Comprehensive Suicide Prevention: Program Profiles

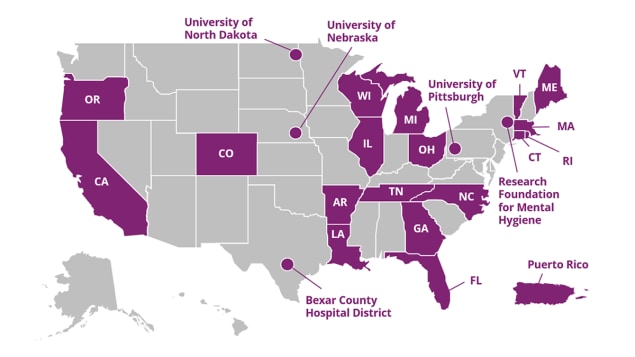
CDC’s Comprehensive Suicide Prevention Program (CSP) funds 24 programs to implement and evaluate a comprehensive public health approach to suicide prevention, with attention to populations that have higher suicide rates compared to other populations in the jurisdiction. CSP’s goal is to reduce suicide and suicide attempts among these populations by 10% over five years. Funded recipients are using data-driven decision-making to implement and evaluate the best available evidence to meet this ambitious goal.
NEW 2023 CSP Recipients:
- Arkansas Department of Health
- Bexar County Hospital District (Texas)
- Illinois Department of Health
- Ohio Department of Health
- Puerto Rico Department of Health
- Rhode Island Department of Health
- University of Nebraska
The CSP Program Profiles show how funded programs are working to implement and evaluate a comprehensive public health approach to suicide prevention. A comprehensive approach uses suicide prevention strategies from CDC’s Suicide Prevention Resource for Action. The seven strategies in the Prevention Resource help communities and states focus on prevention activities with the greatest potential to prevent suicide, and they are implemented on three levels:
- Community-based interventions
- Healthcare-based interventions
- Upstream interventions
- California Department of Public Health
- Colorado Department of Public Health and Environment
- Connecticut Department of Public Health
- Florida Department of Health
- Georgia Department of Public Health
- Louisiana Department of Health
- Maine Department of Health and Human Services
- Massachusetts Department of Public Health
- Michigan Department of Health and Human Services
Strengthen economic supports |
Create protective environments |
Improve access and delivery of suicide care |
Promote healthy connections |
Teach coping and problem-solving skills |
Identify and support people at risk |
Lessen harms and prevent future risk |

Website:
CDPH Suicide Prevention Program
Funding Amount:
- FY20: $900,000
- FY21: $900,000
- FY22: $1,033,000
- FY23: $1,033,000
Focus Populations:
13 counties in California with high rates of suicide and emergency department visits for self-harm
Examples of California’s CSP-funded suicide prevention activities:
- Promoting safe storage practices for both firearms and medications by:
- Training healthcare and behavioral healthcare providers and giving them messaging on safe storage to integrate suicide prevention into their practices
- Implementing the Pharmacists as Gatekeepers project to train pharmacists in suicide prevention practices, including safe storage of medications
- Providing Counseling on Access to Lethal Means (CALM) trainings to communities
- Disseminating educational materials to law enforcement and first responders to promote help-seeking behavior, including education on safe storage
- Sharing educational materials and campaigns that educate partners and community members about existing state policies around safe storage
- Training health and mental health providers, as well as pharmacists, to conduct suicide risk assessments that screen for and detect suicide risk and help connect people to services
- Promoting and advancing the implementation and use of telemental health in California
Leveraging CDC Suicide Prevention Resources to Expand Suicide Prevention Efforts in California
Suicide is a prevalent problem in California with statewide impact. In 2020, there were 4,140 suicide deaths among California residents. Many California counties have residents who are at increased risk for suicide, including counties that are rural and those where firearm ownership is common. The state also experienced a 65.5% increase in handgun ownership sales in 2020 compared to the previous year. Data [PDF – 7 pages] consistently show that firearms are the most common mechanism for suicide, and research has established a link between firearm ownership and increased risk for suicide. Additionally, poisoning [PDF – 2 pages] is a common method of suicide in California, especially for females. To address these issues, the Injury and Violence Prevention Branch (IVPB) within the California Department of Public Health is providing support to 13 counties that participate in the CDC-funded California Violent Death Reporting System and have higher suicide and self-harm injury rates than the state average.
California is using CSP funds to track suicide and self-harm emergency department visits and sharing these findings [PDF – 5 pages] to help build awareness for the need to prevent suicide statewide, and to use data to inform prevention efforts. California shared data with members of the legislature in hearings and with partners across multiple sectors through webinars, presentations, data briefs, and fact sheets.
Sharing these data helped facilitate an allocation of $2.78 million in state funding to establish the Office of Suicide Prevention (OSP), which is intended to be an overarching convener and coordinator of statewide suicide prevention efforts. The CSP program is planning to leverage OSP funding to expand its strategy of reducing access to lethal means among people at risk by purchasing lock boxes to safely store firearms and medications. Lock boxes will be provided to the CSP counties interested in promoting lethal means safety.

Website:
Colorado-National Collaborative
Funding Amount:
- FY20: $901,139
- FY21: $901,139
- FY22: $901,139
- FY23: $901,139
Focus Populations:
6 counties in Colorado with high counts and/or rates of suicide. Within these 6 counties, additional priority populations include:
Youth and young adults (0–24 years), middle-aged men (25–64 years), older adults (65+ years), veterans and military-involved families, LGBTQ+, BIPOC communities, people with disabilities, people working in high-risk industries (construction, agriculture and ranching, oil and gas, and emergency responders), and faith communities
Examples of Colorado’s CSP-funded suicide prevention activities:
- Partnering with counties and local organizations to conduct community events that foster and promote connectedness
- Strengthening postvention (activities which reduce suicide risk and promote healing after a suicide death for survivors of suicide) by coordinating resources and collaboration across counties to implement strategies—such as developing written policies for postvention response and training on responsible media messaging—that help support survivors of suicide loss and survivors of suicide attempts
- Providing gatekeeper training to organizations that serve older adults to enhance opportunities for older adult suicide prevention, and promoting connectedness by coordinating events to connect older adults with social and emotional resources
- Promoting connectedness among LGBTQ+ individuals by supporting public community events inclusive of LGBTQ+ identities, providing suicide prevention awareness training to LGBTQ+ serving organizations, and establishing or promoting Gay-Straight Alliances within schools
- Partnering with local leaders, government agencies, and other community groups to conduct community action planning focused on supporting economic stability initiatives, such as food security, affordable housing and transportation
Colorado-National Collaborative Partner Spotlight: Alliance for Suicide Prevention of Larimer County
The Colorado-National Collaborative (CNC)—supported largely by CSP funding—has an ambitious goal of reducing Colorado’s suicide rate 20% by 2024. CNC identifies, promotes, and implements successful state- and community-based comprehensive strategies for suicide prevention through partnerships among local, state and national scientists and public health professionals working with health and social service agencies, nonprofit organizations, government agencies, businesses, academic organizations and Colorado residents.
Colorado’s Office of Suicide Prevention uses a braided funding approach, including CSP funds, to fund local organizations across six Colorado counties to implement full-scale, community-based comprehensive prevention efforts. These efforts are rooted in six core pillars: Connectedness, Economic Stability, Education and Awareness, Improving Access to Safer Suicide Care, Lethal Means Safety, and Postvention—each adapted from the strategies of the CDC’s Preventing Suicide: A Technical Package of Policy, Programs, and Practices. CSP funding has allowed Colorado to increase personnel within the six counties and expand implementation and evaluation of specific activities.
CNC’s work in Larimer County highlights this collaborative work in action. Larimer County has participated in the CNC project since 2019 and is a priority county because of higher suicide-related indicators. In 2020, the county experienced 82 suicide deaths—a rate of 22.7 per 100,000 population, which is higher than the overall Colorado state rate of 21.5 per 100,000.
The Alliance for Suicide Prevention of Larimer County serves as the county hub for coordination of suicide prevention work across all six CNC core pillars. Examples of their recent activities include:
- Partnering with local food security, housing, and transportation organizations to address economic stability efforts in the community
- Hosting and supporting several events for LGBTQ+ connection
- Training over 2,500 community members per year in Question, Persuade, Refer (QPR), an evidence-based gatekeeper training program that teaches people about warning signs for suicide, how to respond, how to offer hope, and how to get help
- Promoting the Colorado Gun Shop Project that focuses on lethal means safety
- Hosting peer support groups that focus on priority populations including teens, working-aged men, and veterans
- Promoting Zero Suicide (a framework for system-wide transformation of healthcare settings toward safer suicide care) learning collaboratives and Collaborative Assessment and Management of Suicidality (CAMS) trainings
Website:
Connecticut Suicide and Self-Inflicted Injury Prevention Program
Funding Amount:
- FY20: $700,000
- FY21: $700,000
- FY22: $700,000
- FY23: $700,000
Focus Populations:
Youth and young adults (10–24 years), middle-aged adults (35–64 years), and older adults (65+ years)
Examples of Connecticut’s CSP-funded suicide prevention activities:
- Helping to reduce access to lethal means by:
- Promoting safe storage of firearms, prescriptions, and over-the-counter medications
- Expanding access to firearm trigger locks
- Intervening at suicide hotspots by posting suicide prevention signage in high-risk locations throughout the state (such as railroad platforms, bridges, highway overpasses, parking garages, state/local parks, and commuter lots)
- Implementing Counseling on Access to Lethal Means (CALM) training and safety planning at inpatient and outpatient healthcare facilities
- Reducing the stigma of help-seeking by implementing a mental health promotion and substance use prevention awareness campaign for people working in high-risk occupations, including law enforcement, physicians, dentists, corrections staff, and military (active and veteran)
- Providing postvention (activities which reduce risk and promote healing after a suicide death) grief and loss support and resources for suicide loss survivors
- Increasing awareness of mental health resources and services on college and university campuses and for military recruits at the Air and Army National Guard
- Empowering peers to be gatekeepers by understanding suicide warning signs and how to get help
- Supporting mental health and wellness for youth by promoting Gizmo’s Pawesome Guide to Mental Health—an evidence-based program that teaches youth in grades 3–5 how to take care of their mental health, encourages self-identification of warnings signs, and teaches coping strategies to help reduce risk
- Promoting the implementation of suicide risk screening [PDF – 2 pages] and Question, Persuade, Refer (QPR) gatekeeper training in healthcare and behavioral health systems
Connecticut’s CSP Program Shares Data with Local Partners to Inform Suicide Prevention
Prior to CSP funding, local health departments and districts (LHDs) in Connecticut did not have access to near real-time data from emergency departments (EDs) on suspected suicide ideation and suicide attempts. Instead, the state department of public health typically provided ED and hospital discharge data that was up to 18 months old, and only upon request. Connecticut’s CSP Team partnered with LHDs to improve access to near real-time ED data on suicide ideation and attempts.
Near real-time data, or syndromic surveillance, provides public health officials with a timely system for detecting, understanding, and monitoring health events such as suicidal ideation and suicidal attempts. Syndromic surveillance is important to improve awareness of suicide risks in jurisdictions. As a result of CSP funding, since late 2021, LHDs have been able to access syndromic data on suicide ideation and suicide attempts in emergency departments and urgent care centers within a day of occurrence. LHDs can now track counts and rates of suicide ideation and attempts as they occur—rather than waiting over a year for the data—so that they can more quickly address these issues and increase targeted awareness. LHDs can directly access the Connecticut Department of Public Health’s (DPH’s) EpiCenter syndromic surveillance system, which comprises 100% of Connecticut’s EDs and about 40 health system-affiliated urgent care centers.
Connecticut’s CSP program collaborated with three priority LHDs and trained them on the use of the suicide ideation and suicide attempt case definitions, and how to use the data dashboards in the EpiCenter system. LHDs can access aggregate data from 2019–2022 on the state-, county-, region-, LHD-, and zip code-levels, by home and facility location. They can also access line-level data for their jurisdictions’ residents, which include age, date of birth, zip code of residence, sex, race, ethnicity, facility, chief complaint, diagnosis codes, and triage notes. These data can be compared to the state and to other towns and regions in Connecticut, and data can also be compared across time periods. The dashboard is interactive and can be changed to suit the needs of the LHDs.
LHDs can use suicide-related syndromic data to identify populations at increased risk for suicide, connect and outreach to them, and target selected CSP strategies and interventions. LHDs can put data into action by using syndromic surveillance data to target their evidence-based approaches and reach at-risk people.
Website:
Funding Amount:
- FY22: $974,000
- FY23: $871,730
Focus Populations:
Youth and military personnel
Examples of Florida’s CSP-funded suicide prevention activities:
- Providing Applied Suicide Interventions Skills Training (ASIST) to medical providers in counties with the largest military populations.
- Training all county health departments and Veterans Affairs providers in the use of telehealth services and providing outreach and marketing to increase awareness of availability of these services to military personnel.
- Promoting healthy connections by training community-based organizations in Sources of Strength.
- Teaching coping and problem-solving skills in schools using the Strengthening Families Program curriculum.
Website:
Georgia Department of Public Health
Funding Amount:
- FY22: $871,730
- FY23: $871,730
Focus Populations:
Veterans and first responders, and Black Youth (10-24 years) in Clayton County
Examples of Georgia’s CSP-funded suicide prevention activities:
- Providing gatekeeper training to address suicidality and stigma associated with help-seeking among veterans and first responders.
- Collaborating with partners to develop safe messaging and promote existing resources that facilitate suicide prevention efforts.
- Supporting ED CALM trainings for clinicians and professionals within the hospital system and Veteran Administration facilities.
- Offering yearly train-the-trainer sessions to ensure hospital staff are kept up to date with surveillance data and emerging issues.
Website:
Louisiana Injury & Violence Prevention Program
Funding Amount:
- FY21: $651,000
- FY22: $784,000
- FY23: $784,000
Focus Populations:
Youth (10–19 years), veterans, and service members
Examples of Louisiana’s CSP-funded suicide prevention activities:
- Partnering with the Family Tree to provide in-person and virtual Question, Persuade, Refer (QPR) gatekeeper trainings to youth and youth-serving organizations, and disseminating information on youth suicide prevention services and behavioral health resources to training participants
- Partnering with the National Suicidology Training Center (NSTC) to:
- Train healthcare providers working with service members, veterans, and youth, focusing on safety planning, reducing access to lethal means, and safe storage practices for firearms and medications
- Train peers to facilitate peer support groups, focusing on topics including supporting those experiencing suicidal thinking and coping with suicide bereavement
- Partnering with Beacon Community Connections to work with hospitals, law enforcement, and hospital intake specialists to provide care coordination services (such as follow-up services and resources) to youth who visited the emergency department or were admitted to a hospital due to suicidal ideation or attempt
- Partnering with Volunteers of America Greater Baton Rouge to provide peer support services to veterans and service members with a focus on strengthening their household security by connecting them to financial supports and benefit programs
Website:
Maine Suicide Prevention Program
Funding Amount:
- FY21: $849,000
- FY22: $982,000
- FY23: $982,000
Focus Populations:
Rural residents, adults (45+ years) and LGBTQIA+ youth (11–24 years)
- Partnering with the National Alliance on Mental Illness (NAMI) Maine to provide gatekeeper training to individuals (such as home health aides, physical and occupational therapists, and visiting nurses) and nursing and rehabilitation organizations that serve vulnerable populations (adults 45+ years and those living in rural areas) to help identify those at risk for suicide and refer them to care
- Implementing Sources of Strength (SOS) interventions (a program that aims to prevent suicide by increasing help-seeking behaviors and promoting connections between peers and caring adults) to enhance resiliency among LGBTQIA+ youth in school and out-of-school settings
- Collaborating with NAMI Maine to provide SOS training to adult advisors and peer leaders participating in LGBTQIA+ youth-serving organizations
- Expanding postvention (activities which reduce risk and promote healing after a suicide death) to respond to suicides among adults living in rural areas by increasing awareness of and providing access to mental health services and bereavement support after a suicide
- Partnering with the Maine Primary Care Association to implement the Zero Suicide model (a framework for system-wide transformation of healthcare settings toward safer suicide care) in rurally-located community health centers
- Providing community health centers with training and capacity-building for suicide-safer care, including risk screening and assessment, safety planning, evidence-based treatment, and ongoing care management
- Partnering with schools and community behavioral health providers to reduce provider shortages in rural areas by supporting the implementation and availability of tele-behavioral health programs facilitated by community health worker in schools across the state
Website:
Massachusetts Suicide Prevention Program
Funding Amount:
- FY20: $650,000
- FY21: $650,000
- FY22: $650,000
- FY23: $650,000
Focus Populations:
Men of working age (25–64 years) and in certain occupations (construction and fishery), Hispanic/Latinx men, youth and young adults (11–24 years), and military/veterans
Examples of Massachusetts’s CSP-funded suicide prevention activities:
- Implementing the Signs of Suicide (SOS) curriculum, a suicide prevention program that educates students about the relationship between suicide and depression. This program aims to prevent suicide by increasing help-seeking behaviors and promoting connections between peers and caring adults in vocational and technical high schools to reach students who are training for occupations that are at higher risk for suicide.
- Developing a marketing campaign to help men self-identify mental health issues and gain confidence in seeking support for mental health
- Increasing the diversity and inclusivity of the MassMen website—which aims to prevent suicidality among Massachusetts men by promoting their personal mental health and well-being—to reach men of color and gender and sexual minorities
- Providing Question, Persuade, Refer (QPR) gatekeeper training to:
- MassHire Career Centers, which provide jobseekers with career guidance and referrals to jobs and training
- Community behavioral health providers and clinicians in communities with high Hispanic/Latinx populations, as well as those serving youth or serving men in occupations at higher risk for suicide
- Translating and providing QPR and Mental Health First Aid (MHFA) gatekeeper trainings in Spanish to community providers and clients in communities with strong Hispanic/Latinx populations
- Providing training to community behavioral health centers on cultural competency and racial equity to increase understanding of how suicidality is impacted by these factors
- Building resiliency and problem-solving skills in Hispanic/Latinx youth by training elementary school teachers and counselors on how to implement the Good Behavior Game (a classroom management game that aims to reduce aggressive, disruptive classroom behavior, which is a shared risk factor for later problems such as suicidal ideation and behavior)
Building Partnerships with Lawrence Public Schools to Prevent Suicide Among Latinx Youth
The Massachusetts Department of Violence and Injury Prevention’s Comprehensive Suicide Prevention (CSP) program implements upstream prevention strategies that include training elementary, trade/vocational, and high school personnel in teaching coping and problem-solving skills in youth, as well as supporting, assessing, and managing suicidality among Latinx youth. Massachusetts’s CSP program focuses on Latinx individuals and specifically Latinx males, a priority population that experiences significant health disparities related to mental health and lack of access to care.
Evidence shows there is a lack of access to care and resources for suicide prevention for Latinx and other people of color, due in part to deficiencies in reporting of their suicides. According to data from the CDC-funded Massachusetts Violent Death Reporting System (MVDRS), suicides among Latinx males rose 33% between 2018 and 2019. While youth suicide rates have been declining since 2016, suicide is still the 2nd leading cause of death among youth aged 10–24 years in both Massachusetts and the country overall as of 2020. Additionally, between 2017–2019, according to the MA Youth Risk Behavior Survey, Hispanic students were significantly more likely to report attempting suicide compared to White, non-Hispanic students.
Massachusetts’s CSP program has partnered with Lawrence Public School (LPS) to engage in their project and receive support for their current suicide prevention efforts. The program will offer various evidence-based suicide prevention trainings to school staff including Question, Persuade, Refer (QPR) and Youth Mental Health First Aid (YMHFA). Additionally, the CSP program is also offering Assessment and Management of Suicide Risk (AMSR) and Safety Planning Intervention (SPI), which are specialized trainings that teach clinicians and healthcare professionals who conduct suicide risk assessments how to determine the level of suicide risk for an individual, with concrete tools to develop a safety plan in collaboration with the person at risk. The trainings will be offered to school staff such as social workers, psychologists, mental health counselors, adjustment counselors, and cultural specialists as well as community providers.
With the Lawrence community’s participation as well as the LPS officials’ participation and partnership in this project, Massachusetts’s CSP Program will deliver trainings that are culturally appropriate and will advance staff’s capacity and knowledge in promoting help-seeking behaviors and reducing the risk for suicide among their Latinx students and residents.
Website:
Funding Amount:
- FY20: $870,000
- FY21: $870,000
- FY22: $1,003,000
- FY23: $1,002,187
Focus Populations:
Males 25+ years
Examples of Michigan’s CSP-funded suicide prevention activities:
- Promoting, sponsoring, and hosting gatekeeper trainings, such as Assessing and Managing Suicide Risk (AMSR) and Applied Suicide Intervention Skills Training (ASIST), to community gatekeepers statewide, including:
- Working with the Michigan Department of Corrections to implement policies related to suicide prevention, and facilitate gatekeeper trainings among mental and physical health providers to improve response to the corrections population as well as correctional staff who have expressed suicidal ideation
- Increasing the capacity to host gatekeeper trainings by hosting “training for trainers” to create a greater number of available trainers statewide
- Reducing access to lethal means among people at risk by distributing and promoting gun locks and safe storage messages at gatekeeper trainings
- Launching and promoting Man Therapy Michigan, a website that serves as a mental health and suicide prevention intervention for working age adult men and provides information and resources for mental health, coping, resilience, and connection to services
- Developing and disseminating safe messaging standards for reporting on suicide as well as safe messaging for social media, and working with mass communications departments at universities statewide to ensure safe messaging guidelines are taught and applied
- Reducing provider shortages by developing and disseminating a telemental health toolkit that providers can use statewide to provide quality suicide care on virtual platforms for potential increases in access and use of telemental health services
Creating a Diverse Multi-Sectoral Partnership to Reduce Suicide Among Michigan Men
A key component of comprehensive suicide prevention is establishing a multi-sectoral partnership to help address suicide. Michigan’s Comprehensive Suicide Prevention (CSP) program, Preventing Suicide in Michigan Men (PRiSMM), brings together key individuals, organizations, and stakeholders to form the PRiSMM Partnership, which works to prevent suicide in Michigan men, a population that is at disproportionate risk for suicide. PRiSMM includes organizations in the construction, automotive, farming, and television and media industries, as well as the faith community. It includes individuals invested in reducing male suicides but who may not work in the suicide prevention field, as well as individuals working in agriculture, automotive, and construction industries who are able to inform the PRiSMM Partnership of gaps and barriers in suicide messaging. Many of the individuals involved in PRisMM interact with adult men and provide the perspective of Michigan men to help further the work of the overall project.
One of PRiSMM’s non-traditional partners oversees Michigan’s largest construction company. As a result of their participation in PRiSMM, this company plans to implement strategies to improve mental health and suicide prevention among its employees. This partner has also been able to provide insight on how PRiSMM’s suicide prevention messaging can reach Michigan men who work in construction.
PRiSMM shares data and information across a wide network. PRiSMM created a suicide prevention social media guide, a risk factors and warning signs guide, and data presentations to disseminate and inform the PRiSMM Partnership about suicide data and suicide prevention efforts that could be and are implemented in Michigan. PRiSMM also creates and disseminates a quarterly newsletter to keep the Partnership informed of data trends and prevention efforts. The PRiSMM Partnership has pushed a community-driven approach to implementation of suicide prevention efforts, and this approach is critical to the success of suicide prevention among Michigan men.
Website:
Research Foundation for Mental Hygiene, Inc.
Funding Amount:
- FY22: $973,053
- FY23: $973,053
Focus Populations:
Working aged men (25-64), adolescent girls (12-17)
The Research Foundation for Mental Hygiene, Inc is a private, not-for-profit membership corporation organized in 1952, for the purpose of assisting and enhancing the research and training objectives of the New York State Department of Mental Hygiene and its component agencies; the Office of Mental Health, the Office for People with Developmental Disabilities and the Office of Addiction Services and Supports.
Examples of Research Foundation for Mental Hygiene’s CSP-funded suicide prevention activities:
- Partnering with juvenile justice stakeholders, county mental health organizations and youth probation departments to expand e-Connect. E-Connect allows probation staff to provide tablets to youth to complete a self-administered evidence-based screen, quickly identifying those at risk for suicide and connecting them with needed services.
- Providing professional development trainings and workshops including Creating Suicide Safety in Schools, Helping Students at Risk for Suicide, Suicide Safety for Teachers & School Staff, and school programming including Invisible Mentoring and Up to Me program to school staff.
- Increasing access to the Crisis Text Line (CTL) for distressed youth by tailoring campaigns through the use of social media, public announcements, postingCTL posters and stickers in hallways, bathrooms, on back of student IDs, etc.
Website:
Funding Amount:
- FY20: $870,000
- FY21: $870,000
- FY22: $1,003,000
- FY23: $1,003,000
Focus Populations:
Males, rural counties, veterans, and LGBTQ+ youth (10–18 years)
Examples of North Carolina’s CSP-funded suicide prevention activities:
- Planning and hosting the CSP Injury Free NC Academy, a 2-day event that teaches community-based partners to recognize and appropriately respond to suicidality in youth
- Conducting Counseling on Access to Lethal Means (CALM) and Applied Suicide Intervention Skills (ASIST) gatekeeper trainings, in “Train-the-Trainer” events across North Carolina to expand the database of trainers in North Carolina
- Providing Faith, a gatekeeper training designed specifically for the faith community to equip faith leaders to recognize warning signs for suicide and make referrals to care
- Creating and maintaining an interactive, searchable online inventory of suicide prevention efforts across North Carolina
- Expanding the number of Firearm Safety Teams (FST), which consist of local partners who collaborate on safe storage education and strategies
- Developing online trainings to teach communities how to create their own FST
- Partnering with Appalachian State University and NC Department of Health and Human Services to publicly disseminate a map of safe storage locations across the state
Expanding CALM Training Capacity Across North Carolina
North Carolina’s Comprehensive Suicide Prevention (CSP) team is supporting and promoting Counseling on Access to Lethal Means (CALM) training statewide. This training is an evidence-based, effective suicide prevention strategy. Initially, there was no central registry or tracking of CALM trainers in the state, and only two people in the entire state could be identified as CALM trainers. The CSP team partnered with the existing two trainers to conduct three CALM Train-the-Trainer (T4T) events: two in the Fall of 2021 and one in the Fall of 2022. The first two trainings trained 18 additional trainers. A few weeks after the first T4T, the CSP team received feedback from a new trainer concerning a session with a young client:
“Could you please pass on my appreciation for this training? I was able to apply what I learned in training during a session and believe it made a considerable difference in safety.”
After the team announced to partners that there is a team of CALM trainers ready and available, they’ve received requests from multiple parties requesting CALM trainings in their communities. North Carolina’s CSP team checks in with the trainers quarterly, keeping their contact information and availability up to date, and collecting data on how many trainings they have done, numbers of participants, and more. Of the 100 counties in North Carolina, 15 are currently in the coverage area of a CALM trainer. The CSP team anticipates both the number of trainers and how much of North Carolina is covered will increase after the Fall 2022 CALM Train-the-Trainer event.

Website:
Funding Amount:
- FY22: $955,014
- FY23: $871,730
Focus Populations:
Rural residents, Veterans, and LGBTQ+ youth
Examples of the University of North Dakota’s CSP-funded suicide prevention activities:
- Reducing access to lethal means by distributing gun locks and promoting safe storage.
- Providing gatekeeper training in schools and community-based settings.
- Promoting protective factors, resilience, trusting relationships, and help-seeking in schools by providing Sources of Strengths training and engaging peer leaders with adult advisors and students.
- Implementing Zero Suicide in primary care and hospital settings to identify and treat those at risk with evidence-based suicide care.
- Expanding access to telemental health to address provider shortages in rural areas.
Website:
Funding Amount:
- FY22: $855,000
- FY23: $855,000
Focus Populations:
Rural residents, rural residents aged 55 and older, and veterans
Examples of Oregon’s CSP-funded suicide prevention activities:
- Partnering with state & local law enforcement agencies to develop suicide safer Extreme Risk Protection Orders
- Providing culturally adapted QPR and ASIST trainings for rural older firearm owners, veterans, certified older adult peer specialists, members of assisted living communities and caregivers.
- Expanding partnerships with organizations that serve rural residents and veterans (Shooting Sports Association, Veterans of Foreign Wars, Foreign Legion, Elks, gun clubs, senior centers, churches, assisted living facilities) to recruit trainees.
- Providing PEARLS Training to behavior health specialist in senior centers.
Website:
Funding Amount:
- FY20: $598,861
- FY21: $700,000
- FY22: $833,000
- FY23: $700,000
Focus Populations:
Veterans in Northwest Pennsylvania (15 counties)
Examples of University of Pittsburgh’s CSP-funded suicide prevention activities:
- Developing firearm suicide prevention tools, campaigns, and trainings for firearm retailers and owners to identify individuals at risk for suicide and reduce access to lethal means among people at risk
- Planning gatekeeper trainings, such as Question, Persuade, Refer (QPR) and Applied Suicide Intervention Skills Training (ASIST), for healthcare providers, law enforcement, and community members to increase knowledge and awareness of suicide first aid
- Collaborating with a local nonprofit, Hold My Guns, to encourage local firearm retailers to provide offsite safe storage options
- Collaborating with community partners to distribute safe storage items including gun locks and prescription lock boxes
- Promoting and hosting community greening initiatives and local engagement activities to reduce social isolation and promote connectedness
- Partnering with primary care and emergency department settings to implement Zero Suicide (a framework for system-wide transformation of healthcare settings toward safer suicide care) by screening, treating, and referring patients to treatment and providing sustained follow-up care
- Training and educating healthcare providers on using the Columbia-Suicide Severity Rating Scale (C-SSRS), an evidence-based fast and effective suicide screening tool
- Training healthcare providers in primary care and emergency department settings on brief interventions, referral to treatment using warm handoffs, and active follow-up contacts
- Raising awareness and providing education on Pennsylvania’s mental health parity laws and regulations to healthcare providers and community members
The Northwest Pennsylvania Veteran Suicide Prevention Program Implements Gatekeeper Training to Help Prevent Suicide Among Veterans
The Northwest Pennsylvania Veteran Suicide Prevention Program, housed in the University of Pittsburgh School of Pharmacy’s Program Evaluation and Research Unit (PERU), is a collaborative effort between healthcare partners, community organizations, and veteran groups to create significant and lasting change and help prevent veteran suicide in the 15-county northwest Pennsylvania region. The program aims to reduce veteran suicide attempts, injuries, and deaths by 10% over five years. Primary goals are improving access to treatment and support services, increasing awareness of suicide risk, and targeted suicide prevention activities and training opportunities.
Funded by CDC’s Comprehensive Suicide Prevention program, the Northwest Pennsylvania Veteran Suicide Prevention Program provides the Question, Persuade, Refer (QPR) gatekeeper training to healthcare and community organizations throughout the 15-county region. QPR is an evidence-based training that can reduce suicide morbidity and mortality. Such training teaches individuals to recognize a crisis and the warning signs of someone contemplating suicide. Anyone can become a gatekeeper: parents, friends, neighbors, teachers, athletic coaches, ministers, doctors, nurses, office supervisors, squad leaders, police officers, advisors, caseworkers, firefighters, and others. In its inaugural year, the program had overwhelming success in conducting gatekeeper training sessions. The program team planned 12 two-hour virtual QPR trainings scheduled to occur from March to August 2022.
The QPR trainings were promoted widely, including among professional networks, on social media, and on the program website, The Resilient Veteran. As a result of these efforts, all 12 QPR sessions were filled within five days of opening registration. Between March and June 2022, 381 individuals were trained in QPR. Because of this outpouring of support and interest, eight additional QPR sessions were scheduled through December 2022 to accommodate wait-listed individuals. Through these training sessions, the Northwest Pennsylvania Veteran Suicide Prevention Program is providing essential skills to help reduce veteran suicide.
Website:
Funding Amount:
- FY20: $750,000
- FY21: $750,000
- FY22: $883,000
- FY23: $883,000
Focus Populations:
All rural residents, males in rural areas, and rural residents ages 15–64 years
Examples of Tennessee’s CSP-funded suicide prevention activities:
- Identifying and supporting people at risk for suicide by increasing education through gatekeeper training (including Question, Persuade, Refer (QPR), Applied Suicide Intervention Skills Training (ASIST), and Be The One (BTO)) in organizations including behavioral health organizations, high schools and higher education institutions, detention centers, and occupational therapy centers
- Expanding gatekeeper training to healthcare and behavioral healthcare providers in rural areas to reach rural residents, including males and people ages 15–64 years
- Providing safer suicide care through systems change by implementing the Zero Suicide model (a framework for system-wide transformation of healthcare settings toward safer suicide care) in healthcare and behavioral healthcare agencies
- Improving access to mental healthcare and resources by reducing provider shortages in underserved rural areas through telemental health training to providers
- Increasing coverage of mental health conditions in health insurance policies by providing education on mental health parity laws
- Teaching coping and problem-solving skills by increasing social-emotional learning programs such as the Sources of Strength (a classroom management game that aims to reduce aggressive, disruptive classroom behavior, which is a shared risk factor for later problems such as suicidal ideation and behavior) in K-2 classrooms
Suicide Prevention Stakeholder Task Force Expands Reach and Representation
Tennessee’s Suicide Prevention Act of 2018 recognized suicide as a serious public health issue in Tennessee and provided the Commissioner of Health authorization to create a suicide prevention program within the Tennessee Department of Health (TDH). One of the provisions of that act required the TDH to convene relevant partners to review existing data, programs, and resources and identify opportunities to improve data collection, analysis, and programming. First convened in February 2019, the Suicide Prevention Stakeholder Task Force included a diverse group of individuals from across the state representing many sectors involved in suicide prevention activities. The task force convened quarterly to review statewide suicide-related data, programs, and services and to identify opportunities for improving statewide suicide prevention efforts. While the Act expired in June of 2021, TDH continues their work through the Comprehensive Suicide Prevention (CSP) program.
Funding from CDC’s CSP program allowed for the hiring of additional staff to identify populations who are most at risk for suicide, expand suicide-related syndromic surveillance, analyze suicide-related data, implement prevention strategies, and raise awareness of suicide prevention efforts. To support these activities, TDH focused on increasing task force members in disciplines not represented with a goal of multi-disciplinary representation from multiple regions of the state.
The initial task force included members representing healthcare organizations, behavioral healthcare organizations, law enforcement, community-based organizations, emergency response, higher education institutions, substance use treatment facilities, crisis services, military and veteran affairs, and local schools.
Since receiving CSP funding TDH added 69 new members, growing the task force to 99 members. These individuals expanded the reach and representation on the task force and included occupational groups such as construction workers, pharmacists and nurses, vulnerable populations such as men and people with disabilities, rural health care providers, and county government officials.
The TDH strengthened its comprehensive public health approach to suicide prevention by increasing the number of multi-sectoral partners participating in its Suicide Prevention Stakeholders Task Force by nearly 183% and increased attendance and participation in quarterly meetings by 65%. Through this work, TDH has increased their capacity to carry out a comprehensive approach to suicide prevention.
Website:
Funding Amount:
- FY20: $760,000
- FY21: $760,000
- FY22: $893,000
- FY23: $893,000
Focus Populations:
Vermont residents (15–64 years), people with a disability, LGBTQ people, males, and rural residents
Examples of Vermont’s CSP-funded suicide prevention activities:
- Working with hospitals and emergency departments to deliver emergency department Counseling on Access to Lethal Means (CALM) and to incorporate CALM into the list of required training for providers
- Disseminating safe reporting and messaging about suicide guidelines to media partners
- Providing gatekeeper trainings, including Question, Persuade, Refer (QPR), Umatter, and Mental Health First Aid (MHFA), to community partners
- Developing peer support networks among at-risk populations, including first responders, farmers, and suicide loss survivors
- Expanding Zero Suicide (a framework for system-wide transformation of healthcare settings toward safer suicide care) across Vermont primary care practices and hospital emergency departments
- Organizing and hosting trainings to increase mental health providers who can provide suicide safer care via telemental health
- Developing and delivering safe storage training to providers and community members to promote safe storage, including firearm safe storage among rural males, and medication safe storage focused on youth and their families
- Collaborating with Vermont Poison Control Center to develop the Self-Poisoning Prevention Toolkit for Healthcare Providers focusing on youth and their families for use in medical care settings, including emergency departments
- Implementing a public health campaign to raise awareness, reduce the stigma associated with suicide, and increase help-seeking behavior among Vermonters experiencing suicidality
Vermont Department of Health Uses Public-Private Partnership to Improve Emergency Department Suicide Prevention
Vermont has over 1,000 visits to hospital emergency departments (EDs) for intentional self-harm and 4,000 visits for suicidal ideation and self-directed violence each year on average [PDF – 19 pages], yet there is no state-wide model or standard of care for improving suicide care in these settings. EDs and hospitals have also experienced additional pressures due to COVID-19 and shortages in psychiatric inpatient capacity. These factors make it an especially challenging time to engage with EDs to improve mental health and suicide prevention care.
With funding from CDC’s Comprehensive Suicide Prevention program, the Vermont Department of Health (VDH) engaged with the Vermont Program for Quality in Health Care, the Department of Mental Health, the Vermont Association of Hospitals and Health Care Systems, and a private foundation to jointly develop and fund a multi-year quality improvement project to improve screening, assessment, safety planning to reduce access to lethal means, and follow-up care for individuals at risk for suicide in EDs. The project operates under a larger initiative to collaborate with Vermont hospital EDs and support them with monetary, educational, and networking resources to enhance their ongoing quality improvement work to improve care for individuals that present to EDs with mental health and/or substance use needs.
VDH has successfully recruited all of Vermont’s 14 community hospitals to participate in the initiative, and each hospital ED has committed to the following activities in year one: 1) Complete a Zero Suicide organizational assessment, 2) identify a suicide prevention quality improvement project and accompanying metrics to show impact, 3) report on progress at 6- and 12-month marks, 4) engage in suicide prevention in ED educational and networking opportunities, 5) establish a suicide prevention team in the ED implementation team, and 6) train core ED staff on Counseling on Access to Lethal Means (CALM).
Engaging with hospitals in quality improvement activities can be accomplished through key partnerships and programs that are trusted by and have a history of working with hospital EDs, and incentives can also help support participation in those quality improvement activities.
Website:
Wisconsin Department of Health Services
Funding Amount:
- FY22: $868,730
- FY23: $868,730
Focus Populations:
Females aged 10-19, Rural males aged 25 and older
Examples of Wisconsin’s CSP-funded suicide prevention activities:
- Implementing the PRISM Program, a mental wellness resource for LGBTQ+ youth. Offering free one-on-one support through a warmline and support groups online and in-person.
- Implementing the Gun Shop Project and providing safe storage.
- Implementing the LOSS (Local Outreach to Suicide Survivors) team support model.