such report shall be submitted when cases of fraud or abuse are confirmed, and shall be reviewed and signed by an executive officer of the CCE.
-
Member Services Monthly Report. The content of the Member Services Monthly Report is reflected in the following table.
-
Additional Administrative Reports
Other operational data reports may be required from time to time to support the needs of the Program. In such cases, the Administrator of the WTC Health Program or designee will work with the CCEs to coordinate the content of the report and delivery details, as necessary. An example of such a report is the Customer Satisfaction Survey report.
8. CCE Operations Manual
Each CCE has developed a CCE Operations Manual which has been approved by the Administrator of the WTC Health Program. The manual must be updated at least quarterly to reflect changes in WTC Health Program policies and procedures and include the following:- Protocols for medical monitoring exam-related issues, working in conjunction with the CCE’s respective DC
- Protocols for treatment-related issues
- Procedures for providing member services: member retention; outreach and education; benefits counseling; case management; social services; and medical appeals
- Details of the medical review process and records system
- Details of the Workers’ Compensation Assistance program
- Details of the member transfer process
- Details of the quality assurance program
- Details of establishing and credentialing the CCE’s provider network
- Details of the training program
- Details of the records management program
- Details of the transfer of data and information and turnover of services procedure
- Details of other administrative services provided
Chapter 7—Nationwide Provider Network
TABLE OF CONTENTS
Last Revised – August 20231. Purpose and Scope
The purpose of this chapter is to provide a high-level overview of the Nationwide Provider Network (NPN) contractor’s roles, responsibilities, and processes for the WTC Health Program. In addition to this Administrative Manual, further details regarding NPN operations can be referenced in the NPN Operations Manual developed by the NPN and found in the Program’s file of record. Of note, the Clinical Centers of Excellence (CCEs) are discussed separately in Chapter 6 of this manual, while the process for certification of health conditions is provided in Chapter 3, and information on medical benefits are provided in Chapter 4.2. Statutory and Regulatory References
The NPN is responsible for implementing the general requirements of the Act, with its function, roles, and responsibilities specifically guided by the following sections:- Section 3313, which describes the national arrangement for benefits for eligible individuals outside the New York (NY) metropolitan area:
- Section 3312(b)(4)(C), which includes coverage for certain transportation expenses incurred by members securing medically necessary treatment through the NPN, and
- Section 3305(a)(2)(A)(iv), which calls for the Data Centers (DCs) to establish the criteria for credentialing medical providers who participate in the NPN.
3. Roles and Responsibilities
The roles and responsibilities with respect to the NPN are detailed below.
- The NPN is operated by Managed Care Advisors (MCA)-Sedgwick to provide healthcare services for members who reside outside the New York metropolitan area, including Shanksville, PA, and Arlington, VA, the site of the Pentagon. Healthcare services include initial health evaluations for screening-eligible WTC survivors, as well as monitoring and treatment benefits for enrolled WTC responders or certified-eligible WTC survivors. After receiving information regarding approved enrollees from the Health Program Support (HPS) contractor, the NPN enrolls the new members into its system and educates them on NPN processes for obtaining covered benefits. The NPN must maintain a viable provider network to provide monitoring and treatment to NPN members with services available across the country to ensure access near a member’s area of residence. The Program defines NPN network adequacy as having a healthcare provider available within 30 miles in urban areas and 75 miles in rural areas. The NPN will work with members to bring a provider into the network or identify a provider who will meet both member needs and the requirements of the Program. The NPN forwards all medical claims to the Centers for Medicare & Medicaid Services (CMS) contractor responsible for disbursing payment for the program.
- The Program has the responsibility to communicate regularly with the NPN to clarify, modify, or establish WTC Health Program policies and procedures, and provides oversight of NPN operations to verify that the NPN is operating within the WTC Health Program regulations, guidelines, and contract requirements. It also ensures that claims submitted by the NPN’s providers are paid by the CMS contractor.
- The HPS contractor, under the direction of the WTC Health Program leadership, provides the information technology and program management support services that are essential to WTC Health Program NPN operations. The HPS contractor provides weekly updates on new enrollees to the NPN, provides contact center support, and coordinates with the NPN to provide requested reports and data analysis.
4. Overview of NPN Services
The NPN manages a network of providers who are licensed, credentialed, insured and/or certified in accordance with the WTC Health Program requirements. Participating providers receive training on WTC Health Program covered health conditions and protocols from the NPN. In many cases, an enrollee may receive care from more than one NPN provider. The chart below describes the process used by the NPN to select and maintain providers within the NPN provider network.
1. Clinical Management Team Searches for Provider
2. Provider Contacted
3. Complete Services Confirmation Checklist
4. Provider Qualification
5. Provider Completes Subcontractor Agreement
6. Collect and Verify Credentialing Information
- Unrestricted, valid current licensure and certification [Fraud and Abuse Control Information Systems (FACIS) query]
- Ensure all credentials meet all standards for local, state, and federal requirements
-
Accredited Credentialing Verification Organization (CVO)
-
Criminal Search Felony Background – State/ County
- Found Wants and Warrants (open cases)
- Felony and/or Misdemeanor Convictions
-
Criminal Search Felony Background – National
- Includes Office of Foreign Assets Control (OFAC) Specially Designated Nationals (SDN) List
- Includes Sex Offender Registries from all 50 states
- Office of Inspector General (OIG) Excluded Individuals/Entities
- Collect all required credentials
-
Criminal Search Felony Background – State/ County
- General Service Administration (GSA) List of Excluded Parties
- Criminal History Background Check as Required Military Affairs Policy HA97-036
7. Update Provider Information Using Workflow Management Technology
-
Documents scanned in
- Subcontractor agreement
- W-9
- Statement of affirmation
- Signed non-disclosure form
- Facility information form
- Credentialing documents
- Initial Application for Clinical Privileges
- Proof of current malpractice coverage
- Statement of Affirmation/Release of Information
- Credentialing Primary Source Verifications Conducted:
- Proof of Current State licensure(s) and renewal
- License/malpractice/Medicare or Medicaid sanction history
- Current DEA registration for any prescribing clinician
- Proof of degree and state licensure
- Board certification
- Certifications such as Basic Life Support/Cardiopulmonary Resuscitation (BLS/CPR) or Advanced Cardiovascular Life Support (ACLS)
8. Provider Training
- Government guidelines and federal regulations
- Center for Personalized Education for Physicians (CPEP)
- NPN contractor standardized procedures
9. Information Retrieval
All contracting documents, training history, credentialing and licensing reports are maintained for audit access upon request
4.1 Credentialing and Re-credentialing Process
The NPN has a team of individuals whose responsibility it is to ensure all Healthcare Practitioners (HCPs) within the NPN are licensed within the state where they will be performing services. The NPN ensures that all HCPs have unrestricted, valid current licenses, certifications, and registrations as required for their particular profession within the state, district or territory in which they are performing services. The NPN uses both trained credentialing staff and an accredited Credentialing Verification Organization (CVO) to meet the provider credentialing requirements of its WTC Health Program contract.
The NPN tracks the credentialing requirements in its data system for each provider to ensure all documentation is accurate and current.
A qualifying practitioner is not activated within the NPN until the credentialing verification process is complete and the NPN Clinical Director has provided final approval. The NPN performs ongoing monitoring to identify any sanctionable activities or instances of malpractice, fraud, waste or abuse. HCPs are re-credentialed every 36 months.
All subcontracted providers receive training and monitoring of their quality of care and overall performance in the provision of clinical services. All providers receive training from the NPN’s Medical Provider Training department prior to scheduling appointments. Forms, procedures, and expectations are reviewed in the initial training session to ensure compliance with WTC Health Program processes.
4.2 NPN Member Eligibility and Enrollment
As Chapter 2 details, eligibility for all members of the WTC Health Program is determined by the Program. Members are assigned to the NPN by the Program based on their geographic location. These WTC Health Program members may be newly enrolled members or members who transfer from a CCE.
Newly enrolled WTC Health Program members are assigned to the NPN by the WTC Health Program’s Member Services Team based on the new member’s location outside the NY metropolitan area. If a newly enrolled WTC Health Program member who has not been assigned to the NPN contacts the NPN directly, the NPN will work with the member and the Program to confirm eligibility and assignment.
If a WTC Health Program member wishes to transfer from a CCE to the NPN or from the NPN to a CCE, the NPN and relevant CCE will work together to coordinate the transfer using the established WTC Health Program transfer policy, detailed in the Member Services Operations Manual.
The NPN sends each WTC Health Program member who has been assigned to the NPN a Welcome Packet that includes the following materials:- Welcome letter;
- Frequently Asked Questions handout;
- Workers’ compensation application1; and
- Medical record release forms (only for members transferring from a CCE to ensure continuity of care).
1In accordance with Section 3331 of the James Zadroga 9/11 Health and Compensation Act of 2010, WTC Health Program members whose covered conditions are also covered under workers’ compensation may have their payments reduced or recouped to the extent that payment has been made or is reasonably expected to be made under workers’ compensation law.
4.3 Scheduling, Intake Interview, Testing, and Monitoring Exams
Coordination of member intake is managed by the NPN case manager. Ongoing communication with a WTC Health Program member occurs through a variety of media, as necessary, including telephone, email, and fax, and may include the use of Integrated Voice Recognition (IVR) technology.
Pre-scheduling ActivitiesNew Member: The NPN contacts the member to answer questions and schedule an initial monitoring exam or initial health evaluation. Since the member is not transferring from a WTC Health Program CCE, there are no prior medical records to retrieve.
Transfer Member: The NPN contacts the member to answer questions and encourage the member to return the Medical Record Release Form(s), provided in the Welcome Packet. The NPN makes up to six call attempts to reach the member to obtain the completed Medical Record Release Forms, as necessary. Once the forms are received, the NPN coordinates with the member’s CCE to collect the medical records via trackable shipping service, enters information from the records into the NPN database and assigns a case manager to review the records and document the member’s WTC-certified health conditions and medical history. Upon completion of documentation, the case manager schedules the intake interview.
The intake process consists of three parts: an intake interview; testing; and a monitoring exam or initial health evaluation.
Intake Interview
Since NPN members are located throughout the country, face-to-face meetings are not feasible, so the NPN case manager conducts intake interviews by telephone. During the intake interview, the case manager verifies all demographic information with the member, making updates when necessary, in order to ensure proper identification and confidentiality. A Medical Health Questionnaire (MHQ) is completed by the case manager and typically takes between 45 minutes to 1 ½ hours. The MHQ is completed for both new WTC Health Program members and transfers into the NPN to ensure completeness of NPN documentation. If a member uses English as a second language and prefers to speak his/her primary language, the NPN engages a company that offers interpreter services to assist in interpreting the interview.
After the MHQ is conducted, the case manager schedules testing and monitoring exam or initial health evaluation appointments with the assigned provider. These appointments are scheduled immediately for new members; for transfers into the NPN, the appointments are scheduled based on the due date of the member’s next exam. All eligible members are encouraged to have an annual monitoring exam.
Testing and Monitoring Exams
The initial monitoring exam or health evaluation is consistent with those performed by the CCEs and includes a review of the completed MHQ, a general health assessment, vital signs assessment, spirometry testing, blood work, urine collection, and a chest X-ray. The follow-up monitoring exam, where appropriate for the type of member, includes the same components as the initial monitoring exam with the exception of the chest X-ray, which is performed every two years unless an increased frequency is clinically indicated. Follow-up exams or additional testing, scheduled through the case manager, may be required as a result of the monitoring exam to complete a diagnosis. Chapter 6 provides more detail on the components of the monitoring exams.
Within 48 hours of a member completing his/her appointment(s), all documentation is forwarded from the provider to the NPN so that the NPN Clinical Director may determine whether or not to request certification of a health condition. Chapter 3 provides detailed information regarding the certification process. The NPN scans all received documents and archives them in its database. The completeness of the documents is reviewed using a system-generated checklist. If any required materials are missing, the NPN contacts the provider to retrieve the missing component(s) and/or to complete any missing exam elements. In the event providers are not completing the exams/evaluations accurately or completely, re-training may be recommended.
Inform Member of Results
Once all documents are received by the NPN and quality reviews are completed, the case manager conducts a thorough review of the exam findings and drafts a letter to the member informing him/her of the results and any referrals to the treatment program that stemmed from their exam. All exam results are sent no later than two weeks after the monitoring exam or health evaluation services have been completed.
If referrals are identified, the case manager follows up with the member within five days after the letter and exam/evaluation documentation has been sent to the member to discuss the conclusions reached from the initial work-up and the member’s ongoing participation in the Program. The case manager discusses covered health conditions and assists in the coordination of treatment, as necessary. Additionally, the case manager outlines those health conditions that the member may have that are not covered under the WTC Health Program and instructs the member to see his/her primary care provider for treatment of those health conditions. If necessary, the case manager engages the NPN social worker who assists in the processing of social work referrals and benefits counseling for the member.
The NPN’s Social Services Specialist will reach out to provide assistance when a member’s answer to the MHQ either in the mental health section or social benefits section indicates it may be needed, when a need is identified by the case manager through conversation with the member, or when a monitoring exam/initial health evaluation physician identifies the need for a social service referral. Areas of need addressed may include utility needs such as electricity and heating, transportation needs, mental health needs, assistance with Victim Compensation Fund questions, coordination of benefits with other programs such as Medicaid or workers’ compensation, provision of guidance in accessing resource programs such as food stamps or financial assistance, offering guidance in accessing medication assistance or medical assistance programs, providing assistance in accessing local resources in other regions of the country, or other items as requested by the member.
If referrals are not indicated as part of the monitoring exam/initial health evaluation, the NPN will begin the process for scheduling the next monitoring exam 60 days prior to its due date, where appropriate.
4.4 Treatment Services
If a member is referred for treatment, the NPN will begin the request for certification process for all covered health conditions which the clinical director determines that the member’s exposure to airborne toxins, any other hazard, or any other adverse condition resulting from the September 11, 2001, terrorist attacks, is substantially likely to be a significant factor in aggravating, contributing to, or causing the illness or health condition. Chapter 3 describes the process for certifying covered conditions under the program. When a member’s health condition is approved for certification by the WTC Health Program, the Program notifies the NPN electronically and sends the member a letter to inform him/her of the Program’s decision.
The NPN also issues a Member ID Card to all NPN members consistent with the Program’s practices for all members. The card contains a member identification number and the customer service telephone numbers for the NPN and for the Pharmacy Benefits Manager (PBM).
4.5 Processing and Paying Claims
The NPN reimburses every subcontracted provider within 30 days of receipt of their invoice. In order to receive reimbursement, the services rendered must be medically necessary, performed completely and in accordance with the NPN’s authorization, protocols, and direction.
Upon receipt of an invoice, the NPN reviews it for accuracy and completeness. Once the NPN determines that the invoiced services are appropriate and in accordance with WTC Health Program requirements, the invoice is electronically submitted to the HPS contractor for processing and payment. If the NPN determines that the invoiced services are not in accordance with Program requirements, it denies the invoice and sends the provider a letter of explanation permitting the provider to correct any errors and, if appropriate, resubmit a corrected claim to the NPN. See Chapter 5 for more detail on how NPN medical and pharmaceutical claims are processed, paid and can be appealed.
Chapter 8—Member Services and Communication
TABLE OF CONTENTS
Last Revised – February 2026
1. Purpose and Scope
This chapter describes the member services and communication activities provided by the World Trade Center (WTC) Health Program. A member is defined as any responder, screening-eligible survivor, or certified-eligible survivor who has been found eligible for and enrolled in the WTC Health Program.
2. Statutory and Regulatory References
The following sections of the James Zadroga 9/11 Health and Compensation Act of 2010, as amended (Zadroga Act)1, are applicable to this chapter:
-
Section 3303 of the Public Health Service Act (PHS Act) (42 U.S.C. § 300mm-2) describes the education and outreach services the WTC Health Program is required to provide. These services are conducted in a manner intended to reach all affected populations and to support culturally and linguistically diverse populations. The outreach and education services include:
- The establishment of a public website with information about the WTC Health Program;
- Meetings with potentially eligible populations;
- The development and dissemination of outreach materials informing people about the Program; and
- The establishment of phone information services.
- Sections 3305(a)(1)(B)—(E), 3305(a)(2)(A)(iii), and 3305(b)(1)(B)(ix) of the PHS Act (42 U.S.C. §§ 300mm-4(a)(1)(B)—(E), 300mm-4(a)(2)(A)(iii), and 300mm-4(b)(1)(B)(ix)) describe the roles of the Clinical Centers of Excellence (CCEs) and Data Centers (DCs) in providing outreach and retention activities.
- Sections 3311(a)(3)(A)(vi), 3312(b)(1)(B)(iii), 3312(b)(2)(B)(iv), 3312(b)(3)(B), and 3321(a)(1)(C)(i)(IV) of the PHS Act (42 U.S.C. §§ 300mm-21(a)(3)(A)(vi), 300mm-22(b)(1)(B)(iii), 300mm-22(b)(2)(B)(iv), 300mm-22(b)(3)(B), and 300mm-31(a)(1)(C)(i)(IV)) direct the Administrator of the WTC Health Program to establish an appeal process for responder and survivor enrollment, certification, and treatment denials.
The following provisions in the WTC Health Program regulations in 42 C.F.R. Part 88 are also applicable to this chapter:
- Sections 88.6(d)(2), 88.10(b), 88.12(b)(2), 88.13(c), 88.14, 88.18(c), 88.19(b), and 88.21 contain information on the appeals process for responder and survivor enrollment, certification, and treatment denials.
3. Roles and Responsibilities
Member services are a key function of most WTC Health Program components.
3.1 WTC Health Program
The WTC Health Program is a division of the National Institute for Occupational Safety and Health (NIOSH) which is within the Centers for Disease Control and Prevention (CDC) and administers Program services. The WTC Health Program oversees all member services functions, including enrollment, retention, complaints, and appeals, as well as Program communications, including outreach and education activities.
The Program responds to member inquiries, processes enrollments, maintains provider enrollments, oversees member transfers, and develops informational materials and communications, including WTC Health Program website content, which serves as a primary source of information about the Program for all interested parties. The WTC Health Program website can be found at: https://www.cdc.gov/wtc/.
The Program also oversees the development of informational materials about enrollment for potential members and educational information for current members, including the member handbook, annual newsletter, and fact sheets.
3.2 Clinical Centers of Excellence
CCEs provide a range of services to the members they serve. In addition to providing medical care, CCEs assist newly enrolled WTC Health Program members in accessing Program benefits, including scheduling medical appointments. CCE staff meet with potentially eligible populations and existing members face-to-face to provide benefits counseling and other information regarding the services available to them. They assist members in completing application forms and, when requested, submit the forms to the Program on the members’ behalf.
CCEs also conduct member retention activities, support member transfers, review and transmit completed health certification requests to the WTC Health Program, issue social services referrals, provide workers’ compensation assistance, conduct internal member services audits, assist with media relations, and ensure accurate records management.
3.3 Nationwide Provider Network
The Nationwide Provider Network (NPN) assists enrolled Program members who live outside the New York metropolitan area (NYMA) in accessing Program benefits, including scheduling medical appointments. The NPN also conducts education and retention activities for new members, supports member transfers, reviews and transmits completed health certification requests to the WTC Health Program, issues social services referrals, provides workers’ compensation assistance, conducts internal member services audits, manages media relations, and ensures accurate records management.
3.4 Data Centers
The Data Centers (DCs) help coordinate outreach activities with the CCEs and outreach and education contractors.
3.5 Health Program Support/Third-Party Administrator
The Health Program Support (HPS)/Third-Party Administrator (TPA) contractor receives and processes enrollment forms, submits requests for certification of health conditions, submits claims for payment, and responds to other correspondence and inquiries from members, CCEs/NPN, medical providers, pharmacies, and others. As part of its support, the HPS/TPA contractor manages phone information services through its call center.
3.6 Outreach and Education Contractors
Outreach and Education contractors are organizations that partner with NIOSH to support the needs of multiple WTC Health Program populations. These contractors provide additional outreach and education services on behalf of the Program. More information on the contractors is available at https://www.cdc.gov/wtc/outreach.html.
4. Communication Activities
The WTC Health Program implements a variety of activities to ensure full and effective communication with all Program members, potential members, and other interested parties.2 The Program’s communications activities include the following:
- A comprehensive public website is maintained at www.cdc.gov/wtc. This website provides background information on and news about the WTC Health Program; information, links, and downloadable forms for those who wish to apply; resources specific to each category of member; links to webpages on guiding legislation, regulations, policies, and supporting documents; and information about each of the CCEs and the NPN.
- A WTC Health Program annual newsletter includes benefit updates, Program statistics, health information, and other articles of interest to members. The newsletter is mailed to all members and is also posted on the WTC Health Program website.
- A variety of letters are sent to members, including welcome letters for newly enrolled members; letters to update members on their status at various points during the enrollment, certification, and appeal processes; and periodic special mailings to inform members of Program-wide matters, such as changes to benefits.
- The WTC Health Program maintains a general email inbox: WTC@CDC.gov. The WTC inbox is checked daily, Monday–Friday.
Member personal and medical information is handled in a manner that preserves and protects privacy and confidentiality in accordance with all legal requirements.
5. Outreach and Education
The WTC Health Program has a variety of mechanisms in place to communicate Program benefits and to reach potentially eligible populations for enrollment.
-
Outreach materials are developed in English, Spanish, Chinese, and Polish and are widely disseminated to inform potentially eligible populations about the Program and encourage those who are potentially eligible to apply. A list of current outreach materials can be found online at https://www.cdc.gov/wtc/print-materials.html. Examples of outreach materials include:
- A flyer describing the enrollment process;
- Palm cards and ads to encourage enrollment; and
- Video testimonials for the WTC Health Program website.
-
Educational materials are also created to communicate changes in Program benefits or procedures to current members. Examples include, but are not limited to:
- A fact sheet about the List of Covered Conditions;
- An overview of the steps a member should follow to appeal a Program decision; and
- An annual member newsletter.
- Several organizations have been funded through contracts to provide additional outreach and education services on behalf of the Program. These partner organizations are detailed at https://www.cdc.gov/wtc/outreach.html. Contract activities may include the development of public service announcements, conducting outreach at community meetings and health fairs, hosting webinars for potential members, and the development of additional outreach materials, as necessary.
- In addition to print materials and advertising, the Program uses digital platforms like Wikipedia , Facebook , and X , and regularly updates the Program website to keep Program members informed.
6. Member Retention
The CCEs and the NPN perform activities designed to retain members in the WTC Health Program. These activities include maintaining regular contact with currently enrolled members and encouraging continued participation in the Program. See Chapter 6, Clinical Centers of Excellence and Providers, for additional information about CCE member retention activities and Chapter 7, Nationwide Provider Network, for additional information about NPN member retention activities.
7. Phone Information Services
The WTC Health Program has established comprehensive phone information services via its Member Call Center to support education and outreach activities.
- The WTC Health Program Call Center is available at 1-888-982-4748 (1-888-WTC-HP4U), Monday through Friday, 9 a.m.–5. p.m. Eastern Time, to answer questions from members, providers, and others.
- The Call Center is the primary vehicle for responding to individual questions regarding Program benefits, activities, eligibility, enrollment, and claims. Call Center staff have access to information on a variety of Program-related services and resources, as well as member-specific information.
- In addition to the Program’s Call Center, each CCE and the NPN maintains phone information services to meet the needs of their member-specific populations. All contact information is available at https://www.cdc.gov/wtc/clinics.html.
- The Program’s Pharmacy Benefits Manager (PBM) also maintains phone information services (available at 1-800-935-7179).
8. Appeals
WTC Health Program applicants and members may appeal Program decisions regarding denial of enrollment, a decision to disenroll the member from the Program, a decision not to certify a health condition as a WTC-related condition, a decision not to certify a health condition as medically associated with a WTC-related health condition, a decision to decertify a WTC-related health condition, or a decision not to authorize treatment for a certified health condition based on a determination by the WTC Health Program that the treatment is not medically necessary. Appeals are specific to the type of decision rendered. A comprehensive discussion of the appeals process is available at https://www.cdc.gov/wtc/appeals.html.
Summaries of the Eligibility and Enrollment appeals processes can be found in Chapter 2, Eligibility and Enrollment and Chapter 3, Certification of Health Conditions, which includes a description of the appeals processes for denials of certification of a health condition and decertification of a health condition. Chapter 4, Medical Benefits, describes appeal processes for denial of treatment authorization. Appendix 8-A is a fact sheet that outlines the appeals process. It is sent to any member receiving a denial decision for certification of a health condition.
9. Member Concerns
The WTC Health Program addresses member concerns through various mechanisms. In addition to the communication channels outlined above, members can discuss their concerns with their CCE/NPN. The Program has a feedback form on its website, available at https://oasis.cdc.gov/feedback, that allows members to send formal feedback or complaints. Additionally, concerns are reviewed through congressional inquiries and letters sent directly to the Program or its Administrator.
10. Disruptive Behavior
Disruptive behavior from a member potentially impedes WTC Health Program operations and affects the delivery of health care services. The WTC Health Program does not tolerate behavior that shows disrespect for others, or any interpersonal interaction that impedes delivery of care. If such incidents are reported to the Program, immediate steps will be taken to address this behavior and to help ensure a safe and respectful environment for our members, staff, representatives, and affiliated facilities and personnel.
Examples of disruptive behavior include:
- Repeatedly missing appointments,
- Failing to follow Program or CCE/NPN policies and procedures,
- Altering statements or providing false information to obtain benefits such as enrollment or certification,
- Harassment, verbal abuse, stalking, acts or threats of violence towards staff or other patients,
- Engaging in illegal behavior.
The Program or CCE/NPN may take measures for addressing disruptive behavior, which can include:
- Restrictions on in-person visits,
- A requirement to adhere to a Behavioral Plan to continue seeing a provider,
- Limiting communication to written correspondence only,
- Discharge from the CCE/NPN or provider,
- Involvement of law enforcement authorities if necessary.
If a member is discharged from the CCE/NPN due to disruptive behavior, the member may request a transfer to another clinic. If a member cannot be assigned to another CCE/NPN, care through the Program may be suspended.
11. Appendix
Chapter 9—Fraud, Waste, and Abuse
TABLE OF CONTENTS
Last Revised – August, 2014
1. Purpose and Scope
The purpose of this WTC Health Program Fraud, Waste, and Abuse (FWA) policy is to describe the measures taken to prevent, detect, and deter the FWA of public funds. FWA activities target the potential causes of FWA from inadvertent errors to willful deception.
The scope of the WTC Health Program FWA policy includes all areas of the WTC Health Program that could be vulnerable to FWA. These areas include, but are not limited to
- Member Eligibility and Enrollment (Section 4.1)
- Outreach and Education (Section 4.2)
- Provider Credentialing and Registration Section 4.3)
- Health Condition Certification (Section 4.4)
- Medical Benefits (Section 4.5)
- Pharmacy Benefits (Section 4.6)
- Payment for Healthcare Services (Section 4.7)
- Payment for Pharmacy Benefits (Section 4.8)
- Recoupment Activities (Section 4.9)
- Program Performance. (Section 4.10)
2. Statutory and Regulatory References
The Public Health Service Act
The following sections of Title XXXIII of the Public Health Service (PHS) Act are applicable to this chapter:
-
Section 3301(d)(1)-(2):
- FRAUD. -- The Inspector General of the Department of Health and Human Services shall develop and implement a program to review the WTC Program’s health care expenditures to detect fraudulent or duplicate billing and payment for inappropriate services. This title is a Federal health care program (as defined in section 1128B(f) of the Social Security Act) and is a health plan (as defined in section 1128C(c) of such Act) for purposes of applying sections 1128 through 1128E of such Act.
- UNREASONABLE ADMINISTRATIVE COSTS. – The Inspector General of the Department of Health and Human Services shall develop and implement a program to review the WTC Program for unreasonable administrative costs, including with respect to infrastructure, administration, and claims processing.
-
Section 3305(b)(1)(B)(iv) states that a Clinical Center of Excellence (CCE) must agree to:
- Have in place safeguards against fraud that are satisfactory to the Administrator and consistent with the Inspector General of the Department of Health and Human Services.
https://www.gpo.gov/fdsys/pkg/USCODE-2015-title42/pdf/USCODE-2015-title42-chap6A-subchapXXXI.pdf
Other laws and statutes also have direct impact on protecting against FWA. Federal laws include, but are not limited to, the following:
- The Health Care Fraud Statute (18 U.S.C. § 1347)
- The False Claims Act (18 U.S.C. §§ 3729 – 3733)
- The Anti-Kickback Statute (42 U.S.C. §§ 1320a-7b)
- Exclusion Provisions (42 U.S.C. § 1320a-7)
- The Civil Monetary Penalties Law (42 U.S.C. § 1320a-7a)
Health Care Fraud Statute
The Health Care Fraud Statute makes it a criminal offense to knowingly and willfully execute a scheme to defraud a health care benefit program. Health care fraud is punishable by imprisonment for up to 10 years. It is also subject to criminal fines of up to $250,000. Specific intent to violate this section is not required for conviction. 18 U.S.C. § 1347.
https://www.gpo.gov/fdsys/pkg/USCODE-2015-title18/pdf/USCODE-2015-title18-partI-chap63-sec1347.pdf
False Claims Act
The False Claims Act establishes civil liability for offenses related to certain acts, including knowingly presenting a false or fraudulent claim to the government for payment, and making a false record or statement that is material to the false or fraudulent claim. “Knowingly” includes not only actual knowledge but also deliberate ignorance or reckless disregard for the truth or falsity of the information. No specific intent to defraud the government is required. Depending on the circumstances, some examples of potential False Claims Act violations in the health care fraud context include upcoding, billing for unnecessary services, billing for services or items that were not rendered, and billing for services performed by an excluded individual. 31 U.S.C. § 3729.
Individuals and entities that make false claims are subject to civil penalties of up to $11,000 for each false claim, plus three times the amount of damages the government sustains by reason of each claim. Violation of the False Claims Act may lead to exclusion from Federal health care programs. 31 U.S.C. § 3729.
Civil legal actions for penalties and damages under the False Claims Act may be brought not only by the government, but by private persons, such as competitors or employees of a provider, on behalf of the government. If the legal action is successful, the private person is entitled to a percentage of the recovery. The False Claims Act protects all persons from retaliation for reporting false claims or bringing legal actions to recover money paid on false claims. 31 U.S.C. § 3730.
Failure to return overpayments may lead to liability under the False Claims Act. Under section 1128J(d) of the Social Security Act, persons who have received an overpayment from a Federal health care program must report and return the overpayment within 60 days of the date the overpayment was identified. Failure to do so may make the overpayment a false claim. 42 U.S.C. § 1320a-7k; 31 U.S.C. § 3729.
False claims made knowingly may also be subject to criminal prosecution. Persons who knowingly make a false claim may be subject to criminal fines up to $250,000 and imprisonment of up to 5 years. 18 U.S.C. §§ 287; 3571.
Anti-Kickback Statute
The Anti-Kickback Statute, found in Section 1128B(b) of the Social Security Act, prohibits the knowing and willful offer, payment, solicitation, or receipt of any remuneration, in cash or in kind, to induce or in return for referring an individual for the furnishing or arranging of any item or service for which payment may be made under a Federal health care program. Remuneration means anything of value and can include gifts, under-market rent, or payments that are above fair market value for the services provided. Criminal penalties for violation are a fine of up to $25,000 and imprisonment for up to 5 years. 42 U.S.C. § 1320a-7b.
Compliance with the Anti-Kickback Statute is a condition of payment in Federal health care programs. Claims that include items or services resulting from a violation are not payable and may constitute false or fraudulent claims under the False Claims Act. 42 U.S.C. § 1320a-7b.
Under the Civil Monetary Penalties Law, Social Security Act Section 1128A(a)(7), the U.S. Department of Health and Human Services, Office of Inspector General (HHS-OIG) may impose civil penalties for violations of the Anti-Kickback Statute. The penalties are up to $50,000 per violation plus three times the amount of the remuneration. Violation of the Anti-Kickback Statute may also lead to exclusion from Federal health care programs. 42 U.S.C. § 1320a-7a.
The Anti-Kickback Statute provides safe harbors for certain arrangements, such as personal services and rental agreements, investments in ambulatory surgery centers, and payments to bona fide employees. Physicians with questions about the Anti-Kickback Statute and these safe harbor arrangements should consult the regulations and guidance documents available from HHS-OIG. 42 C.F.R. § 1001.952.
Exclusion Provisions
Under Section 1128 of the Social Security Act, HHS-OIG has authority to exclude individuals from participating in Federal health care programs, including Medicaid, for various reasons. Exclusions can be mandatory, meaning HHS-OIG has no choice about whether to exclude, or discretionary, which means the HHS-OIG does have a choice. Exclusion is mandatory for convictions of program-related crimes, convictions related to patient abuse, felony convictions related to health care fraud, and felony convictions related to controlled substances. Exclusion is discretionary for loss of license due to professional competence or financial integrity, convictions related to fraud, convictions related to obstruction of an investigation or audit, misdemeanor convictions related to controlled substances, and participation in prohibited conduct such as kickbacks and false statements. 42 U.S.C. § 1320a-7.
Generally, Federal health care programs will not pay for items or services furnished, ordered, prescribed, or supplied by an excluded individual or entity. 42 C.F.R. § 1001.1901.
Under the Civil Monetary Penalties Law, Social Security Act Section 1128A, HHS-OIG may impose civil monetary penalties of up to $10,000 per item or service claimed while excluded. HHS-OIG may also impose an assessment of up to three times the amount claimed. 42 U.S.C. § 1320a-7a.
1 While a health care professional who provides services through Medicaid may employ an excluded individual who does not provide any items or services paid for, directly or indirectly, by Federal health care programs, practitioners should exercise caution. A professional who contracts with or employs “a person that the provider knows or should know is excluded by OIG … may be subject to CMP (Civil Monetary Penalty) liability if the excluded person provides services payable, directly or indirectly, by a Federal health care program.” The prohibition is not limited to items or services involving direct patient care, but extends for example to filling prescriptions, providing transportation services, and performing administrative and management services that are not separately billable. See U.S. Department of Health and Human Services, Office of Inspector General, “Updated Special Advisory Bulletin on the Effect of Exclusion From Participation in Federal Health Care Programs,” (May 8, 2013). Available at https://oig.hhs.gov/exclusions/files/sab-05092013.pdf. If, for example, a biller is excluded from a government health care program, payments on claims submitted by the practice through the biller may be considered overpayments subject to recoupment. Any person who has received an overpayment must return the money within 60 days of the date on which the overpayment was identified. Failure to do so may subject the person to liability under the False Claims Act and the Civil Monetary Penalties Law. 42 U.S.C. 1320a-7k.
2 It is in the best interest of physicians and other providers to screen potential employees and contractors prior to employment or hiring to ensure they are not excluded from participating in Federal health care programs. In addition, providers should regularly check the exclusions database to ensure that none of the practice’s employees or contractors have been excluded. The Centers for Medicare & Medicaid Services (CMS) has issued guidance to State Medicaid agencies that they should require providers to screen their employees and contractors for exclusions by checking the database on a monthly basis. The guidance further advises States to require all providers to report any exclusion information discovered immediately. The List of Excluded Individuals/Entities (LEIE) database is available at https://exclusions.oig.hhs.gov/ on the HHS-OIG website. Both licensed and unlicensed individuals may be excluded, so it is best to check for both. In addition to checking the LEIE, providers should check the Exclusions Extract, which can be accessed by visiting https://www.sam.gov/ on the System for Award Management website. Centers for Medicare & Medicaid Services, State Medicaid Director Letter 09-001 (p. 4), (Jan. 16, 2009). Available at https://downloads.cms.gov/cmsgov/archived-downloads/SMDL/downloads/SMD011609.pdf.
Civil Monetary Penalties Law
As previously noted, the Civil Monetary Penalties Law, Section 1128A of the Social Security Act, authorizes HHS-OIG to impose civil penalties for violations of the Anti-Kickback Statute as well as a range of other violations. Penalties range from $10,000 to $50,000 per violation. These violations include, but are not limited to, the following:
- Submitting false claims
- Violating Medicare assignment provisions or the physician agreement;
- Providing false or misleading information expected to influence a decision to discharge a patient;
- Failing to provide an adequate medical screening examination for patients who present to a hospital emergency department with an emergency condition or in labor; and
- Making false statements on applications or contracts to participate in a Federal health care program.
42 U.S.C. § 1320a-7a.
3. Categories of FWA
Each suspected case of FWA is reviewed to categorize the allegation as Fraud, Waste, or Abuse. Intent is the key distinction between Fraud and Abuse. An allegation of waste and abuse can escalate into a fraud investigation if a pattern of intent is determined.
Fraud is defined as an intentional deception, false statement, or misrepresentation made by a person with the knowledge that the deception could result in unauthorized benefit to oneself or another person. It includes any act that constitutes fraud under applicable federal or state law. It is a crime to defraud the Federal Government and its programs. 18 U.S.C. § 1001. Punishment may involve imprisonment, significant fines, or both. Criminal penalties for health care fraud reflect the serious harms associated with health care fraud and the need for aggressive and appropriate fraud prevention. In some states, providers and health care organizations may lose their licenses. Convictions also may result in exclusion from participation for a specified length of time. Fraud may also result in civil liability.
Examples of Fraud Could Include:
- Providing false statements on an enrollment application to obtain coverage or concealing information about past medical history/preexisting conditions.
- Using someone else’s ID card or loaning your ID card to someone not entitled to use it.
- Failing to report other insurance or to disclose claims that were a result of a work related injury.
- Billing for services that were not rendered.
- Providing services that are not medically necessary for the purpose of maximizing reimbursement.
- “Upcoding”—billing for a more costly service than was actually provided.
- “Unbundling”—billing each step of a test or procedure as if it were separate instead of billing the test or procedure as a whole.
- Submitting claims with false diagnoses to justify tests, surgeries or other procedures that are not medically necessary.
- Accepting kickbacks for member referrals.
Waste is defined as failure to control costs or regulated payment associated with federal program funding. Furthermore, waste results in taxpayers not receiving reasonable value for their money. Waste relates primarily to mismanagement, inappropriate actions, or inadequate oversight.
Examples of Waste Could Include:
- Poor execution or lack of widespread adoption of best practices, such as effective preventive care practices or patient safety best practices.
- Unnecessary hospital readmissions, avoidable complications, and declines in functional status, especially for the chronically ill.
- Overtreatment.
- Administrative complexity.
Abuse is defined as practices that are inconsistent with professional standards of care; medical necessity; or sound fiscal, business, or medical practices.
Examples of Abuse Could Include:
- Billing for services that were not medically necessary
- Charging excessively for services or supplies
- Coding and billing for 99215 Office or other outpatient visit Evaluation and Management (E/M) for one hour when the visit was actually only 15 minutes.
4. FWA Responsibilities and Activities
Detecting, preventing, and reporting FWA are the responsibilities of everyone associated with the WTC Health Program including employees, members, providers, and contractors.
The WTC Health Program will closely monitor program activities to detect or prevent any FWA. The WTC Health Program will report fraudulent conduct to federal law enforcement agencies and violators may be subject to criminal, civil, or administrative penalties. Information concerning suspected fraud related to the WTC Health Program by contractors, grantees, health care providers, or individual recipients will be reported to the Department of Health and Human Services Office of Inspector General (OIG) by phone at 1-800-HHS-TIPS (1-800-447-8477); online at oig.hhs.gov/report-fraud; or in writing to the following address: U.S. Department of Health and Human Services, Office of Inspector General, ATTN: OIG HOTLINE OPERATIONS, P.O. Box 23489, Washington, DC 20026.
The WTC Health Program has instituted FWA activities including:
- Developing and implementing a WTC Health Program FWA Policy
- Providing FWA education
-
Requiring all contractors to develop and implement a FWA policy
- Clinical Centers of Excellence
- Data Centers
- Nationwide Provider Network
- Health Program Support
- Pharmacy Benefits Manager
- Health Program Evaluation
- Health Insurance Matching Program
- Performing data reviews to detect potential instances of FWA
- Performing FWA audits (internal and external).
The following areas of the WTC Health Program incorporate measures and activities to protect against FWA:
4.1 Member Eligibility and Enrollment
The full application and enrollment process is described in the WTC Health Program Policy and Procedure Manual (PPM, Chapter 2). Using an online portal or by submitting a paper application, applicants apply to the program and submit supporting documentation related to their activities, location, and time periods of exposure. Applications are reviewed for completeness and compliance with the relevant eligibility criteria established in Title XXXIII of the PHS Act and 42 C.F.R. part 88. Quality Control checks are built into the workflow and there is an appeals process for denials of enrollment (see 42 C.F.R. § 88.14). Internal audits of enrollment are conducted on a quarterly basis. Performance metrics are used to monitor the completeness and timeliness of the application/enrollment process, and outreach and communication services. These Quality Control checks facilitate the identification of potential instances of FWA.
4.2 Outreach and Education
Outreach and education materials, including the Member Handbook, incorporate information on member FWA responsibilities, such as avoiding potential fraudulent enrollment. Various Program activities also help to ensure that resources are used efficiently and waste is avoided. The WTC Health Program works strategically with the Responder and Survivor Steering Committees, Clinical Centers of Excellence (CCEs), the Nationwide Provider Network (NPN), and the Data Centers (DCs) to evaluate program participation and client satisfaction. The program seeks to maintain contact with currently enrolled members and to increase participation for those who have been inactive in program follow-up. Together with CCEs, NPN, DCs, and Steering Committees, the WTC Health Program identifies and reduces barriers that affect member participation. The tools employed include surveys, newsletters, websites, key informant feedback, and scheduling reminders.
4.3 Provider Credentialing and Registration
The CCEs/NPN have primary responsibility for safeguarding against fraudulent providers. The CCEs/NPN vary in how they provide medical services; some do most of the services in-house while others refer many services to outside providers. External providers affiliated with the CCEs are credentialed and enrolled in the Program through a third party provider management sub-contractor under a WTC Health Program Support (HPS) contract. This provider management sub-contractor screens CCE-affiliated external providers against the OIG/GSA exclusion lists and/or the CMS Fraud Investigation Database, conducts criminal background checks, establishes business agreements which include a provision that the agreement with the WTC Health Program may be terminated immediately for fraudulent billing, gives guidance to the providers on the limited nature of the WTC Health Program and what costs may be appropriately paid, and informs the network providers of the authorization and billing requirements for member care including the following:
- Referrals from the CCEs are for specific evaluation and care covered by the WTC Health Program;
- Provider bills will be authorized by the CCEs following principles of medical necessity within the limitations set forth by the WTC Health Program;
- Charges will be paid according to billed amounts up to the maximum fee schedule set by the Department of Labor’s Office of Workers Compensation Program (FECA price) or other rate structures approved by the Administrator, with no balance billing of the member;
- Prescribing privileges for providers are individually authorized by the CCEs; and the allowed medications are constrained to the member’s assigned pharmaceutical benefit plan.
External providers affiliated with the NPN are credentialed and enrolled through a separate third party administrator under United Health Care (UHC). NPN authorizes provider bills in the same manner as the CCEs.
Once CCEs/NPN request registration of a provider in the program, the HPS contractor registers the provider in the claims system so that they can be paid. As part of this registration process, the HPS contractor verifies the validity of the provider’s National Provider Identification (NPI) number.
4.4 Health Condition Certification
The WTC Health Program provides a limited health care coverage for qualifying certified WTC-related and medically associated conditions. Treatment benefits are controlled through administrative certification of health conditions on an individual member basis (see PPM Chapter 3 for full details). This process, outlined in Title XXXIII of the PHS Act and in 42 C.F.R. part 88, enables the mandatory requirements for coverage to be determined through a two-step process that first entails a clinical diagnostic evaluation which is subsequently reviewed by a federal official for certification. The process has data quality and control checks built into the workflow, including an administrative appeals procedure (see 42 C.F.R. § 88.21), a decertification procedure (see 42 C.F.R. § 88.19), member communication regarding health condition certification denials, and a procedure for the Administrator’s discretionary reopening of decisions (see 42 C.F.R. § 88.25). The HPS contractor and CCE/NPN exchange certification data to ensure alignment of member information for benefit management. The two-step process consisting of an initial CCE/NPN physician determination, followed by a review and certification by the Administrator or designee provides distinct exercise of independent judgement of the relatedness of the medical diagnosis with exposure information to effect certification of conditions, thus further safeguarding certification against FWA.
4.5 Medical Benefits
The medical benefits available under the program are detailed in Chapter 4 of the PPM. This chapter of the PPM includes FWA mitigation procedures that help prevent unnecessary or unauthorized services being paid under the program.
The WTC Health Program maintains a Code Book of the allowable billing codes by specific benefit plans. The Code Book categorizes the benefit plans for the initial health evaluation, periodic medical monitoring, cancer screening, diagnostic evaluation, and treatment of specific certified conditions (through “care suites”). Further details about benefit control can be found in Chapter 4. There is an administrative medical change control process that ensures oversight for any requested change to the Code Book; and quality control checks are built into the workflow. The Code Book is also subject to modification based on evaluation of reasons for denied service claims, updates to medical guidelines or policy, coding updates from source organizations, and when new health conditions are added for program coverage.
The CCEs, DCs, and NPN must adhere to an operations manual that specifies how they are implementing the tasks in their performance work statement. The elements are addressed in Chapters 6, 7, and 8 of the PPM. These operations include quality assurance metrics for scheduling, completion of all components of the examination and testing, notification and counseling about results and providing professional referrals for further evaluation or treatment compliant with program policy and standards of medical practice.
The WTC Health Program meets with the clinical directors and administrators of the CCEs, DCs, and NPN on a regular basis to calibrate and clarify medical and administrative policies and procedures. Minutes of these meetings are taken and sent out to all participants. Practice guidelines following principles of medical necessity and community standards of care are produced by the DCs in consultation with the CCEs and approved for implementation by the WTC Health Program.
4.6 Pharmacy Benefits
Prescription medications are a significant expenditure for member treatment under the WTC Health Program. Significant controls are in place to prevent FWA and ensure that only those drugs in a specific formulary are authorized and paid by the program.
WTC Health Program members receive outpatient medication to control certified conditions and medically associated conditions arising from the 9/11 terror attacks. Members with certified health conditions are assigned a specific pharmacy benefit plan. Each pharmacy benefit plan has a closed formulary, authorization controls for certain medications, and provides the pharmacist with safety messaging and real-time claims processing at the point of sale. Chapter 12 provides details regarding these benefit plans and the formulary change control process that ensures oversight for requested changes to program formularies. The plan formularies undergo periodic review by the Medical Benefits Team. The WTCHP medical and pharmacy teams work with the CCEs and NPN to determine prescribing patterns, medical necessity criteria, safety concerns, and make cost assessments. The pharmacy team analyzes paid claims and conducts on site audits of the CCE’s to ensure prescriptions are used for certified conditions. New drugs and drug requests get reviewed monthly to determine if they should be added to the formulary. The pharmacy team reviews most frequently prescribed medications, brand vs generic, single source brand use, overrides, DEF costs, coordination of benefits for survivors, opioid use, pharmacy overrides such as prior authorizations, prescription not covered, and refill too soon.
4.7 Payment for Healthcare Services
Claims processing and payment is a critical area in the protection against FWA in the WTC Health Program.
The WTC Health Program uses a fee-for-service reimbursement strategy for health care services (see Chapter 5). The only exception is a capitated fee for a group of services constituting the standardized initial health and annual medical monitoring examination for eligible members (see Chapter 4). The WTC Health Program pays the approved rates to an enrolled provider, for covered, correctly coded and correctly billed services, provided to an eligible beneficiary (see 42 C.F.R. § 88.22).
The claims processing system has been designed to guard against FWA by reducing payment errors by preventing the initial payment of claims that do not comply with the WTC Health Program coverage, coding, payment and billing policies. To maintain or improve provider compliance and lower the error rate, the WTC Health Program follows these parallel strategies:
- Support and promote the use of industry-standard electronic claims submission to optimize claims processing efficiency;
- Ensure the integrity of the HPS contractor’s automated claims processing system logic to verify member status, provider status, and the WTC Health Program coverage and medical policies pertaining to assigned benefit plan(s) based on certification of health condition(s);
- Educate the CCEs/NPN about all health care benefit policies and procedures and how these are presented in the WTC Health Program Code Book;
- Apply the software for the CMS National Correct Coding Initiative, the Department of Labor’s Federal Employees Compensation Act (FECA ) fee schedule, and the CMS Inpatient Prospective Payment System to the HPS contractor’s claims processing workflow to ensure correct coding and pricing;
- Apply a contractual policy limitation requiring that claims be submitted within fifteen (15) months of the date of service to qualify for payment (claims involving coordination of benefits must be submitted within 18 months of the date of service);
- Align payment records with CCEs/NPN, and provide electronic remittance advice notices to providers;
- Identify provider noncompliance with coverage, coding, billing, and payment policies through analysis of data (e.g., profiling utilization of services by CCEs/NPN, types of conditions, high cost, high frequency, or other anomalies);
- Correct past improper payments through claims adjustment and CCEs/NPN education;
- Assess and rectify CCEs/NPN authorization practices with respect to improper bill processing (error rate);
- Audit processed claims to ensure accuracy of payments by the automated system;
- Retrospectively recoup funds due from workers’ compensation carrier(s) using a third party Health Insurance Matching Program contractor.
The CCEs, the NPN, and the HPS contractors analyze provider compliance with WTC Health Program coverage and coding rules and take appropriate corrective action when providers are found to be non-compliant. For example, some errors are the result of provider misunderstanding or failure to pay adequate attention to Program policy. Other errors may represent calculated plans to knowingly acquire unwarranted payment. The CCEs/NPN evaluate the circumstances surrounding the errors and proceed with the appropriate plan of correction. If errors continue to be repeated, or if the errors suggest potential fraud or a pattern of abuse, then more severe administrative action is initiated.
The HPS contractor consults with industry experts to identify medical practice and technology changes that may result in improper billing or program abuse to propose areas for data analysis and remedial action as needed. Types of service claims are routinely assessed for patterns of waste or abuse include, but are not limited to:
- Oxygen and other durable medical equipment
- Administration of anesthesia
- Contrast material for imaging studies
- Psychotherapy service intensity
- Modifier codes indicating multiple surgeries on the same day
- Emergency department services
- Evaluation and management service level of intensity.
While automation is the preferred mode of operation for the claims processing system to minimize error from human touch, based on program findings, the following types of claims are routinely handled through manual processing:
- Cancer, emergency room service and professional services associated with inpatient confinement, since these were beyond the original design of the outpatient Code Book;
- Skilled nursing facility and home care service intensity;
- Drug and alcohol rehabilitation service intensity;
- Procedures that do not have an automated fee determined;
- Contradictions in coding associated with point of service, type of bill, procedure, or revenue code;
- Dental claims, since these are processed according to different industry standards and volume is low;
- Prior authorization (Level 3) requirement by WTC Health Program medical staff.
Metrics are monitored that assess electronic claims submission accuracy, claims processing time, auto-adjudication success and accuracy, claims volume and payment adjustments, volume and reasons for claims being denied or pended for further resolution, and compliance with the Prompt Payment Act.
4.8 Payment for Pharmacy Benefits
All points of sale are connected to the program’s contracted pharmacy benefit manager through software transmitting claims processing rules and safety notices to the pharmacist at the point of sale. The rules require verification of member, pharmacy plan assignment, an authorized prescriber, a supply limit and prevent early refills, off-formulary product dispensing, and dispensing of duplicate ingredients or supplies. Higher tier drugs or select products that may be prone to misuse or abuse require additional authorization by the CCE/NPN in the system before the pharmacist can fill the prescription. Prescriptions are filled with generic formulations unless a brand is authorized. Brand availability on the formulary is subject to considerations of therapeutic efficacy, allergy to ingredients, side effect profile, patient adherence factors, safety, and cost. Continual monitoring to optimize pharmacy cost control strategies include the following:
- Assignment of certain preferred brands to negotiate price/rebate with manufacturer;
- Consistent pricing agreements, including maximum allowable cost, among participating retail chains for brand and generics;
- Improved pricing for mail order pharmacy arrangement on generics;
- Selecting preferred specialty pharmacy for compound medications to control price and quality control;
- Step therapy for medications;
- Split dispensing strategies to ensure effectiveness and side effect tolerance for oral anti-neoplastics;
- Timely alignment of prescribing controls to match shifts in marketing (generic availability and more cost effective over-the-counter preparations);
- Services for drug utilization analyses, pharmacy audits, and provider record audits for policy compliance.
4.9 Recoupment Activities
The following administrative improvements enhance controls for FWA. Title XXXIII of the PHS Act requires recoupment of treatment costs for WTC-related health conditions and medically associated health conditions if the condition is work-related (see also 42 C.F.R. § 88.24). The WTC Health Program determined that the CCEs and NPN did not have the resources to manage this requirement, so an alternative approach was implemented that utilizes the New York State Workers’ Compensation Board Health Insurance Match Program (HIMP) that assists health insurers and health benefits plans to set up a system to identify claims that they have paid which may be the responsibility of the employer, workers' compensation insurance carrier, or special fund, and to obtain reimbursement therefore. The WTC Health Program awarded a contract to HMS Federal to implement the HIMP for our program in September, 2014. The WTC Health Program receives monthly reports on recoupment activities. Since HIMP is a comprehensive and efficient process that interacts directly with the New York State Workers’ Compensation Board and insurers, more funds are recovered and verification of appropriate claims payment is increased.
Additionally, the WTC Health Program is in the process of posting a solicitation to address the provider payments accounts receivables aging balances associated with overpayments made to providers in excess of amounts owed or payments made in error. All overpayments identified as un-recouped (all efforts to offset have been exhausted) will be turned over to the WTC Health Program’s debt collection support services contractor to collect the debt owed the Federal Government. The debt collection support services contract is expected to be awarded during second quarter of 2018.
4.10 Program Performance
The WTC Health Program has created an online set of policies and procedures for transparency and consistency in program administration. In addition to this PPM chapter on FWA, there are requirements for the Health Insurance Portability and Accountability Act (HIPAA) and the Federal Information Security Management Act (FISMA).
Working with the HHS Program Integrity Initiative, the WTC Health Program is addressing data security and privacy (HIPAA and FISMA), resource alignment for performance requirements of CCEs/NPN to comply with benefit administration, streamlining the process of program application/processing, and program communication. In addition, the WTC Health Program periodically reviews metrics that provide qualitative and quantitative measures to assess the Program’s performance on customer service, pharmacy utilization, claims processing, and cost efficiency of managing the WTC Health Program. Review of these metrics facilitates the identification of potential instances of FWA.
5. FWA Allegation Investigation and Resolution Procedure
The WTC Health Program has a Fraud Prevention Officer (FPO) and a Fraud Risk Assessment Team (FRAT) in place who adhere to established procedures for processing allegations pertaining to FWA when received. The FRAT includes the FPO, the WTC Health Program Deputy Division Director, the Office of the General Counsel (OGC), and any other relevant parties related to the specific allegation. The WTC Health Program provides stakeholders with information about the Program’s FWA efforts and procedures through information included on the WTC Health Program website and in the Member Handbook. Allegations of FWA are to be reported to the FPO. In addition, the HHS OIG has a website dedicated to reporting possible FWA. (https://oig.hhs.gov/fraud/report-fraud/index.asp )
If the allegation of FWA comes to the WTC Health Program from the OIG, the FPO will work with the OIG, as requested, to assist with the OIG investigation. When an allegation of FWA is received from any source other than the OIG by the WTC Health Program, the allegation is immediately forwarded to the FPO. The FPO will record receipt of the allegation on the FWA Intake Form, enter the FWA allegation into the FWA Allegation Status Log, and begin an initial investigation to determine if the allegation should be categorized as fraud, waste, or abuse.
As a result of the initial investigation, if the allegation is categorized as potential fraud, the FPO will gather any relevant information and forward the case to the OIG for investigation. The FPO will monitor the status of the OIG investigation and report the OIG’s findings and resolution to the FRAT.
If the allegation is determined to be either waste or abuse, the FPO will continue the WTC Health Program’s internal investigation of the allegation with the assistance of any relevant personnel. Once the investigation is completed, the FPO will present the results of the investigation to the FRAT along with a recommended resolution. The FPO is responsible for ensuring the waste or abuse allegation is resolved based on the decision of the FRAT. The FPO is also responsible for ensuring the waste or abuse investigation and resolution are documented and reported to the appropriate HHS/CDC contact, as required.
Chapter 10—Governmental Affairs
TABLE OF CONTENTS
Last Revised – April, 2025
1.0 Purpose and Scope
The World Trade Center (WTC) Health Program provides healthcare benefits according to the provisions of the James Zadroga 9/11 Health and Compensation Act of 2010 1 (the Zadroga Act), as amended. The Zadroga Act established the WTC Health Program within the U.S. Department of Health and Human Services (HHS). The Program is administered by the National Institute for Occupational Safety and Health (NIOSH), which is a part of the Centers for Disease Control and Prevention (CDC) within HHS.
This chapter describes the relationships and collaborations between the WTC Health Program and various government agencies, some of which have statutory and regulatory roles.
2.0 Oversight and Compliance
2.1 Department of Health and Human Services
- Office of the Inspector General— The Office of the Inspector General (OIG) is required by the Zadroga Act to provide oversight to prevent fraud and unreasonable administrative costs.2 The OIG has developed and implemented programs that review healthcare expenditures for fraudulent or duplicate billing and payment for inappropriate services, as well as monitor Program costs related to infrastructure, administration, and claims processing.3 Additionally, the OIG has the authority to initiate reviews of other Program components as needed.4 OIG reports and other external audits and reports are available here: WTCHP External Audits and Reports.
- Office of the General Counsel— The Office of the General Counsel (OGC) supports the development and implementation of the WTC Health Program by providing legal advice and representation to the WTC Health Program to ensure compliance with the Zadroga Act and other applicable federal laws and regulations.
2.2 Government Accountability Office
To ensure oversight of the Program’s activities, the Government Accountability Office (GAO) conducts ongoing quality assurance and other audits. Reports from GAO audits, as well as other external audits and reports related to the WTC Health Program, can be accessed on the WTCHP External Audits and Reports page.
The Zadroga Act assigned several responsibilities to the GAO to be completed at the outset of the Program in 2011.5 The resulting GAO briefing covered three main areas: (1) the CDC/NIOSH schedule for awarding contracts to the Clinical Centers of Excellence (CCEs), (2) healthcare claims data for the CCEs and planned procedures, and (3) the Administrator of the WTC Health Program’s plans for evaluating each CCE system’s healthcare claims data capabilities during and after contract awards.6 GAO also issued a report that evaluated various aspects of the then-forthcoming Program’s feasibility, efficiency, and effectiveness.7 These analyses investigated whether:
- Using one consolidated data center was preferable to using multiple data centers;8
- The U.S. Department of Veterans Affairs could provide monitoring and treatment to members living outside the New York metropolitan area more efficiently and effectively than the nationwide provider network (NPN);9 and
- Using an existing federal prescription drug purchasing program would provide benefits more efficiently and effectively than through the Program.10
These analyses were submitted to the House Committee on Energy and Commerce and to the Senate Committee on Health, Education, Labor, and Pensions.
In 2015, an amendment to the Zadroga Act assigned an additional reporting responsibility to the GAO.11 The first report, due within 18 months of December 18, 2015, was required to assess the effectiveness of the following:12
- The Program’s quality assurance program;
- The procedures for providing certifications of coverage of conditions as WTC-related health conditions for enrolled WTC responders as well as screening-eligible and certified-eligible survivors; and
- Any action taken under the WTC Health Program to ensure appropriate benefit payments and coordination of benefits for enrolled individuals.
Subsequent assessments are required every five years thereafter through fiscal year 2042.13 In preparing the reports, the Comptroller General must consult with the Senate Committee on Health, Education, Labor, and Pensions and the House Committee on Energy and Commerce regarding assessment objectives and then submit their report to these congressional committees for each five-year reporting period.14
2.3 Congressional Oversight
Under the provisions of the Zadroga Act, the Administrator is required to submit an annual report on the Program’s operations to Congress.15 The report includes, for example, statistics on enrollment, costs of monitoring, screening and treatment, administrative costs and performance, and a summary of new scientific reports or studies that address WTC-related exposures.16 Oversight of the WTC Health Program. is vested in the Senate Committee on Homeland Security and Governmental Affairs and the Senate Committee on Health, Education, Labor, and Pensions, as well as the House Subcommittee on Health under the House Committee on Energy and Commerce.
Additionally, the Zadroga Act directs the Secretary of HHS to notify Congress when enrollments of WTC responders and certifications for certified-eligible WTC survivors reach 80% of numerical limitations set forth in the Act.17 These limits are described in more detail in Chapter 2, Eligibility and Enrollment.
3.0 Grants and Contract Management
3.1 CDC Office of the Director
The CDC Director oversees NIOSH administration of the WTC Health Program. CDC Office of the Director staff, as well as other CDC offices as appropriate, review performance plans, document progress, identify risks, and intercede as necessary to ensure the highest standards of performance.
3.2 CDC Office of Financial Resources
The CDC’s Office of Financial Resources (OFR) assists the WTC Health Program with acquisitions and related activities. OFR is the only entity within CDC that can obligate federal funds. OFR helps implement initiatives and acquisitions for the WTC Health Program through non-programmatic management of financial assistance (grants and cooperative agreements) and contract activities. These responsibilities are carried out by OFR’s Office of Grants Services and Office of Acquisition Services, respectively.
3.3 NIOSH Office of Extramural Programs
The Office of Extramural Programs (OEP) is included within the NIOSH Office of the Director. Under the direction of NIOSH’s Associate Director for Research Integration and Extramural Performance, OEP facilitates the management of the Program’s extramural grant and cooperative agreement portfolios. OEP coordinates with the WTC Health Program to solicit, review, and issue cooperative agreements related to Program activities such as the WTC Health Registry, research projects, and outreach and education activities.18
4.0 Eligibility and Enrollment
4.1 HHS, CDC, NIOSH
The Secretary of HHS has delegated the authority to oversee responder and survivor eligibility and enrollment activities to the CDC Director and NIOSH Director.19 Responsibilities assigned to the Administrator include the following required eligibility and enrollment functions:
- Establishing an enrollment process for individuals who meet eligibility requirements as WTC responders or screening-eligible survivors;20
- Screening applicants against the terrorist watch list prior to enrollment (see Section 4.2, Department of Homeland Security/Department of Justice below); 21 and
- Establishing a suitable appeal process for applicants denied enrollment.22
Chapter 2 of this Administrative Manual provides comprehensive information on the protocols and procedures of the Program’s eligibility and enrollment functions, including the appeals process. Chapter 11 details how the Program ensures that quality assurance standards are met through oversight procedures for these activities.
4.2 Department of Justice
The Zadroga Act disqualifies individuals on the terrorist watch list from eligibility for the WTC Health Program.23 The Federal Bureau of Investigation, within the Department of Justice (DOJ), administers the Terrorist Screening Center and maintains the terrorist watch list.
The Program consults with DOJ to ensure compliance with the eligibility requirements of the Zadroga Act.
5.0 Payment
5.1 Centers for Medicare and Medicaid Services
The Zadroga Act prohibits NIOSH from directly making payments to providers for WTC Health Program healthcare benefits.24 The Secretary of HHS delegated authority for disbursing WTC Health Program payments to the Administrator, Centers for Medicare & Medicaid Services (CMS).25 An interagency agreement between the WTC Health Program and CMS was established for this activity. For details on the CMS payment function, see Chapter 5, Claims Processing and Billing.
5.2 Department of Labor
Reimbursements—As required by the Zadroga Act, the WTC Health Program reimburses providers for healthcare costs based on the payment rates that would apply to such treatment and services under the Federal Employees’ Compensation Act (FECA).26 FECA is administered by the Office of Workers’ Compensation Programs within the Department of Labor (DOL).
- When there is no established FECA rate for a treatment, reimbursement is based on Medicare’s fee-for-service rate, as determined appropriate by the WTC Health Program Administrator.27
- If neither a FECA rate nor a Medicare fee-for-service rate has been established for a specific treatment, reimbursement is provided at an appropriate rate as determined by the WTC Health Program Administrator.28
Claims Processing—Based on consultation with DOL, the WTC Health Program established a system to process claims for reimbursement or payment and ensure they are paid in accordance with the Zadroga Act requirements.29 The WTC Health Program conducts periodic retrospective reviews and analyses of claims to assess its performance and performs audits to ensure compliance with the Zadroga Act. More detailed information on claims processing is in Chapter 5, Claims Processing and Billing.
6.0 Other 9/11- Related Programs
6.1 DOJ, September 11th Victim Compensation Fund
Title II of the Zadroga Act30 reactivated the September 11th Victim Compensation Fund of 2001 (VCF) that previously operated from 2001–2004. The VCF was established within DOJ to provide compensation for any individual (or a personal representative of a deceased individual) who suffered physical harm or was killed as a result of the terrorist-related aircraft crashes of September 11, 2001, or the debris removal efforts that took place in the immediate aftermath of those crashes. The VCF is directed by a Special Master who is appointed by the Attorney General. The VCF was reauthorized in 201531 and again in 2019,32 extending the VCF to 2090.
The VCF only provides compensation for losses due to personal physical injury or death, not mental health conditions. An individual who chooses compensation from the VCF waives their rights to pursue litigation to seek damages for the physical injury or death resulting from the September 11, 2001, terrorist attacks.
The WTC Health Program works collaboratively with the VCF. After the Program receives authorization and consent from the VCF claimant, it performs the following activities:
- For those VCF claimants who participate in both the WTC Health Program and the VCF, the Program transmits information including the WTC Health Program’s decisions regarding the individual’s certification and authorization for treatment, to the VCF to facilitate its evaluation of the individual’s VCF claims; and
- For those VCF claimants who do not receive care within the WTC Health Program, the WTC Health Program reviews the VCF claimants’ exposure and health information to assist the VCF with making compensation determinations in verifying whether claimants’ health conditions are related to their 9/11 exposures.
More information about the VCF can be found online at the: September 11th Victim Compensation Fund website .
Chapter 11—Financial Management Quality Assurance Standards
1. Introduction
The financial management quality assurance standards plan is designed to create the framework for achieving and maintaining financial management control and performance standards in the World Trade Center (WTC) Health Program. A well-executed quality assurance standards program creates awareness of performance standards and emphasizes policies and procedures, controls, performance management, performance measurement, efficiency, and guidance measures to prevent waste, fraud, and abuse. In addition, good quality assurance standards provide reasonable assurance that a program’s goals and objectives will be achieved.
2. Purpose
The purpose of this guidance is to create a framework for WTC Health Program financial controls, performance management, and performance measurement. This framework includes five focus areas relevant to financial controls, performance management, and performance measurement. The five focus areas are as follows:
Fund Control Management
Scope: Provide reasonable assurance that funding requirements adhere to Appropriations Law, U.S. Department of Health and Human Services (HHS) guidelines, James Zadroga 9/11 Health and Compensation Act of 2010 (Zadroga Act) and James Zadroga 9/11 Health and Compensation Reauthorization Act (Reauthorization) requirements and intent, and prevent fraud, waste, and abuse.
Measure: 100% compliance with Appropriations Law, HHS guidelines, and Zadroga Act and Reauthorization requirements.
Spend Plan Development and Management
Scope: Coordinate the planning and development of Spend Plans with appropriate staff. Review prior fiscal year(s) actual results; assess impact of known program and budget issues/decisions; and set priorities based on Program’s goals and mission.
Measure: Spend Plan developed and submitted to Office and Management and Budget (OMB) for approval 30 days prior to new fiscal year.
Budget Execution and Performance
Scope: Track, monitor, and report on use of Spend Plan funds; and track, monitor, and report on Program performance (i.e., Clinical Center of Excellence (CCE) and Nationwide Provider Network (NPN) claims submission and contract invoice submissions).
Measure: Review, approve, and process CCE and NPN invoices within 5 business days of receipt; and 2.) Review and monitor expenditure trends and produce monthly reports.
Analysis and Budget Forecasting
Scope: Conduct regular burn rate reviews of expenditures to determine if current budgets are adequate for balance of performance period.
Measure: Establish notification triggers at 75% and 90% expenditure levels and assess the details at each level to determine if Program action(s) is required.
Quality Assurance
Scope: Quality assurance encompasses all of the above activities and enables the Program to achieve and maintain high performance levels. Our goals are to develop Standard Operating Procedures (SOPs) for each step of the invoice reimbursement process and closely monitor other performance measures to ensure Program is performing according to statutory requirements.
Measure: No deviation from Program’s goals without Core Management Team (CMT) approval.
3. Policy Guidance
The WTC Health Program financial controls and policy and procedures guidance was developed to assist Program and financial management in accomplishing fiscal year fund control objectives. This guidance provides fund control procedures and contract clauses for applicable activities for each fiscal year.
The WTC Health Program works with its contractors, the CCEs and the NPN, to provide quality care to WTC Health Program members. As the Federal entity, the WTC Health Program’s governing role is to ensure that the resources dedicated are properly managed and performance is measured against the Program’s goals and mission to improve financial efficiency.
Procedural Guidance
-
Statutory Authority
Title I of the Zadroga Act amended the Public Health Service Act to add Title XXXIII and established the WTC Health Program within the HHS. In December 2015, Title XXXIII of the Public Health Act was amended by the Reauthorization. The Reauthorization authorized the WTC Health Program through FY 2090.
-
Fiscal Year Spend Plan/Apportionment
Each Fiscal Year’s Spend plan requires the approval of the OMB before execution.
Responsibility: Centers for Disease Control and Prevention (CDC)/National Institute for Occupational Safety and Health (NIOSH)/WTC Health Program
-
Awards
Once the Spend Plan is approved by OMB, the Grants Management Officer (GMO) and Contracting Officer (CO) can begin the process of issuing awards.
Responsibility: OFR/WTC Health Program
-
Personnel
Personnel projections are based on program priorities and are also subject to the availability of funds.
Responsibility: NIOSH/WTC Health Program
-
Governance
NIOSH is the responsible Federal entity and must exercise sound stewardship of appropriated funds.
Responsibility: NIOSH/WTC Health Program/OFR
-
Performance
The WTC Health Program’s overall performance is measured by how effectively and efficiently the Zadroga Act’s and Reauthorization’s requirements were executed.
Responsibility: NIOSH/WTC Health Program
-
Reports
The Zadroga Act requires the WTC Health Program to submit annual reports to Congress. OMB requires monthly report submissions.
Responsibility: NIOSH/WTC Health Program
-
Close out
All awards must be closed out at the end of their performance period.
Responsibility: NIOSH/WTC Health Program
Chapter 12—Pharmacy Benefits
TABLE OF CONTENTS
Last Revised – January 2026
1.0 Purpose and Scope
This chapter describes the pharmacy benefits available through the World Trade Center (WTC) Health Program (the Program) under the James Zadroga 9/11 Health and Compensation Act of 2010 (the Zadroga Act)1 , as amended.
1.1 Statutory and Regulatory References
The following sections of the Zadroga Act apply to this chapter:
- Section 3312(b)(1)(A)(ii) directs that the WTC Health Program shall pay for medically necessary treatment (including pharmaceuticals) for WTC-related health conditions, assuming certain conditions are met;
- Section 3312(b)(3)(B) relates to medical necessity for healthcare services, including a process for determining medical necessity, the scope of treatment, and appeals of decisions regarding medical necessity;
- Section 3312(b)(4)(B) specifies that medically necessary outpatient prescription drugs are provided under arrangements made by the WTC Health Program directly through participating Clinical Centers of Excellence or through one or more outside vendors; and
- Section 3312(c)(1)(B) specifies that the Administrator of the WTC Health Program shall establish a program for paying for the medically necessary outpatient prescription pharmaceuticals prescribed for WTC-related health conditions;
Program regulations relating to pharmacy benefits are established in the following sections of 42 C.F.R. Part 88:
- Section 88.1, Definitions;
- Section 88.20 Authorization of treatment;
- Section 88.22 Reimbursement for medical treatment and services;.
- Section 88.23 Appeal of reimbursement denial; and
- Section 88.24 Coordination of benefits and recoupment.
1.2 Roles and Responsibilities
The parties involved in providing WTC Health Program pharmacy benefits and their responsibilities are detailed below:
- The WTC Health Program establishes pharmacy policies for the Program, manages the formulary and medication criteria, and processes prior authorization requests for non-formulary medications.
- The Clinical Centers of Excellence (CCEs) and Nationwide Provider Network (NPN) provide care coordination, certifications, customer service, and medical services for eligible WTC Health Program members.2 The CCEs and NPN submit prior authorizations (PAs) as required and manage the prescriber network for members.
- The Pharmacy Benefit Manager receives, adjudicates, and processes payments for pharmacy claims. The Pharmacy Benefit Manager (PBM) manages the pharmacy network, prior authorizations, point of sale (POS) rules and restrictions, customer service line, and mails Pharmacy ID cards to certified members. Express Scripts, Inc. is the current PBM for the WTC Health Program. For PBM customer service contact information, please visit: WTC Health Program's Pharmacy page.
- The Health Program Support (HPS)/Third-Party Administrator (TPA) maintains member eligibility for pharmacy benefits and the prescriber network. Karna, LLC is the current HPS/TPA for the WTC Health Program.
2.0 Pharmacy Services
2.1 Pharmacy Network
The WTC Health Program provides members with guidance on filling WTC-related prescriptions based on their enrollment designation as a responder or a survivor.
Responders may receive up to a 30-day supply of medication at any pharmacy within the PBM network. Responder members may receive up to a 90-day supply of medication only when the prescription is filled at Walgreens/Duane Reade.
Survivors may receive up to a 90-day supply of medication at any pharmacy in the PBM network. Coordination of Benefits (COB) is required for survivor members (see Section 7.2). This means that the pharmacy used by a survivor must be in both their primary health insurance plan’s pharmacy network and the WTC Health Program’s PBM’s network. Members should provide both their primary pharmacy insurance ID card and their WTC Health Program Pharmacy ID card with each fill to help expedite the prescription filling process.
All members may speak to their respective CCE/NPN or contact the PBM for help in determining their pharmacy benefits and finding an in-network pharmacy. Members may also visit WTC Health Program's Pharmacy page for additional information regarding the pharmacy network.
2.2 Home Delivery and Specialty Pharmacy Services
-
Home Delivery Services:
WTC Health Program members can access home delivery for maintenance medications, which are prescription drugs that are taken on a regular or an ongoing basis. This service allows members to receive up to a 90-day supply of medication delivered directly to their home or preferred location, eliminating the need for pharmacy visits.
- Responders: Must use Express Scripts Home Delivery Pharmacy. Contact information for the WTC Health Program dedicated Express Scripts phone line can be found on the back of the WTC Health Program Express Scripts Pharmacy ID card.
- Survivors: May use any in-network home delivery pharmacy. In-network mail order pharmacies available to survivors include Express Scripts, CVS/Caremark, and OptumRx. To meet COB requirements, the pharmacy must be in both the member’s primary health insurance plan’s pharmacy network and the PBM’s network.
-
Specialty Pharmacy Services:
Specialty medications are high-cost prescription medications used for complex, chronic conditions such as cancer. These medications often require special handling (e.g., refrigeration during shipping) and administration (e.g., infusions). Specialty medications can be delivered directly to the member’s home or to a chosen location through a specialty pharmacy. The Program limits specialty prescriptions to a 30-day supply per fill.
- Responders: Must use Accredo Specialty Pharmacy, an Express Scripts specialty pharmacy. Contact information for Accredo Specialty Pharmacy can be found on the back of the WTC Health Program Express Scripts Pharmacy ID Card.
- Survivors: May receive specialty medications at any in-network pharmacy. To meet COB requirements, the pharmacy must be in both their primary health insurance plan’s pharmacy network and the PBM's network.
-
Enrollment: To use home delivery or specialty pharmacy services, members should contact the pharmacy to enroll and have their prescriptions sent directly to the pharmacy.
- For additional information, please visit WTC Health Program's pharmacy page.
- Requesting Refills: Members should request refills from their home delivery or specialty pharmacy two weeks before running out of medication to ensure timely processing and shipping.
2.3 Prescriber Networks
The prescriber network is a subset of providers within the CCE/NPN provider networks who are eligible to write prescriptions for the Program.
- Clinical Centers of Excellence and Nationwide Provider Network: Each CCE maintains its own distinct prescriber network that is separate from other CCEs. The NPN also maintains a prescriber network that is distinct from the CCEs. Only providers enrolled as prescribers with the Program are eligible to write prescriptions for the Program.
-
Providers should only be enrolled as prescribers when:
- The provider is going to provide ongoing care to members for WTC-related health conditions or health conditions medically associated with a certified WTC-related health condition;
- The provider is not an emergency room or urgent care physician, surgeon, or other type of provider who will not be involved with the member’s care long term; and
- The provider has been informed of the WTC Health Program requirements and rules and agrees to provide care to the member under these provisions.
- Exclusions: All prescribers on the U.S. Department of Health and Human Services (HHS) Office of Inspector General (OIG) provider exclusion list are excluded from the WTC Health Program. Prescribers may be removed from the Program at the Program’s discretion if there is an indication of fraud, abuse, misconduct, or if the provider’s license(s) and Drug Enforcement Administration (DEA) numbers have been revoked or suspended.
3.0 Pharmacy Formularies
The WTC Health Program assigns members to the appropriate pharmacy formulary based on the member’s certified health conditions and membership type (e.g., responder, screening-eligible or certified-eligible survivor, or immediate family of deceased Fire Department of New York (FDNY) firefighters). This section summarizes the current pharmacy formularies and provides highlights regarding formulary eligibility criteria and content.
3.1 Diagnostic Formulary
- Eligibility Criteria: All members except FDNY family members are eligible for the Diagnostic Formulary if the CCE/NPN determines medications available on the formulary are necessary during the certification process.
- Formulary Content: : The Diagnostic Formulary is limited to those medications used for the purpose of diagnosing a WTC-related health condition or a health condition medically associated with a certified WTC-related health condition and/or managing immediate symptoms.
-
Drug Quantity Limitations:
- 30-day supply limit per fill; and
- Maximum of 90 days’ supply of medication total
-
Criteria for use of the Diagnostic Formulary:
To prescribe medication on the Diagnostic Formulary, the medication must be necessary for one of the following purposes:
- Diagnostic evaluation for a WTC-related health condition or health condition medically associated with a certified WTC-related health condition (see Chapter 4 of this Administrative Manual, Section 2.3: Diagnostics Benefit Plan, and Section 2.6: Cancer Diagnostics Benefit Plan);
- Preparation for an approved cancer screening benefit (e.g., colon or breast cancer); or
- Medically necessary care for a health condition for which the CCE/NPN properly submitted a certification request to the WTC Health Program with a request for Treatment Pending Certification (see Chapter 4, Section 3.5: Authorization of Treatment Pending Certification).
3.2 Standard Formulary
- Eligibility Criteria: Members with at least one certified condition are eligible for the Standard Formulary, except for FDNY family members.
- Formulary Content: The Standard Formulary includes medications for the treatment of all certifiable WTC-related health conditions, including cancer.
3.3 Fire Department of the City of New York (FDNY) Family Mental Health Formulary
- Eligibility Criteria: Surviving immediate family members of FDNY responders who were killed at the World Trade Center site on September 11, 2001, and who are enrolled in the Program with at least one mental health certification.
- Formulary Content: The FDNY Family Mental Health Formulary includes a subset of medications in the Standard Formulary for certified WTC-related mental health conditions.
3.4 Cancer Formulary
- Eligibility Criteria: Members who are certified for at least one WTC-related cancer, are in active cancer treatment, and meet Program criteria to be considered high acuity for case management. Since many medications for cancer treatment are available on the Standard Formulary, a WTC-certified cancer alone is not sufficient to assign the member to the Cancer Formulary. Criteria for assignment are available to CCE/NPN staff for review.
- Formulary Content: The Cancer Formulary includes all medications available on the Standard Formulary and additional medications commonly needed for the routine treatment of health conditions medically associated with a certified WTC-related cancer. The Cancer Formulary has fewer POS restrictions.
4.0 Formulary Management
Medications are selected for review on a quarterly basis by the WTC Health Program. Selected medications include new-to-market medications, medications with newly approved indications, and those already on the formulary. The WTC Health Program selects and reviews classes of drugs for the quarter using the process described in Section 4.1: Formulary Review Process. At the end of each quarter, the WTC Health Program presents the findings and formulary changes to the CCEs/NPN at the Pharmacy and Therapeutics (P&T) Forum.
4.1 Formulary Review Process
-
Drug Selection: The WTC Health Program reviews drugs by therapeutic class. A therapeutic class is a set of medications that have similar chemical structures, the same mechanism of action, a related mode of action, and/or are used to treat the same disease. Factors that may determine which therapeutic classes are selected for review may include the following:
- Time elapsed since previous therapeutic class review;
- Prior authorization request trends;
- CCE/NPN requests;
- Drugs newly approved by the FDA or with newly approved indications;
- Pharmacy claims data; and/or
- PBM Quality Assurance and/or Fraud, Waste, and Abuse report recommendations.
-
Purpose of Therapeutic Class Review: Medications within the therapeutic class are reviewed to determine if:
- Drugs should be added or removed from any of the formularies described in Section 3.0: Pharmacy Formularies based on clinical data and cost effectiveness;
- Criteria should be applied to or removed from a drug (e.g., PAs, quantity limits, etc.); and/or
- Step therapy should be implemented for a class of drugs (see Section 5.3: Step Therapy).
-
Therapeutic Class Review Process: In performing the detailed therapeutic class reviews, the PBM and WTC Health Program pharmacists will:
- Prepare information about drug safety, efficacy, costs, and alternatives;
- Search for government reviews (e.g., U.S. Food and Drug Administration (FDA), Department of Defense, or Veterans Health Administration) comparing the clinical effectiveness of the requested medication with others in its class, and in particular, medications included on the formulary;
- Search and compare other federal health programs’ coverage of the medications (e.g., Centers for Medicare and Medicaid Services, Tricare, etc.);
- Review available resources for information on comparative clinical effectiveness with alternative medications, including available government and other federal sources for analysis. In cases where reliable comparative analysis already exists, a therapeutic drug class review is only performed as new information is published.
- Prepare a summary of the available research comparing the safety and efficacy of the medication to others in its class on the formulary; and/or
- Prepare an estimate of projected cost impact based on the number of members with the certified health condition and prescription trends (e.g., costs per year based on projected switch rates and drug consumption).
-
Expert Input:
- The WTC Health Program consults with and considers the professional opinions of subject matter experts and CCE/NPN clinicians, as necessary; and
- The PBM Clinical Advisory Team acts as a resource for the WTC Health Program pharmacists and clinicians.
4.2 Pharmacy and Therapeutics Forum
The WTC Health Program hosts the P&T Forum that meets quarterly to present clinical information researched during the formulary review process and any changes to pharmacy benefits. This may include formulary changes, POS rules and restriction changes, and policy and/or procedure changes. CCE/NPN clinicians are invited to attend the P&T Forum.
4.3 Formulary Changes
The WTC Health Program makes all decisions related to formulary additions, deletions, or restrictions. The Program will follow the timeline below. In the event of an exception, the CCEs/NPN will be notified accordingly.
- Formulary Change Schedule: All formulary changes will take effect on a quarterly basis, 30 days after the P&T Forum, unless otherwise stated.
- Delayed Implementation for Certain Members: When a POS restriction is added to a drug, members currently taking that drug are permitted to refill the prescription during the initial three-month period after the change is enacted in the system. This allows the CCE/NPN time to review their members’ prescriptions and notify impacted members.
- Distribution of Formulary Updates: The formulary is updated quarterly and is made available to the CCEs/NPN.
5.0 Drug Coverage
Full details can be found in the document Policy and Procedures for Coverage of Drugs [PDF, 9 pages, 320 KB]
5.1 Off-Label Drug Use
All prescription drugs sold in the United States must be approved by the FDA. This approval is based on evidence showing that the drug is safe and effective, as defined by FDA regulations. When a healthcare provider prescribes a drug for a purpose not listed on its FDA-approved label, this is known as an “off-label drug use” (OLDU) or an “unapproved use.”
The WTC Health Program may cover OLDU if it is medically necessary for a member’s certified WTC-related health condition or a health condition medically associated with a certified WTC-related health condition, and if it meets specific off-label criteria. For more details, refer to the document titled Medical Coverage Determination for the Coverage of Off-Label Use of FDA-Approved Drugs [PDF, 4 pages, 230 KB] .
5.2 Generic First Program
The WTC Health Program requires the use of generic medications instead of brand-name medications whenever they are available and appropriate to reduce costs. Brand-name medications that have an FDA-approved generic equivalent are called “multisource brand medications.” Multisource brand medications should only be dispensed when a member has a true contraindication to the generic drug—not simply due to member or prescriber preference.
Multisource brand medications are subject to PA rules and restrictions at the POS. To obtain approval of a multisource brand medication from the Program, the rationale must be documented in the medical record and the following criteria must be met:
- The medication is medically necessary to manage, ameliorate, or cure a certified WTC-related health condition, or health condition medically associated with a certified WTC-related health condition; and
- The member must have previously tried generic medications, including any available substitutable FDA-approved generics, based on formulary guidelines, without achieving sufficient clinical response or must have documented contraindications to the generic medications. Members must try generic medications for an adequate amount of time and at doses that would allow for a clinical response; this duration and dosage may vary depending on the type of drug and health condition being treated. This is indicated by the prescriber with a Dispense as Written (DAW) code = 1.
5.3 Step Therapy
The WTC Health Program implements step therapy for certain classes of medications. Often drugs used to treat the same condition, with similar efficacy, have significant variations in cost. The Program performs cost-benefit analysis, clinical research, and market research to determine if certain medications should be subject to step therapy rules. Step therapy requires the member to try less expensive drugs that are equally efficacious before using higher cost drugs.
- Step 1: Preferred medication: The Program has determined that this medication is the most cost-effective medication to treat a certain condition.
-
Step 2: Non-preferred medication: The Program has determined that there are less expensive medications available that are equally effective. Medications designated as Step 2, non-preferred medications will be subject to a PA. The following criteria must be met:
- The medication is medically necessary to manage, ameliorate, or cure a certified WTC-related health condition, or health condition medically associated with a certified WTC-related health condition; and
- The member must have tried Program-preferred medications based on criteria in the formulary, without a sufficient clinical response, or the member must have documented contraindications to the preferred medications. Preferred medications must be tried for a time period and dose that would be sufficient for a clinical response. The time period and dose may vary depending on the type of drug and condition treated.
The following are examples of some of the types of drugs subject to step therapy guidelines:
- Multisource Drugs (such as non-preferred albuterol inhalers, proton pump inhibitors, antidepressants, and antipsychotics)
- Triple-Therapy Inhalers (such as Trelegy and Breztri)
- Biologics (such as Dupixent, Xolair, Fasenra, and Nucala)
5.4 Compounded Drugs
Compounded prescription drugs are a subset of prescription drugs used to meet a member’s unique health needs that cannot be met by an FDA-approved medication. For example, compounded drugs may be prescribed if a member has an allergy and needs a medication to be made without a certain dye, or if a member cannot swallow a pill and needs a medicine in a liquid form that is not otherwise available. In addition to “active ingredients” (i.e., any ingredient in a medication that has a pharmacologic effect), most compounded medications also contain “inactive ingredients,” which are ingredients that have no pharmacological effect.
-
Prescribing Requirements:
Compounded medications may only be prescribed and approved for use in the Program when:
- There are no FDA-approved, commercially available products that could be used in place of the compounded medication; or
- The member has contraindications to FDA-approved, commercially available products, or has had an inadequate clinical response to such products.
- Coverage Guidelines: : The WTC Health Program covers compounded medications when the active ingredient drug is available on the formulary. Only FDA-approved ingredients may be used in a compounded medication. Bulk powders that are not FDA approved (i.e., active pharmaceutical ingredients for compounding) are not covered by the WTC Health Program.4 Compound medications may be subject to PA requirements.
- Pharmacy Reimbursement: Pharmacies are reimbursed for compounded medications based on their contracted rate of reimbursement with the WTC Health Program PBM for each ingredient billed in the claim. The WTC Health Program does not manage contracts with individual pharmacies and does not manage reimbursement rates. If a member has difficulty finding a compounding pharmacy to fill their prescription, they should contact their CCE/NPN or call the PBM Customer Service phone number printed on the back of their WTC Health Program Pharmacy ID card.
5.5 Over-the-Counter Drugs and Products
The FDA approves some drugs to be available over the counter (OTC) (i.e., non-prescription drug). An OTC drug is considered safe and effective for use by the general public without a physician’s prescription. An OTC healthcare product is a non-drug, non-durable medical equipment item that is used to aid in the diagnosis or treatment of a health condition which can be purchased without a prescription from a physician (e.g., blood pressure self-testing equipment such as monitors and cuffs). Questions regarding the coverage of an OTC product can be directed to the member’s CCE/NPN.
- Coverage Guidelines for OTC Drugs and Healthcare Products: The WTC Health Program provides limited coverage of certain OTC drugs and healthcare products to treat certified WTC-related health conditions, or health conditions medically associated with certified WTC-related health conditions, for medically accepted indications. OTC drugs must be prescribed by a WTC Health Program prescriber, related to the member’s certified WTC-related health condition, and dispensed in conjunction with the quantity and dosing limitations specified in the formulary, along with any requirements for PA.
-
Coverage Categories of OTC Drugs:
Coverage of each category of OTC drug is limited to a specific certified WTC-related health condition; only the following categories of OTC drugs are available for coverage:
- Select proton pump inhibitors;
- Select nasal steroids;
- Select antihistamines;
- Select saline nasal solutions;
- Select nicotine replacement therapies; and
- Select naloxone therapies.
-
Coverage Categories of OTC Healthcare Products:
Only the following categories of OTC healthcare products are eligible for coverage via the non-formulary PA process (see Section 6.6):
- Select asthma-related healthcare products, such as nebulizers, spacers, and peak flow meters;
- Select diabetes-related healthcare products, such as blood glucose monitors, glucose test strips, lancets, pen needles, and syringes;
- Select adult incontinence products; and
- Select enteral nutrition products.
6.0 Point of Sale Adjudication Rules and Restrictions
- Pharmacy Claims Submission: Prescription drugs are adjudicated at the POS through submission of claims at the pharmacy. Members provide their WTC Health Program coverage information to the pharmacy, which confirms enrollment through the PBM.
-
Point of Sale Rules and Restrictions:
These refer to system rules that must be met prior to the pharmacy claim being adjudicated. If the prescription does not meet the Program’s rules, the prescription claim will be rejected at the POS. POS rules and restrictions include the following (described in more detail below):
- Prescriber Not Covered
- Drug Utilization Review
- Refill Too Soon
- Quantity and Days’ Supply Limits
- Prior Authorizations
- Drug Not Covered
- Bill Primary Insurance (survivor coverage only)
6.1 Prescriber Not Covered
If a pharmacy submits a prescription claim from a provider not enrolled in the WTC Health Program prescriber network, the claim will be rejected at the POS with a message stating, “Prescriber is Not Covered.” If this occurs, the CCE/NPN may either uphold the rejection (resulting in the prescription remaining blocked), or override the rejection for up to one year when appropriate to treat the member’s certified WTC-related health condition or health condition medically associated with a certified WTC-related health condition. When overriding the rejection, the override will only apply to that provider that is not enrolled in the CCE/NPN, for that specific drug, and that specific member. The CCE/NPN would have to approve any additional prescriptions for the member from the provider or any additional prescriptions for other members for whom the unenrolled provider seeks to prescribe.
The CCE/NPN may override rejections when:
- The CCE/NPN has decided to enroll the provider in their prescriber network to allow the member to receive their WTC Health Program-related medications until the PBM system is updated;
- The CCE/NPN has decided not to enroll the provider in their prescriber network because the provider will not be treating the member’s condition long-term (e.g., emergency room physician), but has confirmed that the medication is for the member’s certified WTC-related health condition or health condition medically associated with a certified WTC-related health condition. In this case, the CCE/NPN should approve the provider for the short-term time period only; or
- The CCE/NPN has decided not to enroll the provider in their prescriber network because the provider also manages the member’s non-WTC-related health conditions. CCE/NPN overrides can allow payment for specific medications from a provider without adding the provider to their network for up to one year.
6.2 Drug Utilization Review
The PBM system performs a drug utilization review (DUR) on each claim by screening the drug against previously filled medications and other clinically relevant information (e.g., age, sex). The purpose of DUR is to improve patient safety and prevent waste. DUR rules are used by all federal pharmacy programs and managed by the dispensing pharmacy. If the prescription being filled is flagged by any of these screening criteria, then the claim will be rejected at the POS. The pharmacy may override DUR rules based on their professional judgment. DUR rules enforced by the PBM system include the following:
- Allergy Screening
- Drug-Drug Interaction Screening
- Drug-Diagnosis Caution Screening
- Drug-Inferred Health State Screening
- Dosing/Duration Screening
- Drug-Age Caution Screening
- Drug-Sex Caution Screening
- Duplicate Prescription Screening
- Duplicate Therapy Screening
6.3 Refill Too Soon
Refill too soon (RTS) POS rejections mitigate waste by preventing a member from receiving more medication than is medically necessary. Seventy-five percent of the previous refill must be exhausted based on days’ supply prior to the adjudication of another fill (e.g., ≥ 23 days of a 30-day supply, ≥68 days of a 90-day supply). If the refill is submitted before reaching the 75 percent threshold, the prescription will be rejected at the POS.5
The pharmacist may call the PBM Pharmacy Help Desk to request assistance with an override for a non-controlled substance in the following circumstances:
- Lost or Stolen Medication: If a patient reports that a medication was lost or stolen, the Program allows one lost or stolen medication override per year, per medication. The member should file a police report if they suspect a medication was stolen.
- Vacation Supply: If the member is going on vacation and will be unable to fill the prescription while they are away, the Program allows one vacation medication override per year, per prescription, to ensure the member does not run out of medication while on vacation. As necessary, the Program may allow both the lost or stolen medication and vacation supply to be processed within the same year.
Controlled substances are excluded from overrides for early refills using the process above. If needed, the member should speak to their CCE/NPN for assistance with an override request. The member must provide documentation that supports the planned vacation or that the medication was lost/stolen (e.g., filed police report) to the CCE/NPN. The CCE/NPN will forward the controlled substance override request along with the associated documentation to the WTC Health Program for a decision.
6.4 Quantity and Day Supply Limits
Select medications on the formulary have strict quantity and day supply limits. These limits are a type of utilization management criteria that help ensure patient safety and prevent fraud, waste, and abuse in the Program. Quantity and day supply limits are developed by the Program using FDA-approved package inserts and clinical guidelines and benchmarked against industry standards and other federal payers.
- Quantity Limits: Quantity limits restrict the total number of doses a member can receive in a specified amount of time, for example three inhalers over 90 days or six tablets per month. These limits help contain cost and prevent harmful dosing. Requests for exceptions to quantity limits may be submitted through the PA process defined in Section 6.5 below.
- Day Supply Limits: Day supply limits restrict the number of days for which a prescription can be written. For example, a medication may have a strict limit of a 30-day supply. If this medication can be taken once a day or twice a day, the member can receive 30 or 60 tablets as written by the prescriber per month. The pharmacy would not be able to fill a prescription for a 90-day supply. Day supply limits can be implemented through pharmacy network rules (see Section 2.1) or through clinical rules for a specific drug.
6.5 Prior Authorization—Formulary Medications
Some medications on the formulary may require prior authorization (PA) before the medications will be covered by the Program. A PA is used to confirm that a medication is medically necessary, appropriate for a member’s use, and meets Program criteria for coverage. A provider must submit clinical documentation that demonstrates medical necessity for a PA to be considered for review. Members may be notified of a PA requirement by the pharmacy and by the PBM. The prescribing provider may be notified of the PA requirement by a call or fax from the pharmacy, through contact from the CCE/NPN, outreach from the member, or notification from the PBM.
The provider must submit the PA request as outlined below. As with all prescriptions, members should contact the pharmacy to make sure a prescription has been processed before picking up the medication.
The prescribing provider may complete a PA request through one of the following methods:
- Electronic PA (ePA): This is the preferred mechanism for PA request submission. Many health systems have ePA capabilities built into their electronic health record (EHR) systems. This allows the provider to answer all questions electronically and send the completed PA directly to the PBM.
- Telephone: The provider’s office can call the PBM to submit a PA request.
- Fax: In many cases, pharmacies send a PA request fax form directly to the prescribing provider. The Program has PA request forms available to prescribers and clinic staff in an online database. Providers will complete and fax the PA request forms to the appropriate PBM department for review.
Once a PA request is reviewed and a coverage determination is made based on the Program’s criteria, the member and provider are informed of the outcome by letter.
Medications on the formulary that require a PA will go through the following steps. For non-formulary medications, see Section 6.6.
- Primary Review: Providers complete and submit the appropriate PA request form to the PBM for primary review. The PBM will evaluate the submitted information and decide whether to cover the medication according to the Program’s formulary and utilization management criteria. Both the member and the provider will be notified of the PBM’s PA decision by letter.
- Secondary Review: If a PA request is denied, providers are notified and can request to have the PBM reconsider coverage for the medication. The initial denial letter includes a summary of reasons for denial along with contact information for further inquiries. To initiate a secondary review, providers must provide additional justification for coverage of the medication. Providers can submit their secondary review request with the necessary information for PBM evaluation. The PBM will then reassess this information to decide if coverage can be granted based on the Program’s formulary and utilization management criteria. A decision letter indicating either denial or approval is sent to both the member and provider.
- Third and Final Review: If a medication remains denied after a secondary review by the PBM, providers may submit a justification for coverage to the Program for a final review. These requests are sent directly to the Program, which will issue its final decision regarding approval or denial of coverage. Members and providers are notified of the Program’s final decision by a letter from the PBM.
If a member believes that their medication treatment was incorrectly denied, they can file a formal appeal using the Denial of Authorization of Treatment appeals process that is detailed on the Appeals Page of the Program’s website.
6.6 Prior Authorization—Non-formulary
If a pharmacy tries to process a prescription for a non-formulary item, it will receive a rejection message that says “Drug/Product Not Covered.” However, the member may still be able to obtain the medication or product; select products will include additional messaging that states a PA is available. In this case, the CCE/NPN prescriber must submit a PA request to the Program to seek approval for use of the non-formulary item.
To initiate this process, the prescribing provider should contact the PBM for instructions on how to complete the PA request for the non-formulary product. The PA will then be submitted to the Program for review and final decision regarding coverage approval or denial. Note that the PBM does not review, approve, or deny PAs for non-formulary products. Both the member and the provider are notified of the Program’s final decision through a letter from the PBM.
If a member believes their medication treatment was denied in error, they can file a formal appeal using the Denial of Authorization of Treatment appeals process available on the Appeals Page of the Program’s website.
6.7 Billing Primary Insurance (Survivors Only)
The Zadroga Act requires Coordination of Benefits (COB) for treatment for survivor members (see Section 7.2), including pharmacy claims. COB means that the pharmacy must bill all primary health insurance plans, including federal and private plans, before billing the WTC Health Program. The WTC Health Program is the payer of last resort for all survivor members and pays any remaining out-of-pocket costs for prescriptions. If a pharmacy tries to bill the WTC Health Program as the primary payer, the pharmacy will receive a rejection that states “Bill primary payer prior to billing WTC.” Members must provide the pharmacy with their primary insurance information. More information on payer order can be found in the Payer Order Guidance Policy and Procedure [PDF, 7 pages, 215 KB] .
7.0 Submission of Pharmacy Claims
Pharmacies submit claims to the PBM for prescription medications. Claims must be submitted electronically and in compliance with the National Council of Prescription Drug Programs (NCPDP) standards. Eligibility for claim payment is determined by carrier code and member account. If the claim does not align with the carrier code and member account, the claim will be rejected with the message “Member Not Eligible.” All claims submitted by the pharmacy are subject to POS rules and restrictions (see Section 6.0: Point of Sale Adjudication Rules and Restrictions).
Pharmacists have authority to fill and dispense prescriptions and submit claims based on their professional judgment and discretion. If a member has issues filling a prescription, they should contact their CCE/NPN provider’s office or call the Express Scripts Customer Service phone number printed on the back of their WTC Health Program Pharmacy ID card.
Pharmacy claims must be submitted within 365 days (one year) of the fill date; all claims older than 365 days will be rejected.
Pharmacies are reimbursed for claims billed to the WTC Health Program based on their contracted rate of reimbursement with the WTC Health Program PBM. The WTC Health Program does not directly manage contracts with individual pharmacies or reimbursement rates.
7.1 Member Reimbursement
Medications covered by the Program are available at zero out-of-pocket cost for the member. If members are told there is an out-of-pocket charge for a WTC-related medication, members are advised to call the Express Scripts Customer Service phone number printed on the back of their WTC Health Program Pharmacy ID card or to contact their CCE/NPN before purchasing the prescription. The pharmacy should contact the PBM’s Pharmacy Help Desk for assistance with billing if needed.
Members are advised to resolve billing issues before paying for any WTC-related medication to avoid paying out of pocket. While the PBM may provide the opportunity for reimbursement in certain circumstances, reimbursement is not guaranteed. Questions related to reimbursement for a medication can be directed to the Express Scripts Customer Service Line. The Program does not cover additional services related to prescriptions (e.g., delivery fees).
7.2 Survivors Only: Coordination of Benefits for Pharmacy Claims
In accordance with statutory requirements, the WTC Health Program distinguishes between how responder and survivor healthcare claims are billed. The WTC Health Program is the payer of last resort for survivors. This means that a member’s primary insurance (e.g., private group health insurance, Medicare, Medicaid) must be billed first for treatment, including medications; only after all other available insurance has been billed can the remaining balance on the claim be billed to the Program.
To perform coordination of benefits for a pharmacy claim for a survivor, the pharmacy must have both the survivor’s primary insurance billing information and their WTC Health Program billing information on file. The pharmacy then submits the claim for automatic processing with primary and secondary payers. The primary payer will be adjudicated first and any POS rules and restrictions that apply to the plan of the member’s primary payer will be activated.
-
Primary Insurance Restrictions:
The member’s primary insurance may have restrictions on medication claims including, but not limited to:
- Refill Too Soon
- Drug Utilization Review
- Prior Authorization
- Drug Not Covered
- Physician Not Covered
- Quantity and Days’ Supply Limits
- Pharmacy Not in Network
- Secondary/Last Payer Submission: All primary insurance rules and restrictions must be resolved before submitting the claim to the secondary payer and/or payer of last resort (i.e., the WTC Health Program). Once the WTC Health Program is submitted as the last payer, the claim will then be subject to all WTC Health Program adjudication rules and restrictions at the POS including, but not limited to, the rejections listed in paragraph A above.
- Exceptions to COB: Claims for compounded medications are not submitted for COB. The Program does not require compounded drugs to be submitted to primary insurance and will act as primary payer on all claims for compounded drugs for survivor members. Refer to Section 5.4 for more details about compounded medication coverage.
- Discrepancies between Primary Coverage and WTC Health Program Coverage: In some cases, the WTC Health Program formulary requirements may conflict with those of the survivor member’s primary insurance. The Program has developed a system with the PBM to ensure that WTC-related medications may be covered through the Program, when appropriate, if a primary insurance plan will not pay for the medication. For the Program to cover the medication, all measures to have the primary insurance pay for the medication, such as a PA, must be completed first.
- Members with Multiple Pharmacy Plans: : Although rare, survivor members may have more than one primary pharmacy benefit plan. In these cases, the member's primary plans will need to coordinate billing of the prescription first, and only the remaining balance on the claim is billed to the Program as the payer of last resort. This results in no out-of-pocket cost for the member.
More information regarding payer order and COB can be found in the document Policy and Procedures for World Trade Center (WTC) Health Program Identification and Payer Order Guidance for Medicare and Medicaid [PDF, 7 pages; 215 KB]. [PDF, 7 pages, 215 KB]