 |
|
|
|
|
|
|
| ||||||||||
|
|
|
|
|
|
|
||||
| ||||||||||
|
|
|
|
|
Persons using assistive technology might not be able to fully access information in this file. For assistance, please send e-mail to: mmwrq@cdc.gov. Type 508 Accommodation and the title of the report in the subject line of e-mail. Surveillance for Waterborne Disease and Outbreaks Associated with Drinking Water and Water not Intended for Drinking --- United States, 2003--2004Jennifer L. Liang, DVM1,2
Corresponding author: Jennifer L. Liang, DVM, Division of Parasitic Diseases, National Center for Zoonotic, Vector-Borne, and Enteric Diseases (proposed), 4770 Buford Hwy., NE, MS F-22, Atlanta, GA 30341. Telephone: 770-488-7781; Fax: 770-488-7761; E-mail: jliang@cdc.gov. AbstractProblem/Condition: Since 1971, CDC, the U.S. Environmental Protection Agency (EPA), and the Council of State and Territorial Epidemiologists have maintained a collaborative Waterborne Disease and Outbreaks Surveillance System for collecting and reporting data related to occurrences and causes of waterborne disease and outbreaks (WBDOs). This surveillance system is the primary source of data concerning the scope and effects of WBDOs in the United States. Reporting Period: Data presented summarize 36 WBDOs that occurred during January 2003--December 2004 and nine previously unreported WBDOs that occurred during 1982--2002. Description of System: The surveillance system includes data on WBDOs associated with drinking water, water not intended for drinking (excluding recreational water), and water of unknown intent. Public health departments in the states, territories, localities, and Freely Associated States (i.e., the Republic of the Marshall Islands, the Federated States of Micronesia, and the Republic of Palau, formerly parts of the U.S.-administered Trust Territory of the Pacific Islands) are primarily responsible for detecting and investigating WBDOs and voluntarily reporting them to CDC by using a standard form. Results: During 2003--2004, a total of 36 WBDOs were reported by 19 states; 30 were associated with drinking water, three were associated with water not intended for drinking, and three were associated with water of unknown intent. The 30 drinking water-associated WBDOs caused illness among an estimated 2,760 persons and were linked to four deaths. Etiologic agents were identified in 25 (83.3%) of these WBDOs: 17 (68.0%) involved pathogens (i.e., 13 bacterial, one parasitic, one viral, one mixed bacterial/parasitic, and one mixed bacterial/parasitic/viral), and eight (32.0%) involved chemical/toxin poisonings. Gastroenteritis represented 67.7% of the illness related to drinking water-associated WBDOs; acute respiratory illness represented 25.8%, and dermatitis represented 6.5%. The classification of deficiencies contributing to WBDOs has been revised to reflect the categories of concerns associated with contamination at or in the source water, treatment facility, or distribution system (SWTD) that are under the jurisdiction of water utilities, versus those at points not under the jurisdiction of a water utility or at the point of water use (NWU/POU), which includes commercially bottled water. A total of 33 deficiencies were cited in the 30 WBDOs associated with drinking water: 17 (51.5%) NWU/POU, 14 (42.4%) SWTD, and two (6.1%) unknown. The most frequently cited NWU/POU deficiencies involved Legionella spp. in the drinking water system (n = eight [47.1%]). The most frequently cited SWTD deficiencies were associated with distribution system contamination (n = six [42.9%]). Contaminated ground water was a contributing factor in seven times as many WBDOs (n = seven) as contaminated surface water (n = one). Interpretation: Approximately half (51.5%) of the drinking water deficiencies occurred outside the jurisdiction of a water utility in situations not currently regulated by EPA. The majority of the WBDOs in which deficiencies were not regulated by EPA were associated with Legionella spp. or chemicals/toxins. Problems in the distribution system were the most commonly identified deficiencies under the jurisdiction of a water utility, underscoring the importance of preventing contamination after water treatment. The substantial proportion of WBDOs involving contaminated ground water provides support for the Ground Water Rule (finalized in October 2006), which specifies when corrective action is required for public ground water systems. Public Health Actions: CDC and EPA use surveillance data to identify the types of water systems, deficiencies, and etiologic agents associated with WBDOs and to evaluate the adequacy of current technologies and practices for providing safe drinking water. Surveillance data also are used to establish research priorities, which can lead to improved water-quality regulation development. The growing proportion of drinking water deficiencies that are not addressed by current EPA rules emphasizes the need to address risk factors for water contamination in the distribution system and at points not under the jurisdiction of water utilities. IntroductionDuring 1920--1970, statistical data regarding U.S. waterborne-disease outbreaks were collected by researchers and federal agencies (1). Since 1971, CDC, the U.S. Environmental Protection Agency (EPA), and the Council of State and Territorial Epidemiologists (CSTE) have maintained a collaborative Waterborne Disease and Outbreak Surveillance System (WBDOSS) that tracks the occurrences and causes of waterborne disease and outbreaks (WBDOs) associated with drinking water. WBDOs associated with recreational water were added to the surveillance system in 1978 (2); WBDOs associated with occupational settings, water not intended for drinking (WNID)* and commercially bottled water were added in 1999 (3); and WBDOs associated with drinking water contaminated at the point of use, contaminated ice and beverages made with contaminated water, and beverages contaminated as a result of plumbing failures in drink mix/soda machines have been added to this report. This Surveillance Summary includes data from 30 WBDOs related to drinking water, three WBDOs related to WNID, and three WBDOs related to water of unknown intent (WUI). Nine previously unreported outbreaks also have been included in this report. Recreational water-associated disease and outbreaks have been presented in a separate report (4). This Surveillance Summary also introduces multiple changes in the WBDOSS to better characterize the breadth of waterborne-disease challenges in the United States. Waterborne disease and outbreak surveillance activities 1) characterize the epidemiology of WBDOs; 2) identify changing trends in the etiologic agents and other risk factors associated with WBDOs; 3) identify major deficiencies in providing safe drinking water; 4) encourage public health personnel to detect and investigate WBDOs; and 5) foster collaboration among local, state, federal, and international agencies on initiatives to prevent waterborne disease. Data from this surveillance system are useful for identifying major deficiencies in providing safe drinking water, can influence research priorities, and can lead to improved focus in water-quality regulation development. However, the statistics reported in this report represent only a portion of the burden of illness associated with water exposure. In general, the surveillance information does not include endemic, nonoutbreak-related waterborne-disease risks, and reliable estimates of the number of unrecognized WBDOs are not available. BackgroundU.S. Environmental Protection Agency Drinking Water RegulationsPublic water systems are regulated under the Safe Drinking Water Act (SDWA) of 1974 and its subsequent 1986 and 1996 amendments (Table 1) (5--7). SDWA authorizes EPA to set national standards to protect public drinking water and its sources against naturally occurring or man-made contaminants. Previously set standards by which microbial contamination is regulated include the Total Coliform Rule (TCR), Surface Water Treatment Rule (SWTR), Interim Enhanced SWTR (IESWTR), and Long Term 1 Enhanced SWTR (LT1ESWTR). In addition, EPA's lead, copper, and arsenic rules prescribe action levels at which a system must take corrective steps (8,9). These rules have been described in more detail in a previous report (3). All public water systems are required by TCR to monitor for total coliforms at a prescribed frequency (10,11). SWTR (12) and IESWTR (13) apply to public systems that serve >10,000 persons and surface water or ground water under the direct influence of surface water. These two rules are intended to protect the public against exposure to Giardia intestinalis, Cryptosporidium spp., viruses, Legionella spp., and other selected pathogens. LT1ESWTR applies to public systems that serve <10,000 persons and is intended to improve the control of microbial pathogens, especially Cryptosporidium spp. (14). An additional regulation, the Filter Backwash Recycling Rule, requires the return of recycle flows to the water treatment process so that microbial contaminant removal is not compromised (15). Recently finalized microbial and disinfection by-products regulations include the Long Term 2 Enhanced Surface Water Treatment Rule (LT2ESWTR) and the Stage 2 Disinfectants and Disinfection By-products Rule (DBPR2). These regulations were developed simultaneously to address risk tradeoffs between the control of pathogens and limiting exposure to disinfection by-products (DBPs) that can form in water from the disinfection process used to control microbial pathogens (16). LT2ESWTR (17,18) requires the use of treatment techniques and monitoring, reporting, and public notification for all public water systems that use surface water sources. Key provisions include the following: source water monitoring for Cryptosporidium spp.; additional treatment for filtered systems on the basis of source-water Cryptosporidium concentrations; inactivation of Cryptosporidium by all unfiltered systems; disinfection profiling and benchmarking to ensure continued levels of microbial protection while system operators take steps to comply with new DBP limits; and covering, treating, or implementing a risk management plan for uncovered finished water storage facilities. DBPR2 applies to all community and all nontransient, noncommunity water systems that use a disinfectant other than ultraviolet light (17). DBPR2 requires systems to meet maximum contaminant levels for total trihalomethanes and five haloacetic acids at each monitoring site in the distribution system, determine if they are experiencing short-term peaks in DBP levels, and better identify monitoring sites at which customers are exposed to high DBP levels. The 1996 SDWA amendments require EPA to develop regulations that mandate disinfection of public ground water systems, as necessary, to protect the public health. The Ground Water Rule (GWR) (finalized by EPA in October 2006) specifies when corrective action, including disinfection, is required to protect consumers from bacteria and viruses (19). Additional information is available at http://www.epa.gov/safewater/gwr.html. Requirements include periodic sanitary surveys to identify deficiencies, hydrogeologic sensitivity assessments for nondisinfected systems, source-water microbial monitoring from certain systems, and compliance monitoring for systems that disinfect to ensure adequate inactivation or removal of viruses. SDWA Wellhead Protection Program requires every state to develop a program to delineate wellhead protection areas in which sources of contamination are managed to minimize ground water contamination (19). Every 5 years, EPA is required to publish a list of contaminants that are known or anticipated to occur in public water systems and that might need to be regulated. The first drinking water Contaminant Candidate List (CCL1) was issued in 1998 and included 50 chemical and 10 microbial contaminants (20). However, EPA decided not to regulate Acanthamoeba, which was on the first list. The second Contaminant Candidate List 2 (CCL2) carried forward nine microbiologic contaminants from CCLl, excluding Acanthamoeba (21). EPA also must establish criteria for a program to monitor unregulated contaminants and publish a list of contaminants to be monitored (22--25). Microorganisms on this list include those for which analytical methods are available (Aeromonas) and those for which analytical methods are being developed (i.e., Helicobacter pylori, cyanobacteria, coxsackieviruses, microsporidia, adenoviruses, and caliciviruses). An ongoing screening survey for Aeromonas and selected chemical contaminants will help determine whether these should be considered for or excluded from regulation. MethodsData SourcesPublic health departments in the states, territories, localities, and Freely Associated States (FAS) (i.e., the Republic of the Marshall Islands, the Federated States of Micronesia, and the Republic of Palau, formerly parts of the U.S.-administered Trust Territory of the Pacific Islands) have primary responsibility for detecting and investigating WBDOs, which they report voluntarily to CDC by using a standard form (CDC form 52.12, available at http://www.cdc.gov/healthyswimming/downloads/cdc_5212_waterborne.pdf). The form solicits data on characteristics of the WBDO (e.g., cases, time, and location); results from epidemiologic studies; results from clinical specimen and water sample testing; and other factors potentially contributing to the WBDO (e.g., environmental concerns, disinfection deficiencies, and filtration problems). CDC annually requests reports from state, territorial, and FAS epidemiologists or persons designated as WBDO surveillance coordinators and obtains additional information regarding water quality and water treatment as needed. Information also can be solicited from other CDC surveillance systems and confirmed with the state, territory, locality, or FAS for inclusion as a WBDO. Numerical and text data are abstracted from the WBDO report form and supporting documents and entered into a database for analysis. Although reports of WBDOs are collected through the WBDOSS, the cases and outbreaks associated with drinking water, WNID, and WUI are analyzed and published separately from the cases and outbreaks associated with recreational water (4). DefinitionsThe unit of analysis for the WBDOSS is typically an outbreak, not an individual case of a waterborne disease. Two criteria must be met for an event to be defined as a waterborne outbreak associated with drinking water, WNID (excluding recreational water) or WUI. First, two or more persons must be epidemiologically linked by location of exposure to water, time, and illness. This criterion is waived for single cases of laboratory-confirmed primary amebic meningoencephalitis (PAM) and for single cases of chemical/toxin poisoning if water-quality data indicate contamination by the chemical/toxin. Second, the epidemiologic evidence must implicate water as the probable source of illness. Reported cases and outbreaks associated with contaminated drinking water; contaminated commercially bottled water, ice, or beverages made with contaminated water; and deficiencies of equipment/devices for which water is used or distributed (e.g., beverages contaminated by plumbing failures in drink mix/soda machines) are classified as WBDOs. WBDOs associated with cruise ships are not summarized in this report. Tabulation of WBDOs and associated cases is based on location of water exposure, not on state of residence of the ill persons. Numerous types of drinking water systems exist and have been outlined (Figure 1). Public water systems, which are classified as either community or noncommunity , are regulated under SDWA. Of the approximately 167,012 public water systems in the United States, 112,948 (67.6%) are noncommunity systems, including 93,210 transient systems and 19,738 nontransient systems; 54,064 (32.4%) are community systems. Despite representing a minority of water systems, community systems serve 264 million persons (approximately 93.9% of the U.S. population) (26). Furthermore, a limited number of community systems (15%) provide water to 90% of the community system population (26). Noncommunity, nontransient systems provide water to 6.9 million persons, and noncommunity, transient systems provide water to 12.9 million persons (by definition, these populations also use another type of water system at their residences, except for the limited number of permanent residents of nontransient systems) (26). Although the majority of public water systems (91.6%) are supplied by ground water, more persons (63.4%) drink from public systems served by surface water (26). Approximately 15.0% of the U.S. population relies on individual water systems that are privately owned (27). In previous Surveillance Summaries, commercially bottled water, when linked with a WBDO, was classified as an individual water system; these WBDOs are now classified as bottled water. WNID is defined as water used in occupational settings; lakes, springs, and creeks used as drinking water by campers and boaters; irrigation water; and other nonpotable water sources with or without taps. WNID does not include recreational water, which is discussed in a separate Surveillance Summary (4). WBDOs with more than one implicated water system type are tabulated and analyzed as mixed water systems (e.g., noncommunity and individual). Source water is defined as the untreated water (i.e., raw water) used to produce drinking water. WBDOs with more than one implicated water source are tabulated and analyzed as mixed water sources (e.g., lake and well). For WNID or WUI, primary water exposure is defined as the source of contaminated water. Water setting is defined as the location of ill person's exposure to the contaminated water. The setting applies to drinking water, WNID, and WUI. The purpose of this surveillance system is not only to evaluate the relation between water and reported outbreaks and disease, but also to identify system breakdowns, operator errors, and other engineering-related activities that lead to outbreaks. To understand the circumstances and system breakdowns that lead to illness, each WBDO is classified as having one or more deficiencies (Table 2). Waterborne Disease and Outbreak Strength of Evidence ClassificationAll WBDOs reported to the surveillance system have been classified according to the strength of the evidence implicating water as the vehicle of transmission (Table 3). The classification scheme (i.e., Classes I--IV) is based on the epidemiologic and water-quality data provided with the WBDO report form. Although WBDOs without water-quality data might have been included in this report, reports that lacked epidemiologic data, linking the outbreak to water, have been excluded. A classification of I indicates that adequate epidemiologic and water-quality data were reported. However, this classification does not necessarily imply that the investigation was optimally conducted nor does a classification of II, III, or IV imply that the investigation was inadequate or incomplete. WBDOs and their resulting investigations occur under different circumstances, and not all WBDOs can or should be rigorously investigated. In addition, WBDOs that affect few persons are more likely to receive a classification of III or IV because of the limited sample size available for analysis. Changes in the 2003--2004 Surveillance SummaryNames, definitions, and other parameters in this report have been modified and expanded to better reflect the changing epidemiology of WBDOs and capture the wide scope of water-related disease. This section highlights those changes. Title The title of this Surveillance Summary has been changed. The change in the title of this report emphasizes and better represents the public health importance of single cases of waterborne disease and disease associated with water exposures other than drinking water and recreational water. Etiologic Agents Etiologic agents are typically identified through clinical specimen testing. If more than one agent is identified, only those agents that individually represent >5% of positive clinical specimens appear in the tables and calculations as etiologic agents for that WBDO. Occasionally, clinical specimen data are unavailable, but water sample testing implicates a particular etiologic agent that is consistent with the presenting illness. In these situations, the agent identified by water testing is listed as the etiologic agent for that WBDO. WBDOs in which the etiologic agent is unconfirmed or unknown are listed as unidentified, even when other data (e.g., clinical findings) are suggestive of a particular pathogen or chemical/toxin. In previous reports, the term "acute gastrointestinal illness (AGI)" was used to indicate WBDOs of unidentified etiology associated with gastrointestinal symptoms. Because AGI refers to a type of illness and not to an etiologic agent, the term "unidentified" is now used to describe WBDOs with unknown etiology. When each etiologic agent is of the same agent type (i.e., bacterial, chemical/toxin, parasitic, or viral), the WBDO is analyzed within that category (e.g., an outbreak with both Cryptosporidium spp. and Giardia spp. will be analyzed as a parasitic outbreak). When agents represent more than one type, the WBDO is analyzed as a mixed-agent WBDO (e.g., an outbreak with both Giardia spp. and Salmonella spp. will be analyzed as a mixed parasitic and bacterial outbreak). Predominant Illness All WBDOs are categorized according to predominant illness. Whereas the illness associated with a WBDO generally includes only one category of symptoms (e.g., gastroenteritis), WBDOs do occur where the symptoms cluster into more than one category (e.g., gastroenteritis and dermatitis). Therefore, in this report, any illness symptom reported by >50% of patients will be listed; multiple illnesses will be listed for a single WBDO, if applicable. Mixed illness WBDOs are analyzed separately from single illness WBDOs. Case Counts and Deaths The number of deaths associated with each WBDO has been added to the case counts. No deaths occurred unless noted. This change provides greater information on the severity of illness associated with each WBDO. Deficiencies Water utilities manage the drinking water in public systems before the water reaches the water meter (or before the property line if the distribution system is not metered). These public drinking water systems are subject to EPA regulations. Drinking water concerns arising after the meter or property line (e.g., Legionella colonization in plumbing, plumbing contamination and cross-connections within buildings and homes, and drink mix/soda machine deficiencies) might not be under the jurisdiction of water utilities and might not be regulated under current EPA drinking water rules. To characterize drinking water concerns that might have different oversight, the classification of deficiencies leading to WBDOs has been modified in this report. The new deficiency classification (Table 2) provides greater detail concerning the circumstances and risk factors that led to illness and clarifies deficiencies that might require different types of public health responses. In the old deficiency classification (formerly deficiencies 1--5), antecedent circumstances related to WBDOs that occurred outside the jurisdiction of a water utility were 1) classified with water distribution system deficiencies that were within the jurisdiction of a water utility (formerly deficiency 4); 2) classified as miscellaneous deficiencies (formerly deficiency 5); or 3) not classified at all (e.g., Legionella colonization in plumbing). In the new deficiency classification, a clear distinction is made between contamination occurring at or in the source water, treatment facility, or distribution system (SWTD) (deficiencies 1--4), which are under the jurisdiction of a water utility if a public water system is involved versus contamination at points not under the jurisdiction of a water utility or at the point of use (NWU/POU) (i.e., deficiencies 5A, 6--11, and 99A and 99B). The NWU/POU deficiencies include WBDOs associated with drinking water contaminated during shipping, hauling, storing, or use; commercially bottled water; ice or beverages made with contaminated water; and deficiencies of equipment/devices in which water is used or distributed (e.g., beverages contaminated by plumbing failures in drink mix/soda machines). For WBDOs involving consumption or contact with WNID and WUI, separate deficiency classifications (i.e., deficiencies 5B, 5C, 12, 99C, and 99D) are used. The reporting and analysis of deficiencies also have changed to emphasize that individual WBDOs might be associated with more than one deficiency. Instead of reporting and analyzing only the primary deficiency when multiple deficiencies have been identified, all deficiencies are now considered. Identifying only the primary deficiency might be difficult because more than one deficiency might have resulted in contamination of water that would result in illness. To reflect this complexity, tables and figures that report deficiency information report all deficiencies that have likely contributed to the WBDO. Therefore, the total number of deficiencies is greater than the total number of WBDOs. Water System Type Drinking water systems remain categorized as community, noncommunity, or individual systems. For the 1999--2000 and 2001--2002 Surveillance Summaries, WBDOs linked to commercially bottled water and WNID were classified as individual water systems for analysis purposes (3,28). For 2003--2004, to distinguish between piped and nonpiped drinking water, the definition of an individual drinking water system no longer includes commercially bottled water and WNID. WBDOs associated with commercially bottled water are now classified separately (i.e., bottled). Separating piped from nonpiped water also distinguishes between drinking water systems regulated by EPA (community and noncommunity) and the FDA (i.e., bottled). WBDOs associated with WNID no longer have a water system type designation because the risk factors associated with these WBDOs are not relevant to drinking water systems. Analyses involving water system types have also changed. If a WBDO involving more than one water system type occurs, the WBDO is classified and analyzed as a mixed water system. Furthermore, all analyses that involve water system types are limited to WBDOs with deficiencies 1--4 and deficiency 99 when a water system can be identified but insufficient information concerning the deficiency is available. Under the revised deficiency classification, the only deficiencies relevant to the type of drinking water system associated with the WBDO are deficiencies 1--4 (i.e., surface water contamination, ground water contamination, water treatment deficiencies, and distribution system contamination). Water Source The only deficiencies relevant to the type of drinking water source involved in the WBDO are deficiencies 1--3 (i.e., surface water contamination, ground water contamination, and water treatment deficiencies). Therefore, all analyses presented in this report that involve source water type are limited to WBDOs with deficiencies 1--3. If a WBDO involves more than one source water type, the WBDO is classified and analyzed as a mixed source WBDO. Legionella Although outbreaks of Pontiac fever (PF) have been included in the WBDOSS since 1981, outbreaks of Legionnaires' disease (LD) only have been included since the 2001--2002 surveillance period (28). During this period, all PF and LD outbreaks were listed in the drinking water Surveillance Summary in a table separate from the tables listing other drinking water-associated WBDOs; the single PF outbreak associated with recreational water was discussed in the recreational water Surveillance Summary (29). Beginning with the 2003--2004 Surveillance Summary, PF and LD outbreaks associated with drinking water are included in the same line lists with other drinking water-associated WBDOs. Similarly, PF and LD outbreaks associated with recreational water are listed and discussed in the 2003--2004 Surveillance Summary of recreational water-associated WBDOs (4). Inclusion and analysis of PF and LD outbreaks with other drinking water-associated WBDOs is a reflection of the changing epidemiology of WBDOs. Legionella outbreaks that occur in association with WNID or WUI also are listed and discussed in this report. Water Not Intended for Drinking and Water of Unknown Intent In previous Surveillance Summaries, WBDOs (excluding Legionella outbreaks) associated with WNID or with WUI were integrated into the drinking water WBDO line lists. Beginning with this report, WBDOs (including Legionella outbreaks) associated with WNID or with WUI are listed in separate tables to distinguish the different water types. Strength of Evidence Classification for Waterborne Disease and Outbreaks Single cases of PAM or chemical/toxin poisoning are now given strength of evidence classifications (Table 3) along with the other WBDOs. These single cases do not receive rankings higher than III because relative risks, odds ratios, and p values are not calculated from single cases. ResultsDuring 2003--2004, 19 states reported 36 WBDOs (i.e., 14 for 2003 and 22 for 2004). These WBDOs were associated with water intended for drinking (n = 30), WNID (n = three), and WUI (n = three) and are tabulated by year and state (Tables 4--6). Waterborne Disease and Outbreaks Associated with Water Intended for DrinkingThe 30 drinking water-associated WBDOs (i.e., 12 during 2003 and 18 during 2004) were reported by 18 states (Figure 2). The number of drinking water-associated WBDOs reported for 2003--2004 is similar to that reported for 2001--2002 (n = 36, including the five previously unreported outbreaks for 2002 [Table 7; Figure 3]). WBDOs associated with drinking water occurred throughout the year (Figure 4). Five states (Florida, New Jersey, New York, Ohio, and Pennsylvania) reported the highest number of drinking water-associated WBDOs (three each) for 2003--2004. Selected WBDO descriptions have been reported (Appendix B, Descriptions of Selected Waterborne Disease and Outbreaks (WBDOs) Associated with Drinking Water, Water Not Intended for Drinking, and Water of Unknown Intent). The 30 drinking water-associated WBDOs reported for 2003--2004 caused illness among approximately 2,760 persons and resulted in four deaths. The median number of persons affected in a WBDO was seven (range: 1--1,450). Twenty-nine WBDOs were associated with either acute respiratory illness (ARI) or AGI, and one WBDO was associated with both ARI and AGI. All ARI outbreaks were associated with exposure to Legionella spp. (Figure 5). Seven (23.3%) of the 30 drinking water-associated WBDOs were given a strength of evidence Class I ranking on the basis of epidemiologic and water-quality data; one (3.3%) was ranked as Class II; 20 (66.7%) were ranked as Class III; and two (6.7%) were ranked as Class IV. Drinking water-associated WBDOs are tabulated by etiologic agent and type of water system (Table 8), etiologic agent and type of water source (Table 9), type of deficiency and type of water system (Table 10), type of deficiency and type of water source (Table 11), predominant illness and type of water system (Table 12), and predominant illness and type of water source (Table 13). WBDOs were included (Tables 8--13) only if the type of deficiency involved in each WBDO was associated with the summarized variable. WBDOs were not included if the type of deficiency did not reflect the summarized variable (e.g., the source of raw untreated water would unlikely be relevant for a Legionella outbreak associated with a building plumbing system).
Etiologic Agents Twenty-five (83.3%) of the 30 drinking water-associated WBDOs were of known etiology; 17 (68.0%) were attributed to an infectious etiology, and eight (32.0%) were attributed to chemical/toxin poisoning. Of the 17 WBDOs with known infectious etiology, 13 (76.5%) were caused by bacteria (eight [61.5%] of which were caused by Legionella spp.), two (11.8%) were caused by more than one etiologic agent type, one (5.9%) was caused by a parasite, and one (5.9%) was caused by a virus. Five (16.7%) of the 30 drinking water-associated WBDOs were of unknown etiology. The distribution of etiologic agents for the 30 drinking water-associated WBDOs has been reported (Figure 6). Bacteria. Thirteen WBDOs affecting 318 persons were attributed to bacterial infections: eight Legionella spp. outbreaks, three Campylobacter spp. outbreaks, one Salmonella typhimurium outbreak, and one outbreak involving two different bacteria (16 persons had stool specimens that tested positive for C. jejuni, and two persons had stool specimens that tested positive for Shigella spp.). Illnesses from these 13 WBDOs resulted in four deaths, all of which were associated with Legionella spp. Chemicals/Toxins. Eight WBDOs affecting 27 persons were attributed to chemical/toxin poisoning; no deaths were reported. Three WBDOs involved high levels of copper associated with drink mix/soda machines; three WBDOs were a result of contamination of commercially bottled water with bromate and other by-products of disinfection, cleaning products, and gasoline by-products; two WBDOs were a result of large volumes of sodium hydroxide discharged into community water supplies. Mixed agents. Two WBDOs were attributed to more than one type of etiologic agent; no deaths were reported. The largest reported outbreak affected 1,450 persons and involved at least one bacterium (i.e., C. jejuni, although one clinical specimen with S. typhimurium also was reported), one virus (norovirus), and one parasite (Giardia intestinalis). The second mixed-agent outbreak affected 82 persons and involved infection with three different bacteria (i.e., C. jejuni, C. lari, and Helicobacter canadensis) and one parasite (Cryptosporidium spp.). Parasites. One WBDO attributed to G. intestinalis, affected 11 persons. No deaths were reported. Viruses. One WBDO attributed to norovirus affected 70 persons. No deaths were reported. Unidentified etiologic agents. Five WBDOs involving AGI of unidentified etiology affected 802 persons; no deaths were reported. Stool testing to identify a causative agent was attempted in four of the five outbreaks. In one outbreak at a volleyball tournament, norovirus was suspected on the basis of incubation period, symptoms, and duration of illness (Florida, January 2003). However, the implicated water tested negative for norovirus, and patient samples were not collected for confirmatory testing. Reports for the other four WBDOs did not note a suspected etiologic agent. Deficiencies Thirty-three deficiencies were cited in the 30 drinking water-associated WBDOs. Fourteen (42.4%) deficiencies involved the source water, treatment facility, or distribution system (SWTD); 17 (51.5%) deficiencies occurred at points not under the jurisdiction of a water utility or at the point of use (NWU/POU); and two (6.1%) were unknown deficiencies (Figure 7; Table 14). Deficiencies 1-4: Contamination of Water at/in the Water Source, Treatment Facility, or Distribution System Water-quality data. Water-quality data (e.g., data regarding the presence of coliform bacteria, pathogens, or chemical/toxin contaminants; or data regarding levels of disinfectants, such as chlorine) were available for all 11 WBDOs given a deficiency classification of 1-4. Bacterial water-quality data were available for the eight WBDOs with confirmed infectious etiologies, and positive total or fecal coliform results from the implicated water were reported for seven (87.5%). The implicated water was tested for specific pathogens in two (25.0%) of the eight WBDOs with confirmed infectious etiologies. However, a pathogen was isolated from water in only one of these outbreaks; in this mixed-agent outbreak, the implicated water tested positive for Cryptosporidium spp., but the other three implicated infectious agents (C. lari, C. jejuni, and H. canadensis) were not recovered from the water samples. Two (18.2%) of the 11 WBDOs with water-quality data were attributed to chemical/toxin poisoning. In both WBDOs, sodium hydroxide was the implicated agent and the water had a high pH level. One (9.1%) of the 11 outbreaks did not have an etiologic agent identified. However, the implicated water tested positive for both total and fecal coliforms. Water systems. Four (36.4%) of 11 WBDOs with deficiencies 1-4 involved community water systems, four (36.4%) involved noncommunity water systems, two (18.2%) involved individual water systems, and one (9.1%) involved both noncommunity and individual water systems (Tables 8, 10, and 12; Figure 6). Among the four outbreaks involving community water systems, two (50.0%) were associated with a treatment deficiency, and two (50.0%) were associated with problems with the water distribution system or water storage. Among the four outbreaks involving noncommunity water systems, one (25.0%) was associated with contaminated untreated ground water intended for drinking; one (25.0%) was associated with a treatment deficiency; one (25.0%) was associated with a deficiency in the water distribution system; and one was associated with both a treatment and a distribution system deficiency. Among the two outbreaks involving individual water systems, one (50.0%) was associated with contaminated untreated surface water intended for drinking; and one (50.0%) was associated with both contaminated untreated ground water intended for drinking and deficiencies in the water distribution system. The single outbreak involving both noncommunity and individual water systems was associated with both contaminated untreated ground water intended for drinking and deficiencies in the water distribution system. Water sources. Seven (87.5%) of the eight WBDOs with deficiencies 1-3 were associated with ground water sources involving wells, and one (12.5%) WBDO was associated with surface water derived from a spring-fed pond. Among the seven outbreaks related to ground water sources, three (42.9%) were associated with consumption of untreated ground water, and four (57.1%) were associated with treatment deficiencies (Tables 9, 11, and 13; Figure 6). Deficiencies 5A, 6-11, and 99B: Contamination of Water at Points Not Under the Jurisdiction of a Water Utility or at the Point of Use Water-quality data. Water-quality data indicating a problem with the water were available for 16 (94.1%) of 17 WBDOs with an NWU/POU deficiency. Among the nine WBDOs with an infectious etiology, eight (88.9%) were associated with Legionella spp., and one (11.1%) was associated with norovirus (Pennsylvania, January 2004). Legionella spp. were isolated from the implicated water sampled in all of the Legionella outbreaks. The implicated water in the norovirus outbreak tested positive for fecal coliforms. Water-quality data were provided with the reports from all six WBDOs with chemical etiologies. In all six WBDOs, the contaminants causing the WBDO were recovered from the implicated water: copper in three WBDOs (Minnesota, June and November 2003; and South Carolina, July 2004); bromate and other by-products of disinfection in one WBDO (Florida, November 2003); a multiple-chemical cleaning product in one WBDO (Maine, December 2003); and gasoline by-products in one WBDO (Florida, October 2004). In the latter, the mechanism by which gasoline by-products got into the commercially bottled water was unknown, and this WBDO was given a deficiency of 99B. This WBDO is included with the other NWU/POU WBDOs for analysis purposes because commercially bottled water was involved. Water-quality data also were provided with the reports from two WBDOs with unidentified etiologies. In one outbreak, the implicated water tested positive for total coliforms. In the other outbreak, the implicated water was tested specifically for norovirus, but it was not isolated. Deficiency 5A: Legionella in water intended for drinking. All eight of the drinking water-associated Legionella WBDOs occurred in large buildings or in institutional settings and were related to the multiplication of Legionella spp. in the plumbing. Among the 27 cases attributed to these Legionella outbreaks, one case was reported to have symptoms consistent with PF. The majority of cases of legionellosis were diagnosed by urinary antigen testing, which is specific for L. pneumophila serogroup 1 (30). Deficiencies 6-11. Of the eight WBDOs associated with deficiencies 6-11, three (37.5%) were associated with drink mix/soda machine deficiencies resulting in copper intoxication; three (37.5%) were associated with commercially bottled water; one (12.5%) was associated with a cross-connection in the plumbing inside a building; and one (12.5%) was associated with point-of-use contamination of a communal water jug at a worksite. All of these WBDOs have been described (Appendix B). Deficiency 99A: Unknown/Insufficient Information Concerning Contamination of Water Intended for Drinking Tap Water The deficiencies involved in two (6.7%) of the 30 WBDOs could not be identified because of insufficient information or unknown cause of contamination. Water samples from both of these noncommunity water systems and tap-water--associated WBDOs tested positive for E. coli and total coliforms, but etiologic agents were not identified. One outbreak involved ground water (i.e., well water), and one involved tap water from an unknown water source. However, because the mechanism of contamination was unknown and the point of contamination might not have been under the jurisdiction of a water utility, these two WBDOs are analyzed separately from the SWTD and NWU/POU deficiencies. Waterborne Disease and Outbreaks Associated with Water Not Intended for Drinking and Water of Unknown IntentSix WBDOs were associated with either WNID (n = three) or WUI (n = three) (Table 6). More WNID/WUI outbreaks were reported for 2003--2004 (n = six) than during 2001--2002 (n = one). The six WNID/WUI outbreaks caused illness among approximately 36 persons and resulted in four deaths. One (16.7%) WNID/WUI outbreak involved AGI, and five (83.3%) involved ARI. Two (33.3%) of the six WNID/WUI outbreaks were categorized as a strength of evidence Class I ranking; one (16.7%) was ranked as Class III; and three (50.0%) were ranked as Class IV. Etiologic Agents Five (83.3%) of the six WNID/WUI outbreaks were attributed to L. pneumophila serogroup 1, affected 26 persons, and resulted in four deaths. Fifteen of the cases were associated with LD, and 11 were associated with PF. The other WNID/WUI outbreak was attributed to E. coli O157:H7; 10 persons were reported ill. Deficiencies 5B, 5C, 12, 99C, and 99D The six WNID/WUI outbreaks each had one known deficiency: five (83.3%) involved Legionella spp. in the water system (deficiencies 5B and 5C), and one (16.7%) involved WNID unrelated to Legionella (deficiency 12). Two (40.0%) of the five Legionella outbeaks involved WNID (deficiency 5B). In these outbreaks, the aerosolized water from cooling towers was tested and identified as the source of Legionella spp. Three Legionella outbreaks (60.0%) involved WUI (deficiency 5C). In these outbreaks, environmental water testing failed to determine the source of Legionella spp. The one outbreak unrelated to Legionella involved E. coli O157:H7 infection after exposure to sewage from a broken septic line at a camp. Campers might have been exposed in a wash house in which a septic back-up occurred or might have been exposed to surface sewage seepage near the housing area. Campers were observed playing in a wet area near the sewage seepage. No water testing was performed in this outbreak. However, soil from the area of the sewage leakage tested negative for the pathogen. Previously Unreported OutbreaksReports of nine previously unreported drinking water-associated WBDOs that occurred during 1982--2002 were received for this surveillance period (Table 7). An outbreak of diarrheal illness occurred among six attendants of a graduation party (New York, July 2002); two had laboratory-confirmed E. coli O157:H7 infections. This pathogen was isolated from a private well that provided drinking water and matched the two laboratory-confirmed cases by pulsed-field gel electrophoresis pattern. The well water supply was reportedly not disinfected. An outbreak of gastroenteritis occurred among 15 students on a class trip (New York, May 1984). During the trip, 15 (30.6%) of 49 students became ill and experienced nausea and vomiting within 1--2 hours of eating at a restaurant. The ill students had ingested soda from a soda fountain that was described as having a metallic taste. Samples from the soda fountain machine were analyzed for copper, iron, and other metals and were within the normal range. However, testing of urine samples collected 2 days after illness onset demonstrated elevated levels of copper in some students' urine samples. Heavy use of fire hydrants nearby caused pressure problems in the community water main while students were being served at the restaurant. These pressure fluctuations might have stirred up sediment in the distribution system, resulting in excess copper being delivered to the restaurant water supply. During April 2002, an outbreak of gastroenteritis in 59 persons occurred in Palau. Entamoeba histolytica was isolated from nine (30.0%) of 30 stool specimens. All ill persons reported consuming untreated drinking water from the same portable water catchment tank that collected water from a stream. Water sampled from the tank tested positive for total and fecal coliform bacteria. Three outbreaks of gastroenteritis (New York, May 1982, August 1995, and August 1996) involved unidentified etiologic agents. During the 1982 outbreak, drinking water at a restaurant was linked to illness. Samples of water and ice were negative for pathogens, but the raw well water tested positive for fecal coliform bacteria. In addition, although the well water received ultraviolet light treatment before entering the restaurant plumbing system, fecal and total coliforms were found in water samples after treatment. The 1995 outbreak report implicated water and ice served at a hotel restaurant. An untreated well was the source of drinking water and water used to make ice. Water samples from the kitchen faucet were positive for both total coliforms and E. coli. On the basis of the incubation period, symptoms, and duration of illness, norovirus was suspected. Investigators speculated that the well water might have been contaminated or that an ill person might have contaminated the ice after production. During the 1996 outbreak among campers, a viral etiology was suspected based on incubation period, symptoms, and duration of illness. The source of illness was unconfirmed, but a fecally contaminated unchlorinated water supply (i.e., well water) was suspected. Water samples from the untreated well tested positive for E. coli. The well had tested positive the previous year for E. coli after a gastroenteritis outbreak. Reports of two Legionella outbreaks (Maryland and the U.S. Virgin Islands, November 2002) and one mixed-agent outbreak (New York, December 2002) were also received for this surveillance period. These WBDOs have been described (Appendix B). Surveillance Reports Not Classified as Waterborne Disease and OutbreaksThree surveillance reports potentially implicating drinking water were submitted during 2003--2004 but had insufficient epidemiologic or laboratory evidence to warrant inclusion in this report as WBDOs. One surveillance report included only one confirmed case of Legionella infection; the second suspected case was not laboratory confirmed. Regarding the second report, the investigation did not reveal a common point source of Legionella transmission. However, because of the potential link to drinking water, a brief description of the third report has been provided. In July 2003, multiple persons attending a family reunion developed AGI. E. coli O157:H7 was isolated from the stool of four attendees. Lemonade made with untreated water was cited, but other common food and water sources were identified. No epidemiologic studies were conducted. DiscussionConsiderations Regarding Reported ResultsWBDOSS provides information concerning epidemiologic and etiologic trends in outbreaks related to drinking water. However, not all outbreaks are recognized, investigated, or reported to CDC, and studies have not been conducted that assess the sensitivity of this system. Furthermore, outbreaks occurring in national parks, tribal lands, or military bases might not be reported to state or local authorities. For these reasons, the true incidence of WBDOs is probably greater than is reflected in surveillance system data. Multiple factors influence whether WBDOs are recognized and investigated by local or state public health agencies, including public awareness of the outbreak, availability of laboratory testing, requirements for reporting diseases, and resources available to local and state health departments for surveillance and investigation of probable outbreaks. In addition, because differences in the capacity of local and state public health agencies and laboratories to detect WBDOs might result in reporting and surveillance bias, the states with the majority of outbreaks reported for this period might not be the states in which the majority of outbreaks actually occurred. An increase or a decrease in the number of WBDOs reported might reflect either an actual change in the incidence of outbreaks or a change in the sensitivity of surveillance practices. As with any passive surveillance system, the accuracy of the data depends substantially on the reporting agencies (i.e., state, local, and territorial health departments). Therefore, independent of the recognition or investigation of a given outbreak, reporting bias also can influence the final data. The outbreaks most likely to be recognized and investigated are those involving acute illness characterized by short incubation periods, serious illness or symptoms requiring medical treatment, or recognized etiologies for which laboratory methods have become more sensitive or widely available. Increased reporting frequently occurs as etiologies become better recognized, water system deficiencies are identified, and state surveillance activities and laboratory capabilities increase (31--33). Consequently, recommendations for improving WBDO investigations include enhancing surveillance activities, increasing laboratory support for clinical specimen and water sample testing, and assessing sources of potential bias (34--36). The identification of WBDO etiologic agents depends on multiple factors. Investigators must recognize the WBDO in a timely manner so that appropriate clinical specimens and environmental samples can be collected. Collection of water samples further depends on local and state statutory requirements and the availability of investigators. Methods for concentrating large volumes of water for testing are being developed and disseminated to multiple sites in the United States as standard protocols (37). The laboratories involved must have the capacity to concentrate large volumes of water for testing, in addition to the ability to test for the organism, chemical, or toxin in the clinical specimens and environmental samples. For example, routine testing of stool specimens at laboratories includes tests for the presence of enteric bacterial pathogens and also might include ova and parasite examination. However, testing for viral agents is rarely conducted, although norovirus testing is now being performed more commonly. In addition, clinicians and public health officials must know the correct tests to order. For example, testing for Cryptosporidium spp., one of the most commonly reported waterborne pathogens, is frequently not included in standard ova and parasite examinations and therefore must be specifically requested (38). One key limitation of the data collected by the WBDOSS is that the information pertains only to outbreaks of waterborne illness and not to endemic waterborne illness. The epidemiologic trends and water-quality concerns observed in outbreaks might not necessarily reflect or correspond with trends associated with endemic waterborne illness. In response to the Congressional Safe Drinking Water Act Amendments of 1996, in 2005, EPA and CDC completed a series of epidemiologic studies and a national workshop designed to assess the magnitude of endemic waterborne AGI associated with consumption of public drinking water. A joint report on the results of these studies is available at http://www.epa.gov/nheerl/articles/2006/waterborne_disease.html. The report includes multiple documents that discuss various methods for estimating the number of endemic waterborne AGI cases associated with public drinking water systems in the United States. In particular, the authors of two reports used current data and made various assumptions for missing data to derive two different but overlapping estimates of 1) 4.3--11.7 million annual AGI cases (confidence interval unknown) (39) and 2) 16.4 million annual AGI cases (range: 5.5--32.8) (40). These estimates should be interpreted with an understanding that information concerning endemic waterborne-disease risks is imprecise and uncertain and that substantial data gaps remain. The wide range in the number of estimated cases suggests a high level of uncertainty. Nonetheless, workshop participants agreed that enough data were available for rough estimates and that these estimates should be made at this time, with all assumptions and limitations fully described so the approaches can be evaluated. These estimates, however, only describe a portion of the annual incidence of endemic waterborne-disease cases. To describe the overall incidence, estimates also would need to include the number of cases of waterborne disease other than AGI and the number of cases associated with nonpublic drinking water systems, commercially bottled water, recreational water, WNID, and WUI. If these other types and sources of waterborne disease were considered, the estimated number of cases of endemic waterborne disease would be higher than the figures previously presented in this report. WBDOs Associated with Water Intended for DrinkingEtiologic agents Legionella spp. and chemicals were the most commonly reported etiologic agents in drinking water-associated WBDOs. During 2003--2004, eight reported drinking water-associated WBDOs involved Legionella spp. and comprised 26.7% of the total, which is only the second time that data concerning Legionella outbreaks have been included in a Surveillance Summary. Chemical/toxin drinking water-associated WBDOs (n = eight) comprised 26.7% of the total, an increase from the previous surveillance period and the largest number of chemical/toxin-related drinking water WBDOs since the 1993--1994 surveillance period. Of the eight chemical/toxin WBDOs, three (37.5%) resulted from deficiencies related to drink mix/soda machines, and two (25.0%) resulted from deficiencies related to recent maintenance work. These outbreaks stress the importance of proper installation and maintenance of water systems and equipment. The increased number of chemical/toxin-related outbreaks also emphasizes the need for increased awareness among the public and public health officials concerning the role that chemicals and toxins play in WBDOs. During the 2003--2004 surveillance period, five drinking water-associated WBDOs involved only bacteria (other than Legionella spp.), an increase in the number of reported non-Legionella bacterial drinking water outbreaks compared with the 2001--2002 surveillance period (n = three). The ongoing occurrence of bacterial WBDOs, despite available and efficacious treatment practices, underscores the continuing need for protection and treatment of drinking water (41). In addition, two mixed-agent outbreaks occurred during the 2003--2004 surveillance period, which included bacteria (one bacterial/parasitic outbreak and one bacterial/parasitic/viral outbreak). The occurrence of mixed-agent outbreaks emphasizes the importance of considering more than one etiologic agent in outbreak investigations, collecting appropriate specimens for each agent type, and requesting appropriate diagnostic testing for each agent type. In addition, both outbreaks were associated with sewage contamination of wells, underscoring the importance of proper waste management and proper drinking water system and waste water system designs. One viral outbreak involving norovirus was reported for the 2003--2004 surveillance period (Pennsylvania, January 2004). Norovirus was also one of the etiologic agents identified in one of the mixed-agent outbreaks (Ohio, July 2004) and was the suspected etiologic agent in one of the outbreaks of unknown etiology (Florida, January 2003), based on incubation period, symptoms, and duration of illness. Sewage contamination was suspected in both outbreaks in which norovirus was identified. Point-of-use contamination of a water dispenser was a contributing factor in the suspected norovirus outbreak. These three outbreaks represent a decrease in viral drinking water-associated WBDOs compared with the previous surveillance period (n = five) and might reflect a true decrease in viral outbreaks, a lack of outbreak investigation and detection, a lack of viral testing, or a combination of factors. Compared with the previous surveillance period, the number of reported parasitic outbreaks decreased for 2003--2004. Parasites were identified in one single-agent outbreak (G. intestinalis) and two mixed-agent outbreaks (Cryptosporidium spp. and G. intestinalis). All three outbreaks were associated with distribution system deficiencies, but only one also was associated with the use of untreated source water (ground water under the influence of surface water in Ohio, July 2004). No parasitic outbreaks were associated with surface water systems. Both surface water systems and ground water systems under the influence of surface water are regulated under SWTR to protect the public against exposure to Giardia and Cryptosporidium, among other pathogens. The etiologic agent was unidentified in five (16.7%) of the 30 drinking water-associated WBDOs reported during 2003--2004 (Figure 6). This finding is the lowest number and percentage of outbreaks caused by an unknown etiology in any surveillance period since the beginning of the surveillance system in 1971. Five drinking water-associated outbreaks of unknown etiology occurred during 1997--1998, but this number represented 29.4% of the reported non-Legionella outbreaks. This decrease probably reflects the improved diagnostic capability of laboratories and better outbreak investigations, resulting in more rapid and more appropriate specimen collection. Deficiencies 1--4: Contamination of Water at/in the Water Source, Treatment Facility, or Distribution System In general, EPA regulates the public drinking water supplies from the source water up to the water meter (or before the property line if the distribution system is not metered). This segment of the drinking water supply system is associated with deficiencies 1--4: 1) consumption of untreated surface water intended for drinking, 2) consumption of ground water intended for drinking, 3) treatment deficiencies, and 4) distribution system deficiencies before the water meter or property line. During the 2003--2004 surveillance period, 36.7% of drinking-water related outbreaks (n = 11) and 42.4% of deficiencies (n = 14) involved deficiencies 1--4. A single WBDO can be associated with more than one deficiency. Source water. Discussions regarding source water type only include those WBDOs with deficiencies 1--3 because distribution system deficiencies (deficiency 4) are not dependent upon the source water type. Also excluded from discussion involving source water types are drinking water-associated WBDOs with unknown or insufficient information (deficiencies 99A) and outbreaks associated with contamination at points not under the jurisdiction of a water utility or at the point of use (deficiencies 5A, 6--11, and 99B). Surface water. One (12.5%) of the eight outbreaks with deficiencies 1--3 was associated with consumption of untreated surface water (deficiency 1) from a spring-fed pond supplying an individual water system (Ohio, November 2003). This emphasizes the importance of public awareness that surface water, despite its clarity, is prone to contamination by pathogens and should not be directly consumed without first being treated. If water treatment is not available as part of the water system, treatment can be provided at the point of use (e.g., filtration, disinfection by chemicals, or boiling). Manufacturers of point-of-use treatment devices and the National Sanitation Foundation (http://www.nsf.org) provide information regarding different devices, including instructions for their use and their ability to make water safe for human consumption. The WBDO in Ohio in 2003 is the first outbreak associated with consumption of untreated surface water intended for drinking (deficiency 1) since 1999 (3). Since the early 1990s, a decrease has occurred in the percentage of reported WBDOs associated with either untreated or inadequately treated surface water. This decrease is likely attributed to increasingly stringent EPA regulations for treatment of surface water. However, outbreaks might still occur, particularly in water systems that are not subject to EPA regulations. Ground water. Seven (87.5%) of the eight outbreaks with deficiencies 1--3 were associated with consumption of contaminated ground water from wells. This is the smallest number and percentage of ground water-associated WBDOs with deficiencies 1--3 in the previous four surveillance periods (1997--1998 through 2003--2004). Among these seven outbreaks, three (42.9%) involved consumption of untreated ground water (deficiency 2), and four (57.1%) involved treatment deficiencies associated with contaminated ground water (deficiency 3). The highest proportion of these outbreaks (n = three [42.9%]) were associated with noncommunity water systems, but other water system types also were implicated: community (n = 2), individual (n = one), and mixed noncommunity and individual (n = one). The mixed-system outbreak involving noncommunity and individual water systems was the largest outbreak during this surveillance period (Ohio, July 2004). The outbreak occurred on an island in Lake Erie frequented by vacationers. It also was associated with the use of untreated contaminated ground water (deficiency 2) by noncommunity and individual drinking water systems and cross-connections to the community water distribution system (deficiency 4). The environmental investigation identified sewage-contaminated ground water wells used for drinking water as the likely source of exposure to the etiologic agents. Sewage reached the drinking water aquifer because the karst limestone geology of the island forms an aquifer that is vulnerable to contamination. Cracks and fractures in the limestone allow contaminants from upper soil layers to flow through to ground water sources. The severe soil limitations and the karst geology of the island connect sewage system effluent, lake water, and precipitation runoff to the aquifer. In addition to soils and geology, other possible contributing factors include cross-connections in the water distribution system; an increase in precipitation before the outbreak; the volume of wastewater flowing to sewage treatment systems during periods of heavy island visitation; the number, type and maintenance of sewage disposal systems; and groundwater well construction. The seven ground water-associated outbreaks indicate that contaminated ground water that leads to illness is a continuing problem, and efforts should be intensified to identify and remove possible sources of contamination and provide adequate, continuous treatment for those systems that need treatment. Wells and springs must be protected from contamination, even if disinfection is provided, because ground water can become contaminated with pathogens that might overwhelm the disinfection process. EPA requires appropriate treatment, including filtration and disinfection, for public water systems that use ground water under the direct influence of surface water (e.g., those involved in the Ohio outbreak). EPA's GWR establishes multiple barriers for protection against pathogen contamination of drinking water derived from ground water sources. GWR will also establish a targeted strategy to identify ground water systems at high risk for fecal contamination. The multiple barrier approach should begin with protection of the wellhead, an assessment of potential sources of contamination, and periodic sanitary surveys to ensure that wells remain protected. Periodic monitoring of source water is necessary to identify water-quality deterioration, which if discovered, might require mandatory testing. In addition, continuous water treatment is needed for wells that are identified as being vulnerable. Only public water systems will be directly covered by GWR; therefore, protections offered by GWR will not extend to individual ground water systems unless they are regulated by state or local authorities. The quality of water in wells and springs used by individuals and nonpublic systems remains a public health concern; approximately 17 million persons in the United States rely on private household wells for drinking water each year, and >90,000 new wells are drilled annually throughout the United States (42). In addition, contamination of a household well is not only a health concern for the family served by the well but is also a concern for households and other water systems that draw from the same aquifer. To safeguard the quality of well water, homeowners should seek information on needed protective measures and implement recommended operation and maintenance guidelines for private well usage. Homeowners may also choose to protect their own health by purchasing appropriately designed point-of-use devices and by following instructions for operating and maintaining these treatment devices. Although EPA does not regulate individual water systems, EPA recommendations for protecting private wells are available at http://www.epa.gov/safewater/pwells1.html. Additional efforts should be taken by public health officials to educate well owners, users, drillers, and local and state drinking water personnel to encourage practices that best ensure safe drinking water for private well-users. Water treatment. During 2003--2004, four drinking water-related WBDOs associated with water treatment deficiencies were reported. Two outbreaks resulted in burns after the discharge of sodium hydroxide into the distribution system during well maintenance. The other two outbreaks involved temporary interruptions of disinfection (one resulting from a broken chlorine pump [Pennsylvania, June 2004] and one resulting from a faulty ultraviolet light water-treatment apparatus [Montana, August 2004]). All four outbreaks indicate the need for proper equipment handling, maintenance, and postmaintenance safety checks. Distribution system. Distribution system deficiencies make up the largest proportion of the SWTD deficiencies occurring before the water meter or property line during this surveillance period. During 2003--2004, six drinking water-related WBDOs involving distribution system deficiencies occurred. Four (66.7%) of the six WBDOs involved cross-connections to nonpotable water sources. As the use of nonpotable water increases in the United States (e.g., for landscape and agricultural irrigation, toilet flushing, industrial processing, and power plant cooling), the risk for cross-connections between potable and nonpotable water supplies will also probably increase (43). These four outbreaks demonstrate the importance of identifying and clearly labeling potable and nonpotable water lines to prevent cross-connections, which can result in illness. Water systems. Discussions regarding water system types (i.e., community, noncommunity, and individual) include drinking water-associated WBDOs with deficiencies 1--4. Deficiencies in the distribution system are included in these discussions because distribution system problems might be dependent on the type of water system involved. Among the 11 drinking water-associated WBDOs with a deficiency of 1--4, four (36.4%) were associated with community water systems, four (36.4%) with noncommunity water systems, two (18.2%) with individual water systems, and one (9.1%) with both noncommunity and individual water systems (Ohio, July 2004). The proportion (27.3%) of drinking water-related WBDOs associated with unregulated individual water systems (including the Ohio, July 2004 WBDO) is the lowest proportion of outbreaks within the last three surveillance periods (i.e., 1999--2000, 2001--2002, and 2003--2004). This decrease in the proportion of WBDOs associated with individual drinking water systems might reflect a detection bias (given the limited number of persons who are usually affected by these WBDOs), limited resources available to investigate these outbreaks, and the limited number of regulations that govern these systems. Deficiencies 5A, 6-11, and 99B: Contamination of Water at Points Not Under the Jurisdiction of a Water Utility or at the Point of Use By creating additional deficiency classifications, a clear distinction can be made between deficiencies that occur at points NWU/POU and SWTD. During the 2003--2004 surveillance period, more WBDOs were associated with NWU/POU (17 [51.5%]) than with SWTD (14 [ 42.4%]) (Figure 7). Deficiency 5A: Legionella in Water Intended for Drinking. Legionellosis includes two clinically distinct syndromes: LD, a form of pneumonia, and PF, an influenza-like illness without pneumonia. When outbreaks of legionellosis occur in the setting of contaminated drinking water, they typically manifest as cases of LD rather than PF. Regardless of the syndrome, all legionellosis outbreaks share the common features of warm stagnant water, usually documented inadequate biocide concentrations, and aerosolization, which provides the mechanism for inhalation into the lungs. The outbreaks of legionellosis described in this report highlights multiple challenges related to the detection and prevention of legionellosis. LD, the more severe form of legionellosis, is underdiagnosed because multiple patients with community-acquired pneumonia can be treated empirically with broad-spectrum antibiotics (44). However, because Legionella spp. are not transmitted from person-to-person and are always acquired from an environmental source, even a single case of LD implies the presence of a contaminated aquatic source to which others can be exposed. Because host factors, (e.g., underlying lung disease and immunodeficiencies) are essential for the development of disease, the attack rate during documented LD outbreaks is <5%. Identification of two or more cases of LD in association with a potential source is adequate justification for an investigation. All of the outbreaks described in this report involved seven or fewer cases. Nonetheless, in all instances except for one, the epidemiologic and laboratory data were compelling enough to implicate point sources that were subsequently remediated. Three outbreaks occurred among persons in residential settings (i.e., a condominium complex [Maryland, December 2004], an apartment building [New Jersey, June 2004], and a senior housing center [New Jersey, July 2004]). Approximately 70% of sporadic cases of residentially acquired LD occur among persons living in single family homes (45). However, because persons living in multiple-unit settings can be epidemiologically linked to each other, outbreaks that occur in these settings have a higher potential to be recognized by public health authorities. The plumbing systems that serve such buildings tend to be colonized with Legionella spp. in multiple locations, which could increase the risk of LD to other residents of such buildings (46). Guidelines for reducing the risk for legionellosis associated with building water systems are available (47). Providing these guidelines to managers of large residential buildings in addition to other settings more commonly associated with outbreaks of legionellosis might be a useful practice for local and state public health authorities. Three outbreaks demonstrate the propensity for Legionella spp. to colonize potable water systems and cause disease over prolonged periods. Legionella spp. colonize the biofilm layer frequently found inside large, complex plumbing systems (48). This biofilm protects Legionella from biocides and allows the bacteria to amplify to levels sufficient to be transmitted. One outbreak (Maryland, November 2002) previously unreported in any Surveillance Summaries was associated with a health club and resulted in apparent disease transmission during an 8-week period; all ill persons were men aged >65 years. In 2004, the potable water system of a long-term--care facility, which also had experienced an outbreak in 2002, was the source of three additional cases, including one fatality, despite aggressive remediation after the 2002 outbreak (Pennsylvania, April 2004). Finally, LD detected among three guests of a hotel led to an epidemiologic and environmental investigation that identified the potable water system as the likely source (U.S. Virgin Islands, November 2002). The comparison of strains of Legionella spp. isolated during this outbreak with strains recovered from an outbreak at the same hotel that occurred during 1981--1982 revealed remarkable similarity, suggesting that the same strain had colonized the system continuously (49). In summary, Legionella is a hardy organism that resists remediation efforts and therefore can colonize the same potable water system for years or decades. This hotel-associated outbreak also highlights the importance of timely reporting of individual cases of travel-associated legionellosis, as was recently recommended in a 2005 CSTE position statement (http://www.cste.org/PS/2005pdf/final2005/05-ID-01final.pdf). Legionella outbreaks represented >25% of all drinking water-associated WBDOs reported during 2003--2004 and 47.1% of all NWU/POU deficiencies, indicating that Legionella as a public health threat requires further attention. Concerted action is necessary to maintain systems according to published guidelines and to detect and respond to clusters of cases of legionellosis when they occur (47). Deficiencies 6--11. Deficiencies involving water intended for drinking that occur at points after the water meter or the property line include 1) problems with the plumbing; 2) problems with water treatment after the water meter or property line; 3) problems with equipment/devices that use or distribute water (e.g., beverages contaminated by plumbing failures in drink mix/soda machines); 4) contamination of ice or beverages as a result of the use of contaminated water; 5) contamination during commercial bottling; 6) contamination during shipping, hauling, or storage; and 7) contamination at the point of use. The latter three deficiencies frequently involve commercially bottled water. Commercially bottled water is assumed to be a safe source of drinking water; however, the WBDOs associated with commercially bottled water reported during 2003--2004 are examples of the different situations in which contamination can occur. In one WBDO (Florida, November 2003), contamination by disinfection by-products occurred at the plant during production and bottling, indicating that the process of disinfection of bottled water must be closely monitored. In another WBDO (Maine, December 2003), a cleaning product spilled near the bottled water and leached through the plastic bottle to contaminate the water, demonstrating that plastic bottles are permeable to chemicals and therefore commercially bottled water is vulnerable to chemical contamination after production but before the seal is broken. Proper shipping, hauling, and storage of commercially bottled water can prevent this route of contamination. Commercial vendors and the general public need to be aware that commercially bottled water should be stored off the floor and away from any chemical products. In a third WBDO (Florida, January 2003), a large container of commercially bottled water from which multiple persons were served was contaminated at the point of use after the bottle had been opened, underscoring the vulnerability of shared bottles or containers and the importance of practicing good hygiene. A similar outbreak involving a shared container (Michigan, September 2003) further illustrates this problem; however, this WBDO was not associated with commercially bottled water. Three WBDOs were associated with illness attributed to ingestion of copper from drink mix/soda machines. In two of these outbreaks (Minnesota, June 2003; South Carolina, July 2004), problems occurred with backflow of highly acidic, carbonated water from the carbonators back into the building piping and resulted in copper leaching from the pipes. The cause of the malfunction in the third WBDO (Minnesota, November 2003) was less clear and appeared to be a problem with the internal plumbing of a juice machine. Proper installation and maintenance of drink mix/soda machines, with particular attention given to check valves, are critical. One WBDO (Pennsylvania, January 2004) involved a drinking water pipe being inappropriately cross-connected with a nonpotable water source within a building. This WBDO illustrates that cross-connections can be problematic, not only within the distribution system, as illustrated by four outbreaks discussed regarding deficiency 4, but also within building/home plumbing. Potable and nonpotable water lines should be clearly labeled, and plumbing systems should be assessed to prevent and ensure that opportunities for cross-connections do not exist. Approved devices can prevent both the backflow of nonpotable water into the potable water system from backpressure and backsiphonage, but the devices must be maintained and periodically tested (50). The risk for contamination can be reduced by water utilities 1) being cognizant of the potential for the intrusion of contaminants into the water distribution system during transient low or negative water pressure, 2) maintaining an effective disinfectant residual throughout the distribution system, and 3) detecting and repairing pipeline leaks (51). Waterborne Disease and Outbreaks Associated with Water Not Intended for DrinkingDuring the 2003--2004 surveillance period, three WBDOs occurred that were associated with WNID. Two of these outbreaks were associated with Legionella spp. and involved water in cooling towers. The remaining WBDO was associated with E. coli O157:H7 and involved a broken septic line at a camp, which resulted in sewage seepage near the housing area and a septic back-up in a wash house. Whereas WNID outbreaks are less commonly reported than drinking water-related WBDOs, these three outbreaks illustrate that, whether through inhalation or contact, WNID is still associated with disease and requires attention. Broken septic lines, sewage seepage, and improper sewage disposal are public health threats because direct contact with sewage and contamination of drinking water can occur from either ground water or surface water sources. Sewage disposal systems must be properly sited and maintained. If drinking water contamination is suspected, public health officials should 1) institute appropriate measures to prevent consumption of contaminated water (e.g., issuances of boil-water advisories and recommendations to use commercially bottled water), 2) evaluate the sewage disposal system, and 3) address any deficiencies that are identified. Additional Reporting of Historical OutbreaksThis report discusses information concerning nine previously unreported drinking water outbreaks. Six of these outbreaks occurred during 1980--2002 in New York State. Inclusion of the information regarding New York was facilitated by a CDC-funded pilot project to improve waterborne-disease surveillance and waterborne outbreak investigations in New York. In 2005, CDC initiated the project in partnership with the New York State Department of Health (NYSDOH) as part of CDC's Environmental Health Specialist Network (EHS-Net). One element of the project was the hiring of a new full-time employee within the NYSDOH to coordinate the EHS-Net water pilot project. Initial efforts of the pilot project were focused on characterizing the reporting system for waterborne disease in New York State, including reviewing different databases that might contain information concerning waterborne-disease outbreaks. Databases maintained by multiple organizations within NYSDOH and data housed in certain local health departments were reviewed, which resulted in the verification of nine outbreaks associated with water intended for drinking during 1980--2002. Three of these outbreaks had been previously reported to CDC. One outbreak that occurred in 2002 was reported to CDC along with the 2003--2004 outbreaks. The five remaining outbreaks had not been reported to CDC. The EHS-Net water pilot project activities indicate that increased effort and resources, specifically directed at waterborne disease reporting, could result in the identification of previously unreported historical outbreaks. As the EHS-Net water pilot project refines the process for identifying and investigating current waterborne-disease incidents, these efforts might result in enhanced reporting of waterborne outbreaks from New York. In addition, the experience of NYSDOH could provide a template for improving waterborne-disease reporting in other locations. ConclusionData collected as part of the national WBDOSS are used to describe the epidemiology of waterborne disease in the United States. Trends regarding water systems and deficiencies implicated in these WBDOs are used to assess whether regulations for water treatment and water-quality monitoring are adequate to protect the public's health. Identification of the etiologic agents responsible for these outbreaks also is critical because new trends might necessitate different interventions and changes in policies and resource allocations. Surveillance for waterborne agents and WBDOs occurs primarily at the local and state levels (including territories and FAS). Public health authorities at these levels should be able to detect and recognize drinking water-associated WBDOs and implement appropriate prevention and control measures. Improved communication among local and state public health departments, regulatory agencies, and water utilities would aid the detection and control of WBDOs. Routine reporting or sharing of water-quality data within the health department is recommended. Other means of improving surveillance at the local, state, and federal levels might include the additional review and follow-up of information gathered through other mechanisms (e.g., issuances of boil-water advisories or reports of illness associated with agents thought to be waterborne). CSTE passed a position statement at the 2006 annual meeting making waterborne-disease outbreaks, as a unit of reporting, nationally notifiable and reportable to CDC starting in 2007. Adoption of this CSTE recommendation at the state level through state-specific legislative action might improve reporting of waterborne outbreaks at the state and local levels. CSTE also asked CDC and EPA to 1) develop training for WBDO investigations for local and state/territorial public and environmental health workers responsible for WBDO detection, investigation, and reporting; and 2) work with CSTE and EPA to develop national WBDO investigation and surveillance guidelines. The position statement is available at http://www.cste.org/PS/2006pdfs/PSFINAL2006/06-ID-12FINAL.pdf (Box). Acknowledgments The authors thank the following persons for contributions to this report: state and territorial waterborne-disease surveillance coordinators, state epidemiologists, environmental health personnel, and state drinking water administrators; Michael F. Lynch, MD, Ciara E. O'Reilly, PhD, Claressa Lucas, PhD, Christopher Braden, MD, and Rachel Woodruff, MPH, Division of Foodborne, Bacterial and Mycotic Diseases, National Center for Zoonotic, Vector-Borne, and Enteric Diseases, (proposed), CDC; Matthew J. Arduino, DrPH, Division of Healthcare Quality Promotion, National Center for Preparedness, Detection, and Control of Infectious Diseases (proposed), CDC; Mark Eberhard, PhD, Monica E. Parise, MD, Dennis Juranek, DVM, Division of Parasitic Diseases, National Center for Zoonotic, Vector-Borne, and Enteric Diseases (proposed), CDC; John Sarisky, MPH, Division of Emergency and Environmental Health Services, National Center for Environmental Health, CDC; Lorraine Backer, PhD, Division of Environmental Hazards and Health Effects, National Center for Environmental Health, CDC. References
* Additional terms have been defined (Appendix A, Glossary of Definitions). Table 1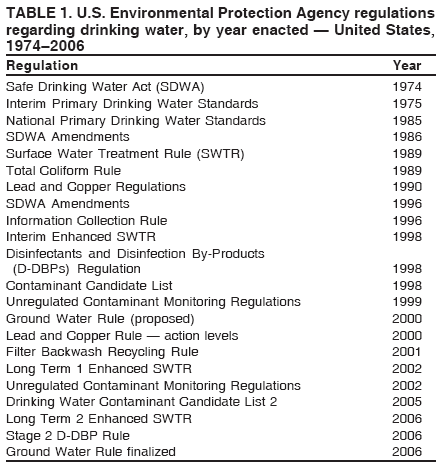 Return to top. Figure 1 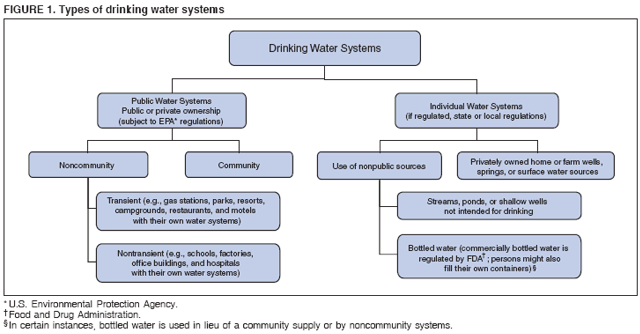 Return to top. Table 2 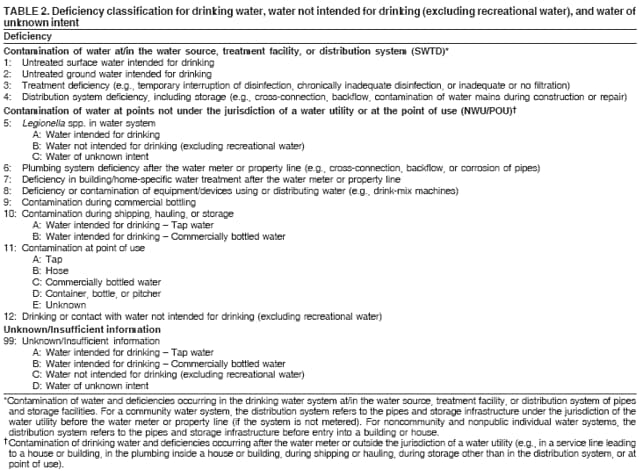 Return to top. Figure 2 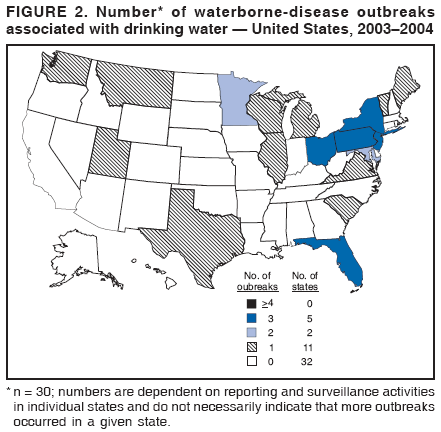 Return to top. Table 3 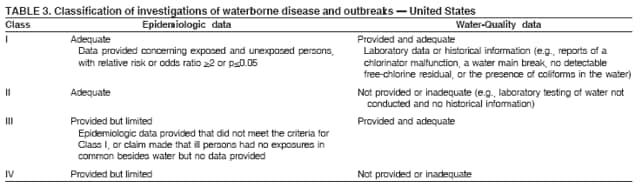 Return to top. Figure 3 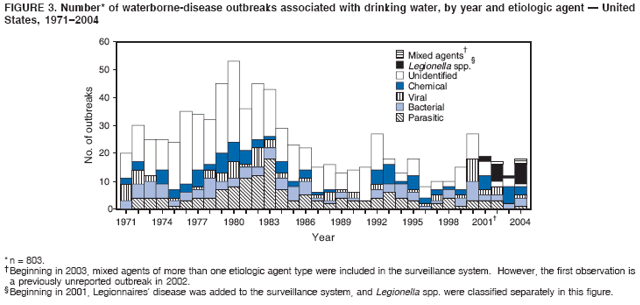 Return to top. Table 4 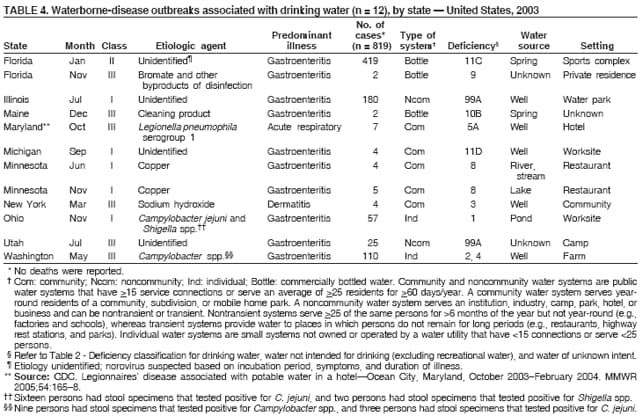 Return to top. Figure 4 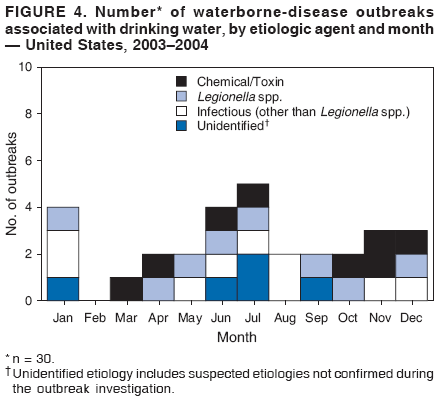 Return to top. Table 5 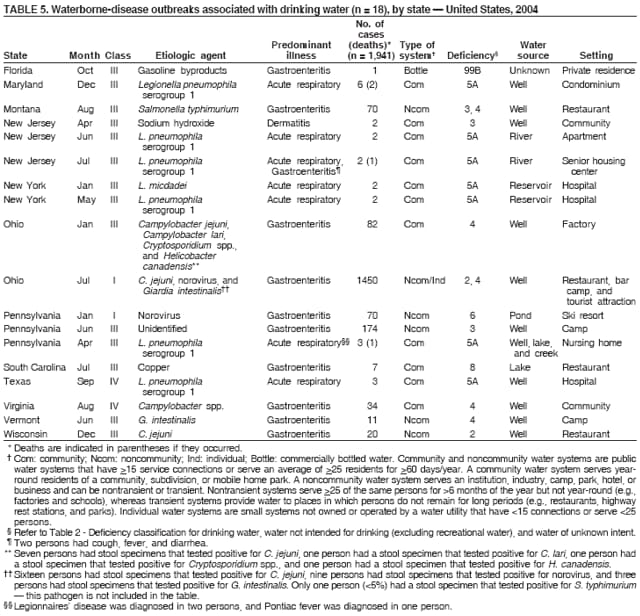 Return to top. Figure 5 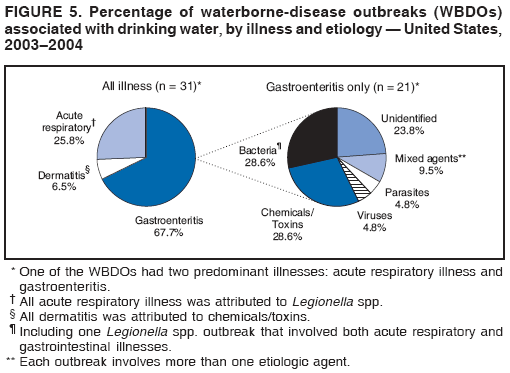 Return to top. Table 6 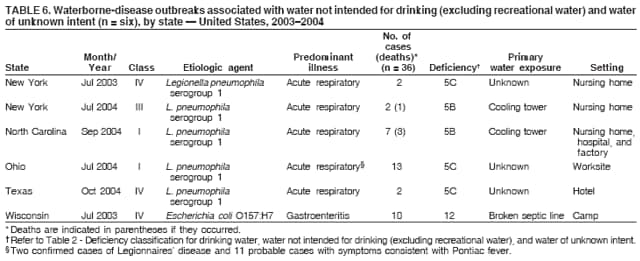 Return to top. Figure 6 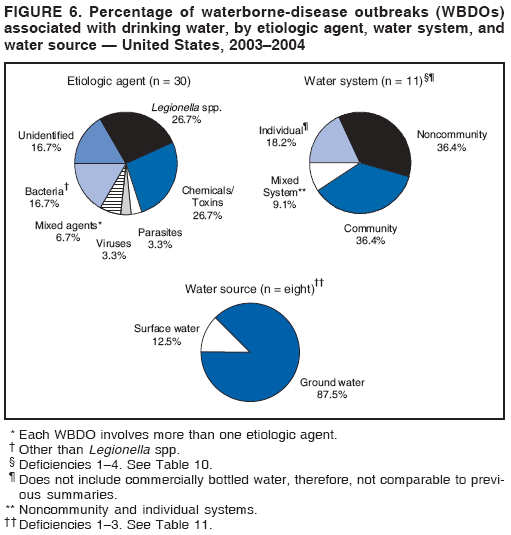 Return to top. Table 7 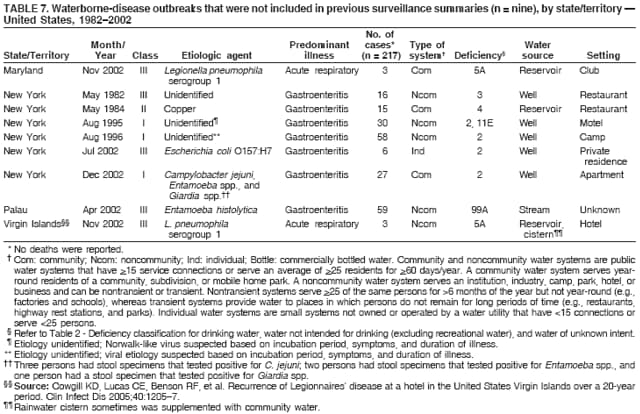 Return to top. Figure 7 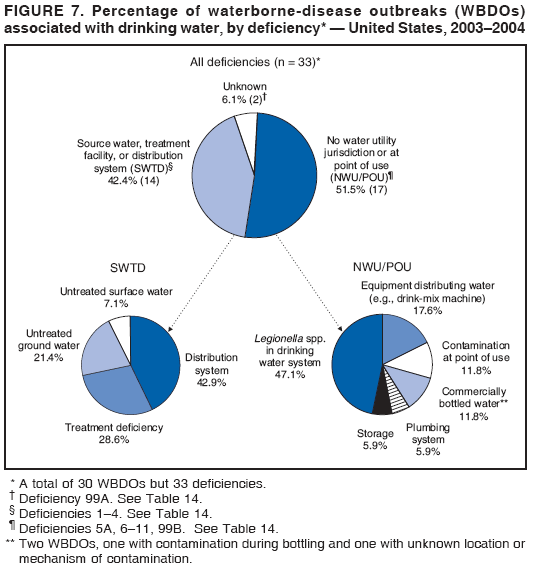 Return to top. Table 8 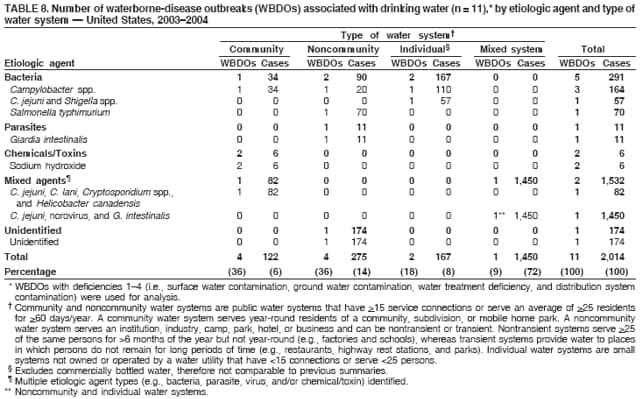 Return to top. Table 9 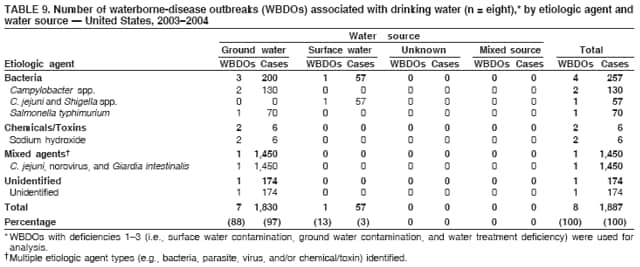 Return to top. Table 10 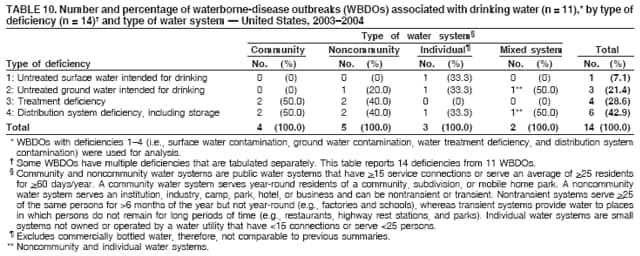 Return to top. Table 11 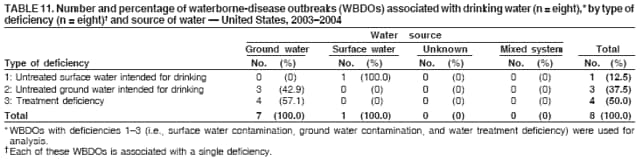 Return to top. Table 12 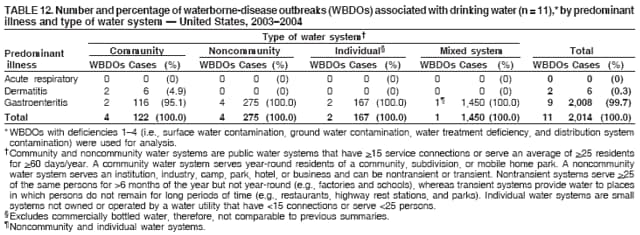 Return to top. Table 13 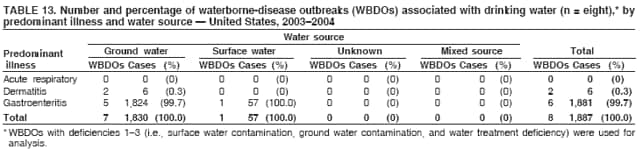 Return to top. Table 14 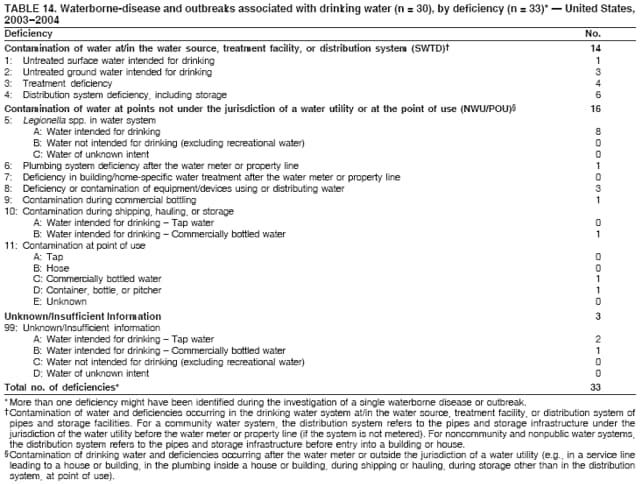 Return to top. Box 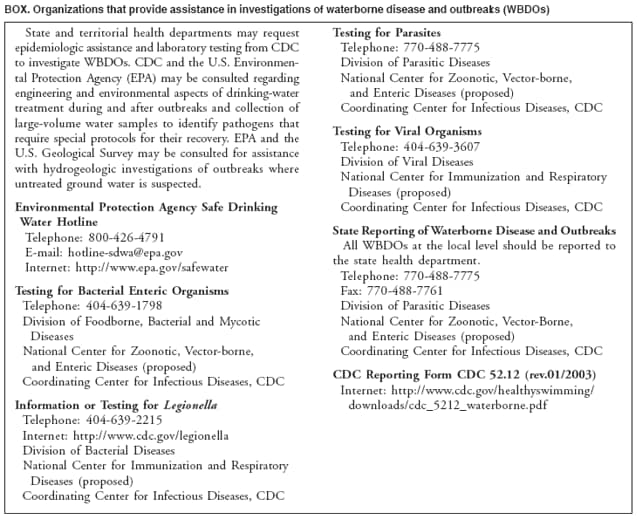 Return to top.
Disclaimer All MMWR HTML versions of articles are electronic conversions from ASCII text into HTML. This conversion may have resulted in character translation or format errors in the HTML version. Users should not rely on this HTML document, but are referred to the electronic PDF version and/or the original MMWR paper copy for the official text, figures, and tables. An original paper copy of this issue can be obtained from the Superintendent of Documents, U.S. Government Printing Office (GPO), Washington, DC 20402-9371; telephone: (202) 512-1800. Contact GPO for current prices. **Questions or messages regarding errors in formatting should be addressed to mmwrq@cdc.gov.Date last reviewed: 12/11/2006 |
|||||||||
|