|
TABLE 1. Number and percentage* of cryptosporidiosis case reports, by state/area --- National Notifiable Disease Surveillance System, United States,† 2006--2008 |
||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
2006 |
2007 |
2008 |
||||||||||
|
State/Area |
No. |
(%) |
Rate§ |
No. outbreak cases¶ |
No. |
(%) |
Rate |
No. outbreak cases |
No. |
(%) |
Rate |
No. outbreak cases |
|
Alabama |
72 |
(1.1) |
1.5 |
126 |
(1.1) |
2.7 |
9 |
74 |
(0.7) |
1.6 |
||
|
Alaska |
4 |
(0.1) |
0.6 |
4 |
(0.0) |
0.6 |
3 |
(0.0) |
0.4 |
|||
|
Arizona |
29 |
(0.4) |
0.4 |
53 |
(0.5) |
0.8 |
89 |
(0.8) |
1.4 |
|||
|
Arkansas |
29 |
(0.4) |
1.0 |
63 |
(0.5) |
2.2 |
95 |
(0.9) |
3.3 |
|||
|
California |
340 |
(5.2) |
0.9 |
303 |
(2.6) |
0.8 |
275 |
(2.6) |
0.7 |
|||
|
Colorado |
77 |
(1.2) |
1.6 |
10 |
216 |
(1.9) |
4.5 |
10 |
113 |
(1.1) |
2.3 |
1 |
|
Connecticut |
38 |
(0.6) |
1.1 |
42 |
(0.4) |
1.2 |
41 |
(0.4) |
1.2 |
|||
|
Delaware |
15 |
(0.2) |
1.7 |
21 |
(0.2) |
2.4 |
12 |
(0.1) |
1.4 |
|||
|
District of Columbia |
17 |
(0.3) |
2.9 |
3 |
(0.0) |
0.5 |
15 |
(0.1) |
2.5 |
|||
|
Florida |
717 |
(11.1) |
3.9 |
219 |
738 |
(6.3) |
4.1 |
115 |
549 |
(5.2) |
3.0 |
72 |
|
Georgia |
275 |
(4.2) |
2.8 |
239 |
(2.1) |
2.5 |
263 |
(2.5) |
2.7 |
|||
|
Hawaii |
4 |
(0.1) |
0.3 |
6 |
(0.1) |
0.5 |
2 |
(0.0) |
0.2 |
|||
|
Idaho |
40 |
(0.6) |
2.6 |
518** |
(4.4) |
34.6 |
365 |
73 |
(0.7) |
4.8 |
5 |
|
|
Illinois |
257 |
(4.0) |
2.0 |
66 |
205 |
(1.8) |
1.6 |
17 |
207 |
(2.0) |
1.6 |
|
|
Indiana |
113 |
(1.7) |
1.8 |
149 |
(1.3) |
2.4 |
203 |
(1.9) |
3.2 |
1 |
||
|
Iowa |
231 |
(3.6) |
7.7 |
610 |
(5.2) |
20.4 |
284 |
(2.7) |
9.5 |
|||
|
Kansas |
82 |
(1.3) |
2.9 |
155 |
(1.3) |
5.6 |
38 |
84 |
(0.8) |
3.0 |
4 |
|
|
Kentucky |
44 |
(0.7) |
1.0 |
249 |
(2.1) |
5.9 |
179 |
36 |
(0.3) |
0.8 |
||
|
Louisiana |
86 |
(1.3) |
1.9 |
64 |
(0.5) |
1.5 |
67 |
(0.6) |
1.5 |
|||
|
Maine |
52 |
(0.8) |
3.9 |
4 |
56 |
(0.5) |
4.3 |
7 |
46 |
(0.4) |
3.5 |
7 |
|
Maryland |
20 |
(0.3) |
0.4 |
36 |
(0.3) |
0.6 |
54 |
(0.5) |
1.0 |
|||
|
Massachusetts |
175 |
(2.7) |
2.7 |
5 |
132 |
(1.1) |
2.0 |
172 |
(1.6) |
2.6 |
||
|
Michigan |
145 |
(2.2) |
1.4 |
1 |
215 |
(1.8) |
2.1 |
284 |
(2.7) |
2.8 |
||
|
Minnesota |
242 |
(3.7) |
4.6 |
12 |
303 |
(2.6) |
5.8 |
14 |
236 |
(2.2) |
4.5 |
6 |
|
Mississippi |
25 |
(0.4) |
0.9 |
103 |
(0.9) |
3.5 |
17 |
(0.2) |
0.6 |
|||
|
Missouri |
283 |
(4.4) |
4.8 |
214 |
(1.8) |
3.6 |
195 |
(1.9) |
3.3 |
|||
|
Montana |
152 |
(2.3) |
15.7 |
46 |
77 |
(0.7) |
8.0 |
45 |
(0.4) |
4.7 |
||
|
Nebraska |
115 |
(1.8) |
6.4 |
1 |
196 |
(1.7) |
11.1 |
2 |
113 |
(1.1) |
6.3 |
11 |
|
Nevada |
14 |
(0.2) |
0.5 |
37 |
(0.3) |
1.4 |
17 |
(0.2) |
0.7 |
4 |
||
|
New Hampshire |
47 |
(0.7) |
3.6 |
47 |
(0.4) |
3.6 |
1 |
61 |
(0.6) |
4.6 |
||
|
New Jersey |
42 |
(0.6) |
0.5 |
1 |
67 |
(0.6) |
0.8 |
1 |
40 |
(0.4) |
0.5 |
|
|
New Mexico |
45 |
(0.7) |
2.3 |
125 |
(1.1) |
6.4 |
242 |
(2.3) |
12.2 |
93 |
||
|
New York†† |
339 |
(5.2) |
1.7 |
1 |
359 |
(3.1) |
1.8 |
4 |
376 |
(3.6) |
1.9 |
|
|
New York City |
155 |
(2.4) |
1.9 |
105 |
(0.9) |
1.3 |
107 |
(1.0) |
1.3 |
|||
|
North Carolina |
101 |
(1.6) |
1.1 |
7 |
132 |
(1.1) |
1.5 |
10 |
79 |
(0.8) |
0.9 |
3 |
|
North Dakota |
20 |
(0.3) |
3.1 |
78 |
(0.7) |
12.2 |
16 |
(0.2) |
2.5 |
|||
|
Ohio |
369 |
(5.7) |
3.2 |
8 |
608 |
(5.2) |
5.3 |
16 |
705 |
(6.7) |
6.1 |
48 |
|
Oklahoma |
56 |
(0.9) |
1.5 |
216 |
(1.9) |
6.0 |
104 |
238 |
(2.3) |
6.5 |
44 |
|
|
Oregon |
82 |
(1.3) |
2.2 |
9 |
163 |
(1.4) |
4.4 |
38 |
69 |
(0.7) |
1.8 |
4 |
|
Pennsylvania |
287 |
(4.4) |
2.3 |
17 |
1,023** |
(8.8) |
8.2 |
488 |
331 |
(3.2) |
2.7 |
9 |
|
Rhode Island |
14 |
(0.2) |
1.3 |
11 |
(0.1) |
1.0 |
10 |
(0.1) |
1.0 |
1 |
||
|
South Carolina |
131 |
(2.0) |
2.9 |
44 |
88 |
(0.8) |
2.0 |
60 |
(0.6) |
1.3 |
||
|
South Dakota |
86 |
(1.3) |
10.7 |
5 |
169 |
(1.4) |
21.2 |
3 |
88 |
(0.8) |
10.9 |
6 |
|
Tennessee |
48 |
(0.7) |
0.8 |
141 |
(1.2) |
2.3 |
5 |
48 |
(0.5) |
0.8 |
1 |
|
|
Texas |
273 |
(4.2) |
1.1 |
37 |
235 |
(2.0) |
1.0 |
2 |
3,342** |
(31.8) |
13.7 |
1,709 |
|
Utah |
21 |
(0.3) |
0.8 |
1,901** |
(16.3) |
71.2 |
1,901 |
49 |
(0.5) |
1.8 |
||
|
Vermont |
54 |
(0.8) |
8.7 |
47 |
(0.4) |
7.6 |
64 |
(0.6) |
10.3 |
|||
|
Virginia |
71 |
(1.1) |
0.9 |
90 |
(0.8) |
1.2 |
81 |
(0.8) |
1.0 |
|||
|
Washington |
95 |
(1.5) |
1.5 |
151 |
(1.3) |
2.3 |
8 |
99 |
(0.9) |
1.5 |
||
|
West Virginia |
20 |
(0.3) |
1.1 |
12 |
(0.1) |
0.7 |
26 |
(0.2) |
1.4 |
|||
|
Wisconsin |
532 |
(8.2) |
9.5 |
26 |
790 |
(6.8) |
14.1 |
786 |
(7.5) |
14.0 |
||
|
Wyoming |
53 |
(0.8) |
9.9 |
71 |
(0.6) |
13.6 |
35 |
26 |
(0.2) |
4.9 |
2 |
|
|
Total |
6,479 |
(100.0) |
2.2 |
519 |
11,657 |
(100.0) |
3.9 |
3,372 |
10,500 |
(100.0) |
3.5 |
2,031 |
|
Sources: Population estimates are from the Population Division, U.S. Census Bureau. Annual estimates of the resident population for the United States, regions states, and Puerto Rico: July 1, 2000 to July 1, 2008 (NST-EST 2008 01). Available at http://www.census.gov/popest/states. Estimates of the New York City population are from Annual estimates of the population for incorporated places over 100,000, ranked by July 1, 2008 population: April 1, 2000 to July 1, 2008 (SUB-EST 2008-01). Available at http://www.census.gov/popest/cities/tables. * Percentages might not total 100% because of rounding. † Cryptosporidiosis is not a reportable condition in U.S. territories or freely associated states. § Per 100,000 population on the basis of U.S. Census Bureau population estimates. ¶ Number of cases linked to a known outbreak. ** Includes cases from large recreational water outbreaks. †† New York State case reports include New York City. |
||||||||||||
Persons using assistive technology might not be able to fully access information in this file. For assistance, please send e-mail to: mmwrq@cdc.gov. Type 508 Accommodation and the title of the report in the subject line of e-mail.
Cryptosporidiosis Surveillance --- United States, 2006--2008
Abstract
Problem/Condition: Cryptosporidiosis is a nationally notifiable gastrointestinal illness caused by chlorine-tolerant protozoa of the genus Cryptosporidium.
Reporting Period: 2006--2008.
System Description: State and two metropolitan health departments voluntarily report cases of cryptosporidiosis through CDC's National Notifiable Diseases Surveillance System.
Results: During 2006--2008, the number of reported cases of cryptosporidiosis increased dramatically (79.9%), from 6,479 for 2006 to 11,657 for 2007, and then decreased (9.9%) to 10,500 in 2008. All jurisdictions reported cryptosporidiosis cases during the reporting period, and the number of jurisdictions reporting >2.5 cases per 100,000 population increased from 20 in 2006 to 26 in 2007 and 27 in 2008. A greater number of case reports were received for children aged 1--9 years and for adults aged 25--39 years than were received for persons in other age groups. The number of cases reported among males and females was similar. Racial and ethnic comparisons were difficult because many case-reports did not report race and ethnicity. Peak onset of illness occurred annually during early summer through early fall.
Interpretation: Transmission of cryptosporidiosis occurs throughout the United States, with more frequent diagnosis or reporting occurring in northern states. An increase in cases reported for 2007 and 2008 is attributable partially to multiple large recreational water-associated outbreaks. State incidence figures should be compared with caution because individual state surveillance systems have varying capabilities to detect cases, and reporting might vary. The seasonal peak in age-specific case reports coincides with the summer recreational water season and likely reflects increased use of communal swimming venues (e.g., lakes, rivers, swimming pools, and water parks) by young children.
Public Health Action: Local and state health departments can use cryptosporidiosis surveillance data to better understand the epidemiologic characteristics and the disease burden of cryptosporidiosis in the United States, design efforts to prevent the spread of disease, and establish research priorities.
Introduction
Cryptosporidiosis is a gastrointestinal illness caused by protozoa of the genus Cryptosporidium (1). In otherwise healthy persons, clinical illness is characterized by watery diarrhea, which can be accompanied by abdominal cramps, loss of appetite, low-grade fever, nausea, vomiting, and weight loss; however, asymptomatic infection occurs frequently (2). Cryptosporidium also can cause an opportunistic infection in human immunodeficiency virus (HIV)--infected patients, who might experience life-threatening infection with profuse, watery, cholera-like diarrhea. In severely immunocompromised patients, disease can progress to cholangitis or pancreatitis (3). However, incidence of this parasitic infection among the HIV-infected population has decreased since the introduction of highly active antiretroviral therapy (HAART) for HIV infection (4). Nitazoxanide is the only broad-spectrum antiparasitic drug that has been approved in the United States for treatment of cryptosporidiosis. Nitazoxanide can be prescribed for children aged >1 year and adults, but it has not proven effective for immunocompromised persons (5,6).
Cryptosporidium is a genus of protozoan parasites within the phylum Apicomplexa, and its taxonomy continues to evolve. Cryptosporidiosis is a zoonotic disease that causes clinical disease in both humans and animals; species names are based primarily on the animal species serving as host (7). Revised Cryptosporidium taxonomy based on recent advances in molecular laboratory testing methods has clarified that multiple species infect humans. C. hominis (known previously as C. parvum genotype I) primarily infects humans and exists in a human-to-human transmission cycle. C. parvum (known previously as C. parvum genotype II) can infect both humans and ruminants, each with their own transmission cycles that intersect in zoonotic disease. In addition, molecular studies have demonstrated that humans are susceptible to infection with multiple subtypes of C. parvum and C. hominis (7). To a lesser extent, human infections also have been documented with C. felis, from cats; C. canis, from dogs; C. meleagridis, from birds; C. suis, from pigs; C. muris, from rodents; and a C. cervine genotype from various animals (7). Illnesses caused by infection with the different Cryptosporidium species might differ clinically (8).
Cryptosporidium infection is transmitted by the fecal-oral route and results from the ingestion of Cryptosporidium oocysts through the consumption of fecally contaminated food or water or through direct person-to-person or animal-to-person contact. The oocysts are infectious immediately upon being excreted in feces. The infectious dose is low; feeding studies have demonstrated that the ingestion of as few as 10--30 oocysts can cause infection in healthy persons (9,10). Infected persons have been reported to shed 108--109 oocysts in a single bowel movement and to excrete infectious oocysts for up to 50 days after cessation of diarrhea (11,12).
Cryptosporidium can exist in a body of water treated with chlorine (i.e., it is chlorine tolerant), which poses challenges for traditional chemical treatment of drinking and recreational water and for environmental surface cleaning. The organism also is not easily inactivated by alcohol-based hand sanitizers. Prevention and control measures include 1) practicing good hygiene (e.g., washing hands and not swimming when ill with diarrhea), 2) treating or avoiding contaminated water (not swallowing pool water, boiling or filtering water, and installing secondary disinfection systems (e.g., ultraviolet irradiation or ozone disinfection systems that inactivate Cryptosporidium) in pools, 3) exercising caution when traveling, and 4) avoiding fecal exposure during sexual activity (13).
Although cryptosporidiosis cases occur sporadically, outbreaks have been well documented since the first reported U.S. drinking water-associated outbreak in 1984 (14) and the first U.S. recreational water-associated outbreak in 1988 (15). Cryptosporidium has since emerged as the most frequently recognized cause of recreational water-associated outbreaks of gastroenteritis, particularly in treated (disinfected) venues. In addition, foodborne outbreaks of cryptosporidiosis linked to ill food handlers and unpasteurized apple cider have been reported (16,17). Outbreaks resulting from person-to-person transmission in child care centers and from animal-to-person transmission in an animal nursery also have been reported (18,19).
In 1994, the Council of State and Territorial Epidemiologists called for reporting of cryptosporidiosis as a nationally notifiable disease; the first full year for reporting began in 1995. Surveillance data for 1995--2005 have been published previously (20--22). This report summarizes national cryptosporidiosis surveillance data for 2006--2008.
Methods
Case Definition
Confirmed and probable cases of cryptosporidiosis are reported voluntarily to CDC. A confirmed case of cryptosporidiosis (i.e., one that has a positive laboratory finding) is defined as one in which Cryptosporidium has been detected in
- organisms in stool, intestinal fluid, or tissue samples or biopsy specimens;
- antigens in stool or intestinal fluid; or
- nucleic acid in stool, intestinal fluid, or tissue samples or biopsy specimens (23,24).
A probable case of cryptosporidiosis is a clinically compatible case that is linked epidemiologically to a confirmed case (23). This report includes both confirmed and probable cases as reported by jurisdictions.
Testing
Testing for Cryptosporidium is not always included in routine examination of stool for ova and parasites (1). Commercially available immunoassay kits are available and might be more sensitive and specific than routine microscopic examination (25). Direct fluorescent antibody (DFA) testing is an extremely sensitive and specific detection method and is considered the "gold standard" by many laboratorians; other immunodiagnostic kits that do not require microscopy (e.g., enzyme immunoassay [EIA] testing and rapid immunochromatographic cartridge assays) also are available (25); they do not take the place of routine ova and parasite examination but might be useful in diagnosing Cryptosporidium infections. Only molecular testing (e.g., polymerase chain reaction) can be used to speciate Cryptosporidium; however, no species data are reported to CDC.
Reporting
State, District of Columbia (DC), and New York City (NYC) health department jurisdictions report cases of cryptosporidiosis to CDC voluntarily through the National Notifiable Diseases Surveillance System (NNDSS). Reports include the patient's place of residence (i.e., state and county), age, sex, race, ethnicity (i.e., Hispanic or non-Hispanic) and date of illness onset and indicate whether the case is linked to a known outbreak. An outbreak-associated case is a laboratory-confirmed or probable case that is linked epidemiologically to an outbreak. Because this report includes probable cases of cryptosporidiosis, and because some of the data were finalized more recently, the number of cases provided in this report might be slightly higher than the number reported in CDC's annual Summary of Notifiable Diseases.
Analysis
Analysis of national cryptosporidiosis surveillance data for 2006--2008 was conducted using SAS v.9.1 (SAS Institute Inc.; Cary, North Carolina) and the Food Safety Information Link (FSI Link). FSI Link is an intranet-based tool available to CDC staff that provides access to NNDSS data and is used to monitor trends in, and investigate outbreaks of, reportable foodborne and waterborne diseases. Population data from the U.S. Census Bureau were used to calculate incidence rates.
Results
During 2006--2008, the number of reported cases of cryptosporidiosis increased dramatically (79.9%), from 6,479 for 2006 to 11,657 for 2007, and then decreased (9.9%) to 10,500 in 2008 (Table 1). All jurisdictions reported cryptosporidiosis cases during the reporting period, and the number of jurisdictions reporting ≥2.5 cases per 100,000 population increased from 20 in 2006 to 26 in 2007 and 27 in 2008 (Table 1).
During 2006--2008, incidence of cryptosporidiosis per 100,000 population ranged from 0.2 cases (in Hawaii, 2008) to 71.2 cases (in Utah, 2007) (Table 1; Figure 1). The higher incidence of cryptosporidiosis in Utah in 2007 was influenced by a single large outbreak among >1,900 persons (26). Increased reporting of cases also occurred in certain Midwestern, Rocky Mountain, and Southwestern states.
Surveillance data displayed a bimodal age distribution, with the greatest number of reported cases occurring among children aged 1--9 years and among adults aged 25--39 years (Figure 2). When reports for which a patient's sex was unknown or missing were excluded, the percentage of cases reported to have occurred among males remained consistent at 51.2% (3,293 of 6,421) for 2006, 49.6% (5,745 of 11,582) for 2007, and 49.7% (5,181 of 10,415) for 2008 (Table 2).
The majority of cases for which data on race were available for 2006--2008 occurred among whites, followed by blacks, Asians/Pacific Islanders, and American Indians/Alaska Natives (Table 2). However, data on race were lacking for 26.7%--32.5% of total annual case reports. Of patients for whom data on ethnicity were reported, 9.4%--15.4% were reported to be Hispanic (Table 2). However, data on ethnicity were lacking for 38%--44% of total annual case reports for 2006--2008.
A tenfold increase in reported cryptosporidiosis cases by illness onset date occurred during June--October compared with January--March (Figure 3). Age-specific analysis indicated that the seasonality in onset of illness was exhibited across all age groups, particularly among children aged 1--4 and 5--9 years (Figure 4).
The increase in cryptosporidiosis cases reported during 2006--2008 is a continuation of the fourfold increase in cryptosporidiosis since 2005 (Figure 5). This coincides with a similar dramatic rise in the number of cryptosporidiosis outbreaks associated with recreational water (Figure 6). During 1988--2006, Cryptosporidium was identified as the causal agent of 41.8% (100 of 239) of reported recreational water-associated outbreaks and of 5.7% (13 of 229) of reported drinking water-associated outbreaks of gastroenteritis in the United States (15,27--39).
Discussion
National cryptosporidiosis surveillance data are used to assess the epidemiologic characteristics and disease burden of cryptosporidiosis in the United States. The total number of cases reported annually and disease incidence increased during 2006--2008 and has increased dramatically since 2004 (Figures 1 and 5). Whether this increase reflects changes in reporting patterns and diagnostic testing practices or an actual change in infection and disease caused by Cryptosporidium is unclear but was clearly influenced by outbreak-related case reporting (Figure 6). However, outbreak-related probable case reporting does not account for the entire increase in reporting (Table 1). This increase also follows the introduction of nitazoxanide, the first licensed treatment for the disease, which was licensed in 2002 for children aged 1--11 years and in 2004 for children aged >11 years and adults (5). Because treatment for cryptosporidiosis now is available, health-care providers might be more willing to request Cryptosporidium testing, leading to an increase in subsequent case reports. However, no data exist to support this hypothesis. The geographic variation, age distribution, and late-summer through early-fall seasonality were consistent with previous cryptosporidiosis surveillance summaries (20--22).
Cryptosporidiosis is widespread geographically in the United States. Whereas previous surveillance data indicated that the diagnosis or reporting of cryptosporidiosis might be higher in northern or midwestern states (20--22), data from 2006--2008 seem to indicate that cryptosporidiosis incidence has increased in all states in recent years (Figure 1). Interpretation of this observation is difficult, and whether this change reflects an improvement in the diagnostics or detection by reporting systems of those states or represents an actual increase in the number of cases is unclear. Varying cryptosporidiosis surveillance systems and differences in reporting among states might affect the capability to detect and report cases.
Although cryptosporidiosis affects persons in all age groups, the number of reported cases was highest among children aged 1--9 years and adults aged 25--39 years (Figure 2). These data are consistent with reports of cryptosporidiosis incidence being higher among younger children and of transmission to their caregivers (e.g., child care staff, family members, and other household contacts) (18,20,21,40,41). Because information regarding immune system status is not collected as part of NNDSS cryptosporidiosis reporting, the number of immunosuppressed persons aged 25--39 years included in these surveillance data is unknown. However, the introduction of HAART therapy for persons with AIDS has decreased the incidence of cryptosporidiosis and the amount of severe cryptosporidiosis being diagnosed among persons with AIDS in the United States (4,42).
The tenfold increase in onset of cryptosporidiosis occurring during summer through early fall (Figure 3) is not unexpected. This increase coincides with increased swimming activities during the summer recreational water season and likely reflects the contribution of recreational water venues in the transmission of Cryptosporidium, particularly among younger children (15,27,29,31--38,43). Cryptosporidium is the leading cause of reported recreational water-associated outbreaks of gastroenteritis (38). Transmission through recreational water is facilitated by the substantial number of Cryptosporidium oocysts that can be shed by a single person; the extended periods of time that oocysts can be shed (11,12); the low infectious dose (9,10); the tolerance of Cryptosporidium oocysts to chlorine (44); and the prevalence of improper pool maintenance (i.e., insufficient disinfection, filtration, and recirculation of water), particularly of children's wading pools (45). This seasonal variation also has been noted in state, Canadian provincial, and previous U.S. national surveillance data for cryptosporidiosis and giardiasis (20--22,40,41,46--48).
The marked seasonal variation, higher incidence among children, and link to recreational water use for cryptosporidiosis is highlighted by the large communitywide outbreak in Utah in 2007 (26). The Utah Department of Health reported 1,901 confirmed cryptosporidiosis cases during June--December 2007, compared with the state's normal annual median of 16 confirmed cases. The full magnitude of the outbreak was likely much larger as investigations were limited to laboratory-confirmed cases. Epidemiologic studies implicated multiple recreational water venues as the source of this outbreak, and 80% of patients reported attending recreational water venues within 14 days of illness onset. In addition, 20% of patients reported swimming while ill with diarrhea, which implicated recreational water venues as an ongoing source of Cryptosporidium transmission. Children aged <5 years represented 32% of patients (median age: 9 years). After the infection rate peaked in mid-August, with nearly 60 confirmed cases of reported onset of illness on a single day, the Utah Department of Health further intensified control efforts, including hyperchlorination of pools and banning of children aged <5 years from community pools. Disease incidence rates began to decline after the stricter control measures and then continued to decline with the closing of seasonal pools in September. As the outbreak progressed, more patients reported having no recreational water exposure but had contact with persons who were ill with diarrhea. This finding supports a role for secondary person-to-person transmission in communitywide outbreaks. The lack of appropriate stool specimens prevented genotyping, which would have aided in determining chains of transmission. Although the water venues were filtered and chlorinated, the treatment was not sufficient to inactivate Cryptosporidium, which is highly chlorine tolerant. After implementation of hyperchlorination and banning of potentially incontinent children from swimming, followed by the closure of community pools at the end of the season, the outbreak began to decline. For 2008, Utah launched an education effort for swimmers and pool operators using multiple media combined with enhanced cryptosporidiosis surveillance and prevention efforts; only 49 cryptosporidiosis cases were reported in 2008 (Table 1).
Outbreak reports reflecting the multiple routes of transmission for Cryptosporidium also were reported during 2006--2008. Twelve cryptosporidiosis outbreaks associated with food, animal contact, or person-to-person transmission were reported to CDC during this period; these outbreaks affected >125 persons (49,50). Six outbreaks were associated with animal exposure, three involved unknown exposure in the home, one was associated with a restaurant, and one was associated with a child care facility. The remaining outbreak involved increased reporting of cryptosporidiosis cases in Colorado, which involved multiple risk factors. Investigation determined that ill persons were more likely to have swallowed untreated water from a lake, river, or stream; have had exposure to recreational water; or have had contact with a child in a child care program or in diapers (51).
Cryptosporidiosis (as with all diseases caused by enteric pathogens) is likely underreported because 1) not all infected persons are symptomatic, 2) those who are symptomatic do not always seek medical care (52,53), 3) health-care providers infrequently include laboratory diagnostics in their evaluation of nonbloody diarrheal diseases (52), 4) the majority of physicians do not specifically request testing for Cryptosporidium as part of ova and parasite testing (54), 5) a majority of laboratories do not test for Cryptosporidium unless it is specifically requested (55), and 6) case-reports are not always completed for positive laboratory results or forwarded to public health officials (56). The licensing of the first treatment for cryptosporidiosis (5) might influence health-care providers to request Cryptosporidium testing more often when ova and parasite exams are ordered. Its low infectious dose (9), protracted communicability (11,12), and chlorine tolerance (44) make Cryptosporidium ideally suited for transmission through drinking and recreational water, food, and both person-to-person and animal-to-person contact. Several studies have characterized risk factors associated with Cryptosporidium. Persons at increased risk for infection include 1) those who have contact with infected animals, 2) those who have ingested contaminated recreational (e.g., lake, river, pool, or hot tub) or drinking water, 3) close contacts of infected persons (e.g., those in the same family or household or in child care settings), and 4) travelers to disease-endemic areas (1,43,57--59).
In recent years, three studies conducted in the United States, the United Kingdom, and Australia used multivariate analysis to identify risk factors associated with sporadic cryptosporidiosis. The important risk factors found in these studies included contact with persons with diarrhea, particularly incontinent persons such as young children, and contact with cattle, especially calves (43,58,59). The U.S. (43) and U.K. (59) studies also identified travel abroad as a risk factor whereas the Australian (58) study excluded persons who had recently traveled abroad to better characterize endemic disease. In addition, the U.S. study identified swimming in fresh water as a risk factor for becoming ill with cryptosporidiosis, and the U.K. and Australian studies identified drinking unboiled water from rural sources as a risk factor.
Several additional studies have identified contact with cattle as a significant risk factor for sporadic cryptosporidiosis. During a foot-and-mouth disease outbreak in the United Kingdom in 2001, millions of animals were slaughtered, and access to the countryside was restricted. During this time, the counties with the heaviest restrictions experienced an 82% reduction in the number of cryptosporidiosis cases reported, particularly in the transmission peak temporally corresponding with the spring calving season, suggesting an association between cattle contact and human disease in the United Kingdom (60). During 2003--2005, genotyping was performed on samples from 49 sporadic human cases of cryptosporidiosis in Wisconsin. Zoonotic genotypes C. parvum and the cervine type were identified in 46 of 49 cases. Nine different subgenotypes of C. parvum were identified, all of which had been previously identified in cattle in the surrounding region (61). Wisconsin has a high rate of cryptosporidiosis disease, but very few cases are associated with outbreaks (Table 1). Sporadic cryptosporidiosis caused by zoonotic transmission from cattle is the likely main cause of this disease in Wisconsin (61).
Non--C. parvum or C. hominis Cryptosporidium species are associated less frequently with human infection. The avian pathogen C. meleagridis is emerging as an important zoonotic pathogen in immune-competent individuals in some communities. In Peru, where a significant number of infections are attributable to zoonotic transmission, 10%--20% of infections are caused by C. meleagridis (62). However, C. meleagridis is detected rarely in immune-competent patients in industrialized countries (63, 64).
Cryptosporidium cannot multiply in food, so transmission of the parasite through food usually occurs through direct contamination of the food by an ill person or fecal contamination caused by improper hygiene practices during food production, processing, or preparation. Limited outbreaks have been associated with nonpasteurized apple cider made from improperly cleaned fruit that was exposed to cattle feces in the orchard (17,65). A 1998 outbreak involving 88 persons in the District of Columbia was traced back to contaminated food that had been handled by a cafeteria worker who was sick with cryptosporidiosis (16). The food handler had recently spent some time with a young relative who was sick with vomiting and diarrhea and another relative who also had become ill with the same symptoms (16). Cryptosporidium oocysts have been detected on produce at markets (66,67). These vegetables were likely contaminated by Cryptosporidium-contaminated water used for irrigation or by the feces of wild animals with access to the fields (68,69). Despite the possibility of produce contamination at the farm level, the link between detection of Cryptosporidium on fresh produce and human infection is not well understood (70). In contrast, case-control studies among persons with sporadic cryptosporidiosis cases have determined that consumption of raw vegetables, particularly carrots, is a protective factor (43,58,59). This finding might be explained by repeated exposures to the small amounts of Cryptosporidium on the vegetables providing a protective immunity or high fiber in the diet increasing gut motility and thereby preventing the oocysts from invading the intestinal mucosa (43).
Water appears to be a more important transmission route for Cryptosporidium and frequently is implicated in cryptosporidiosis outbreaks and in studies of sporadic cases (42,43) (Figure 6). Risk factors for cryptosporidiosis associated with treated recreational water include fecal accidents in the pool, diapered toddlers in the pool, swimming while ill with diarrhea, and swallowing pool water (38,58). Risk factors for cryptosporidiosis associated with drinking water include drinking large amounts of unboiled rural or well water and failure of treatment protocols for public water supplies (58).
Although no formalized national plan exists for preventing cryptosporidiosis in the United States, multiple efforts are focused on reducing the transmission of the parasite through the two major routes of waterborne transmission. For drinking water, the Environmental Protection Agency (EPA) has implemented multiple regulations designed to improve the safety of surface water (e.g., lakes and rivers) supplies, including multiple regulatory changes following an outbreak of cryptosporidiosis in 1993 in Milwaukee, Wisconsin, that sickened >400,000 persons using the city water supply (34,71). Since 1993, no Cryptosporidium outbreaks associated with use of community surface water supplies have occurred in the United States (28,30--34,39). In addition, a study conducted during 1996--2004 in the United Kingdom suggests that improvements in drinking water treatment and source water protection might be responsible for decreasing the number of cryptosporidiosis cases in humans caused by C. parvum from ruminants (72,73). EPA is implementing the Groundwater Rule in an effort to decrease the risk associated with use of groundwater (well) supplies (39). This regulatory change might decrease the occurrence of Cryptosporidium outbreaks associated with groundwater use.
For recreational water, Cryptosporidium remains the leading cause of diarrheal illness outbreaks, especially in chlorinated venues (38). Recently, cryptosporidiosis outbreaks that began in treated recreational water venues have spread to communitywide transmission in multiple venues (e.g., child care centers and schools) (26). In addition, limited outbreaks in child care centers or schools can be amplified into communitywide outbreaks by the use of recreational water by ill persons (74). To address these challenges, CDC has collaborated with state health departments to develop guidelines for rapidly implementing community control measures when a cryptosporidiosis outbreak is identified (26). Efforts to reduce the transmission of this chlorine-tolerant pathogen in pools will require a concerted effort to move beyond existing pool practices to include new secondary disinfection technology (ultraviolet light or ozone inactivation), operational improvements (use of filtration enhancements that improve Cryptosporidium removal), and public education to reduce continued swimming by persons who are ill with diarrhea.
In the United States, no federal oversight of chlorinated swimming venues occurs. All pool codes are reviewed and approved by state or local public health officials. As a result, the United States has no uniform national standards governing the design, construction, operation, and maintenance of swimming pools and other treated recreational water venues. To provide guidance and improve nationwide pool code uniformity, CDC is sponsoring an effort to develop a data-driven, knowledge-based National Model Aquatic Health Code (available at http://www.cdc.gov/healthywater/swimming/pools/mahc/). This effort involves state, local, and federal public health officials and the aquatics industry in creating a voluntary model regulatory structure for state and local health departments to use in developing pool codes. Health communication efforts also should continue to educate swimmers about the hazards of swallowing pool water and swimming while ill with diarrhea.
Limitations
The data provided in this report are subject to certain limitations, including likely underreporting of cases, lack of information on race and ethnicity on most case reports, unknown HIV status, and lack of information on risk factors or attributable fractions by exposure types. Despite these limitations, these data provide the only national estimate of the number of cases of cryptosporidiosis that is available.
Conclusion
Continued efforts to reduce risk and improve diagnosis and reporting of cryptosporidiosis are needed to decrease the transmission of cryptosporidiosis in the United States. Prevention measures (Box 1) and measures to improve surveillance and prevention for cryptosporidiosis and increase understanding of its epidemiology and the associated disease burden (Box 2) have been recommended. Additional information about cryptosporidiosis epidemiology, diagnosis, treatment, prevention, and control is available at http://www.cdc.gov/crypto.
Acknowledgments
This report is based, in part, on contributions by jurisdiction surveillance coordinators; Ruth Ann Jajosky, DMD, Office of Surveillance, Epidemiology, and Laboratory Services (proposed); Michele Hlavsa, MPH, Virginia Roberts, MPH, Division of Foodborne, Waterborne, and Environmental Diseases (proposed), National Center for Emerging and Zoonotic Infectious Diseases (proposed), CDC.
References
- Chen X-M, Keithly JS, Paya CV, LaRusso NF. Cryptosporidiosis. N Engl J Med 2002;346:1723--31.
- Hellard ME, Sinclair MI, Hogg GG, Fairley CK. Prevalence of enteric pathogens among community based asymptomatic individuals. Gastroenterol Hepatol 2000;15:290--3.
- Hunter PR, Nichols G. Epidemiology and clinical features of Cryptosporidium infection in immunocompromised patients. Clin Microbiol Rev 2002;15:145--54.
- Kaplan JE, Hanson D, Dworkin MS, et al. Epidemiology of human immunodeficiency virus-associated opportunistic infections in the United States in the era of highly active antiretrorviral therapy. Clin Infect Dis 2000 (Suppl);30:S5--S14.
- Fox LM, Saravolatz LD. Nitazoxanide: a new thiazolide antiparasitic agent. Clin Infect Dis 2005;40:1173--80.
- Huang DB, Chappell C, Okhuysen PC. Cryptosporidiosis in children. Semin Pediatr Infect Dis 2004;15:253--9.
- Xiao L, Fayer R, Ryan U, Upton SJ. Cryptosporidium taxonomy: recent advances and implications for public health. Clin Microbiol Rev 2004;17:72--97.
- Cama VA, Bern C, Roberts J, et al. Cryptosporidium species and subtypes and clinical manifestations in children, Peru. Emerg Infect Dis 2008;14:1567--74.
- DuPont HL, Chappell CL, Sterling CR, Okhuysen PC, Rose JB, Jakubowski W. The infectivity of Cryptosporidium parvum in healthy volunteers. N Engl J Med 1995;332:855--9.
- Okhuysen PC, Chappell CL, Crabb JH, Sterling CR, DuPont HL. Virulence of three distinct Cryptosporidium parvum isolates for healthy adults. J Infect Dis 1999;180:1275--81.
- Chappell CL, Okhuysen PC, Sterling CR, DuPont HL. Cryptosporidium parvum: intensity of infection and oocyst excretion patterns in healthy volunteers. J Infect Dis 1996;173:232--6.
- Jokipii L, Jokipii AMM. Timing of symptoms and oocyst excretion in human cryptosporidiosis. N Engl J Med 1986;315:1643--7.
- CDC. Cryptosporidiosis prevention. Atlanta, GA: US Department of Health and Human Services, CDC; 2010. Available at http://www.cdc.gov/crypto/gen_info/prevent.html. Accessed May 13, 2010.
- D'Antonio RG, Winn RE, Taylor JP, et al. A waterborne outbreak of cryptosporidiosis in normal hosts. Ann Intern Med 1985;103(6 Pt 1):886--8.
- CDC. Swimming-associated cryptosporidiosis---Los Angeles County. MMWR 1990;39:343--5.
- Quiroz ES, Bern C, MacArthur JR, et al. An outbreak of cryptosporidiosis linked to a foodhandler. J Infect Dis 2000;181:695--700.
- Millard PS, Gensheimer KF, Addiss DG, et al. An outbreak of cryptosporidiosis from fresh-pressed apple cider. JAMA 1994; 272:1592--6.
- Cordell RL, Addiss DG. Cryptosporidiosis in child care settings: a review of the literature and recommendations for prevention and control. Pediatr Infect Dis J 1994;13:310--7.
- Ashbolt RH, Coleman DJ, Misrachi A, Conti JM, Kirk MD. An outbreak of cryptosporidiosis associated with an animal nursery at a regional fair. Commun Dis Intell 2003;27:244--9.
- Deitz VJ, Roberts JM. National surveillance for infection with Cryptosporidium parvum, 1995--1998: what have we learned? Public Health Rep 2000;115:358--63.
- Hlavsa MC, Watson JC, Beach MJ. Cryptosporidiosis surveillance---United States, 1999--2002. In: Surveillance Summaries, January 28, 2004. MMWR 2004;54(No. SS-1):1--8.
- Yoder JS, Beach MJ. Cryptosporidiosis surveillance---United States, 2003--2005. In: Surveillance Summaries, September 7, 2007. MMWR 2007;56(No. SS-7):1--10.
- CDC. Cryptosporidiosis (Cryptosporidium) case definition. Atlanta, GA: US Department of Health and Human Services, CDC; 2010. Available at http://www.cdc.gov/ncphi/disss/nndss/casedef/cryptosporidiosis_2009.htm. Accessed May 13, 2010.
- Arrowood MJ. Diagnosis. In: Fayer R, ed. Cryptosporidium and cryptosporidiosis. Boca Raton, FL; CRC press; 1997:43.
- Johnston SP, Ballard MM, Beach MJ, Causer L, Wilkins PP. Evaluation of three commercial assays for detection of Giardia and Cryptosporidium organisms in fecal specimens. J Clin Microbiol 2003;41:623--6.
- CDC. Communitywide cryptosporidiosis outbreak---Utah, 2007. MMWR. 2008;57:989--93.
- Dziuban EJ, Liang JL, Craun GF, et al. Surveillance for waterborne disease and outbreaks associated with recreational water---United States, 2003--2004. In: Surveillance Summaries, December 22, 2006. MMWR 2006;55(No. SS-12):1--30.
- Liang JL, Dziuban EJ, Craun GF, et al. Surveillance for waterborne disease and outbreaks associated with drinking water and water not intended for drinking---United States, 2003--2004. In: Surveillance Summaries, December 22, 2006. MMWR 2006;55(No. SS-12):31--65.
- Yoder JS, Blackburn BG, Craun GF, et al. Surveillance for waterborne-disease outbreaks associated with recreational water---United States, 2001--2002. In: Surveillance Summaries, October 22, 2004. MMWR 2004;53(No. SS-8):1--21.
- Blackburn BG, Yoder JS, Craun GF, et al. Surveillance for waterborne-disease outbreaks associated with drinking water---United States, 2001--2002. In: Surveillance Summaries, October 22, 2004. MMWR 2004;53(No. SS-8):23--45.
- Lee SH, Levy DA, Craun GF, Beach MJ, Calderon RL. Surveillance for waterborne-disease outbreaks---United States, 1999--2000. In: Surveillance Summaries, November 22, 2002. MMWR 2002;51(No. SS-8):1--48.
- Barwick RS, Levy DA, Craun GF, Beach MJ, Calderon RL. Surveillance for waterborne-disease outbreaks---United States, 1997--1998. In: Surveillance Summaries, May 26, 2000. MMWR 2000;49(No. SS-4):1--35.
- Levy DA, Bens MS, Craun GF, Calderon RL, Herwaldt BL. Surveillance for waterborne-disease outbreaks---United States, 1995--1996. In: Surveillance Summaries, December 11, 1998. MMWR 1998;47(No. SS-5):1--34.
- Kramer MH, Herwaldt BL, Craun GF, Calderon RL, Juranek DD. Surveillance for waterborne-disease outbreaks---United States, 1993--1994. In: Surveillance Summaries, April 12, 1996. MMWR 1996;45(No. SS-1):1--33.
- Moore AC, Herwaldt BL, Craun GF, Calderon RL, Highsmith AK, Juranek DD. Surveillance for waterborne disease outbreaks---United States, 1991--1992. In: Surveillance Summaries, November 11, 1993. MMWR 1993:42(No. SS-5):1--22.
- Herwaldt BL, Craun GF, Stokes SL, Juranek DD. Waterborne-disease outbreaks, 1989--1990. In: Surveillance Summaries, December 1, 1991. MMWR 1991:40(No. SS-3):1--21.
- Levine WC, Stephenson WT, Craun GF. Waterborne disease outbreaks, 1986--1988. In: Surveillance Summaries, March 1, 1990. MMWR 1990; 39(No. SS-1):1--13.
- Yoder JS, Hlavsa M, Craun GF, et. al. Surveillance for waterborne disease and outbreaks associated with recreational water use and other aquatic facility-associated health events---United States, 2005--2006. In: Surveillance Summaries, September 12, 2008. MMWR 2008;57(No. SS-9):1--38.
- Yoder JS, Roberts V, Craun GF, et al. Surveillance for waterborne disease and outbreaks associated with drinking water and water not intended for drinking --- United States, 2005--2006. In: Surveillance Summaries, September 12, 2008. MMWR 2008;57 (No. SS-9):39--69.
- Naumova EN, Chen JT, Griffiths JK, Matyas BT, Estes-Smargiassi SA, Morris RD. Use of passive surveillance data to study temporal and spatial variation in the incidence of giardiasis and cryptosporidiosis. Public Health Rep 2000;115:436--47.
- Majowicz SE, Michel P, Aramini JJ, McEwen SA, Wilson JB. Descriptive analysis of endemic cryptosporidiosis cases reported in Ontario 1996--1997. Can J Public Health 2001;92:62--6.
- Aragón TJ, Novotny S, Enanoria W, Vugia DJ, Khalakdina A, Katz MH. Endemic cryptosporidiosis and exposure to municipal tap water in persons with acquired immunodeficiency syndrome (AIDS): a case-control study. BMC Public Health 2003;3:2.
- Roy SL, DeLong SM, Stenzel S, et al. Risk factors for sporadic cryptosporidiosis among immunocompetent persons in the United States from 1999 to 2001. J Clin Microbiol 2004;42:2944--51.
- Shields JM, Hill VR, Arrowood MJ, Beach MJ. Inactivation of Cryptosporidium parvum under chlorinated recreational water conditions. J Water Health 2008 6:513--20.
- CDC. Violations identified from routine swimming pool inspections---selected states and counties, United States, 2008. MMWR 2010;59:582--7.
- Furness BW, Beach MJ, Roberts JM. Giardiasis surveillance, United States, 1992--1997. In: Surveillance Summaries, August 11, 2000. MMWR 2000;49(No. SS-7):1--13.
- Hlavsa MC, Watson JC, Beach MJ. Giardiasis surveillance---United States, 1998--2002. In: Surveillance summaries, January 28, 2004. MMWR 2004;54(No. SS-1):9--16.
- Yoder JS, Beach MJ. Giardiasis surveillance---United States, 2003--2005. In: Surveillance Summaries, September 7, 2007. MMWR 2007;56(No. SS-7):11--8.
- CDC. Annual listing of foodborne disease outbreaks, United States. Atlanta, GA: US Department of Health and Human Services, CDC; 2010. Available at www.cdc.gov/outbreaknet/surveillance_data.html. Accessed May 13, 2010.
- CDC, National Association of State Public Health Veterinarians. Compendium of measures to prevent disease associated with animals in public settings, 2009. MMWR 2009;58(No. RR-5).
- Valderrama AL, Hlavsa MC, Cronquist A, et al. Multiple risk factors associated with a large statewide increase in cryptosporidiosis. Epidemiol Infect 2009;137:1781--8.
- Scallan E, Jones TF, Cronquist A, et al. Factors associated with seeking medical care and submitting a stool sample in estimating the burden of foodborne illness. Foodborne Pathog Dis 2006;3:432--8.
- Voetsch AC, Van Gilder TJ, Angulo FJ, et al. FoodNet estimate of the burden of illness caused by nontyphoidal Salmonella infections in the United States. Clin Infect Dis 2004;38(Suppl):S127--S134.
- Berger M, Weintraub JM. Testing patterns for cryptosporidiosis: a survey of physicians in three California counties. San Francisco, CA. San Francisco Department of Public Health; 2005. Available at http://www.sfphes.org/water/crypto/Cryptosporidiosis_Testing_Patterns_Among_Physicians.pdf. Accessed May 13, 2010.
- Jones JL, Lopez A, Wahlquist SP, Nadle J, Wilson M. Survey of clinical laboratory practices for parasitic diseases. 1. Clin Infect Dis 2004;38(Suppl):S198--S202.
- Mead PS, Slutsker L, Dietz V, et al. Food-related illness and death in the United States. Emerg Infect Dis 1999;5:607--25.
- Goh S, Reacher M, Casemore DP, et al. Sporadic cryptosporidiosis, North Cumbria, England, 1996--2000. Emerg Infect Dis 2004;10:1007--15.
- Robertson B, Sinclair MI, Forbes AB, et al. Case-control studies of sporadic cryptosporidiosis in Melbourne and Adelaide, Australia. Epidemiol Infect 2002;128:419--31.
- Hunter PR, Hughes S, Woodhouse S, et al. Sporadic cryptosporidiosis case-control study with genotyping. Emerg Infect Dis 2004;10:1241--9.
- Hunter PR, Chalmers RM, Syed Q, Hughes LS, Woodhouse S, Swift L. Foot and mouth disease and cryptosporidiosis: possible interaction between two emerging infectious diseases. Emerg Infect Dis 2003;9:109--12.
- Feltus DC, Giddings CW, Schneck BL, Monson T, Warshauer D, McEvoy JM. Evidence supporting zoonotic transmission of Cryptosporidium spp. in Wisconsin. J Clin Microbiol 2006;44:4303--8.
- Xiao L, Bern C, Limor J, et al. Identification of 5 types of Cryptosporidium parasites in children in Lima, Peru. J Infect Dis 2001;183:492--7.
- Leoni F, Amar C, Nichols G, Pedraza-Díaz S, McLauchlin J. Genetic analysis of Cryptosporidium from 2414 humans with diarrhoea in England between 1985 and 2000. J Med Microbiol 2006;55:703--7.
- Xiao L, Feng Y. Zoonotic cryptosporidiosis. FEMS Immunol Med Microbiol 2008;52:309--23.
- Blackburn BG, Mazurek JM, Hlavsa M, et al. Cryptosporidiosis associated with ozonated apple cider. Emerg Infect Dis 2006;12:684--6.
- Robertson LJ, Gjerde B. Occurrence of parasites on fruits and vegetables in Norway. J Food Prot 2001;64:1793--8.
- Ortega YR, Roxas CR, Gilman RH, et al. Isolation of Cryptosporidium parvum and Cyclospora cayetanensis from vegetables collected in markets of an endemic region in Peru. Am J Trop Med Hyg 1997;57:683--6.
- Thurston-Enriquez JA, Watt P, Dowd SE, Enriquez R, Pepper IL, Gerba CP. Detection of protozoan parasites and microsporidia in irrigation waters used for crop production. J Food Prot 2002;65:378--82.
- Chaidez C, Soto M, Gortares P, Mena K. Occurrence of Cryptosporidium and Giardia in irrigation water and its impact on the fresh produce industry. Int J Environ Health Res 2005;15:339--45.
- Gale P. Land application of treated sewage sludge: quantifying pathogen risks from consumption of crops. J Appl Microbiol 2005;98:380--96.
- Mac Kenzie WR, Hoxie NJ, Proctor ME, et al. A massive outbreak in Milwaukee of Cryptosporidium infection transmitted through the public water supply. N Engl J Med 1994;331:161--7. Erratum in: N Engl J Med 1994;331:1035.
- Lake IR, Nichols G, Bentham G, Harrison FC, Hunter PR, Kovats SR. Cryptosporidiosis decline after regulation, England and Wales, 1989--2005. Emerg Infect Dis 2007;13:623--5.
- Sopwith W, Osborn K, Chalmers R, Regan M. The changing epidemiology of cryptosporidiosis in North West England. Epidemiol Infect 2005;133:785--93.
- Turabelidze G, Lin M, Weiser T, Zhu BP. Communitywide outbreak of cryptosporidiosis in rural Missouri associated with attendance at child care centers. Arch Pediatr Adolesc Med 2007;161:878--83.
FIGURE 1. Incidence* of cryptosporidiosis, by state --- National Notifiable Disease Surveillance System, United States, 2005--2008
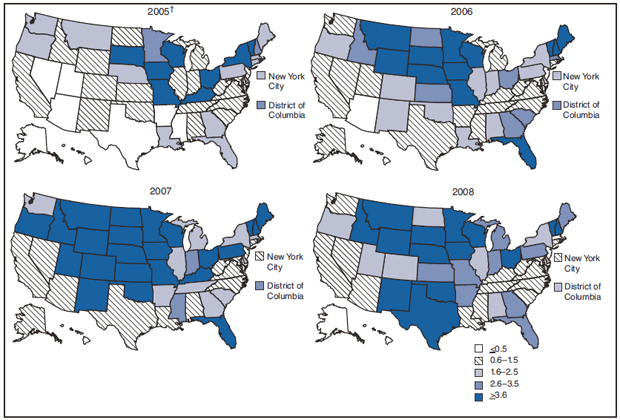
* Per 100,000 population.
† Source: Yoder JS, Beach MJ. Cryptosporidiosis surveillance---United States, 2003--2005. In: Surveillance Summaries, September 7, 2007. MMWR 2007;56(No. SS-7):1--10.
Alternate Text: The figure shows maps of the United States for four years indicating incidence of reported cases of cryptosporidiosis per 100,000 population. Incidence was generally highest in the northern states.
FIGURE 2. Number* of cryptosporidiosis case reports, by age group and year --- National Notifiable Disease Surveillance System, United States, 2006--2008
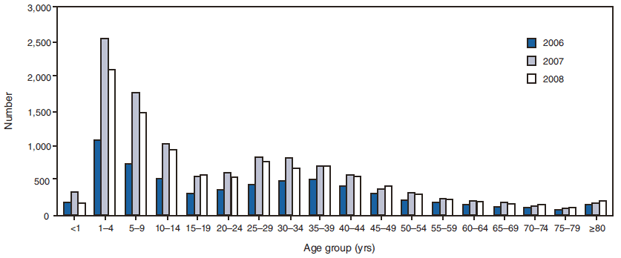
* N = 28,636; age for 332 case-patients was unknown.
Alternate Text: The figure shows the number of cryptosporidiosis case reports broken out by age group and year. The number of case reports was highest for children aged 1-4 years and 5-9 years compared with other age groups.
FIGURE 3. Number* of cryptosporidiosis case reports, by date of illness onset --- National Notifiable Disease Surveillance System, United States, 2006--2008
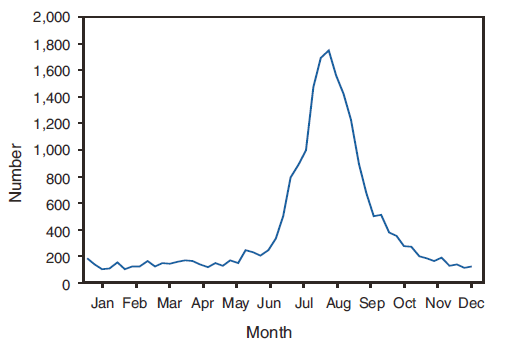
* N = 28,636; date of onset for 7,017 case-patients was unknown.
Alternate Text: The figure shows the number of cryptosporidiosis case reports by month. The greatest number of case reports occur during the summer months.
FIGURE 4. Number* of cryptosporidiosis case reports, by selected age group† and date of illness onset --- National Notifiable Disease Surveillance System, United States, 2006--2008
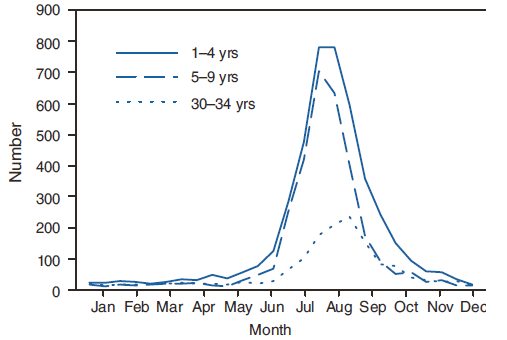
* N = 9,166.
† The 1--4- and 5--9-year age groups are presented because they have the highest numbers of cryptosporidiosis case reports and have the greatest seasonality. The 30--34-year age group was chosen to illustrate the less pronounced seasonality of the other age groups.
Alternate Text: The figure shows the number of cryptosporidiosis case reports by age group and date of illness onset. The 1-4- and 5-9-year age groups have the highest numbers of cryptosporidiosis case reports and have the greatest seasonality. The greatest number of case reports occur during the summer months.
FIGURE 5. Incidence* of cryptosporidiosis, by year --- National Notifiable Disease Surveillance System, United States, 1995--2008†
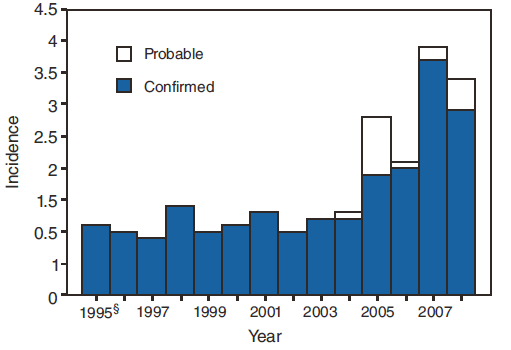
* Per 100,000 population.
† N = 68,907.
§ First full year of national reporting.
Alternate Text: The figure shows the incidence of cryptosporidiosis per 100,000 population by year. Incidence increased dramatically in 2007 and 2008.
FIGURE 6. Number* of outbreaks of cryptosporidiosis associated with water, by water type --- Waterborne Disease and Outbreak Surveillance System, United States, 1988--2008
![The figure shows the number of cryptosporidiosis outbreaks associated with water by water type. Treated recreational water (i.e., water that has undergone a treatment process [e.g., chlorination and filtration] to make it safe for recreation) was associated with the greatest number of outbreaks.](figures/s5906a1f6.gif)
* N = 172.
† Water that has undergone a treatment process (e.g., chlorination and filtration) to make it safe for recreation.
§ Data for 2007 and 2008 are provisional.
Alternate Text: The figure shows the number of cryptosporidiosis outbreaks associated with water by water type. Treated recreational water (i.e., water that has undergone a treatment process [e.g., chlorination and filtration] to make it safe for recreation) was associated with the greatest number of outbreaks.
|
BOX 1. CDC recommendations to prevent and control cryptosporidiosis |
|
Practice good hygiene.
Additional information about hygiene is available at http://www.cdc.gov/healthywater/hygiene.
Additional information about recreational water illnesses and how to stop them from spreading is available at http://www.cdc.gov/healthywater/swimming.
Additional information about cryptosporidiosis prevention and control is available at http://www.cdc.gov/crypto/gen_info/prevent.html. Avoid water that might be contaminated.
Additional information about water filters is available at http://www.cdc.gov/crypto/gen_info/filters.html. Avoid eating food that might be contaminated.
Information about how to prevent illnesses while traveling is available at http://wwwnc.cdc.gov/travel/content/safe-food-water.aspx. Prevent contact and contamination with feces during sex.
|
Use of trade names and commercial sources is for identification only and does not imply endorsement by the U.S. Department of
Health and Human Services.
References to non-CDC sites on the Internet are
provided as a service to MMWR readers and do not constitute or imply
endorsement of these organizations or their programs by CDC or the U.S.
Department of Health and Human Services. CDC is not responsible for the content
of pages found at these sites. URL addresses listed in MMWR were current as of
the date of publication.
All MMWR HTML versions of articles are electronic conversions from typeset documents.
This conversion might result in character translation or format errors in the HTML version.
Users are referred to the electronic PDF version (http://www.cdc.gov/mmwr)
and/or the original MMWR paper copy for printable versions of official text, figures, and tables.
An original paper copy of this issue can be obtained from the Superintendent of Documents, U.S.
Government Printing Office (GPO), Washington, DC 20402-9371;
telephone: (202) 512-1800. Contact GPO for current prices.
**Questions or messages regarding errors in formatting should be addressed to
mmwrq@cdc.gov.


