Persons using assistive technology might not be able to fully access information in this file. For assistance, please send e-mail to: mmwrq@cdc.gov. Type 508 Accommodation and the title of the report in the subject line of e-mail.
Progress Toward Interrupting Wild Poliovirus Circulation in Countries With Reestablished Transmission --- Africa, 2009--2010
Through efforts of the Global Polio Eradication Initiative (GPEI), begun in 1988, indigenous transmission of wild poliovirus (WPV) had been interrupted in all but four countries (Afghanistan, Pakistan, India, and Nigeria) by 2006 (1). Since 2002, a total of 39 previously polio-free countries experienced outbreaks following importation of WPV of Indian or Nigerian origin (2--4). Most outbreaks were stopped <6 months after confirmation. However, circulation in Angola, Chad, Democratic Republic of the Congo (DRC), and Sudan persisted >12 months following importation before 2009 (3,4). A key milestone of the GPEI 2010--2012 strategic plan (5) was to interrupt WPV transmission in these African countries with reestablished transmission by the end of 2010. As of March 8, 2011, the milestone appeared to be on track only in Sudan. In Sudan, WPV type 1 (WPV1) was introduced in 2004, but no cases were detected for a 31-month period during 2005--2008. When resurgence occurred in 2008, surveillance and eradication efforts were enhanced, and no case has been detected since June 2009. In Chad, WPV type 3 (WPV3) transmission has persisted since 2007, although undetected for 7 months in 2010. In Angola, WPV1 circulation has persisted following importation in 2007, and became more widespread in 2010, with subsequent importations into DRC and Republic of the Congo (ROC). In DRC, WPV1 circulation has persisted since introduction in 2006. Achieving polio eradication depends on stopping WPV transmission in the four endemic countries and overcoming substantial, ongoing programmatic weaknesses in Chad, Angola, and DRC.
Methods of Tracking Progress
The 2010--2012 GPEI strategic plan set several milestones. These included 1) stopping WPV transmission following importation in countries with outbreaks in 2009 by mid-2010, 2) stopping WPV transmission in subsequent outbreaks <6 months after confirmation, 3) stopping WPV transmission in countries with reestablished transmission by the end of 2010, 4) stopping WPV transmission in at least two of the four WPV-endemic countries by the end of 2011, and 5) stopping WPV transmission in all countries by the end of 2012.
The World Health Organization (WHO) and UNICEF provide annual estimates of routine coverage with 3 doses of oral poliovirus vaccine (OPV) by age 12 months (OPV3) for each country.* WPV cases are identified through acute flaccid paralysis (AFP) surveillance and testing of stool specimens for polioviruses in WHO-accredited laboratories. Quality standards for AFP surveillance include detection of ≥2 cases of nonpolio AFP (NPAFP) (AFP with no WPV isolated from adequate specimens) per 100,000 population aged <15 years in all provinces or states and adequate stool specimen collection from ≥80% of AFP cases.† Vaccination recall histories collected on children aged 6--35 months with onset of NPAFP in 2010 are used to assess target population vaccination status (the proportion with ≥4 OPV doses and the proportion with no OPV doses) at the time of AFP onset. Independent monitors assess the quality of implementation of supplementary immunization activities (SIAs)§ in areas considered at high risk by surveying the proportion of children missed in the SIA. Monitoring activities are variable; they are intended to provide a crude assessment of SIA quality and to identify areas needing improvement.
The Global Polio Laboratory Network provides comprehensive genomic sequencing of WPV isolates (6), enabling tracing of the origins of virus importations into previously polio-free areas¶ and estimation of the duration of circulation in chains of transmission. Angola, Chad, DRC, and southern Sudan were identified in 2009 as having reestablished WPV transmission (7) because genomic sequence analysis had shown the persistence of one or more chains of WPV transmission for >12 months.
WPV Status by Country
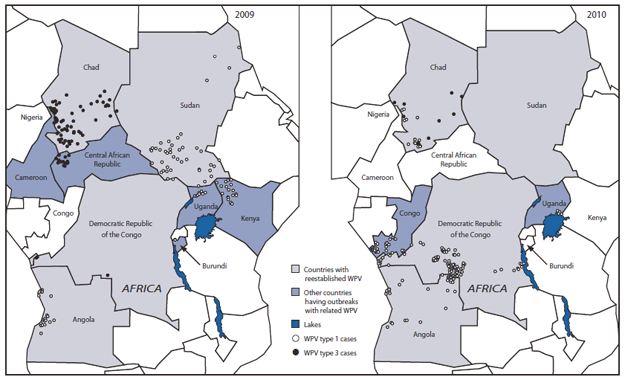
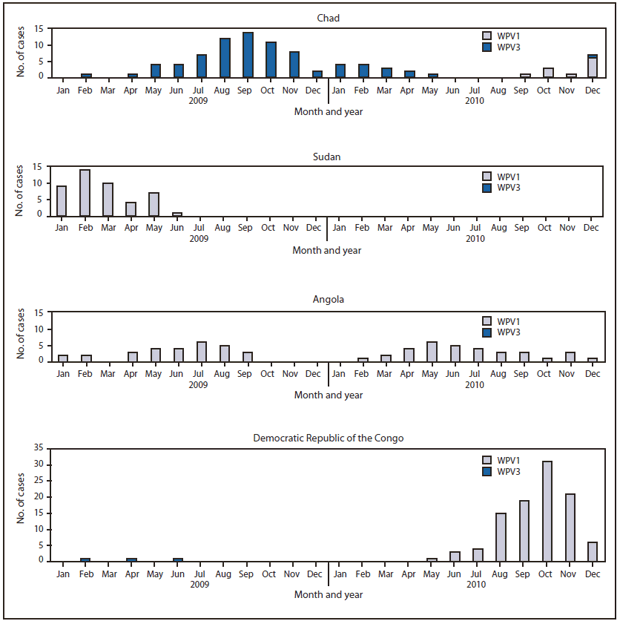
Chad. WPV3 transmission persisted in Chad after importation from Nigeria in 2007 (1,3) resulting in 79 cases in Chad during 2009--2010 in 17 of 18 provinces (Table,
Figures 1 and 2) and further spread to Cameroon and Central African Republic in 2009 (1,4). The monthly case count decreased after improvements in SIA implementation in 2010 (Figure 2). No WPV3 case was detected during May 10--December 23, 2010, but a related WPV3 case was detected in December 2010 and genetic sequencing for an additional WPV3 case detected in January 2011 is being conducted. A new WPV 1 importation from Nigeria in September 2010 resulted in 11 cases during 2010 (and five cases in 2011, as of March 8).
Estimated OPV3 coverage in Chad was 36%; 52% of NPAFP patients had ≥4 doses of OPV and 11% had no doses. Independent monitoring of SIA coverage indicated that 26% of children were missed in the February 2010 SIA. Following an initiative in March 2010, monitoring showed some SIA improvements in Chad; the percentage of children missed decreased to ≤20% during eight of the 10 SIAs implemented during March--December 2010.
AFP surveillance met standards for case detection but not for specimen collection (Table). Only 65% of AFP cases had adequate stool specimens. Difficulties in international shipment of specimens to an accredited Global Poliovirus Network Laboratory contributed to >20% of the specimens arriving at the laboratory in poor condition.
Sudan. WPV1 of Nigerian origin was imported into Sudan via Chad in 2004, resulting in transmission in northern and southern Sudan during 2004--2005 and importation into eight other countries (2). Ongoing transmission of WPV1 from this importation was not detected during August 2005--March 2008. Subsequently, a total of 70 WPV1 cases were reported in Sudan through June 2009, and associated WPV1 outbreaks occurred in 2009 in Ethiopia, Kenya, and Uganda (1,3) (Figures 1 and
2). Since the 2004 importation, 226 related WPV1 cases have been reported in Sudan, including 82 in southern Sudan (Table). Following the 2008--2009 resurgence, extensive assistance was provided to improve SIA implementation and AFP surveillance in southern Sudan.
Overall, 78% of children with NPAFP in Sudan were reported to have received ≥4 doses of OPV; estimated OPV3 coverage was 84%; 3.8% of NPAFP cases nationwide had no OPV doses. Among children with NPAFP residing in the 10 states of southern Sudan, 7.3% had received no OPV doses. Limited independent SIA monitoring data indicated <15% of children were missed in all but one state in November 2010 and <10% in all states in December.
Surveillance indicators did not meet standards in early 2009. In 2010, however, all 25 states met surveillance quality targets, including the 10 states of southern Sudan, which had a NPAFP rate of 4.2 per 100,000 population aged <15 years and an adequate stool collection rate of 94%.
Angola. In less than a decade, Angola has had three separate WPV importations related to WPV last isolated from cases in India. A 2005 WPV1 importation resulted in an outbreak that lasted until 2007 and led to outbreaks in Namibia, DRC, Central African Republic, and Burundi (3,4). A second WPV1 importation was associated with 74 polio cases in Angola during 2007--2010 (Table), and this reestablished transmission has continued into 2011. A WPV3 importation in 2008 was followed by transmission in Angola in 2008 and cases in DRC during 2008--2009 (1,3). Of the 29 WPV1 cases in Angola with onset during 2009, a total of 14 (48%) were reported from the capital, Luanda, and 14 (48%) from the western provinces. During 2010, a total of 18 of 32 (56%) WPV1 cases were detected in central Angola and at the eastern border with DRC, leading to spread to DRC (Table,
Figures 1 and 2) and into ROC (387 provisionally confirmed cases) in 2010 (8).
Estimated OPV3 coverage in Angola was 73%**; 30% of NPAFP patients reported having received ≥4 doses and 13% of NPAFP patients reported no doses. Independent monitoring after SIAs in 2010 indicated that 7%--17% of children were missed in SIAs, overall; >33% of provinces consistently have ≥10% children missed.
AFP surveillance indicators met performance targets in 2009 and 2010 (Table). However, genomic sequence analysis of WPV1 isolates suggested multiple instances of undetected transmission in Angola.
DRC. WPV1 cases occurred during 2006--2008 after being introduced from Angola, with no WPV1 case detected in 2009. During 2010, six WPV1 cases were identified in Katanga Province in southeastern DRC, where Tanzania and DRC are separated by Lake Tanganyika. The cases were genetically most closely related to WPV1 detected in DRC in 2008 and two related WPV1 cases reported from Burundi in 2009 (Figure 1) (1,4). This indicates periods of undetected transmission in eastern DRC and bordering areas. No further related cases have been identified since October 2010. Early in 2010, a new importation of WPV1 from Angola resulted in an outbreak that started in a southern border province of DRC and spread to neighboring provinces. Two additional WPV1 importations from Angola were identified in Bas-Congo Province in 2010. Four WPV3 cases linked to two 2008 importations from Angola occurred during October 2008--June 2009 (Table,
Figure 1).
Estimated OPV3 coverage in DRC was 73%; 28% of patients with NPAFP reported having received ≥4 doses of OPV, and 12% of NPAFP patients reported having received no doses. Subnational SIAs implemented in 2010 covered 20%--65% of the national age <5 years target population; independent monitoring data for the two most recent targeted 2010 SIAs in Bandundu and Kasai-Occidental provinces indicated 11%--16% of children were missed. Independent monitoring of the two most recent 2010 subnational SIAs indicated that 8% of children were missed.
AFP surveillance met standard detection targets in 2010 throughout DRC, and 75% of AFP cases had adequate specimen collection. However, genomic sequence analysis of WPV isolated from patients in Katanga Province substantiate that AFP surveillance missed chains of transmission in the eastern provinces.
Reported by
Polio Eradication Dept, World Health Organization, Geneva, Switzerland. Div of Viral Diseases, Global Immunization Div, National Center for Immunization and Respiratory Diseases, CDC.
Editorial Note
The 2010 GPEI 2010--2012 strategic plan milestone of ending reestablished transmission by the end of 2010 appears to be on track in Sudan.†† The milestone was missed in Angola and is at high risk for being missed in Chad and DRC. Persistent WPV transmission in Angola, Chad, DRC, and Sudan has led to outbreaks in eight polio-free countries, some resulting in substantial morbidity and mortality, as in ROC (3,4,8), and outbreak response activities have diverted limited resources. Achieving the GPEI milestone of ending all WPV transmission by the end of 2012 depends on progress being made in Angola, Chad, DRC, and the four WPV-endemic countries during 2011. Progress toward other milestones of the strategic plan is broadly on track. Among the four endemic countries, India and Nigeria made notable progress during 2010.§§
Among countries with outbreaks following importation, all 15 countries affected by outbreaks in 2009 had their last WPV case before mid-2010. Of the 11 countries with new importations in 2010, seven appear to have stopped transmission within 6 months of confirmation, and the others with more recent transmission also appear to be on track to meet the milestone. One importation has been reported to date in 2011; a WPV1 case was recently confirmed in Gabon, with onset in January 2011, related to the outbreak in ROC (8).
In Chad, southern Sudan, Angola, and DRC, the health infrastructure is weak, routine vaccination coverage in multiple areas is very low, and SIAs repeatedly have failed to reach a sufficient proportion of children in critical areas. SIA quality improvements during 2009--2010 in southern Sudan were the result of more effective governmental engagement and increased external support. All four countries with reestablished WPV transmission have experienced civil war in the recent past. Southern Sudan continued to have civil unrest, but security has improved within the last 2 years. In January 2011, voters in southern Sudan passed a referendum for independence. The security situation in southern Sudan will require close monitoring as the anticipated transition progresses.
Areas of insecurity and civil unrest remain in eastern Chad and in eastern DRC and resources are scarce. Angola, however, has had both the stability and resources to improve the quality of SIA implementation and AFP surveillance. Angola recently served as the WPV source for active outbreaks in three countries. Continued WPV transmission during 2010--2011 in Angola, Chad, and DRC indicates that sufficient improvements in polio eradication activities have not occurred. Virologic evidence of undetected transmission has demonstrated deficiencies in surveillance, sometimes even when performance indicators meet international standards. These deficiencies signify ongoing weaknesses in AFP detection, investigation, specimen collection, and/or transport in major areas of the country. Urgent, coordinated efforts by governmental and external partners are needed to immediately address the substantial, ongoing weaknesses in SIAs and surveillance in Angola and DRC, and to redouble efforts in Chad to continue the progress toward eliminating WPV. Sustaining polio-free status also requires strengthening routine immunization. At the outset of 2011, GPEI partner agency leaders visited heads of state of Angola and DRC to emphasize the urgency of the situation, advocate for increased efforts, and extend offers of further support. To achieve measurable operational improvements and interrupt WPV transmission in these countries, these renewed efforts must begin immediately.
References
- CDC. Progress toward interruption of wild poliovirus transmission---worldwide, 2009. MMWR 2010;59:545--50.
- CDC. Resurgence of wild poliovirus type 1 transmission and consequences of importation---21 countries, 2002--2005. MMWR 2006;55:145--50.
- CDC. Wild poliovirus type 1 and type 3 importations---15 countries, Africa, 2008--2009. MMWR 2009;58:357--62.
- CDC. Outbreaks following wild poliovirus importations---Europe, Africa, and Asia, January 2009--September 2010. MMWR 2010;59:1393--9.
- World Health Organization. Global Polio Eradication Initiative: strategic plan 2010--2012. Geneva, Switzerland: World Health Organization; 2010. Available at http://www.polioeradication.org/content/publications/gpei.strategicplan.2010-2012.eng.may.2010.pdf. Accessed March 8, 2011.
- CDC. Laboratory surveillance for wild and vaccine-derived polioviruses---worldwide, January 2008--June 2009. MMWR 2009;58:950--4.
- World Health Organization. Conclusions and recommendations of the Advisory Committee on Poliomyelitis Eradication, November 2009. Wkly Epidemiol Rec 2010:85;1--11.
- CDC. Poliomyelitis outbreak---Republic of the Congo, 2010. MMWR 2011;60:312--3.
What is already known on this topic?
Four previously polio-free countries (Angola, Chad, Democratic Republic of the Congo [DRC], and Sudan) were designated in 2009 as having reestablished wild poliovirus (WPV) transmission (lasting >12 months). Routine vaccination coverage and polio eradication campaigns were not able to stop the outbreaks following importation in 2009.
What is added by this report?
Because of strengthened immunization campaign and surveillance activities, no further WPV cases related to a 2004 WPV importation have been identified in Sudan since mid-2009. WPV transmission has continued in Chad since a 2007 importation, but decreased during 2010 as a result of somewhat strengthened immunization campaign and surveillance activities. Angola has not interrupted or limited the transmission of imported WPV since introduction in 2007 and WPV from Angola has spread in 2010, causing major outbreaks in neighboring countries. DRC has had transmission of imported WPV since introduction in 2006 with extended periods without detection. Chad and the DRC are at high risk for reestablished transmission continuing.
What are the implications for public health practice?
Achieving polio eradication depends on stopping WPV transmission in the countries that have never interrupted WPV transmission and in those that have reestablished WPV transmission. To interrupt reestablished transmission, current efforts in Chad must be reinforced and those in Angola and DRC must be improved markedly to overcome ongoing programmatic weaknesses.
|
Country
|
WPV importation/outbreak characteristics
|
Country surveillance indicators
|
Outbreak response immunization
|
|
Importation† by WPV type
|
Onset date of first polio case with imported WPV
|
Onset date of most recent polio case during 2009--2010
|
WPV source by genomic sequencing
|
No. of related WPV cases confirmed to date (2009--2010 cases)
|
NPAFP rate per 100,000 population aged <15 years, 2010§
|
No. (%) of provinces¶ with NPAFP ≥2 per 100,000 population aged <15 years, 2010
|
% adequate specimen collection, 2010**
|
Longest period (months) between detected WPV cases to date since introduction
|
No. of SIAs†† conducted since onset of first confirmed import-related WPV
|
|
Angola
|
WPV1
|
4/25/2007
|
12/12/2010
|
India
|
73 (62)
|
3.3
|
18 (94)
|
87
|
6
|
22
|
|
Chad
|
WPV3
|
11/27/2007
|
5/10/2010
|
Nigeria
|
84 (75)
|
4.3
|
17 (94)
|
65
|
15
|
20
|
|
|
WPV3
|
8/9/2009
|
|
Nigeria
|
1 (1)
|
|
|
|
|
|
|
|
WPV3
|
10/30/2009
|
|
Nigeria
|
1 (1)
|
|
|
|
|
|
|
|
WPV3
|
1/6/2010
|
|
Nigeria
|
1 (1)
|
|
|
|
|
|
|
|
WPV1
|
9/17/2010
|
12/24/2010
|
Nigeria
|
11 (11)
|
|
|
|
1
|
|
|
DRC§§
|
WPV1
|
2/27/2006
|
10/27/2010
|
Angola
|
68 (8)
|
5.0
|
11 (100)
|
75
|
27
|
29
|
|
|
WPV1
|
5/25/2010
|
12/1/2010
|
Angola
|
89 (89)
|
|
|
|
1
|
|
|
|
WPV1
|
11/10/2010
|
|
Angola
|
1 (1)
|
|
|
|
|
|
|
|
WPV1
|
11/18/2010
|
|
Angola
|
1 (1)
|
|
|
|
|
|
|
|
WPV3
|
10/18/2008
|
2/10/2009
|
Angola
|
2 (1)
|
|
|
|
3
|
|
|
|
WPV3
|
4/18/2009
|
6/24/2009
|
Angola
|
2 (2)
|
|
|
|
2
|
|
|
Sudan
|
WPV1
|
5/20/2004
|
6/27/2009
|
Chad
|
226 (45)
|
2.8
|
25 (100)
|
96
|
31
|
38
|
FIGURE 1. Cases of wild poliovirus (WPV), types 1 and 3, in countries with reestablished transmission and related cases in other countries* --- Africa, 2009 and 2010
Alternate Text: The figure above shows cases of wild poliovirus (WPV), types 1 and 3, in countries with reestablished transmission and related cases in other countries in Africa in 2009 and 2010.
FIGURE 2. Cases of wild poliovirus (WPV), types 1 and 3 detected in countries with reestablished transmission, by type and month* --- Chad, Sudan, Angola, and Democratic Republic of the Congo, 2009--2010
Alternate Text: The figure above shows cases of wild poliovirus (WPV), types 1 and 3, by type and month detected in countries with reestablished transmission in Angola, Chad, Democratic Republic of the Congo, and Sudan in 2009–2010.