Variation in Residential Care Community Resident Characteristics, by Size of Community: United States, 2020
NCHS Data Brief No. 454, December 2022
PDF Version (356 KB)
Christine Caffrey, Ph.D., Amanuel Melekin, Ph.D., Zhaohui Lu, M.S., and Manisha Sengupta, Ph.D.
- Key findings
- In 2020, residents in larger communities were older than those in smaller communities.
- The percentage of females, non-Hispanic White residents, and Medicaid recipients varied by community size.
- The prevalence of selected medical conditions, including dementia and heart disease, varied by community size.
- The percentage of residents needing assistance in bathing, dressing, toileting, transferring, walking, and eating was highest in communities with 4–25 beds.
- Summary
Data from the 2020 National Post-acute and Long-term Care Study
- In 2020, a greater percentage of residents in residential care communities with 26 beds or more were aged 85 and over compared with smaller communities.
- About 18% of all residential care community residents were Medicaid beneficiaries, and the percentage of Medicaid recipients decreased with increasing bed size.
- The prevalence of selected medical conditions, including Alzheimer disease and heart disease, varied by community size.
- The percentage of residents needing assistance in bathing, dressing, toileting, transferring, walking, and eating was highest in communities with 4–25 beds.
Residents of residential care communities are people who cannot live independently but generally do not require the skilled care provided by nursing homes. On any given day in 2020, an estimated 818,800 residents lived in residential care communities (1,2). With the aging of the population, the number of people living in residential care communities will likely increase, creating a sizeable group within the long-term care population. This report presents national estimates of selected characteristics of residential care community residents in 2020 and compares these characteristics by community size.
Keywords: assisted living, long-term services and supports, National Post-acute and Long-term Care Surveys
In 2020, residents in larger communities were older than those in smaller communities.
- Among all residential care communities, one-half of the residents (50%) were aged 85 and over (Figure 1).
- In 2020, 13% of residents living in residential care communities with 4–25 beds were under age 65, compared with 6% in communities with 26–50 beds and 4% in communities with more than 50 beds.
- Residents aged 85 and over made up a higher percentage of residents in communities with more than 50 beds (51%) and 26–50 beds (52%) than in communities with 4–25 beds (45%).
Figure 1. Age distribution of residential care residents, by community size: United States, 2020
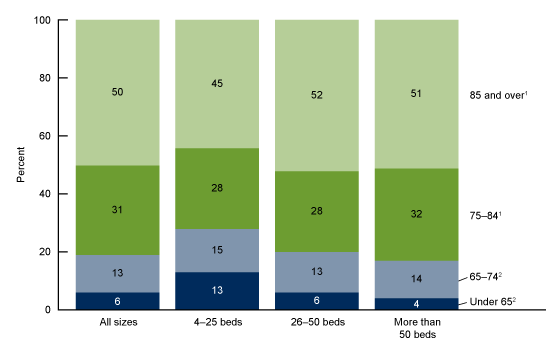
1Significantly increasing linear trend by community size.
2Significantly decreasing linear trend by community size.
NOTE: Percentages are based on unrounded numbers; estimates may not add up to totals because of rounding. Access data table for Figure 1.
SOURCE: National Center for Health Statistics, National Post-acute and Long-term Care Study, 2020.
The percentage of females, non-Hispanic White residents, and Medicaid recipients varied by community size.
- Among all residential care communities, 69% of residents were female. The percentage of female residents in communities with 26–50 and more than 50 beds was 70% compared with 68% in communities with 4–25 beds (Figure 2).
- Almost 9 in 10 (88%) residential care community residents were non-Hispanic White. The percentage of non-Hispanic White residents was lower among communities with 4–25 beds (81%) compared with 26–50 beds (91%) and more than 50 beds (89%).
- About 18% of all residential care community residents were Medicaid beneficiaries, and the percentage of Medicaid recipients decreased with increasing bed size. Of the residents in communities with 4–25 beds, 24% had at least some services paid by Medicaid compared with 23% of residents in communities with 26–50 beds and 15% in communities with more than 50 beds.
Figure 2. Selected characteristics of residential care residents, by community size: United States, 2020
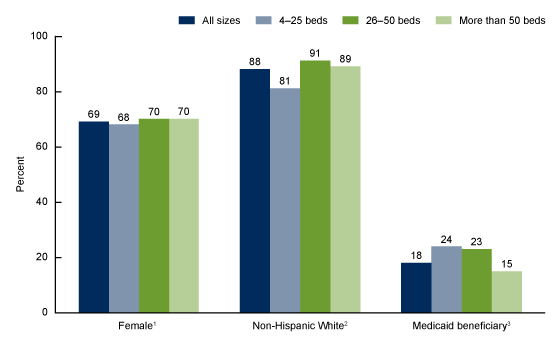
1Significant difference between communities with 4–25 beds and communities with more than 50 beds (p < 0.05).
2Significantly increasing linear trend by community size.
3Significantly decreasing linear trend by community size (p < 0.05).
NOTES: For the Medicaid variable, cases with missing data are excluded; see “Data source and methods” for details. Access data table for Figure 2.
SOURCE: National Center for Health Statistics, National Post-acute and Long-term Care Study, 2020.
The prevalence of selected medical conditions, including dementia and heart disease, varied by community size.
- Among all residential care communities, about 4 in 10 residents were diagnosed with Alzheimer disease or other dementias (42%), about 3 in 10 were diagnosed with heart disease (31%) or depression (29%), and nearly 2 in 10 were diagnosed with diabetes (17%) (Figure 3).
- The percentage of residents with Alzheimer disease and other dementias decreased with increasing community size, from 51% of residents in communities with 4–25 beds to 47% in communities with 26–50 beds to 39% in communities with more than 50 beds.
- The percentage of residents with heart disease was higher in communities with 26–50 beds (36%) compared with communities with 4–25 beds and more than 50 beds (30% each).
- The percentage of residents who had ever been diagnosed with depression was lower in communities with more than 50 beds (27%) compared with communities with 4–25 beds and 26–50 beds (33% and 32%, respectively).
- The percentage of residents with diabetes was 17% among all residential care communities and decreased with increasing bed size.
Figure 3. Selected diagnosed medical conditions among residential care residents, by community size: United States, 2020
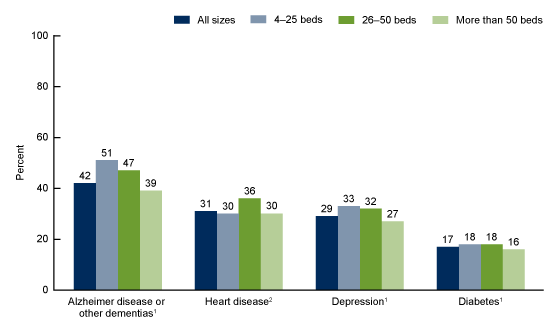
1Significantly decreasing linear trend by community size.
2Significant difference between communities with 26–50 beds and other community sizes (p < 0.05).
NOTES: Cases with missing data are excluded. The four diagnosed medical conditions each had 13% missing; see “Data source and methods” for details. Changes in question wording may have contributed to a difference in the estimates from earlier National Post-acute and Long-term Care Study surveys. Access data table for Figure 3.
SOURCE: National Center for Health Statistics, National Post-acute and Long-term Care Study, 2020
The percentage of residents needing assistance in bathing, dressing, toileting, transferring, walking, and eating was highest in communities with 4–25 beds.
- Among all residential care communities, 64% of residents needed assistance with bathing, which was the most frequent functional limitation among residents, and this percentage decreased with increasing community size. Of those in communities with 4–25 beds, 79% needed help with bathing compared with 60% of those in communities with more than 50 beds (Figure 4).
- The need for eating assistance decreased with increasing community size, from 38% of residents in communities with 4–25 beds to 17% of residents in communities with more than 50 beds.
- The need for assistance with walking, dressing, toileting, and transferring in or out of bed or a chair was higher for residents in communities with 4–25 beds compared with larger communities.
Figure 4. Need for assistance with selected activities of daily living among residential care residents,
by community size: United States, 2020
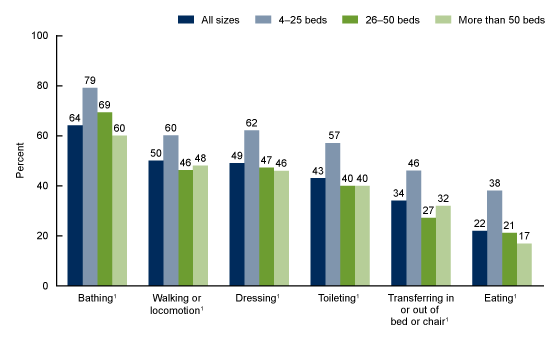
1Significantly decreasing linear trend by community size.
NOTES: Cases with missing data are excluded; see “Data source and methods” for details. Changes in question wording may have contributed to a difference in the estimates from earlier National Post-acute and Long-term Care Study surveys. Access data table for Figure 4.
SOURCE: National Center for Health Statistics, National Post-acute and Long-term Care Study, 2020
Summary
In 2020, the resident population living in residential care communities with 4–25 beds differed from the resident population living in larger residential care communities in a variety of sociodemographic, functional and health status, and service use characteristics.
Compared with residents in communities with 26 or more beds, a higher percentage of residents in 4–25 bed communities were Medicaid beneficiaries; living with Alzheimer disease or other dementias; and needing assistance with each of the six activities of daily living (ADLs) examined. Conversely, residents living in communities of 4–25 beds were less likely to be 85 years and over, non-Hispanic White, and female compared with residents in communities with 26 beds or more.
This report presents the most current national estimates of selected characteristics of residents in residential care communities and compares these characteristics by community size. This brief profile of residential care residents provides information to policy makers, providers, researchers, and consumer advocates as they plan how best to meet the needs of an aging population.
Definitions
Assistance with selected activities of daily living (ADLs): Refers to residents needing any help or supervision from another person, or use of assistive devices, with limitations in up to six ADLs (bathing; walking or locomotion—includes using a cane, walker, or wheelchair, or help from another person; dressing; transferring in and out of a bed or chair; toileting; and eating) that reflect a resident’s capacity for self-care.
Community size: Residents were grouped based on the number of licensed, registered, or certified residential care beds (both occupied and unoccupied) in their residential care community: 4–25 beds, 26–50 beds, and more than 50 beds.
Heart disease: Includes conditions such as congestive heart failure, coronary or ischemic heart disease, heart attack, and stroke.
Medicaid beneficiary: Refers to residents who had some or all their long-term care services paid by Medicaid during the 30 days before the survey.
Residential care communities: Includes assisted living communities and other residential care communities (for example, personal care homes, adult care homes, board care homes, or adult foster care) that meet the study eligibility criteria described in “Data source and methods.”
Data source and methods
Data for this report are from the Residential Care Community Survey component of the 2020 wave of the biennial National Post-acute and Long-term Care Study (NPALS), conducted by the National Center for Health Statistics. To be eligible for the study, a residential care community must (a) be regulated by the state to provide room and board with at least two meals a day, around-the-clock on-site supervision, and help with personal care such as bathing and dressing or with health-related services such as medication management; (b) have four or more licensed, certified, or registered beds; (c) have at least one resident currently living in the community at the time of the survey; and (d) serve a predominantly adult population. The survey used a combination of probability sampling and taking a census. More details about the NPALS design and outcomes are available elsewhere (1,2). The percentage of cases with missing data for variables in this report ranged from 1.2% for Medicaid to 11.3% for each of the four medical conditions: Alzheimer disease, depression, diabetes, and heart disease. These cases were excluded from the analyses on a variable-by-variable basis. If the percentage missing was higher than 10%, it is noted in the data. Missing values for race, ethnicity, sex, and age were imputed.
Data analyses were performed using the following statistical packages: SAS, Version 9.3 (SAS Institute, Cary, N.C.); SAS-callable SUDAAN, Version 11.0.0 (RTI International, Research Triangle Park, N.C., 2012); and STATA/SE, Version 17 (StataCorp, College Station, Tex., 2013). Statements of differences among subgroups are based on two-tailed chi-square and t tests with significance at the p < 0.05 level. If a chi-square test was statistically significant, a post hoc t test procedure was used to make pairwise comparisons among different community sizes. A weighted least-squares regression method was used to test the significance of linear trends in bed size.
About the authors
Christine Caffrey, Amanuel Melekin, Zhaohui Lu, and Manisha Sengupta are with the National Center for Health Statistics, Division of Health Care Statistics.
References
- National Center for Health Statistics. 2020 National Post-acute and Long-term Care Study survey methodology for the Adult Day Services Center and Residential Care Community components. 2022.
- National Center for Health Statistics. 2020 National Post-acute and Long-term Care Study (formerly called the National Study of Long-term Care Providers) Residential Care Community (RCC) Restricted Data File: Data description and usage. 2022.
Suggested citation
Caffrey C, Melekin A, Lu Z, Sengupta M. Variation in residential care community resident characteristics, by size of community: United States, 2020. NCHS Data Brief, no 454. Hyattsville, MD: National Center for Health Statistics. 2022. DOI: https://dx.doi.org/10.15620/cdc:121910.
Copyright information
All material appearing in this report is in the public domain and may be reproduced or copied without permission; citation as to source, however, is appreciated.
National Center for Health Statistics
Brian C. Moyer, Ph.D., Director
Amy M. Branum, Ph.D., Associate Director for Science
Division of Health Care Statistics
Carol J. DeFrances, Ph.D., Acting Director
Alexander Strashny, Ph.D., Associate Director for Science