IRIS® Registry
IRIS® Registry at a Glance
| IRIS® Registry | |
|---|---|
| Description | Developed by the American Academy of Ophthalmology, IRIS® Registry compiles information from participating ophthalmology practices’ electronic medical records systems. |
| Sample | Large convenience sample of patients visiting IRIS-participating ophthalmology practices, which includes approximately 95% of US ophthalmology practices, but an unknown percentage of ophthalmology patients. |
| VEHSS Topics Included |
|
| Approximate Size | Over 50 million patients per year |
Compiled by the American Academy of Ophthalmology (AAO), the IRIS® (Intelligent Research In Sight) Registry is the nation’s first comprehensive eye disease clinical registry. The IRIS® Registry enables ophthalmologists to use clinical data to improve care delivery and patient outcomes and help practices meet the requirements of the federal Physician Quality Reporting System (PQRS). The IRIS® Registry uses methods compliant with the Health Insurance Portability and Accountability Act of 1996 (HIPAA) to collect data from patient records directly from practices’ individual electronic medical record (EMR) systems. These EMR systems periodically report health record data based on the IRIS® Registry data fields on a nightly or weekly basis. The system tracks diagnosed disorders based on ICD-9/ICD-10 codes and includes procedures and visual acuity measures and other clinical data documented in the medical record.
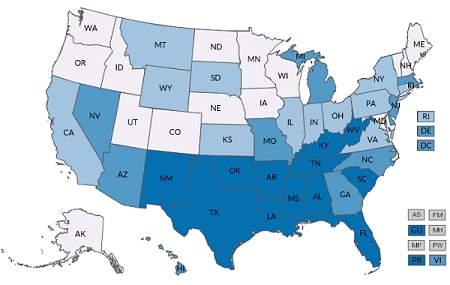
IRIS® Registry coverage began in 2013, and sample size has increased over time. As of 2019, IRIS® Registry contained more than 50 million patients and 230 million encounters. In 2018, the IRIS® Registry collected data from a convenience sample of more than 95% of ophthalmology practices nationally.
The main advantages of IRIS® Registry are its wide coverage and availability of diagnostic test results such as acuity values. However, IRIS® Registry is a convenience sample of ophthalmology practices and cannot by itself produce national prevalence estimates. IRIS® Registry has not been externally evaluated for data completeness, reliability, or validity. The IRIS® Registry team provided summary-level frequencies and prevalence values to the VEHSS system and has not granted access to person-level data. This limits the ability to assess the quality of IRIS® Registry data.
For the VEHSS project, the AAO calculated prevalence of diagnosed eye and vision disorders and prevalence of receipt of eye care services in the IRIS® Registry based on the presence of ICD9 and ICD10 diagnosis codes and CPT procedure codes on any patient record during the year of observation.
VEHSS reports summary prevalence rates for the topics and categories by the geographic levels and stratification factors listed below.
Note that patient counts and denominators for IRIS Registry are not publicly released; VEHSS releases only prevalence percentage and confidence intervals. In addition, the IRIS Registry dataset is not available in the VEHSS data portal. Please contact AAO for further information on the IRIS Registry.
Available Geographic Levels
| National | State |
|---|---|
| Included Stratification Factors (State and National Estimates) | |
|---|---|
| Age Group |
|
| Gender |
|
| Race/Ethnicity |
|
| Risk Factors |
|
| Data Type |
|
A detailed description of the analytical steps is described in the report “VEHSS Claims & Registry Data Analysis Plan [PDF – 579 KB] .”
Full analysis documentation is included in the “VEHSS IRIS® Registry Data Report [PDF – 1.5 MB] .”
AAO reported summary outcome statistics using VEHSS-defined data indicators and case definitions for visual function, eye examinations, and medical diagnoses. Some of the possible limitations include the following:
- VEHSS does not have access to patient-level data nor details on the process of mapping EMR data to IRIS® Registry. The quality of underlying EMR data, and the process of mapping EMR records to IRIS® Registry could not be validated.
- IRIS® Registry data represents a convenience sample of current ophthalmology patients and should not be considered representative of the general population. IRIS® Registry rates contained in this report are calculated per 100 current ophthalmology patients.
- IRIS® Registry does not include all ophthalmology practices and may be more likely to include private practices and practices who primarily serve Medicare patients because automated PQRS reporting is a motivating factor for providers to register with IRIS® Registry.
- IRIS® Registry only includes patients of ophthalmology practices. However, about 20% to 30% of providers in IRIS® Registry are optometrists who work for mixed-provider practices participating in IRIS® Registry.
- IRIS® Registry includes services provided regardless of payer but cannot identify the payer of specific procedures.