Facts about Hypospadias
Hypospadias (pronounced hype-oh-spay-dee-us) is a birth defect in boys where the opening of the urethra (the tube that carries urine from the bladder to the outside of the body) is not located at the tip of the penis.
What is Hypospadias?
Hypospadias is a birth defect in boys in which the opening of the urethra is not located at the tip of the penis. In boys with hypospadias, the urethra forms abnormally during weeks 8–14 of pregnancy. The abnormal opening can form anywhere from just below the end of the penis to the scrotum. There are different degrees of hypospadias; some can be minor and some more severe.
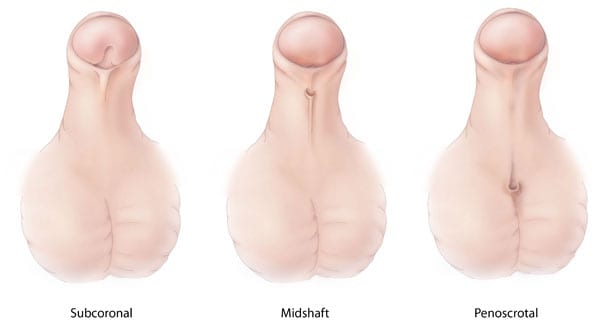
Types of Hypospadias
The type of hypospadias a boy has depends on the location of the opening of the urethra:
- Subcoronal: The opening of the urethra is located somewhere near the head of the penis.
- Midshaft: The opening of the urethra is located along the shaft of the penis.
- Penoscrotal: The opening of the urethra is located where the penis and scrotum meet.
Other Problems
Boys with hypospadias can sometimes have a curved penis. They could have problems with abnormal spraying of urine and might have to sit to urinate. In some boys with hypospadias, the testicle has not fully descended into the scrotum. If hypospadias is not treated it can lead to problems later in life, such as difficulty performing sexual intercourse or difficulty urinating while standing.
How Many Babies are Born with Hypospadias?
Researchers estimate that about 1 in every 200 babies is born with hypospadias in the United States,1,2 making it one of the most common birth defects.
Causes and Risk Factors
The causes of hypospadias in most infants are unknown. In most cases, hypospadias is thought to be caused by a combination of genes and other factors, such as things the mother comes in contact with in her environment, or what the mother eats or drinks, or certain medications she uses during pregnancy.
Just like the many families affected by birth defects, CDC wants to find out what causes them. Understanding the risk factors that are more common among babies with birth defects will help us learn more about the causes. CDC funds the Centers for Birth Defects Research and Prevention, which collaborate on large studies such as the National Birth Defects Prevention Study (NBDPS; births 1997-2011) and the Birth Defects Study to Evaluate Pregnancy exposureS (BD-STEPS; began with births in 2014), to understand the causes of and risks for birth defects, like hypospadias.
In recent years, CDC researchers have reported important findings about some factors that affect the risk of having a baby boy with hypospadias:
- Age and weight: Mothers who were age 35 years or older and who were considered obese had a higher risk of having a baby with hypospadias.3
- Fertility treatments: Women who used assisted reproductive technology to help with pregnancy had a higher risk of having a baby with hypospadias.4
- Certain hormones: Women who took certain hormones just before or during pregnancy were shown to have a higher risk of having a baby with hypospadias.5
CDC continues to study birth defects like hypospadias and how to prevent them. If you are pregnant or thinking about becoming pregnant, talk with your doctor about ways to increase your chance of having a healthy baby.
Diagnosis
Hypospadias is usually diagnosed during a physical examination after the baby is born.
Treatments
Treatment for hypospadias depends on the type of defect the boy has. Most cases of hypospadias will need surgery to correct the defect.
If surgery is needed, it is usually done when the boy is between the ages of 3–18 months old. In some cases the surgery is done in stages. Some of the repairs done during the surgery might include placing the opening of the urethra in the right place, correcting the curve in the penis, and repairing the skin around the opening of the urethra. Because the doctor might need to use the foreskin to make some of the repairs, a baby boy with hypospadias should not be circumcised.
Other Resources
The views of this organization are its own and do not reflect the official position of CDC.
- Hypospadias and Epispadias Association (HEA)
HEA offers support and education of people born with hypospadias or epispadias and their families, loved ones, and medical care givers.
References
- Paulozzi LJ, Erickson JD, Jackson RJ. Hypospadias trends in two US surveillance systems. Pediatrics 1997; 100:831–834.
- Mai CT, Isenberg J, Langlois PH, Alverson CJ, Gilboa SM, Rickard R, Canfield M, Anjohrin SB, Lupo PJ, Jackson DR, Stallings EB, Scheuerle AE, Kirby RS for the National Birth Defects Prevention Network. Brief report, Population-based birth defects data in the United States, 2008 to 2012: Presentation of state-specific data and descriptive brief on variability of prevalence. Birth Def Res (Part A). 2015; 103:972-994.
- Carmichael SL, Shaw GM, Laurent C, Olney RS, Lammer EJ, and the National Birth Defects Prevention Study. Maternal reproductive and demographic characteristics as risk factors for hypospadias. Paediatr Perinat Epidemiol. 2007; 21: 210–218.
- Reefhuis J, Honein MA, Schieve LA, Correa A, Hobbs CA, Rasmussen SA, and the National Birth Defects Prevention Study. Assisted reproductive technology and major structural birth defects in the United States. Human Rep. 2009; 24:360–366
- Carmichael SL, Shaw GM, Laurent C, Croughan MS, Olney RS, Lammer EJ. Maternal progestin intake and risk of hypospadias. Arch Pediatr Adolesc Med. 2005;159: 957–962