Opioid Rapid Response Program (ORRP)
Mitigate Drug Overdose Risks Among Patients Experiencing Disrupted Access to Prescribers
The Opioid Rapid Response Program (ORRP) is an interagency, coordinated federal effort to help mitigate overdose risks among patients who lose access to a prescriber of opioids, medications for opioid use disorder, or other controlled substances, such as benzodiazepines. Disrupted access could be due to law enforcement actions or other events, such as the retirement, death, or voluntary closure by a clinician who prescribes controlled substances. ORRP helps address care continuity and risk reduction for patients by alerting state health agencies about law enforcement events that might disrupt patients’ access to care and supporting state and local capacity building to prepare for and respond to disruptions in care.
ORRP helps ensure all agencies act quickly so patients can get the care they need.
- ORRP is overseen by the Office of the Assistant Secretary for Health (OASH) and managed by the Centers for Disease Control and Prevention (CDC), in partnership with the Office of the Inspector General within the US Department of Health and Human Services (HHS OIG).
ORRP supports all 50 US states and the District of Columbia. The program leverages relationships across federal and state agencies to facilitate timely communication, care coordination, risk reduction, and other overdose prevention activities. ORRP coordinators within CDC’s Division of Overdose Prevention and HHS OIG receive notifications from federal law enforcement agents, and ORRP coordinators communicate potential patient risks to state health agencies. State health agencies may then take steps to assess risks; communicate with partners; and facilitate continuity of care, referrals, and overdose prevention.
ORRP’s role is to facilitate timely communication and coordination across state and federal health agencies and to ensure that available public health, healthcare, and treatment services supported by the federal government are known to and leveraged by state health officials working to mitigate risks among patients.
CDC does not participate in active law enforcement investigations taken by federal or state agencies, nor does CDC deploy health professionals to states in response to disruptions in patient care.
ORRP’s Strategic Components
All ORRP efforts align with one of four strategic components to help strengthen care continuity and overdose risk mitigation.
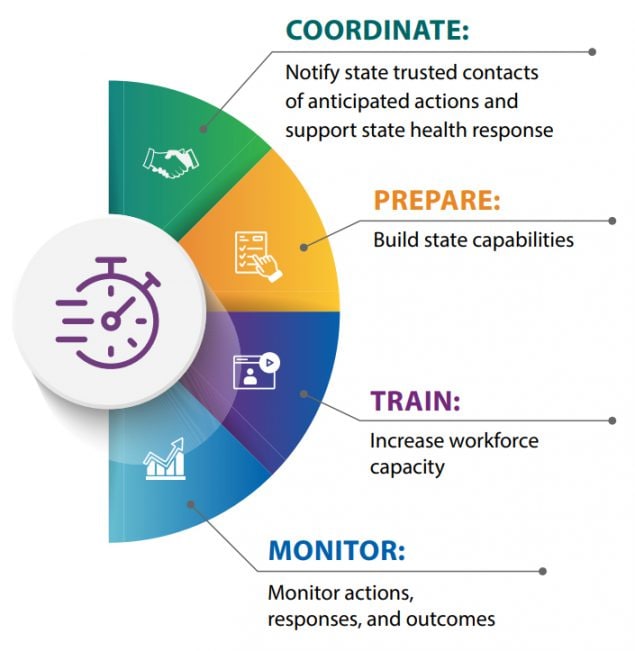
Establish and engage state public health and behavioral health agency officials as trusted contacts in every state and DC
- Engage with federal law enforcement agents before they take action that could result in a prescription supply disruption (e.g., search warrants, arrests, and surrenders or suspensions of DEA registrations or licenses)
- Assist states in assessing risks to patient populations and determining appropriate mitigation measures
- Follow up with state health and federal law enforcement after a law enforcement action and state response have occurred
- Provide technical support and training for state and local jurisdictions preparing for a disruption in prescription opioid or MAT/MOUD supply
- Develop communication materials and templates for state and local health officials to use during clinic closures and overdose spikes (e.g., health alerts, flyers with referral hotlines, information about risks associated with counterfeit pills, and how to access harm reduction resources)
- Conduct practice scenarios with states in partnership with the Association of State and Territorial Health Officials (ASTHO)
- Monitor states’ preparedness efforts
- Develop and disseminate ORRP training on opioids, treatment, and overdose prevention for clinicians and non-clinicians
- Train law enforcement officials on opioid use disorders, treatment, and overdose prevention strategies
- Support the training of healthcare professionals to support jurisdictions’ opioid rapid response efforts, including linkages to care, gap care, care coordination, motivational interviewing, and pain management
- Monitor law enforcement notifications, state notifications, and response capacity building efforts
State Capacity Building and Risk Mitigation Strategies
ORRP staff work with state health officials to identify and anticipate risks among patients affected by law enforcement actions. They provide technical assistance to states as they identify and implement various risk mitigation activities. CDC continues to partner with the Association of State and Territorial Health Officials (ASTHO) to help build states’ capacity to respond to ORRP notifications. ASTHO facilitates scenario-based practice exercises with states, organizes and convenes learning community webinars, and develops resources to support states’ preparedness. CDC and ASTHO worked together to incorporate lessons learned from actual ORRP actions and state responses into the practice exercises and to ensure that appropriate state agencies, such as Medicaid and prescription drug monitoring program (PDMP) administrators, be included in the exercises. Preparedness exercises help states develop and test their response plans. They can serve as a valuable opportunity to bring together various state and local agencies that may be involved in a disruption and begin identifying assets that can be leveraged to mitigate risks to patients.
Online Training Available: The Opioid Rapid Response Program Online Training provides federal responders with knowledge of the current opioid crisis. State, local, tribal, and territorial health agencies can now access this training to support their agency’s efforts. Learn more about Opioid Rapid Response Program Online Training [PDF].
Responding to Disruptions: ORRP partners with ASTHO to facilitate scenario-based practice exercises with states. ASTHO also collects and shares materials developed and used by state, local, tribal, and territorial health agencies to respond to disruptions in prescription opioid supply.
Communicating in a Crisis: Crisis and Emergency Risk Communication (CERC) in Response to an Opioid Overdose Event [PDF] outlines the six principles of CERC and how to apply them to an opioid overdose event.
