At a glance
- Infections monitored by FoodNet increased or remained at levels observed from 2016–2018.
- More work is needed to meet Healthy People 2030 goals for reducing foodborne illness.
- Continued surveillance and culturing of patient samples can help guide public health decisions.
Background
Documenting the major sources of and trends in foodborne illness provides important information needed to determine whether prevention measures are working. Each year, FoodNet reports on the number of infections in the FoodNet surveillance area from pathogens transmitted commonly through food: Campylobacter, Cyclospora, Listeria, Salmonella, Shiga toxin-producing E. coli (STEC), Shigella, Vibrio, and Yersinia. Laboratory tests, including cultures and culture-independent diagnostic tests (CIDTs), detected these pathogens. To calculate incidence, FoodNet tracks the number of reported infections per 100,000 people per year.
Full report available
Key findings
This year's report summarizes 2023 preliminary surveillance data from the Foodborne Diseases Active Surveillance Network (FoodNet). It describes 2023 incidence compared with the average annual incidence from 2016–2018, the reference period used for the U.S. Department of Health and Human Services (HHS) Healthy People 2030 goals for reducing infections from select pathogens. The report also summarizes cases of hemolytic uremic syndrome (HUS) for 2022.
General trends
- Campylobacter and Salmonella remain the top causes of enteric (intestinal) infections monitored by FoodNet.
- Enteric infections monitored by FoodNet either increased or remained at levels observed from 2016–2018.
- Incidence of Campylobacter, Cyclospora, STEC, Vibrio, and Yersinia infections increased in 2023 compared with 2016–2018.
- Incidence of Listeria, Salmonella, and Shigella infections did not change in 2023 compared with 2016–2018.
- Incidence of Campylobacter, Listeria, Salmonella, and STEC infections in 2023 was higher than the Healthy People 2030 target rates. Incidence of these infections must decrease to meet the target rates.
- Incidence of HUS did not change in 2022 compared with 2016–2018.
- Incidence of Campylobacter, Cyclospora, STEC, Vibrio, and Yersinia infections increased in 2023 compared with 2016–2018.

Increased use of CIDTs may be driving increases in reported illnesses
- More infections were diagnosed by CIDT in 2023 than in previous years.
- Increases in incidence would normally mean that more people are getting sick. Increases in CIDT use suggest that we may just be detecting infections that would otherwise not be diagnosed.
Moving forward
- More work is needed to reduce disease burden and meet Healthy People 2030 goals.
- Continued surveillance is needed to monitor the effects of changing diagnostic practices on disease trends.
- Laboratories can provide information key to guiding public health decisions by culturing patient samples after receiving a positive CIDT result.
- CIDT developers can help by ensuring new CIDTs are compatible with culture-based methods, so culture can be attempted following a positive CIDT result.
- Laboratories can provide information key to guiding public health decisions by culturing patient samples after receiving a positive CIDT result.
Expanding the FoodNet surveillance area
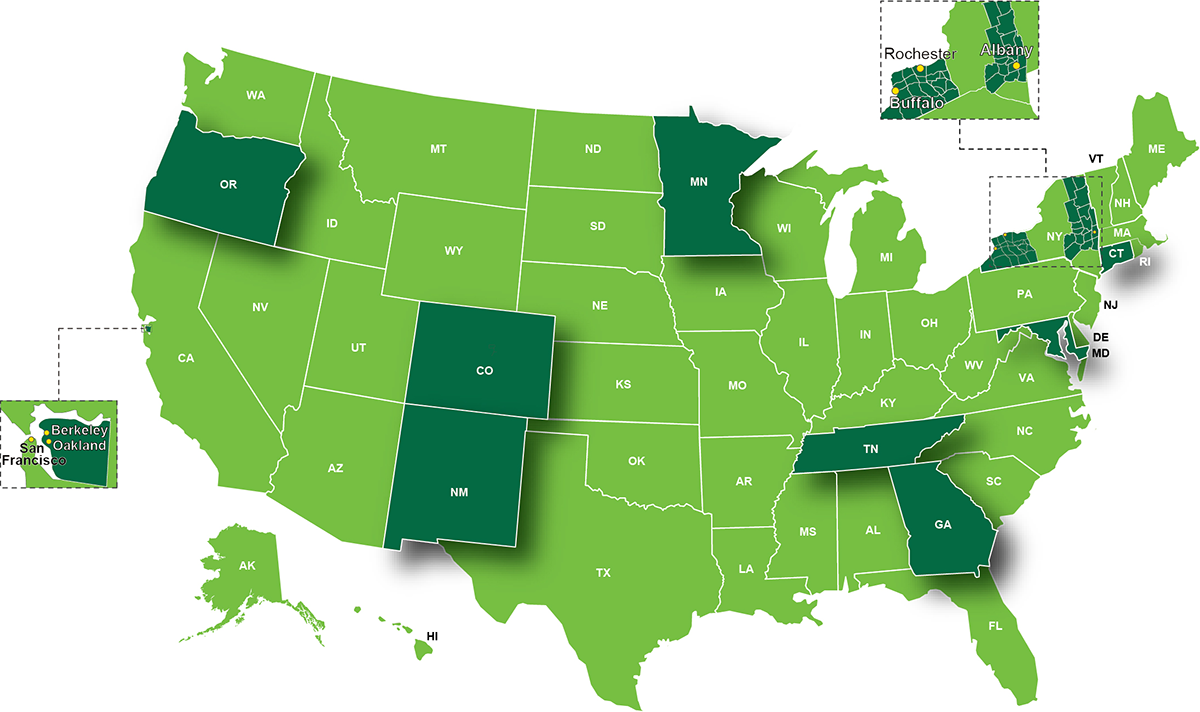
- FoodNet's surveillance area expanded during 2023 to include all of Colorado.
- The expansion increased representation for specific populations, including
- People identifying as Hispanic, American Indian/Alaska Native, Native Hawaiian/Pacific Islander, or as of more than 1 race
- People living in rural counties
- People identifying as Hispanic, American Indian/Alaska Native, Native Hawaiian/Pacific Islander, or as of more than 1 race
- Increased representation
- Improves FoodNet's ability to monitor disease trends
- Makes FoodNet data more applicable to a larger population
- Improves FoodNet's ability to monitor disease trends
Interpreting changes in incidences of infection
Assessing how various factors affect individual pathogens is challenging. Several factors are likely responsible, including
- More sick people might have been tested because CIDTs are fast and easy to use.
- Increased used of CIDTs might have allowed laboratories to detect infections that would have previously been missed.
- People might have had more exposure to some pathogens.
Use of CIDTs continues to increase, leading to increased detection of infections.
Most of these are true infections that, without CIDTs, would have otherwise been missed. Some infections are harder to detect by traditional methods (e.g., culture-based)—including those caused by STEC, Vibrio, and Yersinia. Before widespread use of CIDTs, many patient samples were not tested for these infections. When samples were tested, false negative results were frequent.
CIDTs likely were not the only factor that affected the number of reported infections in 2023. For infections caused by some pathogens, increases in incidence appear to outpace increased CIDT usage.
FoodNet sets a reference period that can be used for many years. FoodNet used 1996–1998 and 2006–2008 as reference periods in earlier reports. The current reference period matches the reference period used for the Healthy People 2030 goals for Campylobacter, Listeria, Salmonella, and STEC.
FoodNet uses a Bayesian model to estimate changes in the incidence of infections. The model uses the average annual incidence for 2016–2018 for comparisons. This model adjusts for site-specific trends, reduces sensitivity to single-year events (e.g., outbreaks), and reduces biases towards more populous sites.
What's being done
Since 1996, FoodNet has been counting cases and tracking trends for infections transmitted commonly through food. Information gathered on which illnesses are decreasing and which are increasing provides a foundation for food safety policy and prevention efforts. FoodNet's surveillance data, such as those in this report, show where efforts are needed to reduce foodborne illnesses. Learn more about FoodNet.
CDC uses the best scientific methods and information available to monitor, investigate, control, and prevent foodborne illness. Using epidemiology and laboratory science, CDC assesses public health threats. CDC works closely with state health departments to monitor the frequency of specific diseases and to conduct national surveillance for the diseases it monitors.
When food safety threats appear, CDC collaborates with public health partners, including state health departments, the U.S. Food and Drug Administration (FDA), and the U.S. Department of Agriculture (USDA), to conduct epidemiologic and laboratory investigations to determine the causes of these threats and ways to control them. Although CDC does not regulate the safety of food, CDC works with regulatory agencies to help them develop robust food safety policies and assess the effectiveness of current prevention efforts. CDC provides independent scientific assessment of what the problems are, how they can be controlled, and where the gaps exist in our knowledge. You can find more information on foodborne illness and CDC's prevention activities on CDC's Food Safety website.
Government regulation related to food safety is the responsibility of FDA, USDA's Food Safety and Inspection Service (USDA-FSIS), the National Marine Fisheries Service (NOAA Fisheries), and other regulatory agencies. Visit the websites below to learn about each agency's actions and activities to improve food safety.
CDC works closely with regulatory agencies as they, along with industry, develop and implement measures to make our food safer.
Following four simple food safety steps – clean, separate, cook, and chill – can help protect you and your loved ones when preparing food at home.
Suggested citation
Centers for Disease Control and Prevention (CDC). Reported incidence of infections caused by pathogens transmitted commonly through food: Impact of increased use of culture-independent diagnostic tests — Foodborne Diseases Active Surveillance Network, 1996–2023. MMWR Morb Mortal Wkly Rep. 2024 July 3.
