Necrotizing Fasciitis: All You Need to Know
Necrotizing fasciitis (NECK-re-tie-zing FASH-e-i-tis) is a rare bacterial infection that spreads quickly in the body and can cause death.
Accurate diagnosis, rapid antibiotic treatment, and prompt surgery are important to stopping this infection.
See a doctor right away if your skin becomes red, warm, swollen, or very painful soon after an injury or surgery.

Group A strep thought to be most common cause
There are many types of bacteria that can cause the “flesh-eating disease” called necrotizing fasciitis. Public health experts believe group A Streptococcus (group A strep) are the most common cause of necrotizing fasciitis. This web page only focuses on necrotizing fasciitis caused by group A strep bacteria.
Bacteria that live in water, including Vibrio vulnificus, can also cause necrotizing fasciitis. Learn about Vibrio wound infections.
How you get necrotizing fasciitis
The bacteria most commonly enter the body through a break in the skin. Different breaks in the skin can include:
- Cuts and scrapes
- Burns
- Insect bites
- Puncture wounds (including those due to intravenous [IV] drug use)
- Surgical wounds
However, people can also get necrotizing fasciitis after blunt trauma (an injury that does not break the skin).
Necrotizing fasciitis is rarely contagious
Most cases of necrotizing fasciitis occur randomly. It is very rare for someone with necrotizing fasciitis to spread the infection to other people. For this reason, doctors usually do not give preventive antibiotics to close contacts of someone with necrotizing fasciitis.
Necrotizing means causing the death of tissues. Fasciitis means inflammation of the fascia (the tissue under the skin that surrounds muscles, nerves, fat, and blood vessels).
Symptoms can often be confusing and develop quickly
The infection often spreads very quickly.
Early symptoms of necrotizing fasciitis can include:
- A red, warm, or swollen area of skin that spreads quickly
- Severe pain, including pain beyond the area of the skin that is red, warm, or swollen
- Fever
See a doctor right away if you have these symptoms after an injury or surgery. Even though minor illnesses can cause symptoms like these, people should not delay getting medical care.
Later symptoms of necrotizing fasciitis can include:
- Ulcers, blisters, or black spots on the skin
- Changes in the color of the skin
- Pus or oozing from the infected area
- Dizziness
- Fatigue (tiredness)
- Diarrhea or nausea
Some people are at increased risk
While anyone can get necrotizing fasciitis, it is rare.
Other health factors
Most people who get this illness have other health problems that may lower their body’s ability to fight infections. Some conditions that weaken the body’s immune system include:
- Diabetes
- Kidney disease
- Cirrhosis (scarring) of the liver
- Cancer
Diagnosis can be difficult and acting fast is key
There are many infections that look similar to necrotizing fasciitis in the early stages, which can make diagnosis difficult. In addition to looking at the injury or infection, doctors can diagnose necrotizing fasciitis by:
- Performing a biopsy (taking a tissue sample)
- Looking at bloodwork for signs of infection and muscle damage
- Looking at imaging (CT scan, MRI, ultrasound) of the damaged area
However, it is important to start treatment as soon as possible. Therefore, doctors may not wait for test results if they think a patient might have necrotizing fasciitis.
Prompt treatment is key
Necrotizing fasciitis is a very serious illness that requires care in a hospital. Antibiotics and surgery are typically the first lines of defense if a doctor suspects a patient has necrotizing fasciitis.

Doctors treat necrotizing fasciitis with IV antibiotics.
Antibiotics
To try to stop the infection, doctors give antibiotics through an IV, which allows medicine to flow into a vein.
Sometimes, however, antibiotics cannot reach all the infected areas because the bacteria have killed too much tissue and reduced blood flow. When this happens, doctors must surgically remove the dead tissue.
Surgery
Since necrotizing fasciitis can spread so rapidly, patients often must get surgery done very quickly. It is not unusual for someone with necrotizing fasciitis to end up needing multiple surgeries. In serious cases, the patient may need a blood transfusion.

Up to 1 in 5 people with necrotizing fasciitis die from the infection.
Serious complications are common
Necrotizing fasciitis can lead to
- Sepsis
- Shock
- Organ failure
It can also result in life-long complications from loss of limbs or severe scarring due to surgically removing infected tissue.
Looking at data from the most recent five years:
- Even with treatment, up to 1 in 5 people with necrotizing fasciitis died from the infection
- Up to 1 in 3 people who got both necrotizing fasciitis and streptococcal toxic shock syndrome at the same time died from their infections
Prevent necrotizing fasciitis
There are no vaccines to prevent group A strep infections, but there are things you can do to help protect yourself and others.
To help prevent group A step infections, you should:
- Wash your hands often
- Clean and care for wounds
Clean and care for wounds
Wash hands often
Wash hands often with soap and water or use an alcohol-based hand rub if washing is not possible.
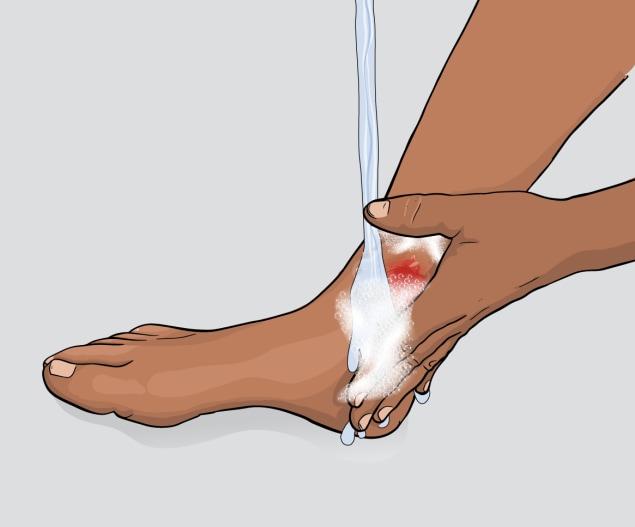
Clean wounds
Clean all minor cuts and injuries that break the skin (like blisters and scrapes) with soap and water.

Bandage wounds
Clean and cover draining or open wounds with clean, dry bandages until they heal.

See a doctor
See a doctor for puncture and other deep or serious wounds.
If you have an open wound or skin infection, avoid spending time in:
- Hot tubs
- Swimming pools
- Natural bodies of water (e.g., lakes, rivers, oceans)
Care for fungal infections like athlete’s foot to help prevent group A strep infections. Learn about athlete’s foot (ringworm).
CDC tracks necrotizing fasciitis caused by group A strep bacteria
CDC tracks necrotizing fasciitis caused by group A strep bacteria with a special system called Active Bacterial Core surveillance (ABCs). Since 2010, approximately 700 to 1,150 cases occur each year in the United States. This is likely an underestimate. According to ABCs data, the number of annual group A strep necrotizing fasciitis infections reported to ABCs does not appear to be rising.



