Fungal Infections: Protect Your Health

These 10 questions will help you understand your risk of getting fungal infections and what you can do to protect yourself.
Fungi can live outdoors in soil and on plants, indoors on surfaces and in the air, and on people’s skin and inside the body. There are millions of fungal species, but only a few hundred of them can make people sick.
Fungal infections can range from mild fungal skin infections, like ringworm, to lung infections from breathing in fungal spores, like Valley fever. Severe and life-threatening fungal infections are less common and are often associated with medical procedures or healthcare facilities. For all fungal infections, finding the correct diagnosis can be difficult and cause delays in getting the right treatment.
The more you know about fungal infections and your chances of getting one, the better you can protect your health.
Find Out If You’re at Risk of Getting a Fungal Infection
- Where do you live and travel? Some disease-causing fungi are more common in certain places. For example, in the United States, the fungus that causes Valley fever is found mainly in the Southwest and parts of the Pacific Northwest. Histoplasmosis and blastomycosis occur most often in the central and eastern United States.
- What types of activities are you doing? Harmful fungi can be found in air, dust, and soil. You could inhale fungi during activities like digging, gardening, cleaning chicken coops, and visiting caves. Histoplasma grows especially well in soil that contains bird or bat droppings.
- Do you have a dog or cat? People can get ringworm from their pets. A fungus called Sporothrix brasiliensis is spreading in South America to people from cats. It is not spreading in the United States, but it is possible that the infection could be brought here someday. If you think your pet might be sick, talk to your veterinarian.
- Have you recently taken antibiotics? Antibiotics can make women more likely to get a vaginal yeast infection, also known as vulvovaginal candidiasis. Men also can get genital candidiasis. In hospitals and healthcare settings, patients who take broad-spectrum antibiotics (those that work against a wide range of bacteria) are at a higher risk for infections like C. auris and Candidemia.
- Are you taking any medicines or receiving treatments that weaken your immune system? Medicine like steroids, biologics (made from living things and their products), radiation therapy, and chemotherapy can weaken your immune system. This makes it harder for your body to fight against fungal infections. If you are taking one of these medicines, learn what you can do to help prevent fungal infections.
- Do you use communal showers or locker rooms or share linens or towels? Ringworm can live on skin, surfaces, and household items like clothing, towels, and bedding. To prevent ringworm, do not walk barefoot in communal showers or locker rooms; do not share clothing, towels, or sheets; and keep skin clean and dry.
- Are you living with HIV? People living with HIV (particularly those with CD4 counts less than 200) may be more likely to get fungal infections. Two well-known fungal infections associated with HIV in the United States are oral candidiasis (thrush) and Pneumocystis pneumonia. Worldwide, cryptococcal meningitis and histoplasmosis are major causes of illness in people living with HIV.
- Have you recently had a transplant? People who recently had an organ transplant or a stem cell transplant have weakened immune systems. That means they have a greater chance of developing a fungal infection. Doctors prescribe antifungal medicine for some transplant patients to prevent fungal infections.
- Are you staying in a healthcare facility (long-term care, hospital, or skilled nursing facility)? In the United States, one of the most common bloodstream infections acquired in the hospital is caused by a fungus called Candida. Candida normally lives in the gastrointestinal tract and on skin without causing any problems, but it can enter the bloodstream and cause infection. Invasive medical devices (for example, central lines, catheters, total parental nutrition) increase the risk of Candida. A type of Candida called Candida auris is often resistant to antifungal medicines and can spread between patients in healthcare settings.
- Do you have symptoms of pneumonia that are not getting better with antibiotics? Fungal infections, especially lung infections like Valley fever, histoplasmosis, and blastomycosis, can have similar symptoms to bacterial infections. However, antibiotics don’t work for fungal infections. Early testing for fungal infections reduces unnecessary antibiotic use and allows people to start treatment with antifungal medicine, if necessary.
Anyone can get a fungal infection. Many types of fungi do not normally cause infections in healthy people but can cause illness in people with weakened immune systems. Risks of serious fungal infections increase among patients in healthcare settings. To learn more about the signs, symptoms, and treatment of fungal infections and get prevention tips, visit CDC’s fungal diseases website and talk with your healthcare provider.
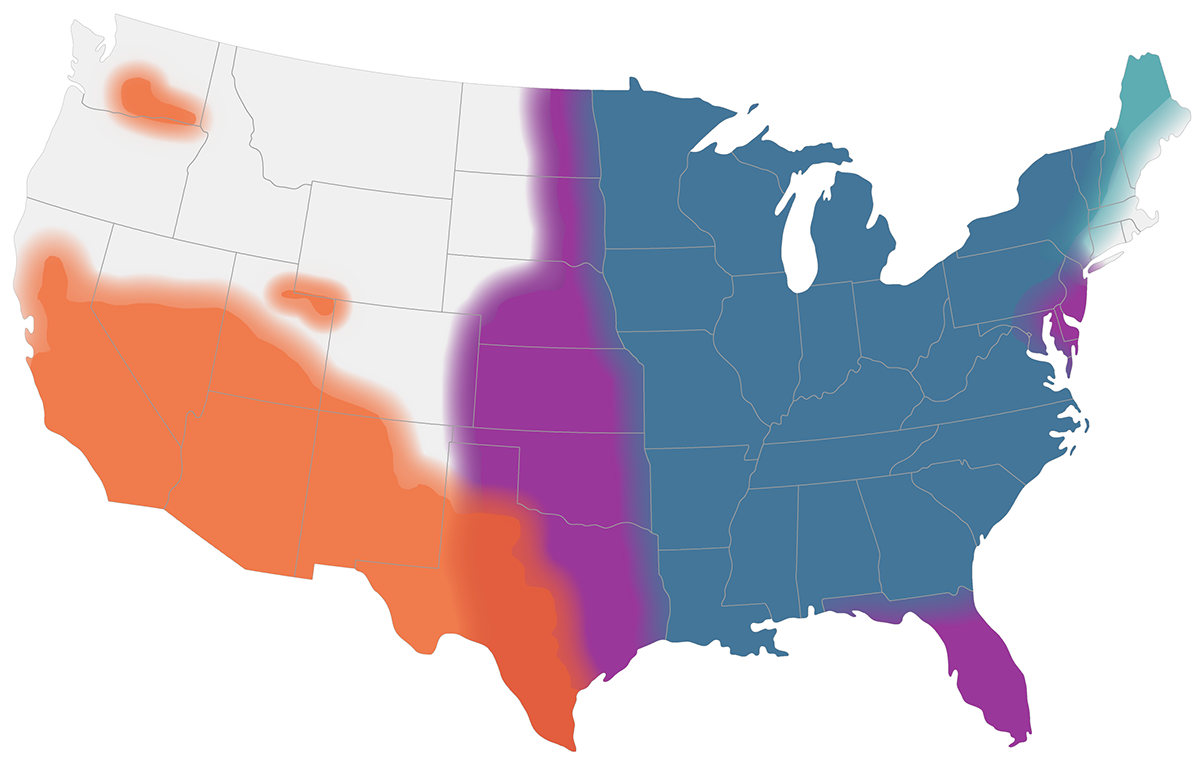
This map shows CDC’s current estimates of where the fungi that cause blastomycosis (blue), Valley fever (orange), and histoplasmosis (purple) live in the environment in the United States. These fungi are not distributed evenly in the shaded areas, might not be present everywhere in the shaded areas, and can also be outside the shaded areas.
Join CDC in sharing information to increase awareness in your community about fungal diseases during Fungal Disease Awareness Week, September 18–22, 2023.