Emergency Department Visit Rates by Selected Characteristics: United States, 2021
Data from the National Hospital Ambulatory Medical Care Survey
- The overall emergency department (ED) visit rate was 43 visits per 100 people in 2021.
- ED visit rates were highest for infants under age 1 year (103 visits per 100 infants) and adults aged 75 and over (66 per 100 people).
- The ED visit rate for Black or African-American non-Hispanic people (81) was the highest among the selected racial and ethnic groups.
- The ED visit rate for patients with private insurance was lowest compared with all other primary expected sources of payment, and the rate for patients with Medicaid was highest.
- In 2021, a COVID-19 diagnosis was confirmed for 3.8% of all ED patient visits.
In 2021, 140 million emergency department (ED) visits occurred in the
United States (1). During that year, about 4% of children had two or more ED visits in the past 12 months, and 18% of adults had visited the ED in the past 12 months (2,3). This report presents characteristics of ED visits by age group, sex, race and ethnicity, insurance, and mentions of COVID-19, using data from the 2021 National Hospital Ambulatory Medical Care Survey (NHAMCS) (4).
Keywords: COVID-19, emergency care, patient characteristics, National Hospital Ambulatory Medical Care Survey
What was the ED visit rate in 2021, and did visit rates vary by age?
- The total ED visit rate was 43 visits per 100 people in 2021 (Figure 1).
- The ED visit rate was highest for infants under age 1 year (103 visits per 100 infants), followed by adults aged 75 and over (66 visits per 100 people). These rates were higher than for all other age groups.
- ED visit rates were similar for patients in age groups between ages 1 year and 74, ranging from 36 to 45 visits per 100 people.
Figure 1. Emergency department visit rates, by age group: United States, 2021
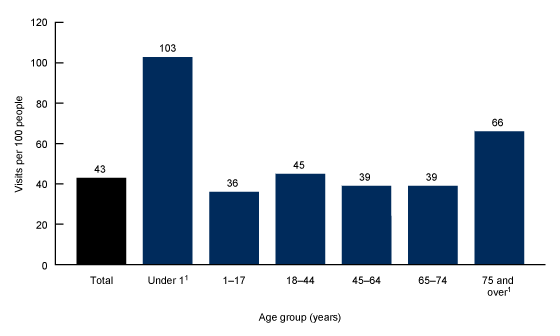
1Significantly different from all other age groups.
NOTES: Data are based on a sample of 16,207 emergency department visits made by patients in 2021, representing about 140 million emergency department visits. Visit rates are based on the July 1, 2021, set of estimates of the U.S. civilian noninstitutionalized population developed by the U.S. Census Bureau. Access data table for Figure 1.
SOURCE: National Center for Health Statistics, National Hospital Ambulatory Medical Care Survey, 2021.
Did ED visit rates vary by sex or race and ethnicity?
- The 2021 ED visit rate for females (46 visits per 100 females) was similar to the ED visit rate for males (40 visits per 100 males) (Figure 2).
- In 2021, the ED visit rate was highest for Black or African-American non-Hispanic (subsequently, Black) people (81 visits per 100 people) compared with White non-Hispanic (subsequently, White) people (41); Hispanic people (36); and people of other non-Hispanic races (subsequently, other races) (17). Rates were lowest among other races.
Figure 2. Emergency department visit rates, by patient sex and race and ethnicity: United States, 2021
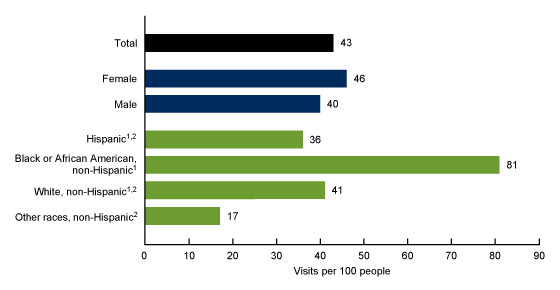
1Significantly different from patients of other non-Hispanic races (subsequently, other races).
2Significantly different from Black or African-American non-Hispanic (subsequently, Black) patients.
NOTES: Data are based on a sample of 16,207 emergency department visits by patients in 2021, representing about 140 million emergency department visits. Visit rates are based on the July 1, 2021, sets of estimates of the U.S. civilian noninstitutionalized population developed by the U.S. Census Bureau. For 2021, 20.3% of weighted race data and 15.3% of weighted ethnicity data were missing for emergency department visits, and race and ethnicity were imputed for these missing records. Race and Hispanic ethnicity were collected separately, imputed, and converted to a single combined variable that includes Hispanic, Black, and White non-Hispanic patients, and patients of other races. People of Hispanic origin may be of any race. Race and ethnicity data were imputed on the data file using a model-based, single, sequential regression imputation method, with missing race values imputed as Black only, White only, or other races only, and Hispanic ethnicity imputed as Hispanic or non-Hispanic. Other races include Asian, American Indian or Alaska Native, and Native Hawaiian or Other Pacific Islander patients and patients of two or more races. Access data table for Figure 2.
SOURCE: National Center for Health Statistics, National Hospital Ambulatory Medical Care Survey, 2021.
What were the ED visit rates for each primary expected source of payment, and did these rates vary?
- The ED visit rate was highest for patients with Medicaid, Children’s Health Insurance Program, or other state-based programs (89 visits per 100 people) and lowest for patients with private insurance (22) (Figure 3).
- The ED visit rates for patients with Medicare (46), patients with other primary expected sources of payment (43), and patients with no insurance (33) were not significantly different.
Figure 3. Emergency department visit rates, by primary expected source of payment: United States, 2021
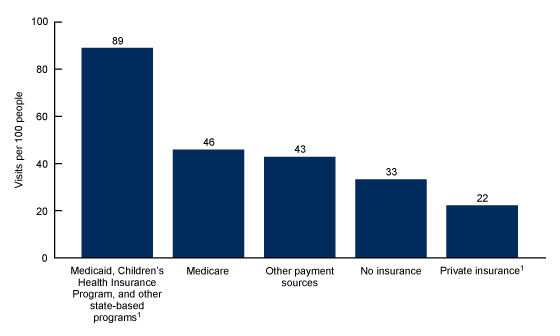
1Significantly different from all other sources of payment.
NOTES: Data are based on a sample of 16,207 emergency department visits by patients in 2021, representing about 140 million emergency department visits. Visit rates are based on the patient’s primary expected source of payment and proportional insurance data from the 2021 National Health Interview Survey, calculated from: https://www.cdc.gov/nchs/nhis/2020nhis.htm. Access data table for Figure 3.
SOURCE: National Center for Health Statistics, National Hospital Ambulatory Medical Care Survey, 2021.
What percentage of ED visits were related to COVID-19?
- An estimated 14.2% of all ED visits in 2021 had any mention of COVID-19 (Figure 4).
- COVID-19 cases were confirmed at 3.8% of ED visits.
- The percentage of ED visits with a COVID-19 test or screening was 8.8%, and 3.2% of visits included suspected exposure to COVID-19.
Figure 4. Percentage of emergency department visits with mention of COVID-19: United States, 2021
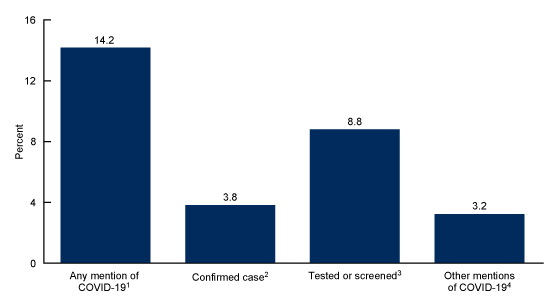
1Includes all measures shown.
2Consists of International Classification of Diseases, 10th Revision, Clinical Modification (ICD–10–CM) code U07.1.
3Consists of ICD–10–CM code Z11.52 and any mention of COVID-19 testing or screening in validated, word-for-word item notes or medication fields.
4Consists of ICD–10–CM code Z20.822 and any other mention of COVID-19 in validated, word-for-word item notes or medication fields that did not mention testing or screening.
NOTES: Categories are not mutually exclusive. Data are based on a sample of 16,207 emergency department visits made by patients in 2021, representing about 140 million emergency department visits. Access data table for Figure 4.
SOURCE: National Center for Health Statistics, National Hospital Ambulatory Medical Care Survey, 2021.
Summary
In 2021, an estimated 140 million ED visits occurred, with a total ED visit rate of 43 visits per 100 people. The ED visit rates for both infants under age 1 year and adults aged 75 and over were higher than rates for all other age groups. The ED visit rate for Black people was higher than the rates for people of all other racial and ethnic groups. The ED visit rate for patients with Medicaid was highest compared with all other sources of payment, while the rate for patients with private insurance was lowest. Data in this report show that in 2021, an estimated 14.2% of all ED visits had a mention of COVID-19, and 3.8% of all visits recorded a confirmed COVID-19 diagnosis. COVID-19 testing or screening accounted for 8.8% of all ED visits, and 3.2% of all ED visits had some mention of COVID-19 without mention of a confirmed diagnosis, test, or screening.
Definitions
COVID-19 measures: These measures are not mutually exclusive—for example, a patient may have been coded as both a confirmed and tested case:
- Any mention of COVID-19: Includes any of the measures listed in the following categories.
- Confirmed case of COVID-19: Consists of any listed diagnosis with ICD–10–CM code U07.1.
- Tested or screened for COVID-19: Consists of any listed diagnosis with ICD–10–CM code Z11.52 or any mention of COVID-19 testing or screening in validated, word-for-word item notes or medication fields.
- Other mentions of COVID-19: Consists of any listed diagnosis with ICD–10–CM code Z20.822 for suspected exposure to COVID-19 or any mention of COVID-19 in validated, word-for-word item notes or medication fields with no reference to testing or screening.
ED visit rates: Calculated by dividing the number of ED visits by estimates of the U.S. civilian noninstitutionalized population (developed by the U.S. Census Bureau’s Population Division) for selected characteristics including age group, sex, and race and ethnicity. Visit rates by patient’s primary expected source of payment are based on the patient’s primary expected payment source and proportional insurance data from the 2021 National Health Interview Survey, available from: https://www.cdc.gov/nchs/nhis/2021nhis.htm.
Primary expected source of payment: During data collection, all sources of payment were collected. For patients with more than one source of payment, the following hierarchy was used (with Medicare counted first and self-pay and no charge counted last) to combine payments into one mutually exclusive variable (primary expected source of payment):
- Medicaid: Partial or full payment by a Medicaid plan includes payments made directly to the hospital or reimbursed to the patient. Charges covered under a Medicaid-sponsored prepaid plan (such as a health maintenance organization), managed Medicaid, Children’s Health Insurance Program, and other state-based programs are included.
- Medicare: Partial or full payment by a Medicare plan includes payments made directly to the hospital and payments reimbursed to the patient. Charges covered under a Medicare-sponsored prepaid plan are included.
- Private insurance: Partial or full payment by a private insurer (such as BlueCross BlueShield) includes payments made directly to the hospital or reimbursed to the patient. Charges covered under a private insurance-sponsored prepaid plan are included.
- Uninsured: Includes self-pay and no charge or charity. Self-pay is charges paid by the patient or patient’s family that will not be reimbursed by a third party. Self-pay includes visits for which the patient is expected to be ultimately responsible for most of the bill, even if the patient never actually pays it. This does not include copayments or deductibles. No charge or charity are visits for which no fee is charged (such as charity, special research, or teaching).
- Other payment sources: Includes worker’s compensation and other sources of payment not covered by the preceding categories, such as TRICARE, state and local governments, private charitable organizations, and other liability insurance (such as automobile collision policy coverage).
Race and ethnicity: Race and Hispanic ethnicity were collected separately, imputed, and converted into a single combined variable that includes Hispanic, Black non-Hispanic, White non-Hispanic, and other races non-Hispanic. Other races includes Asian, American Indian or Alaska Native, and Native Hawaiian or Other Pacific Islander people, and people with two or more races. Statistically reliable rates could not be made for the specific race and non-Hispanic groups included under other races. For 2021, 20.3% of weighted race data and 15.3% of weighted ethnicity data were missing for ED visits; race and ethnicity were imputed for these missing records. Race and ethnicity data were imputed on the data file using a model-based, single, sequential regression imputation method. Missing race values were imputed as Black, White, or other races. This decision was based on quality concerns with imputed estimates for race categories other than Black and White, based on research by the imputation work group (5). Hispanic ethnicity was imputed as Hispanic or non-Hispanic.
Data source and methods
Data for this report are from NHAMCS, an annual, nationally representative survey of nonfederal, general, and short-stay hospitals (4). NHAMCS provides data on the use and provision of ambulatory care services in hospital EDs. In 2021, the weighted NHAMCS response rate was 46%. Analyses for this report were conducted using data from a restricted-use data file. A public-use version of this file is available from: https://www.cdc.gov/nchs/ahcd/datasets_documentation_related.htm. Count estimates and measures of variance may differ between the restricted-use and public-use files. Information on accessing the restricted-use data file is available from: https://www.cdc.gov/rdc/index.htm.
Data analyses were performed using the statistical packages SAS version 9.4 (SAS Institute, Cary, N.C.) and SAS-callable SUDAAN version 11.0 (RTI International, Research Triangle Park, N.C.). Two-tailed t tests with a significance level of p < 0.05 were used to determine statistically significant differences between ED visit rates.
About the authors
Christopher Cairns and Jill J. Ashman are with the National Center for Health Statistics, Division of Health Care Statistics. J.M. King is with RELI Group, Inc.
References
- Cairns C, Kang K. National Hospital Ambulatory Medical Care Survey: 2021 emergency department summary tables. 2023.
- National Center for Health Statistics. Percentage of two or more hospital emergency department visits in the past 12 months for children under age 18 years: United States,
2019–2021. Interactive summary health statistics for children—2019–2021. June 21, 2023.
- National Center for Health Statistics. Percentage of having a hospital emergency department visit in past 12 months for adults aged 18 and over: United States, 2019–2021. Interactive summary health statistics for adults—2019–2021. June 21, 2023.
- National Center for Health Statistics. 2021 NHAMCS micro-data file. 2023.
- National Center for Health Statistics. 2021 NHAMCS micro-data file documentation. 2023.
Suggested citation
Cairns C, Ashman JJ, King JM. Emergency department visit rates by selected characteristics: United States, 2021. NCHS Data Brief, no 478. Hyattsville, MD: National Center for Health Statistics. 2023. DOI: https://dx.doi.org/10.15620/cdc:131757.
Copyright information
All material appearing in this report is in the public domain and may be reproduced or copied without permission; citation as to source, however, is appreciated.
National Center for Health Statistics
Brian C. Moyer, Ph.D., Director
Amy M. Branum, Ph.D., Associate Director for Science
Division of Health Care Statistics
Carol J. DeFrances, Ph.D., Director
Alexander Strashny, Ph.D., Associate Director of Science