Facts about Tetralogy of Fallot
Tetralogy of Fallot (pronounced te-tral-uh-jee of Fal-oh) is a birth defect that affects normal blood flow through the heart. It happens when a baby’s heart does not form correctly as the baby grows and develops in the mother’s womb during pregnancy.
What is Tetralogy of Fallot?
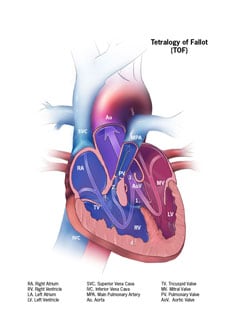
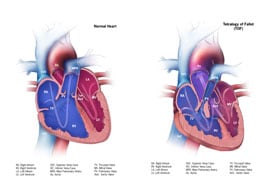
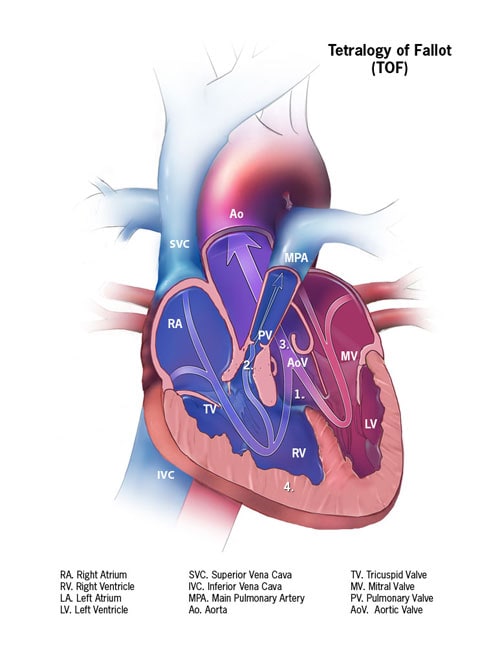
Tetralogy of Fallot is made up of the following four defects of the heart and its blood vessels:
- A hole in the wall between the two lower chambers―or ventricles―of the heart. This condition also is called a ventricular septal defect.
- A narrowing of the pulmonary valve and main pulmonary artery. This condition also is called pulmonary stenosis.
- The aortic valve, which opens to the aorta, is enlarged and seems to open from both ventricles, rather than from the left ventricle only, as in a normal heart. In this defect, the aortic valve sits directly on top of the ventricular septal defect.
- The muscular wall of the lower right chamber of the heart (right ventricle) is thicker than normal. This also is called ventricular hypertrophy.
Because a baby with tetralogy of Fallot may need surgery or other procedures soon after birth, this birth defect is considered a critical congenital heart defect. Congenital means present at birth.
This heart defect can cause oxygen in the blood that flows to the rest of the body to be reduced. Infants with tetralogy of Fallot can have a bluish-looking skin color―called cyanosis―because their blood doesn’t carry enough oxygen. At birth, infants might not have blue-looking skin, but later might develop sudden episodes of bluish skin during crying or feeding. These episodes are called tet spells.
Infants with tetralogy of Fallot or other conditions causing cyanosis can have problems including:
- A higher risk of getting an infection of the layers of the heart, called endocarditis.
- A higher risk of having irregular heart rhythms, called arrhythmia.
- Dizziness, fainting, or seizures, because of the low oxygen levels in their blood.
- Delayed growth and development.
Learn more about how the heart works »
Occurrence
The Centers for Disease Control and Prevention (CDC) estimates that each year about 1,660 babies in the United States are born with tetralogy of Fallot.1 In other words, about 1 in every 2518 babies born in the United States each year are born with tetratology of Fallot.
Causes and Risk Factors
The causes of heart defects (such as tetralogy of Fallot) among most babies are unknown. Some babies have heart defects because of changes in their genes or chromosomes. Heart defects such as tetralogy of Fallot also are thought to be caused by a combination of genes and other risk factors, such as the things the mother or fetus come in contact with in the environment or what the mother eats or drinks or the medicines she uses.
Read more about CDC’s work on causes and risk factors »
Diagnosis
Tetralogy of Fallot may be diagnosed during pregnancy or soon after a baby is born.
During Pregnancy
During pregnancy, there are screening tests (also called prenatal tests) to check for birth defects and other conditions. Tetralogy of Fallot might be seen during an ultrasound (which creates pictures of the body). Some findings from the ultrasound may make the health care provider suspect a baby may have tetralogy of Fallot. If so, the health care provider can request a fetal echocardiogram to confirm the diagnosis. A fetal echocardiogram is an ultrasound of the heart of the fetus. This test can show problems with the structure of the heart and how the heart is working with this defect.
After a Baby Is Born
Tetralogy of Fallot usually is diagnosed after a baby is born, often after the infant has an episode of turning blue during crying or feeding (a tet spell). Some findings on a physical exam may make the health care provider think a baby may have tetralogy of Fallot, including bluish-looking skin or a heart murmur (a “whooshing” sound caused by blood not flowing properly through the heart). However, it is not uncommon for a heart murmur to be absent right at birth.
The health care provider can request one or more tests to confirm the diagnosis. The most common test is an echocardiogram. An echocardiogram is an ultrasound of the heart that can show problems with the structure of the heart and how the heart is working (or not) with this defect. Echocardiography also is useful for helping the doctor follow the child’s health over time.
Tetralogy of Fallot is a critical congenital heart defect (critical CHD) that may be detected with newborn screening using pulse oximetry (also known as pulse ox). Pulse oximetry is a simple bedside test to estimate the amount of oxygen in a baby’s blood. Low levels of oxygen in the blood can be a sign of a critical CHD. Newborn screening using pulse oximetry can identify some infants with a critical CHD, like tetralogy of Fallot, before they show any symptoms.
Treatments
Tetralogy of Fallot can be treated by surgery soon after the baby is born. During surgery, doctors widen or replace the pulmonary valve and enlarge the passage to the pulmonary artery. They also will place a patch over the ventricular septal defect to close the hole between the two lower chambers of the heart. These actions will improve blood flow to the lungs and the rest of the body.
Most infants will live active, healthy lives after surgery. However, they will need regular follow-up visits with a cardiologist (a heart doctor) to monitor their progress and check for other health conditions that might develop as they get older. As adults, they may need more surgery or medical care for other possible problems.
Learn more about living with a CHD »
References
- Parker SE, Mai CT, Canfield MA, et al; for the National Birth Defects Prevention Network. Updated national birth prevalence estimates for selected birth defects in the United States, 2004-2006. Birth Defects Res A Clin Mol Teratol. 2010;88:1008-16.