Mental health and retention in HIV care: A systematic review and meta-analysis.
Citation
Rooks-Peck, C. R., Adegbite, A. H., Wichser, M. E., Ramshaw, R., Mullins, M. M., Higa, D., Sipe, T. A., & the Prevention Research Synthesis Project. (2018). Mental health and retention in HIV care: A systematic review and meta-analysisexternal icon. Health Psychology, 37(6), 574-585. doi:10.1037/hea0000606
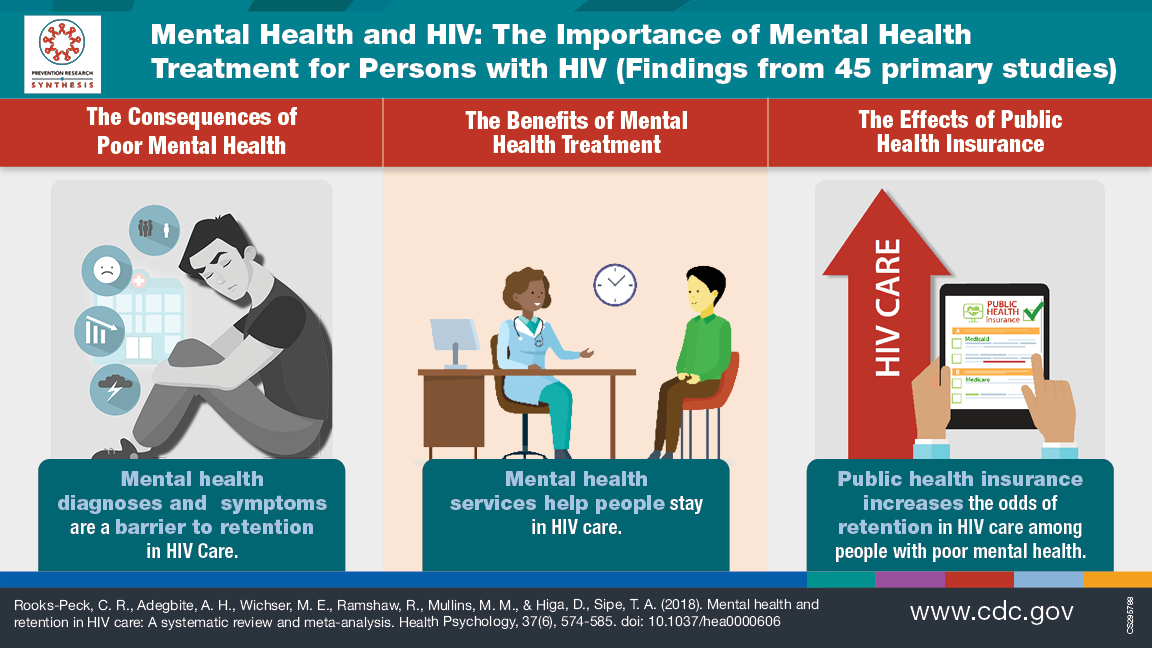
Visual Abstract
Background
Persons with HIV infection who have a mental health condition may be at higher risk for not staying in HIV care. More information is needed about this relationship.
Questions addressed in the review
- What is the evidence about the effect of having a mental health condition and staying in HIV care for people who have HIV?
- What is the evidence about the effect of getting treatment for a mental health condition on staying in HIV care?
Search Date
This review was finalized in August 2017 and covers studies published between January 2002-August 2017.
Study Characteristics
Forty-five studies, involving about 57,000 people, were included in the review. Thirty-nine studies looked at mental health conditions, and 14 studies looked at getting treatment for the mental health condition. Some studies reported both outcomes.
Key results
Overall, people with a mental health condition are less likely to stay in HIV care. Having public health insurance may change this result. Studies with lower proportions of people on public health insurance appeared to be less likely to stay in HIV care compared to studies with higher proportions of people on public health insurance. There were not enough studies to look at the effects of private health insurance. In addition, if people got treatment for their mental health condition, they were more likely to stay in HIV care.
None of the studies reported harms or negative effects from getting treatment for the mental health condition.
Quality of the evidence
The overall quality of the evidence was considered fair (versus good or poor quality) as many studies were not designed to test if confounders (that is, things other than mental health or insurance that could have influenced the findings) changed the results. Studies with lower quality showed a bigger effect for some outcomes.
Study funding source
This study was funded by the Centers for Disease Control and Prevention.
Related Resources

