Improving Tobacco Control

The Problem
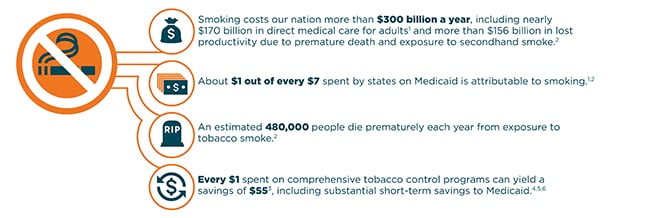
Tobacco use imposes a considerable burden on society, including disease, lives lost, health care costs, and economic costs resulting from lost productivity. Smoking is the leading cause of premature death and preventable disease in the United States and is responsible for about 480,000 premature deaths each year.
Smoking is a multi-billion dollar problem causing hundreds of thousands of premature deaths.
What Can Be Done?
Comprehensive tobacco control efforts save lives, improve health outcomes, and reduce health care and lost-productivity costs. To maximize health and economic benefits, CDC recommends investments in comprehensive statewide tobacco control programs that include the following components:
- State and community interventions to prevent initiation of tobacco use, promote tobacco cessation, eliminate exposure to secondhand smoke, and identify and eliminate tobacco-related disparities;
- Mass-reach health communication interventions to raise awareness of the health effects of smoking and secondhand smoke exposure, promote tobacco cessation, and discourage tobacco use initiation;
- Cessation interventions that expand insurance coverage for cessation treatments and use of these treatments, make tobacco-dependence treatment part of routine clinical care, and increase quitline capacity;
- Surveillance and evaluation of attitudes, behaviors, and health outcomes to assess program effectiveness and impact over time; and
- Infrastructure, administration, and management to achieve the capacity needed to sustain program effectiveness and efficiency and foster collaboration among state and local entities.
Resources for Action
Public Health Practitioners
Additional resources for state health officials, local health department officials, or other public health practitioners:
- : The CDC Office on Smoking and Health homepage, featuring the latest scientific research and a media campaign resource center.
- Best Practices for Comprehensive Tobacco Control Programs—2014: CDC’s guide to assist states in making decisions about investments in their tobacco control programs. The report outlines the vision of how sustained resources can be invested in specific programmatic interventions proven to prevent and reduce tobacco use.
- The Health Consequences of Smoking—50 Years of Progress: A Report of the Surgeon General: The latest synthesis of the scientific evidence of the harms of smoking and tobacco use, and what we know works to reduce and prevent tobacco use.
- : CDC’s Tips from Former Smokers resource page, containing Tips national education campaign materials for states and programs to use.
- CDC Cessation Materials and Guidelines: CDC’s resources on what works to promote cessation through health care systems.
- CDC Vital Signs on Secondhand Smoke: CDC’s February 2015 Vital Signs report on the dangers of secondhand smoke and what can be done to prevent or reduce exposure to tobacco smoke.
State Decision Makers
Additional resources for governors, health policy advisors, legislators, budget officers, or other decision makers:
- : The CDC Office on Smoking and Health homepage, featuring the latest scientific research and a media campaign resource center.
- Best Practices for Comprehensive Tobacco Control Programs—2014: CDC’s guide to assist states in making decisions about investments in their tobacco control programs. The report outlines the vision of how sustained resources can be invested in specific programmatic interventions proven to prevent and reduce tobacco use.
- The Health Consequences of Smoking—50 Years of Progress: A Report of the Surgeon General: The latest synthesis of the scientific evidence of the harms of smoking and tobacco use, and what we know works to reduce and prevent tobacco use.
- CDC State Activities Tracking and Evaluation System (STATE) System: CDC’s STATE System allows users to compare state data on epidemiology, funding, legislation, and other topics to other states and over time.
- Prevention Status Report for Tobacco Use: The Prevention Status Reports highlight—for all 50 states and D.C.—the status of select policies and practices that can help states prevent or reduce smoking or exposure to secondhand smoke.
State Medicaid Officials
Additional resources for state Medicaid programs:
- : The CDC Office on Smoking and Health homepage, featuring the latest scientific research and a media campaign resource center.
- : CDC’s Tips from Former Smokers resource page, containing Tips national education campaign materials for states and programs to use.
- CDC Cessation Materials and Guidelines: CDC’s resources on what works to promote cessation through health care systems.
- CDC Case Study: The Effect of Expanding Cessation Coverage—The Massachusetts Medicaid Cessation Benefit: A CDC case study highlighting how a broad Medicaid cessation benefit can increase use of evidence-based cessation treatments, reduce smoking rates, improve health outcomes, and decrease medical costs over a short time period.
- Medicaid Tobacco Cessation: : Centers for Medicare & Medicaid Services’ resources for Medicaid coverage of tobacco-cessation programs, including recent changes provided under the Patient Protection and Affordable Care Act.
- The Kaiser Family Foundation: State Medicaid Program Coverage of Tobacco Dependence Treatments by Type of Coverage: A comparison of state coverage for different types of cessation treatments.
Health System Stakeholders
Additional resources for stakeholders affiliated with a health system, including health providers, health insurers, or other health system stakeholders:
- : The CDC Office on Smoking and Health homepage, featuring the latest scientific research and a media campaign resource center.
- : CDC’s Tips from Former Smokers resource page, containing Tips national education campaign materials for states and programs to use.
- CDC Cessation Materials and Guidelines: CDC’s resources on what works to promote cessation through health care systems.
- AHRQ Systems Change: Treating Tobacco Use and Dependence : Strategies for health care systems to improve tobacco-cessation treatment.
- Code of practice on tobacco control for health professional organizations : World Health Organization’s Tobacco Free Initiative, including the code of practice on tobacco control for health professional organizations.
State Examples
California
Between 1989 and 2008, the California tobacco control program, which cost an estimated $2.4 billion, reduced health care expenditures statewide by an estimated $134 billion. California used a comprehensive approach to tobacco control efforts, including community interventions, smoke-free laws, tobacco tax increases, and media campaigns that included promotion of state cessation and quitline services. Between 1988 and 2010, the adult smoking rate in California fell from 22.7 percent to 11.9 percent. Since 1998, lung cancer incidence in California has been declining four times faster than in the rest of the United States.7
Arizona
Arizona’s tobacco control program has focused on preventing youth initiation of tobacco use.8 Between 1996 and 2004, the Arizona program, which cost $235 million, generated about $2 billion in health care cost savings.9
Florida
From 1998 to 2003, a comprehensive prevention program in Florida, anchored by an aggressive youth-oriented health communication campaign, reduced the prevalence of smoking among middle- and high-school students by 50 percent and 35 percent, respectively.10
New York
From 2001 to 2010, the New York State Tobacco Control Program reported declines in the preva¬lence of smoking among adults and youth that outpaced declines nationally.11 As a result, smoking-attributable personal health care expen¬ditures in New York in 2010 were $4.1 billion less than they would have been had the prevalence of smoking remained at 2001 levels.8
Strategies for Improved Public Health
State and Community Interventions
Active, coordinated, state- and community-level interventions form the foundation of comprehensive tobacco control programs. These interventions mobilize communities to:
- Promote tobacco use cessation;
- Prevent tobacco use initiation;
- Eliminate secondhand smoke exposure; and
- Identify and eliminate tobacco-related disparities.
Mass-Reach Health Communication Interventions
Typically, the most effective state and community interventions are those that are combined with mass-reach health communication interventions. This involves strategic, culturally appropriate, and high-impact messages delivered through sustained and adequately funded campaigns and a variety of media, such as television, radio, print, Internet and social media, and local events.
Cessation Interventions
Comprehensive tobacco cessation activities can focus on three broad goals: 1) promoting health systems change to fully integrate tobacco-dependence treatment into routine clinical care; 2) expanding public and private insurance coverage of proven cessation treatments; and 3) supporting state quitline capacity.
Surveillance and Evaluation
Monitoring the achievement of program goals and evaluating implementation and outcomes increase efficiency and impact over time, demonstrate accountability, and provide credible information for programmatic decision making.
Infrastructure, Administration, and Management
To be effective, efficient, and sustainable, comprehensive tobacco control programs need to be appropriately resourced with adequate funding, staff, leadership, and support.
References
1 Xu X, Bishop EE, Kennedy SM, Simpson SA, Pechacek TF. Annual healthcare spending attributable to cigarette smoking: An update. American Journal of Preventive medicine 2014; 48(3). doi: 10.1016/j.amepre.2014.10.012.
2 U.S. Department of Health and Human Services. The Health Consequences of Smoking—50 Years of Progress. A Report of the Surgeon General. Atlanta, GA: U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health, 2014.
3 Lightwood J, Glantz SA. The effect of the California tobacco control program on smoking prevalence, cigarette consumption, and healthcare costs: 1989-2008. PLoS One 2013; 8(2):e47145.
4 Richard P, West K, Ku L. The Return on Investment of a Medicaid Tobacco Cessation Program in Massachusetts. PLoS ONE 2012; 7(1): e29665. doi:10.1371/journal.pone.0029665.
5 McCallum, D. M. & Fosson, G. H. & Pisu, M. Making the Case for Medicaid Funding of Smoking Cessation Treatment Programs: An Application to State-Level Health Care Savings.” Journal of Health Care for the Poor and Underserved, vol. 25 no. 4, 2014, pp. 1922-1940. Project MUSE. doi:10.1353/hpu.2014.0171.
6 Athar, H., et al. Impact of Increasing Coverage for Select Smoking Cessation Therapies With no Out-of-Pocket Cost Among the Medicaid Population in Alabama, Georgia, and Maine. Journal of Public Health Management and Practice 2016. 22(1): 40-47.
7 Centers for Disease Control and Prevention. Best Practices for Comprehensive Tobacco Control Programs—2014. Atlanta: U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health, 2014.
8 Meister JS. Designing an effective statewide tobacco control program—Arizona. Cancer 1998; 83(S12A): 2728–32, doi: 10.1002/(SICI) 1097-0142(19981215)83:12A+<2728::AID-CNCR13>3.0.CO; 2-3. Available at Wiley Online Library .
9 Lightwood J, Glantz S. Effect of the Arizona tobacco control program on cigarette consumption and healthcare expenditures. Soc Sci Med 2011; 72(2): 166–72, doi: 10.1016/j.socscimed.2010.11.015.
10 Bauer UE, Johnson TM, Hopkins RS, Brooks RG. Changes in youth cigarette use and intentions following implementation of a tobacco control program. JAMA 2000; 284(6): 723–8.
11 RTI International. 2011 Independent Evaluation Report of the New York Tobacco Control Program. Albany, NY: New York State Department of Health, 2011.