Emergency Department Visit Rates for Assault: United States, 2019–2021
NCHS Data Brief No. 481, October 2023
PDF Version (462 KB)
Danielle Davis, M.P.H., and Loredana Santo, M.D., M.P.H.
- Key findings
- The annual average ED visit rates for assault differed among age groups, but not by sex.
- The annual average ED visit rates for assault differed by race and ethnicity.
- The annual average ED visit rates for assault differed by primary expected source of payment.
- The annual average ED visit rate for assault differed by metropolitan statistical area but not by region.
- Summary
Data from the National Hospital Ambulatory Medical Care Survey
- During 2019–2021, the overall emergency department (ED) visit rate for assault was 4.5 visits per 1,000 people per year.
- ED visit rates for assault were highest for people ages 18–24 (9.2) and 25–44 (7.7), and then declined with age.
- The ED visit rate for assault was highest for Black non-Hispanic people compared with all other race and ethnicity groups.
- Medicaid, Children’s Health Insurance Program, or other state-based program was the most common primary expected source of payment among ED visits for people injured by assault.
- The ED visit rate for assault was higher for people who visited hospitals in metropolitan statistical areas (4.9) compared with nonmetropolitan statistical areas (2.0).
Nonfatal injuries are major causes of emergency department (ED) visits in the United States (1). The National Center for Injury Prevention and Control estimated that, in 2020, 22.9 million ED visits related to nonfatal injuries occurred (1). Visits for assault (excluding sexual assault) represented 5.8% of these visits (1). This report uses the most recent data from the National Hospital Ambulatory Medical Care Survey (NHAMCS) to present assault-related ED visit (excluding sexual assault) rates by selected demographic and hospital characteristics.
Keywords: injury, victim, race and ethnicity, National Hospital Ambulatory Medical Care Survey
The annual average ED visit rates for assault differed among age groups, but not by sex.
- The 2019–2021 annual average visit rate for assault injuries was 4.5 visits per 1,000 people (Figure 1).
- The ED visit rate for assault was similar for males (4.9) and females (4.2).
- Among adults, ED visit rates for assault injuries decreased with increasing age, from 9.2 for adults ages 18–24 to 1.9 for adults ages 55 and older. The rate for visits for people ages 0–17 years (2.6) was lower than the rate for people ages 18–54 but was not significantly different from the rate for the oldest age group.
Figure 1. Annual average visit rate to emergency departments for assault, by sex and age, United States: 2019–2021
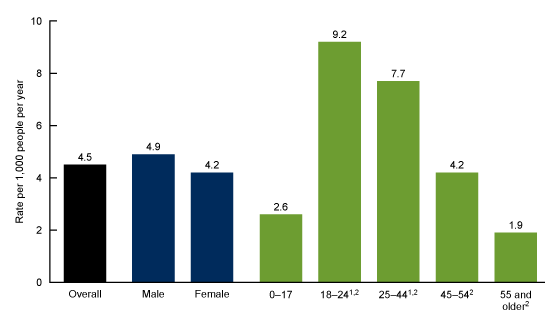
1Rate is significantly higher than rates for 0–17, 45–54, and 55 and older age groups.
2Statistically significant decreasing trend with increasing age (p < 0.05).
NOTES: Data are based on a sample of 603 emergency department visits by patients with any listed diagnosis or cause of injury of assault using International Classification of Diseases, 10th Revision, Clinical Modification codes X92–Y09, representing an annual average of approximately 1.5 million emergency department visits (1.1% of all emergency department visits and 4.4% of all injury visits). Visit rates are based on sets of estimates of the U.S. civilian noninstitutionalized population developed by the U.S. Census Bureau and reflect the population as of July 1 of each year during 2019–2021. Access data table for Figure 1.
SOURCE: National Center for Health Statistics, National Hospital Ambulatory Medical Care Survey, 2019–2021.
The annual average ED visit rates for assault differed by race and ethnicity.
- The ED visit rate for assault injuries was highest for Black non-Hispanic (subsequently, Black) people (13.8 visits per 1,000 people per year), followed by Hispanic people (4.6) and White non-Hispanic people (3.1). Rates were lowest among people of other non-Hispanic races (1.4) (Figure 2).
Figure 2. Annual average visit rate to emergency departments for assault, by race and ethnicity: United States, 2019–2021
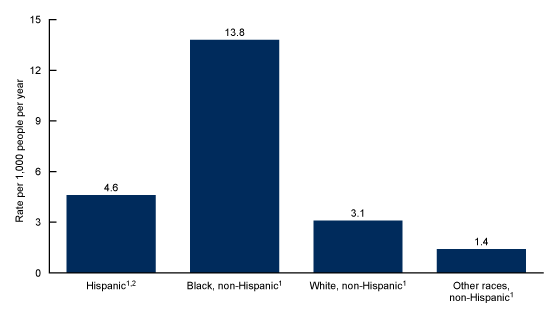
1Rate is significantly different from all other rates.
2People of Hispanic origin may be of any race.
NOTES: Data are based on a sample of 603 emergency department visits by patients with any listed diagnosis or cause of injury of assault using International Classification of Diseases, 10th Revision, Clinical Modification codes X92–Y09, representing an annual average of approximately 1.5 million emergency department visits (1.1% of all emergency department visits and 4.4% of all injury visits). Visit rates are based on sets of estimates of the U.S. civilian noninstitutionalized population developed by the U.S. Census Bureau and reflect the population as of July 1 of each year during 2019–2021. Other races non-Hispanic includes Asian, Native Hawaiian or Other Pacific Islander, and American Indian and Alaska Native people, and people of two or more races. Access data table for Figure 2.
SOURCE: National Center for Health Statistics, National Hospital Ambulatory Medical Care Survey, 2019–2021.
The annual average ED visit rates for assault differed by primary expected source of payment.
- The ED visit rate for assault injuries was highest for visits covered by Medicaid, Children’s Health Insurance Program, or other state-based program as the primary source of payment (11.3 visits per 1,000 people per year), followed by no insurance (6.3), private insurance (1.6), and Medicare (1.6) (Figure 3).
Figure 3. Annual average visit rate to emergency departments for assault, by primary expected source of payment: United States, 2019–2021
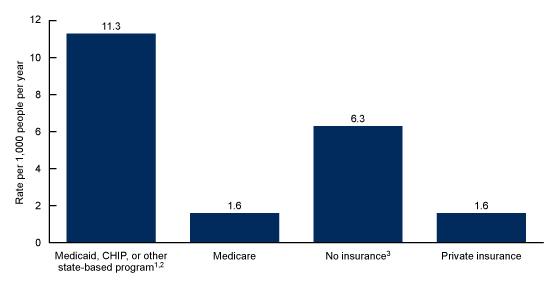
1Rate is significantly higher than all other rates.
2CHIP is the Children’s Health Insurance Program.
3Rate is significantly different from all other rates.
NOTES: Data are based on a sample of 603 emergency department visits by patients with any listed diagnosis or cause of injury of assault using International Classification of Diseases, 10th Revision, Clinical Modification codes X92–Y09, representing an annual average of approximately 1.5 million emergency department visits (1.1% of all emergency department visits and 4.4% of all injury visits). Visit rates are based on the patient’s primary expected source of payment (a recoded variable based on a hierarchical model that accounts for the possibility of multiple payment sources being reported) and proportional insurance data from the 2019–2021 National Health Interview Survey Person Files. Visits with workers’ compensation as the primary expected source of payment represented 1.5% of weighted data, and other sources of payment represented 5.1% of weighted data. These data are included in the denominator but are not reported separately due to small sample sizes. Access data table for Figure 3.
SOURCE: Center for Health Statistics, National Hospital Ambulatory Medical Care Survey, 2019–2021.
The annual average ED visit rate for assault differed by metropolitan statistical area but not by region.
- ED visit rates were similar by U.S. Census region. Hospitals in the Northeast had 4.9 visits for assault injuries, hospitals in the Midwest had 5.3 visits, hospitals in the South had 4.3 visits, and hospitals in the West had 4.0 visits (Figure 4).
- The ED visit rate for assault injuries for people who visited hospitals in metropolitan statistical areas (MSAs) (4.9 per 1,000 people per year) was higher than the rate for people who visited hospitals in non-MSAs (2.0).
Figure 4. Annual average visit rate to emergency departments for assault, by census region and hospital metropolitan statistical area: United States, 2019–2021
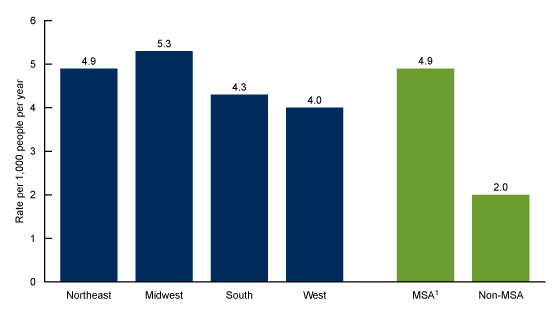
1Rate is significantly higher than rate for non-MSA.
NOTES: Data are based on a sample of 603 emergency department visits by patients with any listed diagnosis or cause of injury of assault using International Classification of Diseases, 10th Revision, Clinical Modification codes X92–Y09, representing an annual average of approximately 1.5 million emergency department visits (1.1% of all emergency department visits and 4.4% of all injury visits). Visit rates are based on sets of estimates of the U.S. civilian noninstitutionalized population developed by the U.S. Census Bureau and reflect the population as of July 1 of each year during 2019–2021. MSA is metropolitan statistical area, a population with more than 50,000 people. A non-MSA includes populations with less than 50,000 people, including noncore rural areas. Access data table for Figure 4.
SOURCE: National Center for Health Statistics, National Hospital Ambulatory Medical Care Survey, 2019–2021.National Center for Health Statistics, National Health Interview Survey, 2022.
Summary
This report examines ED visit rates for assault during 2019–2021. Differences by age, race and ethnicity, primary expected source of payment, and hospital location are identified. ED visit rates related to assault for people ages 18–44 were higher than rates for children and adolescents and decreased with increasing age for adults. The ED visit rate for assault was highest for Black people and for people with Medicaid as the primary source of payment. The ED visit rate for assault was higher for people who visited hospitals in MSAs than for those who visited hospitals in non-MSAs. This report, based on the most recent estimates from NHAMCS on ED visits made by people with injuries related to assault, highlights differences in ED use by demographic and hospital characteristics.
Definitions
Metropolitan statistical area (MSA): Based on the actual location of the hospital and the definition of the U.S. Census Bureau and the Office of Management and Budget; updated each year based on the latest Office of Management and Budget guidance.
- MSA: Has at least one urbanized area of 50,000 or more population, plus adjacent territory that has a high degree of social and economic integration with the core as measured by commuting ties.
- Non-MSA: Includes noncore rural areas as well as micropolitan statistical areas, areas that have at least one urban cluster of at least 10,000 but less than 50,000 population, plus adjacent territory that has a high degree of social and economic integration with the core as measured by commuting ties.
Primary expected source of payment for this visit: During data collection, all sources of payment were collected. For patients with more than one source of payment, the hierarchy below was used (with Medicare counted first and self-pay and no charge counted last) to combine payments into one mutually exclusive variable (primary expected source of payment). Primary expected source of payment data were missing for 15.7% of ED visits for assault.
- Medicare: Charges paid in part or in full by a Medicare plan. Includes payments made directly to the hospital as well as payments reimbursed to the patient. Charges covered under a Medicare-sponsored prepaid plan are included.
- Medicaid or Children’s Health Insurance Program: Charges paid in part or in full by a Medicaid plan. Includes payments made directly to the hospital or reimbursed to the patients. Charges covered under a Medicaid-sponsored prepaid plan or the Children’s Health Insurance Program are included as well as other state-based programs.
- Private insurance: Charges paid in part or in full by a private insurer (for example, BlueCross BlueShield). Includes payments made directly to the hospital or reimbursed to the patient. Charges covered under a private insurance-sponsored prepaid plan are included.
- Workers’ compensation or other: Includes programs designed to enable employees injured on the job to receive financial compensation regardless of fault. Also includes other sources of payment. Visits with workers’ compensation as the primary expected source of payment represented 1.5% of weighted data, and other sources of payment represented 5.1% of weighted data. These data are included in the denominator but are not reported separately due to small sample sizes.
- No insurance: Includes self-pay and no charge or charity. Self-pay includes charges that are paid by the patient or patient’s family, which will not be reimbursed by a third party. Self-pay includes visits for which the patient is expected to be ultimately responsible for most of the bill, even if the patient never actually pays it. This does not include copayments or deductibles. No charge or charity is the category for visits for which no fee is charged (for example, charity, special research, or teaching). No charge or charity does not include visits paid for as part of a total package (for example, prepaid plan visits, postoperative visits included in a surgical fee, and pregnancy visits included in a flat fee charged for the entire pregnancy).
Race and ethnicity: Race and Hispanic ethnicity were collected separately and converted into a single combined variable that includes Black non-Hispanic, White non-Hispanic, Hispanic, and other races non-Hispanic. Overall, from 2019 to 2021, 21.3% of weighted race data and 16.5% of weighted ethnicity data were reported missing for ED visits for assault. Race and ethnicity were imputed for these missing records using a model-based, single, sequential regression imputation method (2–4). Other races includes Asian, Native Hawaiian or Other Pacific Islander, and American Indian and Alaska Native people, and people of two or more races.
Visit for assault: An injury-related visit with any listed diagnosis or external cause-of-injury code related to assault from the International Classification of Diseases, 10th Revision, Clinical Modification (ICD–10–CM). Specifically, these codes are X92–Y09, based on the revised ICD–10–CM surveillance case definition for injury-related ED visits (5). Injury-related ED visits for sexual assault were not included in the documented case definition for assault.
Data source and methods
Analyses for this report were conducted using data from a restricted-use data file. A public-use version of this file is available from: https://www.cdc.gov/nchs/ahcd/datasets_documentation_related.htm.
Count estimates and measures of variance could differ between the restricted-use and public-use files. Information for accessing the restricted-use data file is available from: https://www.cdc.gov/rdc/index.htm.
This report analyzed data files from the 2019, 2020, and 2021 NHAMCS, a nationally representative survey of nonfederal, general, and short-stay hospitals conducted by the National Center for Health Statistics. NHAMCS uses a multistage probability design with samples of geographic primary sampling units, hospitals within primary sampling units, and patient visits within EDs. Additional information on the methodology of NHAMCS is available online, as are the public-use data files (2–4).
The study population includes any listed cause-of-injury ED visits made by patients who were victims of assault. ED rates by age, sex, race and ethnicity, and region were calculated by dividing the number of ED visits caused by assault from the July 1, 2019; July 1, 2020; and July 1, 2021, sets of estimates of the U.S. civilian noninstitutionalized population (obtained from the U.S. Census Bureau’s Population Division) for each demographic group. Three years of data were combined to increase estimate reliability. Visit rates for assault injuries for 2019–2021 displayed a similar pattern; no significant differences were found across years. Rates by expected source of payment were calculated by dividing the number of ED visits caused by assault by the National Health Interview Survey 2019–2021 estimates of insurance coverage in the U.S. civilian noninstitutionalized population. The observed differences were statistically significant unless indicated otherwise.
Data analysis was performed using the statistical packages SAS version 9.4 (SAS Institute, Cary, N.C.) and SAS-callable SUDAAN version 11.0 (RTI International, Research Triangle Park, N.C.). Linear regression was used to test the significance of slope for age trends. All rate estimates presented meet National Center for Health Statistics guidelines for presentation of rates and follow National Center for Health Statistics trend analysis guidelines (6). Differences among subgroups were evaluated using a two-tailed t test (p < 0.05).
About the authors
Danielle Davis and Loredana Santo are with the National Center for Health Statistics, Division of Health Care Statistics.
References
- Centers for Disease Control and Prevention, National Center for Injury Prevention and Control. WISQARS. Injury counts and rates.
- National Center for Health Statistics. 2019 NHAMCS micro-data file documentation. 2021.
- National Center for Health Statistics. 2020 NHAMCS micro-data file documentation. 2022.
- National Center for Health Statistics. 2021 NHAMCS micro-data file documentation. 2023.
- Hedegaard H, Garnett MF, Johnson RL, Thomas KE. A revised ICD–10–CM surveillance case definition for injury-related emergency department visits. National Health Statistics Reports; no 164. Hyattsville, MD: National Center for Health Statistics. 2021. DOI: https://dx.doi.org/10.15620/cdc:109050.
- Ingram DD, Malec DJ, Makuc DM, Kruszon-Moran D, Gindi RM, Albert M, et al. National Center for Health Statistics guidelines for analysis of trends. National Center for Health Statistics. Vital Health Stat 2(179). 2018.
Suggested citation
Davis D, Santo L. Emergency department visit rates for assault: United States, 2019–2021. NCHS Data Brief, no 481. Hyattsville, MD: National Center for Health Statistics. 2023. DOI: https://dx.doi.org/10.15620/cdc:133058.
Copyright information
All material appearing in this report is in the public domain and may be reproduced or copied without permission; citation as to source, however, is appreciated.
National Center for Health Statistics
Brian C. Moyer, Ph.D., Director
Amy M. Branum, Ph.D., Associate Director for Science
Division of Health Care Statistics
Carol J. DeFrances, Ph.D., Director
Alexander Strashny, Ph.D., Associate Director for Science