Teen Newsletter: Gonorrhea
April 2024
The David J. Sencer CDC Museum (CDCM) Public Health Academy Teen Newsletter was created to introduce teens to public health topics. Each newsletter focuses on a different public health topic that CDC studies. Newsletter sections are: Introduction, CDC’s Work, The Public Health Approach and Out of the CDC Museum Collection.
Gonorrhea is a sexually transmitted infection, or STI (sometimes called a sexually transmitted disease, or STD), that can cause infection in the genitals, rectum, and throat. It is very common, especially among people ages 15-24 years. In fact, gonorrhea is the in the U.S.
Sexually active people can get gonorrhea through vaginal, anal, or oral sex without a condom with a partner who has gonorrhea. If you are sexually active, you can lower your chances of getting gonorrhea by using condoms the right way every time you have sex and by being in a long-term mutually monogamous relationship with a partner who has tested negative for gonorrhea.
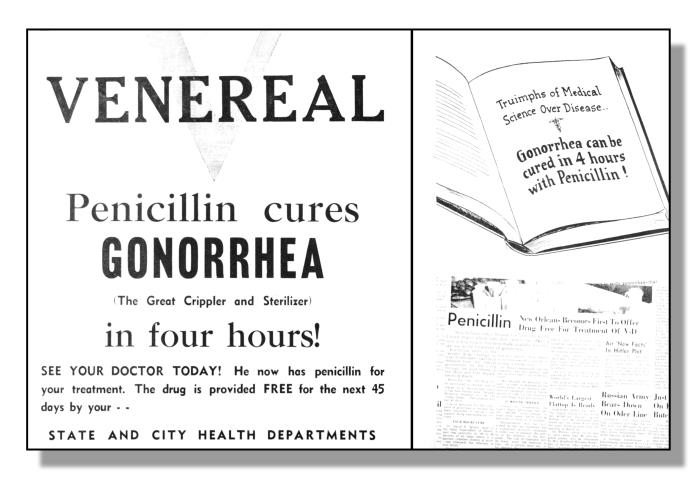
An educational poster from the World War II era, which announced how gonorrhea can be cured by penicillin, the most prominent antibiotic at the time
Symptoms can include an unusual sore, a smelly discharge, burning when peeing, or bleeding between periods. However, most people have no symptoms. Even when there are symptoms, they are often mild and can be mistaken for something else, like a bladder or vaginal infection. It is important to note that gonorrhea cause serious health problems, even with mild or no symptoms.
Anyone who is sexually active should discuss their sexual history and any symptoms they have with a healthcare provider and ask whether they should be tested for gonorrhea or other STIs.
Gonorrhea can be cured with the right antibiotics. While penicillin was originally used to cure gonorrhea, this is no longer the case. It has become harder to treat some gonorrhea, as drug-resistant strains of gonorrhea are increasing. If symptoms continue for more than a few days after receiving treatment, it is important to return to your healthcare provider. Know the steps to take if you are diagnosed.

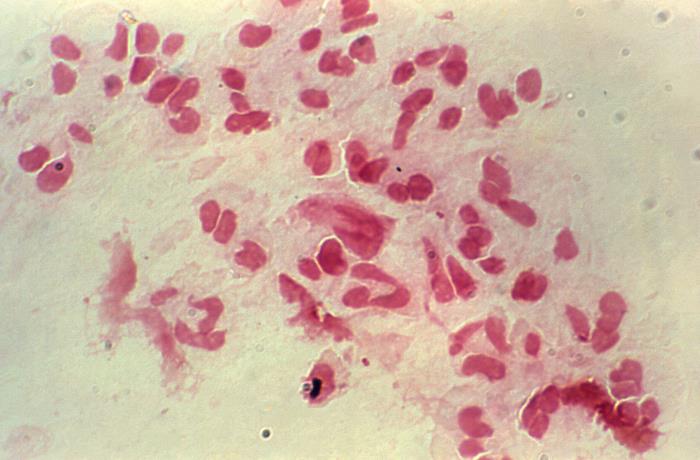
A picture from 1970 that shows a gonococcal lesion, the result of gonorrhea spreading throughout the body
It is essential to seek treatment and to follow up about symptoms, as gonorrhea can cause severe and permanent health problems. In women, untreated gonorrhea can cause pelvic inflammatory disease (PID). Learn about the complications of PID. In men, gonorrhea can cause a painful condition in the tubes attached to the testicles, which can, in rare cases, lead to infertility.
Rarely, untreated gonorrhea can also spread to your blood or joints. This condition is life-threatening. Untreated gonorrhea may also increase your chance of getting or giving HIV.
The National Center for HIV, Viral Hepatitis, STD, and TB Prevention (NCHHSTP), is the CDC center that leads work on gonorrhea. NCHHSTP is committed to a future free of HIV, viral hepatitis, STIs, and TB. The Center addresses some of the nation’s most prevalent infectious diseases with the goals to reduce incidence of infection, morbidity and mortality, and health disparities.
The Division of STD Prevention (DSTDP), within NCHHSTP, specifically coordinates gonorrhea prevention and response. The mission of DSTDP is to provide national leadership, research, policy development, and scientific information to help people live safer, healthier lives by the prevention of STIs and their complications.
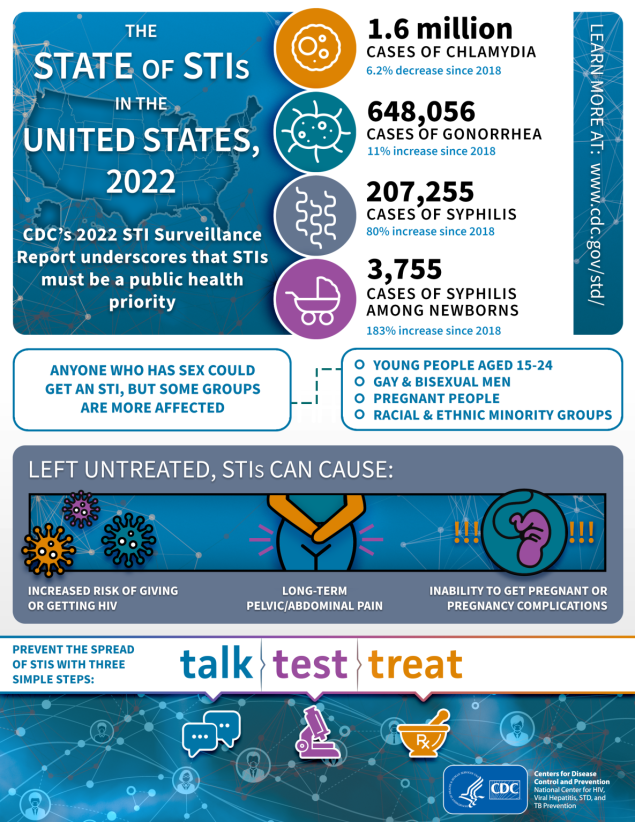
An infographic showing the state of STIs in the United States, as of 2022
The NCHHSTP and DSTDP websites are both great places to look for information on gonorrhea. For instance, on the NCHHSTP website you can access AtlasPlus, an interactive mapping tool that can be used to research rates & cases of specific illnesses, including gonorrhea. On the DSTDP website, you can learn about gonorrhea prevention and how it fits into the broader framework of the social determinants of health and the promotion of sexual health.
Public health problems are diverse and can include infectious diseases, chronic diseases, emergencies, injuries, environmental health problems, as well as other health threats. Regardless of the topic, we take the same systematic, science-based approach to a public health problem by following four general steps.
- Surveillance (What is the problem?). In public health, we identify the problem by using surveillance systems to monitor health events and behaviors occurring among a population.

Reported cases by sex, United States, 2013–2022. Rates increased from 2013 to 2021, and began to decrease between 2021 and 2022
For this section of the newsletter, we are going to dog into an example of public health in action in Baltimore, Maryland.
The Community-based Approaches to Reducing STDs (CARS) initiative mission to address STI rates among adolescents. Before diving into the details of this public health initiative, we need to understand how CDC compiles the STI data that inform public health interventions. The CDC collects nation-level data on gonorrhea rates through the National Notifiable Disease Surveillance System (NNDSS). This data showed that rates of reported gonorrhea increased from 2013 through 2021.
From 2021 to 2022, rates of reported gonorrhea began to decrease. However, there were still 648, 056 total cases of gonorrhea reported in 2022. And, disparities remain in reported STIs among some racial minority or Hispanic ethnicity groups, when compared with rates among non-Hispanic White persons. Furthermore, adolescents are disproportionately affected by STIs. In 2022, half (49.8%) of reported cases of chlamydia, gonorrhea, and syphilis (all stages) were among adolescents and young adults aged 15–24 years.
Many infections go undetected and unreported to CDC. To take this into account, CDC uses rigorous modeling approaches to better understand the vast scope of the STI epidemic and who is most affected. Separate estimates suggest there are approximately 26 million new STIs every year, and almost half of these new infections occur in young people ages 15-24.
- Risk Factor Identification (What is the cause?). After we’ve identified the problem, the next question is, “What is the cause of the problem?” For example, are there factors that might make certain populations more susceptible to diseases, such as something in the environment or certain behaviors that people are practicing?

Caption: Gonorrhea disproportionately affects those who are between 15 and 24
To address disparities in STI prevention, the Community-based Approaches to Reducing STDs (CARS) initiative was established. During CARS Phase 2 (September 2014-September 2017), the Baltimore City Health Department collaborated with the Johns Hopkins School of Medicine’s Center for Child and Community Health Research. The main goal of the effort was to reduce chlamydia and gonorrhea among Baltimore City’s young people aged 15-24 in selected areas.
Typically, STI programs have focused on individual-level interventions that can be difficult to sustain without funding. The Baltimore City Health Department engaged community board members and partners on how to best address health disparities and STI prevention. They conducted a root cause analysis with members to help them to identify underlying causes of the prioritized social determinants of health. Young board members identified the following three priority social determinants: lack of sexual health education, lack of sexual health services, and negative culture/perceptions of STI testing.
- Intervention Evaluation (What works?). Once we’ve identified the risk factors related to the problem, we ask, “What intervention works to address the problem?” We look at what has worked in the past in addressing this same problem and if a proposed intervention makes sense with our affected population.
The CARS initiative uses one of CDC’s key strategies: employing community engagement methods to achieve health equity. Health equity is achieved when everyone has an equal chance to be healthy regardless of his or her race/ethnicity, sexual orientation, or social class. Learning more about the individual and social factors that sustain STI epidemics is a vital first step in assisting affected communities to improve their health status. To prevent and control STIs, communities need quality health information and services. Before it was established in Baltimore, the CARS initiative was implemented in Los Angeles, Philadelphia, Richmond, and San Antonio. In this first stage of the CARS initiative, important lessons were learned: to maintain frequent, regular contact with partners and in a timely manner.
- Implementation (How did we do it?). In the last step, we ask, “How can we implement the intervention? Given the resources we have and what we know about the affected population, will this work?”

Picture of an STI kit that Baltimore residents can access through the I Want the Kit program
To address the lack of sexual health services and negative culture of STI testing, the health department worked with Johns Hopkins to develop and implement protocols for expanded community based STI testing and improve the STI testing environment for clients.
Johns Hopkins contracted with the Maryland Institute College of Arts Center for Social Design to assist with the development and design of communication materials to address the negative culture of SI testing. Changes addressed the issues raised by clinic clients: lack of transparency and predictability of the STI testing process, long wait times, and anxiety. The health department also worked with the community-based program, I Want the Kit, to test 461 youth for chlamydia and gonorrhea in the community.
The CARS Program in Baltimore was very successful! Its major strength was its emphasis on recruiting responsible youth to provide meaningful, engaging outreach to their peers to help lower rates of chlamydia and gonorrhea. Between June 2016 and March 2018, the Baltimore County Health Department/CARS program provided: 663 tests for chlamydia, gonorrhea, syphilis, and HIV; 25 outreach trainings for Baltimore communities; and reached 6800+ young adults via CARS educational events.

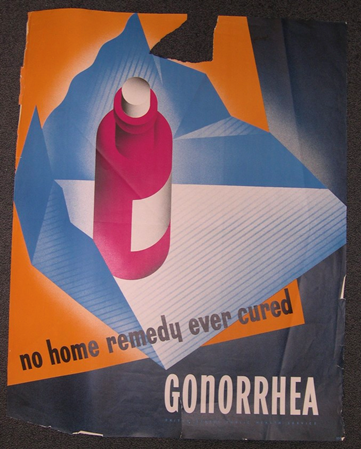
No home remedy ever cured gonorrhea, by Leonard Karsakov, ca. 1945
This newsletter’s Out of the CDC Museum Collection is a poster by the artist Leonard Karsakov. It was commissioned by the U.S. Public Health Service. Originally created to protect the health of sailors and immigrants in the late 1700s, the USPHS’s role in healthcare soon grew to encompass many aspects of public health, including STI prevention. A new division of the USPHS was formed, called the Venereal Disease Division. Venereal disease, or VD, is the older term for what now is referred to as sexually transmitted infections, or STIs.
This poster encouraged people to seek medical treatment for gonorrhea, instead of home remedies. At the time, many people were unaware that antibiotics could effectively cure STIs. It was important that people know that there was a solution to their sickness before the effects of their gonorrhea could worsen.
Around 12 years after this poster was made, in 1957, the Public Health Service transferred its Venereal Disease Division to CDC. These were the origins of CDC’s Division of STD Prevention.