About Healthcare-Associated Mold Outbreaks
Frequently asked questions and answers about mold in healthcare facilities
Where does mold grow?
Mold lives both outdoors and indoors. It can grow in homes and other buildings, including healthcare facilities, and it grows best in places with lots of moisture.
How can mold affect health?
Mold can cause a variety of health problems, or none at all. The most severe health problems caused by mold include serious infections. For more information about how mold can affect health, visit CDC’s Mold site.
Talk to your healthcare provider if you have symptoms that you think are related to a serious mold infection.
How do people get mold infections?
Most people breathe in mold spores every day without getting sick. However, some people, especially those with weakened immune systems, can develop infections after breathing in mold or having other contact with mold. Usually, it is difficult to tell exactly where in the environment the infection came from. Sometimes, patients get exposed to mold inside a healthcare facility (for example, a hospital).
What can a healthcare facility do to prevent invasive mold infections?
Healthcare facilities take special precautions to prevent patients from getting sick from indoor mold.
These precautions include:
- Filtering the air.
- Giving some patients with weakened immune systems antifungal medicine to prevent mold infections.
- Placing some patients in rooms where the air flow reduces the chances of the patient getting an infection.
- Fixing water leaks and repairing damages as fast as possible.
- Reducing dust during construction.
- Tracking the number of patients with mold infections to monitor for an increase, which could signal a problem with indoor mold.
For public health and healthcare professionals: investigating outbreaks of mold infections
A higher number of patients with invasive mold infections than usual within a healthcare facility could indicate an outbreak. Most invasive mold infections are caused by Aspergillus and mucormycetes, but other molds can also cause outbreaks. Detecting outbreaks of invasive mold infections early is important to help patients get the right treatment and so healthcare personnel can take action to prevent others from getting sick.
What should I do if suspect an outbreak of mold infections?
One of the first steps of an investigation is to establish the existence of an outbreak. However, determining whether a cluster of mold infections (i.e., a suspected outbreak) represents a true outbreak can be difficult. Cases of mold infections are often diagnosed using multiple methods (e.g., culture, histopathology, serologic testing, PCR), making tracking these infections difficult. Also, case numbers are often small, making it difficult to tell if infection rates are truly above baseline. Finally, the incubation period for most mold infections is unclear, but when a patient’s mold infection begins more than 1–2 weeks after admission to a hospital or is a surgical site infection, healthcare acquisition should be suspected.
Any cluster of invasive mold infections that appears to be above the baseline rate or is otherwise concerning to healthcare staff, particularly those involving cases with onset >1 week after admission, should be investigated as a suspected outbreak. When healthcare personnel begin to investigate a mold infection cluster, they should also notify their local or state public health department. These notifications should occur at the earliest stages of a facility investigation, recognizing that most clusters will not be confirmed as outbreaks after further investigation.
How can I request CDC assistance with a mold infection outbreak?
CDC works closely with local and state health departments to help identify, investigate, and contain fungal outbreaks. Public health officials, healthcare facilities, and laboratories can request CDC assistance with fungal diagnostics and epidemiologic investigations by emailing FungalOutbreaks@cdc.gov.
Consultations with CDC on suspected outbreaks can be more effective if the healthcare facility or health department shares a brief summary beforehand that includes:
- Information about each patient who might have a mold infection (e.g., mold genus or species, underlying disease, estimated onset date, date of diagnosis, and method of diagnosis).
- Locations where patients with mold infection have been in the facility before their infections.
- The number of patients with invasive mold infections at the facility in recent years, grouped by month of diagnosis.
- A description of any investigation conducted to date.
- A description of any recent construction or demolition activity in or near the facility.
- What specimens are still available for further testing.
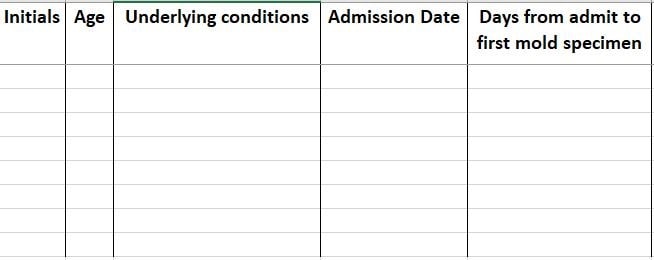
Sample line list for investigating healthcare-associated mold outbreaks [16 KB].
Healthcare officials should ask the laboratory to preserve any remaining specimens. Patients’ personally identifiable information (PII) should not be shared with CDC.
Healthcare officials can gather case information using the sample line list provided in the document below, A Guide to Investigating Suspected Outbreaks of Mucormycosis in Healthcare. This line list is a template used to collect some of the key pieces of information for investigating a mold infection outbreak.
- A Guide to Investigating Suspected Outbreaks of Mucormycosis in Healthcare. This document can also be helpful when investigating outbreaks of other types of mold infections, such as aspergillosis.
- A checklist for conducting environmental investigation and sampling within the context of an epidemiologic investigation [20 pages].
Previous outbreaks of healthcare-associated mold infections have been linked to contaminated healthcare linens (e.g., bed sheets, towels). Checklists are available for infection preventionists to assess laundry management practices at laundry facilities and health care facilities.
Should we conduct environmental sampling?
Environmental sampling can be difficult to interpret. Simply detecting a certain mold species or level of mold spores in a specific place or on an object does not necessarily mean that place or object should be implicated as a source of mold or mold infections. Similarly, failure to detect mold in a certain location does not rule out a source, since mold can be found intermittently and can occur across multiple sources throughout a healthcare facility.
In the context of an epidemiologic investigation, environmental sampling is most effective using a predefined sampling strategy. If you are planning to perform environmental sampling, consider involving an industrial hygienist with experience in healthcare settings who can help create a sampling strategy.
When should a healthcare facility notify patients about a suspected outbreak of healthcare-associated mold infections? Why is patient notification important?
We recommend notifying patients who may be at risk of mold infections, as well as those with mold infections, of a cluster or suspected outbreak as early as possible. Healthcare personnel may be reluctant to notify patients, especially when it is not clear if an outbreak truly exists or whether exposures occurred at the hospital. Healthcare personnel might be concerned about creating unnecessary patient anxiety, which must be balanced against potential benefits. However, in practice, research suggests that healthcare facilities increase patient trust through notifications, and trust can be severely degraded if an outbreak is later disclosed by other means, even if healthcare facilities took appropriate steps in remediating problems.
In general, it is best to notify patients at greatest risk of invasive mold infections (e.g., transplant recipients, patients with hematologic malignancies) as soon as possible once a cluster of invasive mold infections is identified. Notification should occur even before an investigation is complete or a common source is identified. Early patient notification about a suspected outbreak can help:
- Encourage patients to seek care early if they have concerning symptoms, potentially reducing delays in diagnosis and treatment.
- Build and maintain trust with patients and the public in their facilities and staff.
- Better educate patients on invasive mold infections and ways to avoid exposure to mold.
- Remind patients, visitors, and clinicians about the importance of proper infection control measures and how to reduce the risk of getting sick.
Patient notification can occur in a number of ways, including verbal communication by healthcare providers based on a healthcare facility–developed template. For more information and examples of ways to notify patients, visit CDC’s Patient Notification Toolkit.
- CDC: Mold
- A guide to investigating suspected outbreaks of mucormycosis in healthcare. J Fungi. 2019 Jul 24.
- Outbreaks and infection control breaches in health care settings: Considerations for patient notification. AJIC. 2020 Jun.
- CDC: Targeted environmental investigation checklist for outbreaks of invasive infections caused by environmental fungi (e.g., Aspergillus, Mucormycetes) [PDF – 20 pages]
- CDC: Introduction to the Patient Notification Toolkit
- CDC: Communicating during an outbreak or public health investigation
- CDC: Basic facts about mold and dampness
- CDC: Invasive mold infections in immunocompromised people
- CDC: Healthcare-associated infection (HAI) outbreak investigation toolkit
- American Industrial Hygiene Association (AIHA): FAQs About Spore Trap Air Sampling for Mold for Direct Examination [PDF – 8 pages]