Facts about Tricuspid Atresia
Tricuspid atresia (pronounced try-CUSP-id uh-TREE-zhuh) is a birth defect of the heart where the valve that controls blood flow from the right upper chamber of the heart to the right lower chamber of the heart doesn’t form at all. In babies with this defect, blood can’t flow correctly through the heart and to the rest of the body.
What is Tricuspid Atresia?
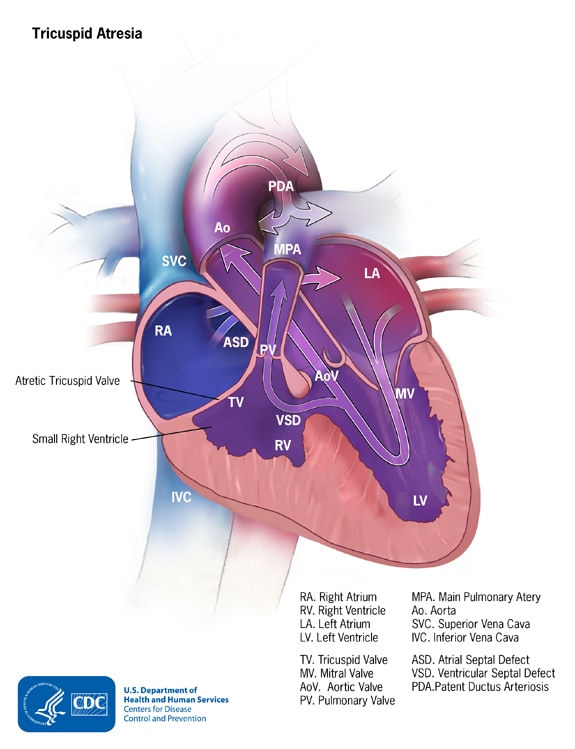
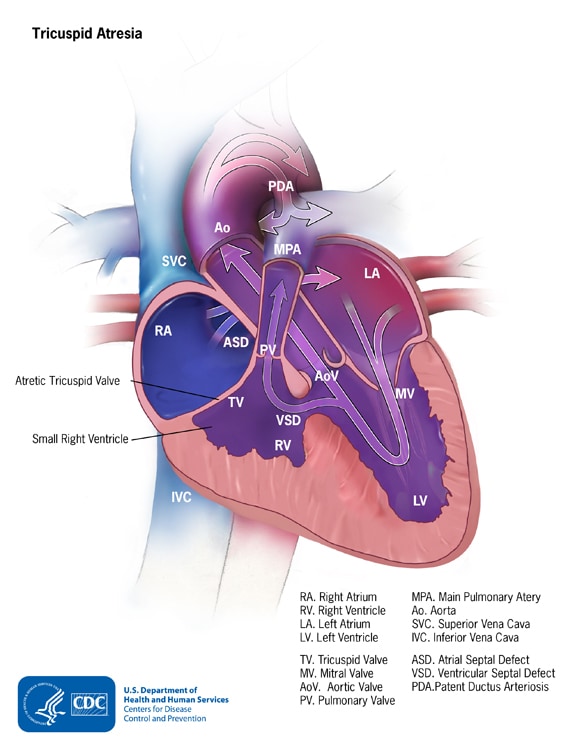
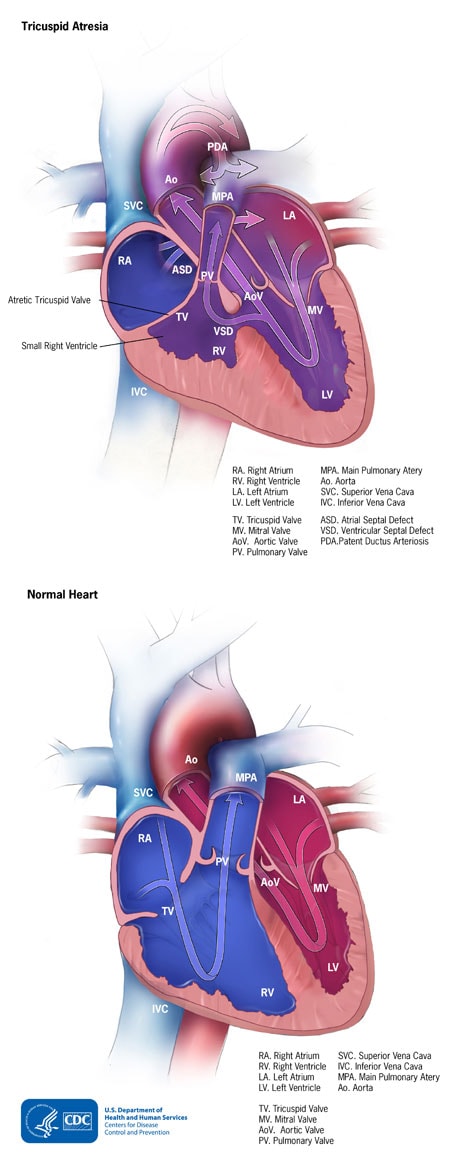
Tricuspid atresia is a birth defect of the tricuspid valve, which is the valve that controls blood flow from the right atrium (upper right chamber of the heart) to the right ventricle (lower right chamber of the heart). Tricuspid atresia occurs when this valve doesn’t form at all, and no blood can go from the right atrium through the right ventricle to the lungs for oxygen. Because a baby with tricuspid atresia may need surgery or other procedures soon after birth, this birth defect is considered a critical congenital heart defect. Congenital means present at birth.
In a baby without a congenital heart defect, the right side of the heart pumps oxygen-poor blood from the heart to the lungs through the main pulmonary artery. The blood that comes back from the lungs is oxygen-rich and can then be pumped to the rest of the body through the aorta. In babies with tricuspid atresia, the tricuspid valve that controls blood flow from the right atrium to the right ventricle is not formed, so blood is unable to get to the right ventricle and out to the lungs. For this reason, the right ventricle can be underdeveloped. The main pulmonary artery may also be small with very little blood going through it to the lungs.
In tricuspid atresia, since blood cannot directly flow from the right atrium to the right ventricle, blood must use other routes to bypass the unformed tricuspid valve. Babies born with tricuspid atresia often also have an atrial septal defect, which is a hole between the right and left atria, or a ventricular septal defect, which is a hole between the right and left ventricles. These defects allow oxygen-rich blood to mix with oxygen-poor blood, so that oxygen-rich blood has a way to get pumped to the rest of the body.
Doctors may give the baby medicine to keep the baby’s patent ductus arteriosus (PDA in the image) open after the baby’s birth. The PDA is the blood vessel that allows blood to move around the baby’s lungs before the baby is born, and it usually closes after birth. Keeping this connection open allows blood to get to the lungs for oxygen and bypass the small right side of the heart.
Some babies with tricuspid atresia can also have other heart defects, including transposition of the great arteries (TGA). In TGA, the main connections (arteries) from the heart are reversed. The main pulmonary artery, which normally carries oxygen-poor blood from the right side of the heart to the lungs, now arises from the left side and carries oxygen-rich blood returning from the lungs back to the lungs. The aorta, which normally carries blood from the left side of the heart to the body, now arises from the right side and carries oxygen-poor blood back out to the body. When a baby has both tricuspid atresia and TGA, blood is able to get to the lungs because the main pulmonary artery arises from the developed left ventricle. However, blood cannot get out to the body because the aorta arises from the poorly formed right ventricle and is small.
Learn more about how the heart works »
Occurrence
In a 2019 study using data from birth defects tracking systems across the United States, researchers estimated that each year about 404 babies in the United States are born with tricuspid atresia. In other words, about 1 in every 9,751 babies born in the United States each year are born with tricuspid atresia.1
Causes and Risk Factors
The causes of heart defects, such as tricuspid atresia, among most babies are unknown. Some babies have heart defects because of changes in their genes or chromosomes. Heart defects also are thought to be caused by a combination of genes and other factors, such as the things the mother comes in contact with in the environment, or what the mother eats or drinks, or certain medicines she uses.
Read more about CDC’s work on causes and risk factors for birth defects
Diagnosis
Tricuspid atresia may be diagnosed during pregnancy or soon after a baby is born.
During Pregnancy
During pregnancy, there are screening tests (also called prenatal tests) to check for birth defects and other conditions. Tricuspid atresia might be seen during an ultrasound (which creates pictures of the body). Some findings from the ultrasound may make the health care provider suspect that a baby might have tricuspid atresia. If so, the health care provider can request a fetal echocardiogram to confirm the diagnosis. A fetal echocardiogram is an ultrasound specifically of the baby’s heart and major blood vessels that is performed during the pregnancy. This test can show problems with the structure of the heart and how the heart is working with this defect.
After a Baby is Born
Babies born with tricuspid atresia will show symptoms at birth or very soon afterwards. They may have a bluish looking skin color, called cyanosis, because their blood doesn’t carry enough oxygen. Infants with tricuspid atresia can have additional symptoms such as:
- Problems breathing
- Ashen or bluish skin color
- Poor feeding
- Extreme sleepiness
During a physical examination, a doctor can see the symptoms, such as bluish skin or problems breathing. Using a stethoscope, a doctor will check for a heart murmur (an abnormal “whooshing” sound caused by blood not flowing properly), or other sounds that may indicate a heart problem. However, it is not uncommon for a heart murmur to be absent right at birth.
If a doctor suspects that there might be a problem, the doctor can request one or more tests to confirm the diagnosis of tricuspid atresia. The most common test is an echocardiogram. This is an ultrasound of the heart that can show problems with the structure of the heart, like holes in the walls between the chambers, and any irregular blood flow. Cardiac catheterization (inserting a thin tube into a blood vessel and guiding it to the heart) also can confirm the diagnosis by looking at the inside of the heart and measuring the blood pressure and oxygen. An electrocardiogram (EKG), which measures the electrical activity of the heart, and other medical tests may also be used to make the diagnosis.
Tricuspid atresia is a critical congenital heart defect (critical CHD) that also can be detected with newborn screening using pulse oximetry (also known as pulse ox). Pulse oximetry is a simple, painless bedside test to estimate the amount of oxygen in a baby’s blood. The test is done using a machine called a pulse oximeter, with sensors placed on the baby’s skin. Low levels of oxygen in the blood can be a sign of a critical CHD. Newborn screening using pulse oximetry can identify some infants with a critical CHD, like tricuspid atresia, before they show any symptoms.
Treatment
Medicines
Some babies and children will need medicines to help strengthen the heart muscle, lower their blood pressure, and help the body get rid of extra fluid.
Nutrition
Some babies with tricuspid atresia become tired while feeding and do not eat enough to gain weight. To make sure babies have a healthy weight gain, a special high-calorie formula might be prescribed. Some babies become extremely tired while feeding and might need to be fed through a feeding tube.
Surgery
Surgical treatment for tricuspid atresia depends on its severity and presence of other heart defects. Soon after a baby with tricuspid atresia is born, one or more surgeries may be needed to increase blood flow to the lungs and bypass the poorly functioning right side of the heart. Other surgeries or procedures may be needed later. These surgeries, described below, do not cure tricuspid atresia, but they help restore heart function. Sometimes medicines are given to help treat symptoms of the defect before or after surgery.
- Septostomy
A septostomy may be done within the first few days or weeks of a baby’s life, and creates or enlarges the atrial septal defect, the hole between the right and left upper chambers (atria). This is done so that more oxygen-poor blood can mix with oxygen-rich blood, so that more oxygen-rich blood can get to the body.
- Banding
If the baby has other heart defects along with tricuspid atresia, sometimes there is too much blood flowing to the lungs and not enough going out to the rest of the body. Too much blood in the lungs can damage them. If this is the problem, surgery may be done within the first few weeks of a baby’s life to place a band around the artery going to the lungs (main pulmonary artery) to control the blood flow to the lungs. This banding is a temporary procedure and will likely be removed.
- Shunt Procedure
This surgery usually is done within the first 2 weeks of a baby’s life. Surgeons create a bypass (shunt) from the aorta to the main pulmonary artery, allowing blood to get to the lungs. If the aorta is small, as occurs when the baby also has transposition of the great arteries, the surgeon will also enlarge the aorta at this time. After this procedure, an infant’s skin still might look bluish because oxygen-rich and oxygen-poor blood still mix in the heart.
- Bi-directional Glenn Procedure
This usually is performed when an infant is 4 to 6 months of age. This procedure creates a direct connection between the main pulmonary artery and the superior vena cava, the vessel returning oxygen-poor blood from the upper part of the body to the heart. This allows blood returning from the body to flow directly to the lungs and bypass the heart.
- Fontan Procedure
This procedure usually is done sometime around 2 years of age. Doctors connect the main pulmonary artery and the inferior vena cava, the vessel returning oxygen-poor blood from the lower part of the body to the heart, allowing the rest of the blood coming back from the body to go to the lungs. Once this procedure is complete, oxygen-rich and oxygen-poor blood no longer mix in the heart and an infant’s skin will no longer look bluish.
Infants who have these surgeries are not cured; they might have lifelong complications. If the tricuspid atresia is very complex, or the heart becomes weak after the surgeries, a heart transplant might be needed. An infant or child who receives a heart transplant will need to take medicines for the rest of his or her life to prevent the body from rejecting the new heart.
Babies born with tricuspid atresia will need regular follow-up visits with a cardiologist (a heart doctor) to monitor their progress and check for other health conditions that might develop as they get older. As adults, they may need more surgery or medical care for other possible problems.