2015 Waterborne Disease Outbreaks Annual Surveillance Report
82
1,276
185
27
More than half of reported waterborne disease outbreaks were linked to recreational water in 2015
Legionella caused nearly half of reported waterborne disease outbreaks and more than 90% of hospitalizations and deaths
- Legionella (43%)
- Cryptosporidium (28%)
- Giardia (5%)
- Norovirus (5%)
- Pseudomonas (4%)
18% of reported cases
94% of hospitalizations
100% of deaths
Background
Each year, pathogens transmitted through water are estimated to cause 7.15 million cases of waterborne illness (95% credible interval [CrI], 3.9–12.0 million), 118,000 hospitalizations (95% CrI, 86,800–150,000) and 6,630 deaths (95% CrI, 4,520–8,870) in the United States (1). Summaries of waterborne disease outbreak data can inform prevention efforts for infectious and non-infectious etiologies.
Methods
For an event to be defined as a waterborne disease outbreak, two or more cases of similar illness must be epidemiologically linked by location and time of exposure to contaminated water, contaminated aerosols, or gases volatilized from water. Cases are defined as lab-confirmed or probable using outbreak-specific case definitions. The epidemiologic evidence must implicate water exposure as the outbreak source and can be strengthened by environmental health and laboratory data.
CDC has conducted national surveillance for waterborne disease outbreaks since 1971 via the Waterborne Disease and Outbreak Surveillance System (WBDOSS). Public health officials in U.S. jurisdictions (the 50 states, the District of Columbia, territories, and freely associated states) have voluntarily reported waterborne disease outbreaks through the web-based platform, National Outbreak Reporting System (NORS) since 2009. WBDOSS has captured data regarding outbreaks associated with recreational water, drinking water, and other or unknown types of exposures to water. Water from an identified source other than a recreational venue or drinking water system is referred to as “other water” (e.g., industrial water, flood waters). An outbreak with insufficient data to link the outbreak to one specific source is reported as an unknown water exposure. Individual outbreaks associated with multiple types of water exposures are also reported as unknown.
Agencies use a standard form [PDF – 12 pages] to report waterborne disease outbreaks. Data collected include the implicated outbreak water exposure (recreational, drinking, other, or unknown water); earliest illness onset date; etiology; implicated recreational water venue or drinking water system; the setting of exposure (e.g., a hotel, apartment complex, hospital); relevant epidemiologic data; and contributing factors. NORS data are available for download and visualization using the NORS Dashboard, a web-based tool for searching and accessing outbreak data.
This summary includes waterborne disease outbreaks reported through NORS as of March 23, 2022, and for which the earliest illness onset was in 2015. Outbreak reports went through a standardized data cleaning process, a collaboration between CDC and reporting jurisdictions. Agencies can submit new outbreak reports and revise or delete reports as additional data become available. Thus, data reported in future analyses for 2015 might differ from the numbers presented here.
Findings
All Water Exposures
During 2015, 82 waterborne disease outbreaks were reported, resulting in at least 1,276 cases, 185 hospitalizations, and 27 deaths (Table 1). Recreational water was implicated in investigations of over half of outbreaks (57%, 47/82), resulting in nearly two-thirds of cases (62%, 787/1,276). Drinking water was implicated in investigations of about one-quarter of outbreaks (28%, 23/82), resulting in about one-third of cases (34%, 429/1,276) and most hospitalizations (67%, 124/185) and deaths (93%, 25/27). Other exposure to water was implicated for 7% (6/82) of outbreaks, resulting in 4% (47/1,276) of cases. In 7% of outbreaks (resulting in 1% of cases) the water outbreak source was unknown.
| Outbreak Exposure | Outbreaks N (%) | Cases N (%) | Hospitalizations N (%) | Deaths N (%) |
|---|---|---|---|---|
| Recreational water | 47 (57%) | 787 (62%) | 23 (12%) | 1 (4%) |
| Drinking water | 23 (28%) | 429 (34%) | 124 (67%) | 25 (93%) |
| Other water§ | 6 (7%) | 47 (4%) | 27 (15%) | 1 (4%) |
| Unknown water | 6 (7%) | 13 (1%) | 11 (6%) | 0 (0%) |
| Total | 82 (100%) | 1,276 (100%) | 185 (100%) | 27 (100%) |
* Percentages might not sum to 100 due to rounding.
§ Water from an identified source other than a recreational venue or drinking water system is referred to as “other water” (e.g., industrial water, flood waters).
For 2015, public health officials reported 82 waterborne outbreaks resulting from exposures in 32 states. (Figure 1). No outbreaks involving multi-state exposures were reported.
Outbreaks most frequently occurred June–August (51%, 42/82) (Figure 2).
Bacteria were implicated in 54% (44/82) of outbreaks with a confirmed or suspected etiology; parasites were implicated in 35% (29/82) of outbreaks (Figure 3).
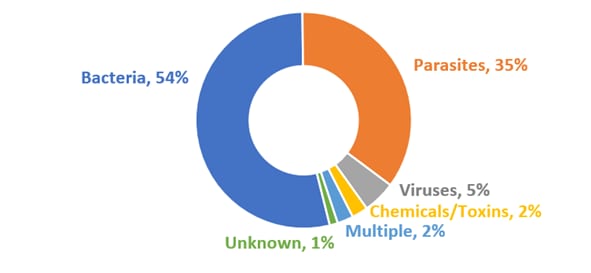
* Percentages do not sum to 100 due to rounding.
§ Outbreaks of confirmed or suspected etiologies are summarized together. Multiple etiology outbreaks include one outbreak suspected to be caused by Shigella sonnei, Campylobacter jejuni, and norovirus; and one outbreak caused by Campylobacter jejuni and suspected to be caused by Giardia duodenalis.
| Etiology Type | n | % |
|---|---|---|
| Bacteria | 44 | 54 |
| Parasites | 29 | 35 |
| Viruses | 4 | 5 |
| Chemicals/Toxins | 2 | 2 |
| Multiple§ | 2 | 2 |
| Unknown | 1 | 1 |
At least one etiology was confirmed in 85% (70/82) of investigations of outbreaks (Table 2). Among outbreaks with a confirmed or suspected etiology, Legionella was most frequently reported, accounting for 43% (35/82) of outbreaks. This was followed by Cryptosporidium, which accounted for 28% (23/82) of outbreaks. Cryptosporidium caused 28% (362/1,276) of cases among outbreaks, followed by norovirus (21% [263]) and Legionella (18% [234]). Legionella accounted for 94% (174/185) of hospitalizations and all 27 deaths.
| Etiology | Outbreaks | Cases | Hospitalizations | Deaths | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| n | % | Confirmed | Suspected | n | % | Confirmed | Suspected | n | % | Confirmed | Suspected | n | % | Confirmed | Suspected | |
| Legionella | 35 | 43 | 33 | 2 | 234 | 18 | 224 | 10 | 174 | 94 | 164 | 10 | 27 | 100 | 26 | 1 |
| Cryptosporidium | 23 | 28 | 22 | 1 | 362 | 28 | 355 | 7 | 6 | 3 | 6 | 0 | 0 | 0 | 0 | 0 |
| Giardia | 4 | 5 | 4 | 0 | 14 | 1 | 14 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Norovirus | 4 | 5 | 4 | 0 | 263 | 21 | 263 | 0 | 1 | 1 | 1 | 0 | 0 | 0 | 0 | 0 |
| Pseudomonas | 3 | 4 | 1 | 2 | 22 | 2 | 13 | 9 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Chemicals/Toxins¶ | 2 | 2 | 0 | 2 | 51 | 4 | 0 | 51 | 1 | 1 | 0 | 1 | 0 | 0 | 0 | 0 |
| Escherichia | 2 | 2 | 2 | 0 | 15 | 1 | 15 | 0 | 2 | 1 | 2 | 0 | 0 | 0 | 0 | 0 |
| Mycobacterium | 2 | 2 | 1 | 1 | 13 | 1 | 9 | 4 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Acanthamoeba | 1 | 1 | 1 | 0 | 2 | 0 | 2 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Avian schistosomes | 1 | 1 | 0 | 1 | 22 | 2 | 0 | 22 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Campylobacter | 1 | 1 | 1 | 0 | 4 | 0 | 4 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Salmonella | 1 | 1 | 0 | 1 | 3 | 0 | 0 | 3 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Multiple† | 2 | 2 | 1 | 1 | 259 | 20 | 9 | 250 | 1 | 1 | 1 | 0 | 0 | 0 | 0 | 0 |
| Unknown ‡ | 1 | 1 | — | — | 12 | 1 | — | — | 0 | 0 | — | — | 0 | 0 | — | — |
* Confirmed and suspected totals might not sum to outbreak, case, or hospitalization count due to exclusion of unknown etiologies.
§ Percentages might not sum to 100 due to rounding.
¶ Chemical/toxin exposures include suspected chlorine and chloramine exposures.
† Multiple etiology outbreaks include one outbreak suspected to be caused by Shigella, Campylobacter, and norovirus and one outbreak caused by Campylobacter and suspected to be caused by Giardia.
‡ Outbreaks of unknown etiology cannot be classified according to confirmed or suspected etiology for outbreak, cases, hospitalizations, or deaths. In 2015, there was one reported outbreak with an unknown etiology.
The most frequently reported outbreak settings were hotels or motels (22%, 18/82 outbreaks), outdoor recreational areas (10%, 8/82), hospitals or healthcare facilities (9%, 7/82), and communities or municipalities (7%, 6/82) (Table 3).
| Water Setting | Outbreaks n (%) | Cases n (%) |
|---|---|---|
| Hotel/Motel | 18 (22%) | 165 (13%) |
| Outdoor Recreational Area | 8 (10%) | 265 (21%) |
| Hospital/Healthcare Facility§ | 7 (9%) | 65 (5%) |
| Community/Municipality¶ | 6 (7%) | 283 (22%) |
| Long Term Care Facility/Assisted Living | 5 (6%) | 78 (6%) |
| Camp/Cabin | 4 (5%) | 108 (8%) |
| Private Residence | 4 (5%) | 19 (1%) |
| Recreational Facility | 3 (4%) | 45 (4%) |
| Waterpark | 3 (4%) | 61 (5%) |
| Beach | 2 (2%) | 18 (1%) |
| Club (Requires Membership) | 2 (2%) | 16 (1%) |
| Resort | 2 (2%) | 12 (1%) |
| Multiple† | 4 (5%) | 20 (2%) |
| Other‡ | 7 (9%) | 45 (4%) |
| Not Reported | 4 (5%) | 21 (2%) |
| Unknown | 3 (4%) | 55 (4%) |
| Total | 82 (100%) | 1,276 (100%) |
* Percentages might not sum to 100 due to rounding.
§ A healthcare institution providing inpatient medical or surgical treatment or nursing care for sick or injured persons, or a healthcare facility other than a long-term care or assisted-living facility.
¶ Includes recreational water facilities owned by a community/municipality.
† Multiple setting includes: waterpark and child care/daycare center (1), hotel/motel and resort (1), outdoor recreational area and school/college/university (1), and multiple private residences (1).
‡ Other setting includes: amusement park (1), casino (1), church/place of worship (1), factory/industrial facility (1), farm/agricultural setting (1), indoor workplace/office (1), and restaurant/cafeteria (1).
Recreational Water Exposures
Recreational water was the most frequently reported source of waterborne disease outbreaks, associated with 57% (47/82) of outbreaks, resulting in 62% (787/1,276) of reported cases (Table 1). Recreational water–associated outbreaks occurred year round but peaked during June–August (Figure 4). The seasonality of recreational water–associated outbreaks drove the seasonality of waterborne disease outbreaks overall.
Among recreational water outbreaks, 47% (22/47) were caused by Cryptosporidium and 19% (9/47) by Legionella (Table 4). Among 787 reported cases resulting from recreational water exposure and with a confirmed or suspected etiology, 46% (360/787) of cases were caused by Cryptosporidium and 33% (263/787) caused by norovirus. Over three quarters of 23 hospitalizations in those affected by recreational water–associated outbreaks were caused by Legionella (57%, 13/23) or Cryptosporidium (26%, 6/23). One death was reported for the 47 recreational water–associated outbreaks.
| Outbreaks | Cases | Hospitalizations | Deaths | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Etiology | n (%) | Confirmed | Suspected | n (%) | Confirmed | Suspected | n (%) | Confirmed | Suspected | n (%) | Confirmed | Suspected |
| Cryptosporidium | 22 (47%) | 21 | 1 | 360 (46%) | 353 | 7 | 6 (26%) | 6 | 0 | 0 (0%) | 0 | 0 |
| Legionella | 9 (20%) | 9 | 0 | 30 (4%) | 30 | 0 | 13 (57%) | 13 | 0 | 1 (100%) | 1 | 0 |
| Norovirus | 4 (9%) | 4 | 0 | 263 (33%) | 263 | 0 | 1 (4%) | 1 | 0 | 0 (0%) | 0 | 0 |
| Pseudomonas | 3 (6%) | 1 | 2 | 22 (3%) | 13 | 9 | 0 (0%) | 0 | 0 | 0 (0%) | 0 | 0 |
| Chemicals/Toxins¶ | 2 (4%) | 0 | 2 | 51 (7%) | 0 | 51 | 1 (4%) | 0 | 1 | 0 (0%) | 0 | 0 |
| Acanthamoeba | 1 (2%) | 1 | 0 | 2 (0%) | 2 | 0 | 0 (0%) | 0 | 0 | 0 (0%) | 0 | 0 |
| Avian schistosomes | 1 (2%) | 0 | 1 | 22 (3%) | 0 | 22 | 0 (0%) | 0 | 0 | 0 (0%) | 0 | 0 |
| Campylobacter | 1 (2%) | 1 | 0 | 4 (1%) | 4 | 0 | 0 (0%) | 0 | 0 | 0 (0%) | 0 | 0 |
| Escherichia | 1 (2%) | 1 | 0 | 9 (1%) | 9 | 0 | 2 (9%) | 2 | 0 | 0 (0%) | 0 | 0 |
| Giardia | 1 (2%) | 1 | 0 | 3 (0%) | 3 | 0 | 0 (0%) | 0 | 0 | 0 (0%) | 0 | 0 |
| Mycobacterium | 1 (2%) | 1 | 0 | 9 (1%) | 9 | 0 | 0 (0%) | 0 | 0 | 0 (0%) | 0 | 0 |
| Unknown† | 1 (2%) | — | — | 12 (2%) | — | — | 0 (0%) | — | — | 0 (0%) | — | — |
* Confirmed and suspected totals might not sum to outbreak, case, or hospitalization count due to exclusion of unknown etiologies.
§ Percentages might not sum to 100 due to rounding.
¶ Chemical/toxin exposures include suspected chlorine and chloramine exposures.
† Outbreaks of unknown etiology cannot be classified according to confirmed or suspected etiology for outbreak, cases, hospitalizations, or deaths. In 2015, there was one reported outbreak with an unknown etiology.
Recreational water–associated outbreaks were most frequently associated with recreational water venues at hotels or motels (26%, 12/47), outdoor recreational areas (13%, 6/47), or communities or municipalities (11%, 5/47) (Table 5).
| Water Setting | Outbreaks n (%) | Cases n (%) |
|---|---|---|
| Hotel/Motel | 12 (26%) | 150 (19%) |
| Outdoor Recreational Area | 6 (13%) | 258 (33%) |
| Community/Municipality§ | 5 (11%) | 33 (4%) |
| Camp/Cabin | 3 (6%) | 104 (13%) |
| Recreational Facility | 3 (6%) | 45 (6%) |
| Waterpark | 3 (6%) | 61 (8%) |
| Beach | 2 (4%) | 18 (2%) |
| Club (Requires Membership) | 2 (4%) | 16 (2%) |
| Private Residence | 2 (4%) | 13 (2%) |
| Resort | 2 (4%) | 12 (2%) |
| Amusement Park | 1 (2%) | 7 (1%) |
| Multiple¶ | 1 (2%) | 7 (1%) |
| Not Reported | 3 (6%) | 18 (2%) |
| Unknown | 2 (4%) | 45 (6%) |
| Total | 47 (100%) | 787 (100%) |
* Percentages do not sum to 100 due to rounding.
§ A recreational water facility owned by a community/municipality.
¶ Multiple setting includes: a waterpark and child care/daycare center.
Treated water (e.g., in pools, hot tubs, or splash pads) was associated with 85% (40/47) of these outbreaks, resulting in 62% (490/787) of cases; untreated recreational water was associated with 15% (7/47) of outbreaks, resulting in 38% (297/787) of cases (Table 6–7). Among the 40 treated recreational water–associated outbreaks, 45% (18/40) were associated with pools. Eight (20%, 8/40) outbreaks were associated with multiple venue types (Table 6). Nearly all untreated recreational water outbreak venues were associated with a lake or reservoir (86%, 6/7); the remaining outbreak was associated with a river or stream (Table 7).
| Venue | Outbreaks n (%) | Cases n (%) |
|---|---|---|
| Pool | 18 (45%) | 286 (58%) |
| Hot Tub | 6 (15%) | 30 (6%) |
| Splash Pad | 3 (8%) | 9 (2%) |
| Inflatable or Plastic Pool/Temporary Water Slide | 1 (3%) | 4 (1%) |
| Multiple Venue Types§ | 8 (20%) | 120 (24%) |
| Not Reported | 3 (8%) | 18 (4%) |
| Unknown | 1 (3%) | 23 (5%) |
| Total | 40 (100%) | 490 (100%) |
* Percentages do not sum to 100 due to rounding.
§Multiple venue types includes: pool and hot tub (5); pool and splash pad (1); pool, inflatable or plastic kiddie/wading pool, and splash pad (1); pool, inflatable or plastic pool, and hot tub (1).
| Jurisdiction | Month | Etiology* | Cases | Hospitalizations§ | Deaths | Water Venue(s)§ | Water Setting(s)§ |
|---|---|---|---|---|---|---|---|
| Alabama | January | Cryptosporidium sp. | 7 | 0 | 0 | Pool | Recreational Facility |
| Alabama | June | Cryptosporidium sp. | 3 | 0 | 0 | Pool | Waterpark |
| Alaska | February | Chlorine (S) | 19 | 0 | 0 | Pool | Community/Municipality |
| Colorado | March | Legionella pneumophila serogroup 1 | 2 | 2 | 1 | Hot Tub | Hotel/Motel |
| Florida | June | Legionella pneumophila | 2 | 2 | 0 | Hot Tub | Resort |
| Florida | July | Cryptosporidium parvum | 21 | 0 | 0 | Pool | Waterpark |
| Florida | July | Cryptosporidium sp. | 15 | 1 | 0 | Pool | Hotel/Motel |
| Florida | July | Cryptosporidium sp. | 7 | 0 | 0 | Splash Pad, Pool | Child Care/Daycare Center, Waterpark |
| Florida | August | Cryptosporidium hominis IfA12G1 | 10 | 0 | 0 | Hot Tub, Pool | Resort |
| Florida | August | Cryptosporidium sp. | 4 | 0 | 0 | Temporary Water Slide | Private Residence |
| Florida | December | Legionella pneumophila serogroup 1 | 2 | 2 | 0 | Hot Tub | Community/Municipality |
| Florida | December | Legionella pneumophila serogroup 1 | 2 | 1 | 0 | Hot Tub | Hotel/Motel |
| Georgia | April | Legionella pneumophila serogroup 1 | 2 | 2 | 0 | Hot Tub, Pool | Club (Requires Membership) |
| Hawaii | July | Cryptosporidium hominis IgA20 | 7 | 0 | 0 | Pool | Amusement Park |
| Illinois | June | Pseudomonas sp. | 13 | 0 | 0 | Hot Tub | Hotel/Motel |
| Kansas | December | Cryptosporidium sp. | 2 | 0 | 0 | Pool | Hotel/Motel |
| Kentucky | June | Norovirus Genogroup II | 14 | 0 | 0 | Pool | Club (Requires Membership) |
| Kentucky | July | Cryptosporidium hominis | 11 | 2 | 0 | Pool | Recreational Facility |
| Kentucky | August | Legionella pneumophila | 3 | 2 | 0 | Hot Tub, Inflatable or Plastic Kiddie/Wading Pool, Pool | Hotel/Motel |
| Louisiana | May | Legionella pneumophila | 9 | NR | 0 | NR | NR |
| Louisiana | June | Legionella pneumophila | 6 | 1 | 0 | NR | NR |
| Louisiana | June | Giardia duodenalis | 3 | 0 | 0 | NR | NR |
| Minnesota | March | Pseudomonas sp. (S) | 2 | 0 | 0 | Hot Tub, Pool | Hotel/Motel |
| Missouri | July | Cryptosporidium sp. | 37 | 0 | 0 | Pool | Waterpark |
| Nebraska | August | Cryptosporidium sp. | 23 | 0 | 0 | Unknown | Unknown |
| North Carolina | July | Cryptosporidium sp. | 3 | 0 | 0 | Pool | Community/Municipality |
| North Carolina | November | Cryptosporidium sp. (S) | 7 | 0 | 0 | Pool | Community/Municipality |
| North Dakota | September | Legionella pneumophila serogroup 1 | 2 | 1 | 0 | Hot Tub, Pool | Hotel/Motel |
| Ohio | July | Chloramines (S) | 32 | 1 | 0 | Pool | Hotel/Motel |
| Ohio | August | Cryptosporidium sp. | 27 | 0 | 0 | Kiddie/Wading Pool | Recreational Facility |
| Ohio | August | Cryptosporidium sp. | 3 | 0 | 0 | Splash Pad | Community Park |
| Oregon | June | Mycobacterium avium | 9 | 0 | 0 | Hot Tub | Private Residence |
| South Carolina | November | Acanthamoeba sp. | 2 | 0 | 0 | Pool | Community/Municipality |
| Tennessee | January | Bacterial – Unknown (S) | 12 | 0 | 0 | Pool | Hotel/Motel |
| Tennessee | July | Cryptosporidium hominis IfA12G1 | 58 | 1 | 0 | Pool | Hotel/Motel |
| Virginia | May | Campylobacter jejuni | 4 | 0 | 0 | Splash Pad | Community Park |
| Virginia | July | Cryptosporidium hominis IfA12G1 | 87 | 0 | 0 | Inflatable or Plastic Kiddie/Wading Pool, Pool, Splash Pad | Camp/Cabin |
| Virginia | August | Cryptosporidium sp. | 2 | 0 | 0 | Splash Pad | Community Park |
| Wisconsin | March | Pseudomonas aeruginosa (S) | 7 | 0 | 0 | Hot Tub, Pool | Hotel/Motel |
| Wisconsin | August | Cryptosporidium sp. | 9 | 0 | 0 | Pool | Camp/Cabin |
| Jurisdiction | Month | Etiology* | Cases | Hospitalizations | Deaths | Water Venue | Water Setting |
|---|---|---|---|---|---|---|---|
| Idaho | May | Avian schistosomes (S) | 22 | 0 | 0 | Lake/Reservoir | Unknown |
| Minnesota | August | Norovirus Genogroup II GII.2 | 18 | 0 | 0 | River/Stream | Outdoor Recreational Area |
| Missouri | July | Cryptosporidium parvum | 8 | 0 | 0 | Lake/Reservoir | Camp/Cabin |
| Ohio | July | Escherichia coli, Shiga toxin-producing | 9 | 2 | 0 | Lake/Reservoir | Beach |
| Pennsylvania | July | Norovirus unspecified | 107 | 1 | 0 | Lake/Reservoir | State Park |
| Tennessee | June | Cryptosporidium sp. | 9 | 2 | 0 | Lake/Reservoir | Beach |
| Vermont | August | Norovirus Genogroup II GII.6 | 124 | 0 | 0 | Lake/Reservoir | State Park |
* (S) = Suspected Etiology.
Drinking Water Exposures
Drinking water exposure was associated with 28% (23/82) of outbreaks, resulting in 34% (429/1,276) of reported cases, nearly 70% (124/185) of reported hospitalizations, and 93% of deaths (25/27) (Table 1). Drinking water–associated outbreaks did not display seasonality in when they occurred (Figure 5).
Among drinking water–associated outbreaks, 78% (18/23) of outbreaks were caused by Legionella (Table 10). Outbreaks with multiple etiologies accounted for 9% (2/23) of drinking water outbreaks. The remaining outbreaks were caused by Escherichia, Giardia, and Mycobacterium. Drinking water outbreaks associated with multiple etiologies caused 60% (259/429) of cases. Legionella caused 37% (157/429) of cases, 99% (123/124) of hospitalizations, and all drinking water–associated outbreak deaths.
| Etiology | Outbreaks | Cases | Hospitalizations | Deaths | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| n (%) | Confirmed | Suspected | n (%) | Confirmed | Suspected | n (%) | Confirmed | Suspected | n (%) | Confirmed | Suspected | |
| Legionella | 18 (78%) | 16 | 2 | 157 (37%) | 146 | 10 | 123 (99%) | 113 | 10 | 25 (100%) | 24 | 1 |
| Escherichia | 1 (4%) | 1 | 0 | 6 (1%) | 6 | 0 | 0 (0%) | 0 | 0 | 0 (0%) | 0 | 0 |
| Giardia | 1 (4%) | 1 | 0 | 3 (1%) | 3 | 0 | 0 (0%) | 0 | 0 | 0 (0%) | 0 | 0 |
| Mycobacterium | 1 (4%) | 0 | 1 | 4 (1%) | 0 | 4 | 0 (0%) | 0 | 0 | 0 (0%) | 0 | 0 |
| Multiple§ | 2 (9%) | 1 | 1 | 259 (60%) | 9 | 250 | 1 (1%) | 1 | 0 | 0 (0%) | 0 | 0 |
| Total | 23 (100%) | 19 | 4 | 429 (100%) | 165 | 264 | 124 (100%) | 114 | 10 | 25 (100%) | 24 | 1 |
* Percentages might not sum to 100 due to rounding.
§ Multiple etiology outbreaks include one outbreak suspected to be caused by Shigella, Campylobacter, and norovirus and one outbreak caused by Campylobacter and suspected to be caused by Giardia.
Outbreaks associated with drinking water most frequently occurred in hospitals or healthcare facilities (30%, 7/23), long term care or assisted living facilities (17%, 4/23), and hotels or motels (13%, 3/23).
| Water Setting | Outbreaks n (%) | Cases n (%) |
|---|---|---|
| Hospital/Healthcare Facility§ | 7 (30%) | 65 (15%) |
| Long Term Care Facility/Assisted Living | 4 (17%) | 72 (17%) |
| Hotel/Motel | 3 (13%) | 8 (2%) |
| Private Residence | 2 (9%) | 6 (1%) |
| Community/Municipality¶ | 1 (4%) | 250 (58%) |
| Multiple† | 1 (4%) | 9 (2%) |
| Other‡ | 4 (17%) | 16 (4%) |
| Not Reported | 1 (4%) | 3 (1%) |
| Total | 23 (100%) | 429 (100%) |
* Percentages might not sum to 100 due to rounding.
§ A healthcare institution providing inpatient medical or surgical treatment and nursing care for sick or injured persons, or a healthcare facility other than a long-term care facility.
¶ A city, town, or other settlement where a large group of people live and work served by a community or municipal water system.
† Multiple setting includes: a hotel/motel and resort.
‡ Other setting includes: casino (1), factory/industrial facility (1), farm/agricultural setting (1), restaurant/cafeteria (1).
Among drinking water outbreaks, about 70% (16/23) were associated with community water systems. Individual or private water systems (e.g., private wells) accounted for four outbreaks (17%, 4/23). In 2015, there were no reported drinking water outbreaks associated with non-community water systems. By definition, a community water system is a public water system that supplies water to the same population year round; community, individual/private, and non-community water systems are mutually exclusive (3).
| Water System | Outbreaks n (%) | Cases n (%) |
|---|---|---|
| Community | 16 (70%) | 351 (82%) |
| Individual/Private | 4 (17%) | 69 (16%) |
| Not Reported | 1 (4%) | 3 (1%) |
| Unknown | 2 (9%) | 6 (1%) |
| Total | 23 (100%) | 429 (100%) |
Ground water was the reported source for 43% (10/23) of drinking water outbreaks, resulting in 65% (277/429) of cases, while surface water was associated with 17% (4/23) of outbreaks, resulting in 26% (110/429) of cases. Nine percent (2/23) of outbreaks were associated with both ground water and surface water, and 4% (1/23) of outbreaks were associated with ground water under the influence of surface water.
| Water Source | Outbreaks n (%) | Cases n (%) |
|---|---|---|
| Ground Water | 10 (43%) | 277 (65%) |
| Surface Water | 4 (17%) | 110 (26%) |
| Ground & Surface Water | 2 (9%) | 14 (3%) |
| Ground Water Under Influence of Surface Water | 1 (4%) | 6 (1%) |
| Not Reported | 2 (9%) | 7 (2%) |
| Unknown | 4 (17) | 15 (3%) |
| Total | 23 (100%) | 429 (100%) |
* Percentages might not sum to 100 due to rounding.
| Jurisdiction | Month | Etiology* | Cases | Hospitalizations§ | Deaths | Water System§ | Water Source Description§ | Water Setting§¶ |
|---|---|---|---|---|---|---|---|---|
| Arizona | October | Campylobacter jejuni (S), Norovirus unspecified (S), Shigella sonnei subgroup D (S) | 250 | 0 | 0 | Community | Well | Community/Municipality |
| Florida | February | Legionella sp. | 3 | 1 | 0 | Community | Unknown | Private Residence |
| Florida | June | Legionella pneumophila serogroup 1 | 7 | 7 | 2 | Community | Unknown | Assisted Living Facility |
| Florida | September | Legionella pneumophila serogroup 1 | 2 | 2 | 0 | Community | Well | Hotel/Motel |
| Florida | November | Legionella pneumophila | 5 | 4 | 0 | Community | Unknown | Assisted Living Facility |
| Florida | November | Legionella pneumophila | 2 | 2 | 1 | Community | Well | Hospital/Healthcare Facility |
| Florida | December | Legionella pneumophila serogroup 1 | 2 | 2 | 0 | Community | Well | Hotel/Motel |
| Georgia | July | Legionella pneumophila serogroup 1 | 3 | 3 | 0 | Community | NR | Hospital/Healthcare Facility |
| Georgia | December | Legionella pneumophila serogroup 1 (S) | 6 | 6 | 0 | Community | NR | Factory/Industrial Facility |
| Georgia | December | Legionella pneumophila (S) | 4 | 4 | 1 | Community | NR | Hospital/Healthcare Facility |
| Illinois | July | Legionella pneumophila serogroup 1 | 58 | 36 | 13 | Individual/Private | River/Stream | Long Term Care Facility |
| Illinois | October | Legionella pneumophila serogroup 1 | 2 | 1 | 0 | Unknown | NR | Long Term Care Facility |
| Maryland | October | Legionella pneumophila serogroup 1 | 4 | 1 | 0 | Community | Well | Hotel/Motel |
| Michigan | May | Legionella pneumophila serogroup 1 | 43 | 43 | 5 | Community | River/Stream | Hospital/Healthcare Facility |
| Minnesota | December | Legionella pneumophila serogroup 1 | 2 | 2 | 0 | Community | Unknown | Restaurant/Cafeteria |
| Missouri | March | Legionella pneumophila serogroup 1 | 3 | NR | 1 | NR | NR | NR |
| New York | January | Legionella pneumophila serogroup 1 and 6 | 4 | 4 | 1 | Community | Lake/Reservoir | Hospital/Healthcare Facility |
| New York | March | Escherichia coli, Shiga toxin-producing | 6 | 0 | 0 | Individual/Private | NR | Farm/Agricultural Setting |
| New York | March | Legionella pneumophila serogroup 1 and 4 | 5 | 3 | 1 | Community | Lake/Reservoir | Hospital/Healthcare Facility |
| New York | December | Giardia duodenalis | 3 | 0 | 0 | Individual/Private | Well | Private Residence |
| Ohio | January | Mycobacterium sp. (S) | 4 | 0 | 0 | Unknown | NR | Hospital/Healthcare Facility |
| Pennsylvania | July | Legionella pneumophila | 2 | 2 | 0 | Individual/Private | Well | Casino |
| Utah | June | Campylobacter jejuni, Giardia duodenalis (S) | 9 | 1 | 0 | Community | Well, Other | Private Residence |
* (S) = Suspected Etiology.
§ NR = Not Reported.
¶ A Community/Municipality is a city, town, or other settlement where a large group of people live and work served by a community or municipal water system. A Hospital/Healthcare Facility is as a healthcare institution providing inpatient medical or surgical treatment and nursing care for sick or injured persons, or a healthcare facility other than a long-term care facility.
Other Exposures to Water
Non-drinking, non-recreational exposures to water (referred to as “other exposures to water”—e.g., industrial water exposures, flood waters) were associated with 7% (6/82) of outbreaks and 4% of cases (47/1,276) (Table 1).
Cooling devices were reported in half (3/6) of the other exposures to water outbreaks (Table 15). Untreated water consumed from river/streams (33%, 2/6) and a spring (17%, 1/7) were the remaining reported water exposure types.
| Water Type | Outbreaks n (%) | Cases n (%) |
|---|---|---|
| Cooling Device§ | 3 (50%) | 36 (77%) |
| River/Stream | 2 (33%) | 7 (15%) |
| Spring | 1 (17%) | 4 (9%) |
| Total | 6 (100%) | 47 (100%) |
* Percentages might not sum to 100 due to rounding.
§ Cooling device includes: cooling tower (2) and evaporative condenser/air conditioner (1).
Legionella caused 50% (3/6) of other water-associated outbreaks, 77% (36/47) of cases, and all hospitalizations. There was one death caused by Legionella. The remaining outbreaks were caused by Giardia (33%, 2/6) and Salmonella (17%, 1/6).
| Etiology | Outbreaks | Cases | Hospitalizations | Deaths | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| n (%) | Confirmed | Suspected | n (%) | Confirmed | Suspected | n (%) | Confirmed | Suspected | n (%) | Confirmed | Suspected | |
| Legionella | 3 (50%) | 3 | 0 | 36 (77%) | 36 | 0 | 27 (100%) | 27 | 0 | 1 (100%) | 1 | 0 |
| Giardia | 2 (33%) | 2 | 0 | 8 (17%) | 8 | 0 | 0 (0%) | 0 | 0 | 0 (0%) | 0 | 0 |
| Salmonella | 1 (17%) | 0 | 1 | 3 (6%) | 0 | 3 | 0 (0%) | 0 | 0 | 0 (0%) | 0 | 0 |
| Total | 6 (100%) | 5 | 1 | 47 (100%) | 44 | 3 | 27 (100%) | 27 | 0 | 1 (100%) | 1 | 0 |
| Jurisdiction | Month | Etiology* | Cases | Hospitalizations | Deaths | Water Type | Setting |
|---|---|---|---|---|---|---|---|
| Kansas | September | Salmonella enterica Paratyphi B (S) | 3 | 0 | 0 | River/Stream | Outdoor Recreational Area |
| New Mexico | July | Giardia duodenalis | 4 | 0 | 0 | River/Stream | Camp/Cabin |
| New York | September | Giardia duodenalis | 4 | 0 | 0 | Spring | Outdoor Recreational Area |
| Ohio | May | Legionella pneumophila serogroup 5 | 20 | 11 | 0 | Cooling Tower | Indoor Workplace/Office |
| Ohio | June | Legionella pneumophila serogroup 1 | 6 | 6 | 1 | Evaporative Condenser/Air Conditioner | Assisted Living Facility |
| Washington | October | Legionella pneumophila serogroup 1 | 10 | 10 | 0 | Cooling Tower | Unknown |
* (S) = Suspected Etiology.
Unknown Exposures to Water
In 7% (6/82) of outbreaks and 1% of cases (13/1,276) the type of water exposure was unknown. Among the six outbreaks where the type of water exposure was unknown, 67% (4/6) had an unknown water exposure and 33% (2/6) had multiple water exposures (Table 18). Outbreaks involving unknown exposures to water most frequently occurred in hotels or other lodging facilities (67%, 4/6) (Table 20).
| Water Type | Outbreaks n (%) | Cases n (%) |
|---|---|---|
| Multiple* | 2 (33%) | 4 (31%) |
| Unknown | 4 (67%) | 9 (69%) |
| Total | 6 (100%) | 13 (100%) |
* Multiple exposure outbreaks includes: Hot Tub and Well (1); Pool and River/Stream (1).
Among outbreaks with an unknown water exposure, 83% (5/6) were caused by Legionella and 17% (1/6) by Cryptosporidium (Table 19).
| Etiology | Outbreaks | Cases | Hospitalizations | ||||||
|---|---|---|---|---|---|---|---|---|---|
| n (%) | Confirmed | Suspected | n (%) | Confirmed | Suspected | n (%) | Confirmed | Suspected | |
| Legionella | 5 (83%) | 5 | 0 | 11 (85%) | 11 | 0 | 11 (100%) | 11 | 0 |
| Cryptosporidium | 1 (17%) | 1 | 0 | 2 (15%) | 2 | 0 | 0 (0%) | 0 | 0 |
| Total | 6 (100%) | 6 | 0 | 13 (100%) | 13 | 0 | 11 (100%) | 11 | 0 |
| Jurisdiction | Month | Etiology | Cases | Hospitalizations | Deaths | Water Type | Water Setting |
|---|---|---|---|---|---|---|---|
| Florida | January | Legionella pneumophila serogroup 1 | 2 | 2 | 0 | Treated recreational and drinking water exposure* | Hotel/Motel, Resort |
| Illinois | July | Legionella pneumophila serogroup 1 | 2 | 2 | 0 | Unknown | Hotel/Motel |
| Ohio | August | Legionella pneumophila serogroup 1 | 2 | 2 | 0 | Unknown | Church/Place of Worship |
| Texas | November | Legionella pneumophila serogroup 1 | 2 | 2 | 0 | Unknown | Hotel/Motel |
| Washington | June | Legionella pneumophila serogroup 1 | 3 | 3 | 0 | Unknown | Hotel/Motel |
| Wisconsin | August | Cryptosporidium sp. | 2 | 0 | 0 | Treated and untreated recreational water exposure* | Outdoor Recreational Area, School/College/University |
* Illnesses could not be associated with a single type of water exposure.
Limitations
The findings in this summary are subject to at least three limitations. First, only a proportion of waterborne outbreaks are detected, investigated, and reported to the National Outbreak Reporting System (NORS). The counts here are an underestimate of the true burden of waterborne disease outbreaks in the United States and should not be used to estimate the actual number of outbreaks or cases of waterborne disease. Second, these numbers are largely dependent on public health capacity and reporting requirements, which vary across jurisdictions, and therefore do not necessarily indicate the true occurrence in each state. Third, data on outbreaks with a chemical/toxin etiology might be limited because of differences in how these outbreaks are detected and investigated compared with infectious disease outbreaks or characteristics of the contaminants (e.g., persistence in the environment).
Conclusions
Public health surveillance is key to understanding the epidemiology of waterborne disease and outbreaks. Legionella and Cryptosporidium were the most frequently reported outbreak etiologies of waterborne disease outbreaks for 2015. Filtration and disinfection of water have reduced (though not eliminated) the burden of waterborne disease outbreaks caused by disinfectant-sensitive pathogens. Much of the remaining burden is driven by pathogens that are resistant to disinfection, either through their affinity for biofilm (Legionella and Pseudomonas) or intrinsic structural resistance (Cryptosporidium oocysts are extremely chlorine tolerant due to their hard outer shell). Effective prevention strategies beyond traditional filtration and disinfection of water include developing and implementing water management programs and adoption of CDC’s Model Aquatic Health Code.
Acknowledgements
The authors thank local, DC, state, territorial, and freely associated state public health officials and CDC staff for collecting and submitting outbreak data that made this summary possible.
References
- Collier SA, Deng L, Adam EA, et al. Estimate of Burden and Direct Healthcare Cost of Infectious Waterborne Disease in the United States. Emerging Infectious Diseases. 2021;27(1):140-149. doi:10.3201/eid2701.190676.
- Detecting and Investigating Waterborne Diseases and Outbreaks. 2019 4/25/2019 [cited 2020 5/4].
- Information about Public Water Systems. 2021 11/10/2021 [cited 2021 11/22].
