Caring for Infants & Children
Notice: On October 20, 2017, CDC released updated interim clinical guidance for healthcare providers caring for infants born to people with possible Zika virus infection during pregnancy.
Changes in guidance are summarized below:
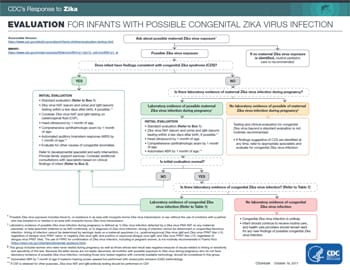
- To assist healthcare providers with evaluation, diagnosis, and clinical management decisions, infants have been categorized into three main groups: 1) infants with birth defects consistent with congenital Zika syndrome born to people with possible Zika virus exposure during pregnancy; 2) infants without birth defects consistent with congenital Zika syndrome, but who were born to people with laboratory evidence of possible Zika virus infection during pregnancy; and 3) infants without birth defects consistent with congenital Zika syndrome born to people with possible congenital Zika virus exposure during pregnancy but without laboratory evidence of Zika virus infection.
- The new guidance provides updated information on how infant laboratory testing results should be interpreted.
- Recommendations for vision and hearing screening have been updated.
- Some of the previously recommended screenings (e.g., thyroid screening, complete blood count [CBC], liver function tests [LFTs], hearing screening at 4-6 months) are no longer recommended because data are lacking to show that these screenings might be needed.
- For infants with birth defects consistent with congenital Zika syndrome, healthcare providers should monitor for an expanded listed of potential problems. In addition, initial and follow-up care of these infants are no longer dependent on the infant’s Zika virus testing results.
- For infants without birth defects consistent with congenital Zika syndrome born to people with laboratory evidence of possible Zika virus infection during pregnancy, an ophthalmologist should perform an eye examination.
- For infants without birth defects consistent with congenital Zika syndrome born to people with exposure to Zika virus but no laboratory evidence of Zika virus infection during pregnancy, further testing for Zika virus and clinical evaluation are not recommended.
Summary
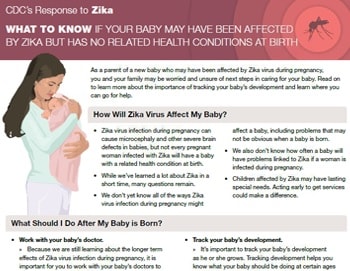
- All infants born to people with possible exposure to Zika virus during pregnancy should receive a standard evaluation at birth and at each well-child visit. A standard evaluation should include a comprehensive physical exam (including growth parameters), age-appropriate vision screening and developmental screening and monitoring, and a standard newborn hearing screening at birth, preferably using auditory brainstem response (ABR) methodology.
- Testing is recommended for infants with birth defects consistent with congenital Zika syndrome born to people with possible Zika virus exposure during pregnancy (regardless of the person’s Zika virus testing results) and for infants without birth defects consistent with congenital Zika syndrome who were born to people with laboratory evidence of possible Zika virus infection during pregnancy.
- For infants recommended to receive testing for congenital Zika virus infection, concurrent Zika virus RNA nucleic acid amplification testing (NAAT) of serum and urine and Zika virus IgM testing of serum should be performed within a few days after birth, if possible. However, testing specimens collected within the first few weeks to months after birth may still be useful in the evaluation for possible congenital Zika virus infection.
- Guidance for testing and clinical management of infants and children with postnatal Zika virus infection is in line with testing and clinical management recommendations for adults. Zika virus PCR and serologic testing is recommended during the first 2 weeks after symptom onset to diagnose postnatal Zika virus disease. Serologic testing is recommended 2-12 weeks after symptom onset.
Guidance
- Update: Interim Guidance for the Diagnosis, Evaluation, and Management of Infants with Possible Congenital Zika Virus Infection — United States, October 2017 (MMWR, Oct. 19, 2017)
- Interim Guidance for the Evaluation and Management of Infants with Possible Congenital Zika Virus Infection – United States, August 2016 (MMWR, August 19, 2016)
- Interim Guidelines for Healthcare Providers Caring for Infants and Children with Possible Zika Virus Infection – United States, February 2016 (MMWR, Feb. 19, 2016)
- Interim Guidelines for the Evaluation and Testing of Infants with Possible Congenital Zika Virus Infection – United States, 2016 (MMWR, Jan. 29, 2016)
Featured Tools
Page last reviewed: April 22, 2022