Background and Rationale — CDC Guidance for Communities Assessing, Investigating, and Responding to Suicide Clusters, United States, 2024
Supplements / February 29, 2024 / 73(2);1–7
Michael F. Ballesteros, PhD1; Asha Z. Ivey-Stephenson, PhD1; Eva Trinh, PhD1; Deborah M. Stone, ScD1 (View author affiliations)
View suggested citationAltmetric:
Summary
To assist community leaders in public health, mental health, education, and other fields with developing a community response plan for suicide clusters or for situations that might develop into suicide clusters, in 1988, CDC published Recommendations for a Community Plan for the Prevention and Containment of Suicide Clusters (MMWR Suppl 1988;37[No. Suppl 6]:1–12). Since that time, the reporting and investigation of suicide cluster events has increased, and more is known about cluster risk factors, assessment, and identification. This supplement updates and expands CDC guidance for assessing, investigating, and responding to suicide clusters based on current science and public health practice. This report is the first of three in the MMWR supplement that describes an overview of suicide clusters, information about the other reports in this supplement, methods used to develop the supplement guidance, and the intended use of the supplement reports. The second report, CDC Guidance for Community Assessment and Investigation of Suspected Suicide Clusters — United States 2024, describes the potential methods, data sources and analysis that communities can use to identify and confirm suspected suicide clusters, and better understand the relevant issues. The final report, CDC Guidance for Community Response to Suicide Clusters — United States, 2024, describes how local public health and community leaders can develop a response plan for suicide clusters. The guidance in this supplement is intended as a conceptual framework that can be used by public health practitioners and state and local health departments to develop response plans for assessing and investigating suspected clusters that are tailored to the needs, resources, and cultural characteristics of their communities.
Introduction
In 2021, approximately 48,000 lives were lost to suicide in the United States (1). During this time, suicide was among the 10 leading causes of death among persons aged 10–64 years and the second leading cause of death among children and adolescents aged 10–14 and adults aged 25–34 years. Suicide rates peaked in 2018, followed by two consecutive years of declines (5%) during COVID-19; during 2020–2021, rates nearly rebounded to the 2018 peak (1,2). Age-adjusted rates increased approximately 36% from 10.4 suicides per 100,000 population in 2000 to 14.1 in 2021 (1,3). Many more persons think about or attempt suicide. In 2021, a total of 12.3 million U.S. adults reported serious thoughts of suicide, 1.7 million attempted suicide (4), 22% of high school students seriously considered suicide, and 10% attempted suicide (5).
When a group of suicides or suicide attempts occur closer together in time, space, or both than would normally be expected in a community, they are defined as a suicide cluster (6,7). Suicide clusters are rare and are believed to comprise only a small proportion of overall deaths by suicide; for example, in the United States, an estimated 1%–2% of teenage suicides are part of clusters (8). However, suicide clusters can have unique characteristics and challenges and, when they occur, are often highly publicized and can have considerable negative effects on the community, including prolonged grief and elevated fear and anxiety about further deaths (9,10).
Overview and Types of Suicide Clusters
Suicide clusters have been reported in diverse populations and settings including psychiatric inpatients (11,12), teenagers and young adults (8,13–15), schools (16–18), prison inmates (19,20), and American Indian and Native American communities (21–25). The two most commonly reported types of suicide clusters are point clusters and mass clusters. Point clusters (or spatial-temporal clusters) represent a greater-than-expected number of suicides or suicide attempts that occur within a time period in a specific location (https://www.cdc.gov/suicide/resources/suicide-clusters.html). Point clusters might occur in a community/county or an institution such as a school, university, or psychiatric inpatient setting. Mass clusters (or temporal clusters) represent a greater-than-expected number of suicides or suicide attempts spread out geographically within a time period (https://www.cdc.gov/suicide/resources/suicide-clusters.html).
The causes of suicide clusters are not well understood. Available reports of point clusters tend to only describe the characteristics of decedents involved in the cluster and are not designed to rigorously assess risk. Persons involved in point clusters tend to be male and adolescents or young adults and have a history of substance use, self-harm, and mental illness (7,26–28). Risk factors for point clusters are postulated to be the same as general risk factors for suicide (28) and therefore do not aid in identifying those most at risk for becoming part of a suicide cluster.
Certain methodological barriers have been identified that preclude better understanding of cluster risks. These barriers include selection bias in the available reported clusters, limited opportunities for comparison groups, relatively small numbers of suicides in diverse populations, and the absence of a standard definition for time and space parameters (28,29), which make combining or comparing individual case studies challenging. In addition, no standard analytic approach exists to test whether the observed number of suicides is greater than expected. Several different methods have been used, including the application of spatial statistics using geographic information systems, and statistical methods such as Knox, Poisson, and Scan tests (30–32). These methods can individually serve the organizations and communities experiencing potential clusters but also complicate fully understanding the overall risk for clusters.
Although understanding and evidence of what triggers suicide clusters is lacking, suicide clusters, especially mass clusters, might occur through a process of contagion (i.e., when the exposure to the suicide or suicidal behavior of one or more persons influences others to attempt suicide) (26). An exposure can be direct by having a personal connection to the person who has died by suicide, or indirect through media reporting or social media posts about a person who was not a personal connection (28). Media influence can be both a risk and protective factor depending on its duration, prominence of source, messaging, and extent of coverage (33,34).
Media reporting of suicides might be a risk factor when it unintentionally influences increases in suicides, particularly in reporting that mentions the suicide method in the headline and in the text, and includes a statement that suicide is inevitable (35). When similar suicides occur after this type of media reporting, the increase might be attributed to the “Werther effect” (also called copycat behavior) (34,36,37). Media influence can relate to point clusters as well as mass clusters. For example, extensive and prominent news coverage of suicides has been reported to play a role in the emergence of point clusters among youth (33). Several reports have documented increases in suicide rates following media reports of high-profile celebrities, who might be considered models for imitation (38–41). In addition, there might be unintended negative consequences of entertainment media portrayals of suicide that do not adhere to best practices for safe reporting (42,43).
Conversely, responsible media reporting of suicide can be a protective factor and make a positive contribution to prevention efforts by educating the public about coping strategies and treatment (“Papageno effect”) (34,44,45). Accepted best practices (https://reportingonsuicide.org) for reporting on suicide include reporting suicide as a public health problem, including resources (e.g., hotline information and treatment options), providing warning signs, using appropriate language (e.g., “died by suicide” instead of “committed suicide”), emphasizing help and hope, and including information from suicide prevention or mental health experts, and providing resources, such as the recently updated 988 number for the national Suicide & Crisis Lifeline (https://988lifeline.org).
About this Supplement
CDC has developed new expanded guidance for investigating and responding to potential suicide clusters by using updated information from the literature on suicide clusters, input from subject matter experts, and experiences of public health practitioners and others involved in a cluster identification. The second report in this supplement, CDC Guidance for Community Assessment and Investigation of Suspected Suicide Clusters–United States, 2024 (46), describes for communities the potential methods and data sources that can be monitored for suicide clusters or be further analyzed to confirm suspected suicide clusters and builds on the 1990 CDC Guidelines for Investigating Clusters of Health Events (47), which considered clusters of noninfectious diseases, injuries, birth defects, and previously unrecognized syndromes or illnesses, but frames its content and guidance to suicide clusters, which have unique characteristics and challenges. The third report, CDC Guidance for Community Response to a Suicide Cluster–United States, 2024 (48), describes guidance to assist local public health and community leaders on how to develop a community response plan for suicide clusters. This supplement updates and expands the guidance from the 1988 CDC document (6).
Methods
To gather information for the second and third reports in this supplement, in September 2021, staff members from the Division of Injury Prevention in CDC’s National Center for Injury Prevention and Control including behavioral scientists, epidemiologists, and developmental psychologists, with support from a contracted consultant team, Ross Strategic, initiated activities that included a literature review, environmental scan, media review, and input from subject matter experts in the field.
Literature Review, Environmental Scan, and Media Review
The CDC team conducted a literature review of suicide cluster research to determine the latest science on suicide cluster identification, risk and protective factors, opportunities for using social media as a tool for prevention and response, and best practices and challenges for identifying and responding to suspected clusters. The team searched the English-language published literature via PubMed, Google Scholar, ProQuest, and JSTOR. The following keywords were used to search English language journals: “suicide clusters” OR “suicide cluster” OR “suicide contagion” and “risk factors” or “identifying” or “protective factors” or “prevention” or “containment” or “demographics” or “social media” or “media.” For cluster identification and social media publications, searches went back in time as far as possible with the earliest paper included published in 1990; however, for risk and protective factors, and prevention and response, the search as restricted to publications after 2000 to focus on the most recent reports. No geographic restrictions were placed on articles included. In addition, the team included articles from the CDC’s Suicide, Suicide Attempt, or Self-Harm Clusters website (https://www.cdc.gov/suicide/resources/suicide-clusters.html) and articles provided by suicide cluster subject matter experts.
This process resulted in 245 articles. Duplicates were removed and abstracts were reviewed to exclude articles on suicide risk and protective factors that were not specific to clusters. All suicide-related social media articles were included even if they were not specifically about clusters because of the limited number of publications in this area. This process resulted in 166 articles that discussed cluster identification (included papers published during 1990–2022), risk and protective factors (2001–2022), prevention and response (2003–2022), and social media (2007–2022) (Figure). The quality of the literature was not formally assessed because of the relatively small number of publications found. Although findings from international settings would largely apply to the United States, some issues described might be unique to specific cultural environments.
In addition, the team conducted an environmental scan that included eight internal Epidemiologic Assistance (Epi-Aid) reports from 2004–2018 documenting CDC support to local health jurisdictions to investigate and respond to a suspected suicide cluster. Other local investigations might have occurred without CDC involvement, and the team was not able to identify related reports to include in the review. The team also reviewed U.S. media reports during 2017–2022 to gather additional contextual information from communities that identified and responded to a suicide cluster but did not request Epi-Aid support from CDC. Media reports were identified through a Google News search of terms such as “suicide clusters united states.” A total of 14 news articles about clusters at the city, county, or university-level were identified and reviewed. Findings from reviews and scans might not be representative of all suicide clusters because of publication bias.
Input from Subject Matter Experts
From December 2021 to May 2022, the team collected qualitative data through outreach to researchers and public health practitioners with suicide cluster subject matter expertise to gather input on lessons learned based on experiences responding to suspected suicide clusters; opportunities and challenges for using social media and the internet for suicide cluster identification, prevention, and response; and strengths and limitations of syndromic surveillance systems for identifying clusters. To do this, CDC participated in various virtual online meetings with grantees of three CDC-funded programs: Emergency Department Surveillance of Nonfatal Suicide-Related Outcomes (https://www.cdc.gov/suicide/programs/ed-snsro/index.html); Comprehensive Suicide Prevention (https://www.cdc.gov/suicide/programs/csp/index.html); and Injury Control Research Centers (https://www.cdc.gov/injury/erpo/icrc/index.html). In addition, CDC’s Center for Surveillance, Epidemiology, and Laboratory Services, which runs the National Syndromic Surveillance Program, provided information about how syndromic surveillance systems can be used for cluster detection and responses by communities. The team also attempted to connect with health departments who requested support from CDC for suicide cluster response during 2004–2018 to better understand key lessons from Epi-Aid investigations. Three health departments responded with feedback via email. In addition, the team conducted an online virtual topical focus group and individual virtual interviews with social media subject matter experts to discuss its role in suicide clustering. Social media subject matter experts were identified through suggestions from knowledgeable CDC team members and from author lists from published papers on this topic. Although all participants came from a convenience sample of subject matter experts known by the team, their input was critical to informing the guidance in this supplement. These discussions did not seek consensus from external subject matter experts on guidance or activities but were used to gather more information to inform CDC’s development of the reports in this supplement. Discussion questions used are presented (Box).
CDC used the information from the literature review, environmental scan, media review, and subject matter expert discussions to draft the reports and guidance in this supplement. Several additional external partners reviewed the drafts and provided high-level feedback, which CDC discussed and incorporated, as needed. CDC Guidance for Community Assessment and Investigation of Suspected Suicide Clusters — United States, 2024 (46), describes guidance on responding to initial concerns for a suspected suicide cluster, confirming a cluster, and conducting an epidemiologic investigation. CDC Guidance for Community Response to a Suicide Cluster — United States, 2024 (48), describes guidance on preparatory community action before cluster identification, direct response to the cluster, and action to help prevent the next cluster.
Use of this Supplement
The guidance in this supplement is intended for public health practitioners, and state and local health departments. The guidance should not be considered explicit instructions to be followed by every community, but as suggestions on best practices. This information is meant to provide community leaders with a conceptual framework for assessing and investigating suspected clusters and developing their own suicide-cluster-response plans. These plans can be tailored to the particular needs, resources, and cultural characteristics of their communities.
Acknowledgments
Jennifer Major, Jessie Doody, Lissette Halle Palestro, Ross Strategic; Dan Reidenberg, National Council for Suicide Prevention; Thomas Neiderkrotenthaler, Medical University Vienna; Madelyn Gould, Columbia University; Jo Robinson, University of Melbourne; Mark Sinyor, University of Toronto; Alex Crosby, Morehouse School of Medicine; Richard McKeon, SAMHSA; Pamela End of Horn, Indian Health Service; Jane Pearson, NIH/NIMH; Holly Wilcox, Johns Hopkins University; Caitlin Quinn, Vermont Department of Health; Derek Smolenski, Defensive Health Agency; Jelena Allen, Department of Defense; grantees from Emergency Department Surveillance of Nonfatal Suicide-Related Outcomes, Comprehensive Suicide Prevention, and Injury Control Research Centers programs
Corresponding author: Michael F. Ballesteros, PhD, Division of Injury Prevention, National Center for Injury Prevention and Control, CDC. Telephone: 770-488-1481; Email: mballesteros@cdc.gov
Conflicts of Interest
All authors have completed and submitted the International Committee of Medical Journal Editors form for disclosure of potential conflicts of interest. No potential conflicts of interest were disclosed.
References
- CDC. CDC WONDER: About multiple cause of death, 2018–2021, single race. Atlanta, GA: US Department of Health and Human Services, CDC; 2023. https://wonder.cdc.gov/mcd-icd10-expanded.html
- Stone DM, Mack KA, Qualters J. Recent changes in suicide rates, by race and ethnicity and age group—United States, 2021. MMWR Morb Mortal Wkly Rep 2023;72:160–2. https://doi.org/10.15585/mmwr.mm7206a4 PMID:36757870
- CDC. CDC WONDER: About underlying cause of death, 1999–2020. Atlanta, GA: US Department of Health and Human Services, CDC; 2023. https://wonder.cdc.gov/ucd-icd10.html
- Substance Abuse and Mental Health Services Administration. Highlights for the 2021 National Survey on Drug Use and Health. Rockville, MD: US Department of Health and Human Services, Substance Abuse and Mental Health Services, Center for Behavioral Health Statistics and Quality; 2023. https://www.samhsa.gov/data/sites/default/files/2022-12/2021NSDUHFFRHighlights092722.pdf
- CDC. Youth Risk Behavior Survey: data summary & trends report 2011–2021. Atlanta, GA: US Department of Health and Human Services, CDC; 2023. https://www.cdc.gov/healthyyouth/data/yrbs/pdf/YRBS_Data-Summary-Trends_Report2023_508.pdf
- O’Carroll PW, Mercy JA, Steward JA. CDC recommendations for a community plan for the prevention and containment of suicide clusters. MMWR Suppl 1988:37(Suppl 6):1–12. https://doi.org/10.1111/sltb.12091 PMID:24702173
- Niedzwiedz C, Haw C, Hawton K, Platt S. The definition and epidemiology of clusters of suicidal behavior: a systematic review. Suicide Life Threat Behav 2014;44:569–81. https://doi.org/10.1111/sltb.12091 PMID:24702173
- Gould MS, Wallenstein S, Kleinman M. Time-space clustering of teenage suicide. Am J Epidemiol 1990;131:71–8. https://doi.org/10.1093/oxfordjournals.aje.a115487 PMID:2293755
- Abbott CH, Zakriski AL. Grief and attitudes toward suicide in peers affected by a cluster of suicides as adolescents. Suicide Life Threat Behav 2014;44:668–81. https://doi.org/10.1111/sltb.12100 PMID:24806293
- Heffel CJ, Riggs SA, Ruiz JM, Ruggles M. The aftermath of a suicide cluster in the age of online social networking: a qualitative analysis of adolescent grief reactions. Contemp Sch Psychol 2015;19:286–99. https://doi.org/10.1007/s40688-015-0060-z
- Haw CM. A cluster of suicides at a London psychiatric unit. Suicide Life Threat Behav 1994;24:256–66. https://doi.org/10.1111/j.1943-278X.1994.tb00750.x PMID:7825198
- Taiminen T, Salmenperä T, Lehtinen K. A suicide epidemic in a psychiatric hospital. Suicide Life Threat Behav 1992;22:350–63. https://doi.org/10.1111/j.1943-278X.1992.tb00740.x PMID:1440749
- Annor FB, Zwald ML, Wilkinson A, et al. Characteristics of and precipitating circumstances surrounding suicide among persons aged 10–17 years—Utah, 2011–2015. MMWR Morb Mortal Wkly Rep 2018;67:329–32. https://doi.org/10.15585/mmwr.mm6711a4 PMID:29565844
- Fowler KA, Crosby AE, Parks SE, Ivey AZ, Silverman PR. Epidemiological investigation of a youth suicide cluster: Delaware 2012. Del Med J 2013;85:15–9. PMID:23513329
- Gould MS, Wallenstein S, Kleinman MH, O’Carroll P, Mercy J. Suicide clusters: an examination of age-specific effects. Am J Public Health 1990;80:211–2. https://doi.org/10.2105/AJPH.80.2.211 PMID:2297071
- Swedo EA, Beauregard JL, de Fijter S, et al. Associations between social media and suicidal behaviors during a youth suicide cluster in Ohio. J Adolesc Health 2021;68:308–16. https://doi.org/10.1016/j.jadohealth.2020.05.049 PMID:32646827
- Askland KD, Sonnenfeld N, Crosby A. A public health response to a cluster of suicidal behaviors: clinical psychiatry, prevention, and community health. J Psychiatr Pract 2003;9:219–27. https://doi.org/10.1097/00131746-200305000-00005 PMID:15985934
- Brent DA, Kerr MM, Goldstein C, Bozigar J, Wartella M, Allan MJ. An outbreak of suicide and suicidal behavior in a high school. J Am Acad Child Adolesc Psychiatry 1989;28:918–24. https://doi.org/10.1097/00004583-198911000-00017 PMID:2808263
- McKenzie N, Keane M. Contribution of imitative suicide to the suicide rate in prisons. Suicide Life Threat Behav 2007;37:538–42. https://doi.org/10.1521/suli.2007.37.5.538 PMID:17967120
- Cox B, Skegg K. Contagious suicide in prisons and police cells. J Epidemiol Community Health 1993;47:69–72. https://doi.org/10.1136/jech.47.1.69 PMID:8436899
- Substance Abuse and Mental Health Services Administration. Suicide Clusters within American Indian and Alaska Native Communities: a review of the literature and recommendations. Rockville, MD. US Department of Health and Human Services, Center for Mental Health Services; 2017. https://store.samhsa.gov/sites/default/files/d7/priv/sma17-5050.pdf
- Wissow LS, Walkup J, Barlow A, Reid R, Kane S. Cluster and regional influences on suicide in a Southwestern American Indian tribe. Soc Sci Med 2001;53:1115–24. https://doi.org/10.1016/S0277-9536(00)00405-6 PMID:11556603
- Wilkie C, Macdonald S, Hildahl K. Community case study: suicide cluster in a small Manitoba community. Can J Psychiatry 1998;43:823–8. https://doi.org/10.1177/070674379804300807 PMID:9806089
- Bechtold DW. Cluster suicide in American Indian adolescents. Am Indian Alsk Native Ment Health Res 1988;1:26–35. https://doi.org/10.5820/aian.0103.1988.26 PMID:3154765
- Ward JA, Fox J. A suicide epidemic on an Indian reserve. Can Psychiatr Assoc J 1977;22:423–6. https://doi.org/10.1177/070674377702200804 PMID:597804
- Lake AM, Gould MS. Suicide clusters and suicide contagion. In: Koslow SH, Ruiz P, Nemeroff CB, eds. A concise guide to understanding suicide. Cambridge, MA: Cambridge University Press; 2014:52–61.
- Wołodźko T, Kokoszka A. [Classification of persons attempting suicide. A review of cluster analysis research]. Psychiatr Pol 2014;48:823–34. PMID:25314806
- Haw C, Hawton K, Niedzwiedz C, Platt S. Suicide clusters: a review of risk factors and mechanisms. Suicide Life Threat Behav 2013;43:97–108. https://doi.org/10.1111/j.1943-278X.2012.00130.x PMID:23356785
- Gould MS, Wallenstein S, Davidson L. Suicide clusters: a critical review. Suicide Life Threat Behav 1989;19:17–29. https://doi.org/10.1111/j.1943-278X.1989.tb00363.x PMID:2652386
- Benson R, Rigby J, Brunsdon C, Cully G, Too LS, Arensman E. Quantitative methods to detect suicide and self-harm clusters: a systematic review. Int J Environ Res Public Health 2022;19:5313. https://doi.org/10.3390/ijerph19095313 PMID:35564710
- Cheung YTD, Spittal MJ, Williamson MK, Tung SJ, Pirkis J. Application of scan statistics to detect suicide clusters in Australia. PLoS One 2013;8:e54168. https://doi.org/10.1371/journal.pone.0054168 PMID:23342098
- Gibbons RD, Clark DC, Fawcett J. A statistical method for evaluating suicide clusters and implementing cluster surveillance. Am J Epidemiol 1990;132(Supp 1):183–91. https://doi.org/10.1093/oxfordjournals.aje.a115781 PMID:2356830
- Gould MS, Kleinman MH, Lake AM, Forman J, Midle JB. Newspaper coverage of suicide and initiation of suicide clusters in teenagers in the USA, 1988–96: a retrospective, population-based, case-control study. Lancet Psychiatry 2014;1:34–43. https://doi.org/10.1016/S2215-0366(14)70225-1 PMID:26360401
- Niederkrotenthaler T, Voracek M, Herberth A, et al. Role of media reports in completed and prevented suicide: Werther v. Papageno effects. Br J Psychiatry 2010;197:234–43. https://doi.org/10.1192/bjp.bp.109.074633 PMID:20807970
- Sinyor M, Schaffer A, Nishikawa Y, et al. The association between suicide deaths and putatively harmful and protective factors in media reports. CMAJ 2018;190:E900–7. https://doi.org/10.1503/cmaj.170698 PMID:30061324
- Niederkrotenthaler T, Till B, Kapusta ND, Voracek M, Dervic K, Sonneck G. Copycat effects after media reports on suicide: a population-based ecologic study. Soc Sci Med 2009;69:1085–90. https://doi.org/10.1016/j.socscimed.2009.07.041 PMID:19682782
- Phillips DP. The influence of suggestion on suicide: substantive and theoretical implications of the Werther effect. Am Sociol Rev 1974;39:340–54. https://doi.org/10.2307/2094294 PMID:11630757
- Pirkis J, Currier D, Too LS, et al. Suicides in Australia following media reports of the death of Robin Williams. Aust N Z J Psychiatry 2020;54:99–104. https://doi.org/10.1177/0004867419888297 PMID:31749369
- Sinyor M, Tran US, Garcia D, Till B, Voracek M, Niederkrotenthaler T. Suicide mortality in the United States following the suicides of Kate Spade and Anthony Bourdain. Aust N Z J Psychiatry 2021;55:613–9. https://doi.org/10.1177/0004867420976844 PMID:33300363
- Niederkrotenthaler T, Fu KW, Yip PS, et al. Changes in suicide rates following media reports on celebrity suicide: a meta-analysis. J Epidemiol Community Health 2012;66:1037–42. https://doi.org/10.1136/jech-2011-200707 PMID:22523342
- Queinec R, Benjamin C, Beitz C, Lagarde E, Encrenaz G. Suicide contagion in France: an epidemiologic study. Inj Prev 2010;16(Supp 1):A241. https://doi.org/10.1136/ip.2010.029215.858
- Bridge JA, Greenhouse JB, Ruch D, et al. Association between the release of Netflix’s 13 Reasons Why and suicide rates in the United States: an interrupted time series analysis. J Am Acad Child Adolesc Psychiatry 2020;59:236–43. https://doi.org/10.1016/j.jaac.2019.04.020 PMID:31042568
- National Action Alliance for Suicide Prevention. National recommendations for depicting suicide. Waltham, MA: National Action Alliance for Suicide Prevention; 2023. https://theactionalliance.org/messaging/entertainment-messaging/national-recommendations
- Domaradzki J. The Werther effect, the Papageno effect or no effect? A literature review. Int J Environ Res Public Health 2021;18:2396. https://doi.org/10.3390/ijerph18052396 PMID:33804527
- Colman I. Responsible reporting to prevent suicide contagion. CMAJ 2018;190:E898–9. https://doi.org/10.1503/cmaj.180900 PMID:30061323
- Trinh E, Ivey-Stephenson AZ, Ballesteros MF, Idaikkadar N, Wang J, Stone DM. CDC guidance for community assessment and investigation of suspected suicide clusters—United States, 2024. In: CDC guidance for communities assessing, investigating and responding to suicide clusters, United States, 2024. MMWR Suppl 2024;73(No. Suppl 1):8–16.
- CDC. Guidelines for investigating clusters of health events. MMWR Recomm Rep 1990;39(No. RR-11):1–23. PMID:2117247
- Ivey-Stephenson AZ, Ballesteros MF, Trinh E, Stone DM, Crosby AE. CDC guidance for community response to suicide clusters—United States, 2024. In: CDC guidance for communities assessing, investigating and responding to suicide clusters, United States, 2024. MMWR Suppl 2024;73(No. Suppl 1):17–26.
 FIGURE. Number of articles identified, screened, and included during literature review of suicide clusters*, CDC guidance, 2024
FIGURE. Number of articles identified, screened, and included during literature review of suicide clusters*, CDC guidance, 2024
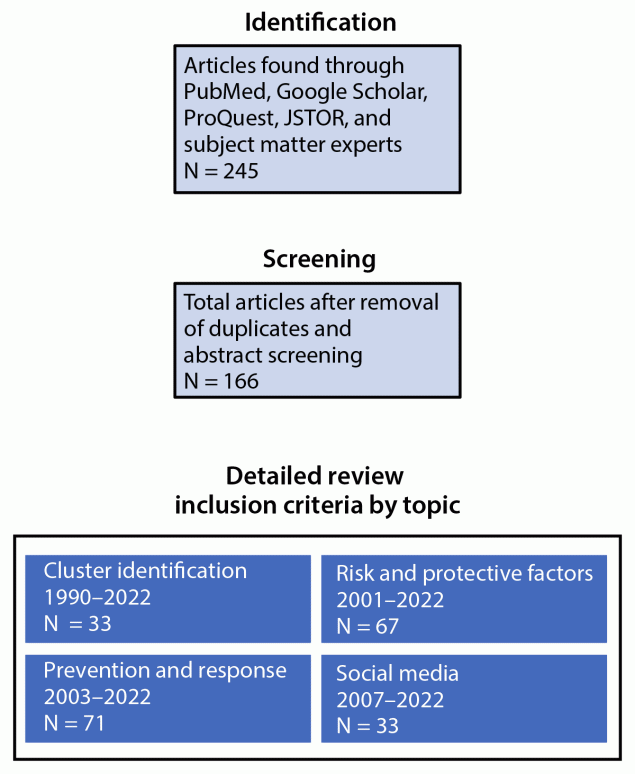
* Article counts by topic area are not mutually exclusive. There were no geographic restrictions.
 BOX. Discussion questions used for subject matter expert* outreach, CDC guidance, 2024
BOX. Discussion questions used for subject matter expert* outreach, CDC guidance, 2024
Emergency Department Surveillance of Nonfatal Suicide-Related Outcomes Grantees
|
Comprehensive Suicide Prevention Grantees
|
Injury Control Research Centers
|
Health Departments That Requested CDC Assistance for Suicide Cluster Investigations
|
Social Media Experts
|
*Fewer than 10 respondents participated within each subject matter expert group.
†Responsible media reporting of suicide being a protective factor and making a positive contribution to prevention efforts by educating the public about coping strategies and treatment.
Suggested citation for this article: Ballesteros MF, Ivey-Stephenson AZ, Trinh E, Stone DM. Background and Rationale — CDC Guidance for Communities Assessing, Investigating, and Responding to Suicide Clusters, United States, 2024. MMWR Suppl 2024;73(Suppl-2):1–7. DOI: http://dx.doi.org/10.15585/mmwr.su7302a1.
MMWR and Morbidity and Mortality Weekly Report are service marks of the U.S. Department of Health and Human Services.
Use of trade names and commercial sources is for identification only and does not imply endorsement by the U.S. Department of
Health and Human Services.
References to non-CDC sites on the Internet are
provided as a service to MMWR readers and do not constitute or imply
endorsement of these organizations or their programs by CDC or the U.S.
Department of Health and Human Services. CDC is not responsible for the content
of pages found at these sites. URL addresses listed in MMWR were current as of
the date of publication.
All HTML versions of MMWR articles are generated from final proofs through an automated process. This conversion might result in character translation or format errors in the HTML version. Users are referred to the electronic PDF version (https://www.cdc.gov/mmwr) and/or the original MMWR paper copy for printable versions of official text, figures, and tables.
Questions or messages regarding errors in formatting should be addressed to mmwrq@cdc.gov.