Notes from the Field: Vibriosis Cases Associated with Flood Waters During and After Hurricane Ian — Florida, September–October 2022
Weekly / May 5, 2023 / 72(18);497–498
Nicole Sodders, MPH1; Kimberly Stockdale, MSPH1; Kayla Baker2; Arielle Ghanem, MPH2; Benjamin Vieth, MA3; Terri Harder3 (View author affiliations)
View suggested citationAltmetric:
On the afternoon of September 28, 2022 (epidemiologic week 40), Hurricane Ian made landfall on Florida’s southwest coast as a category 4 hurricane with maximum sustained winds of 150 miles per hr (241 km per hr). The storm surge (the abnormal rise in seawater related to a storm) reached 12–18 ft (3.6–5.5 m) above ground level in some coastal areas of Lee and Collier counties, on southwest Florida’s Gulf coast (1). In the days after the hurricane, a notable increase in cases of vibriosis was observed by the Florida Department of Health: 38 cases and 11 vibriosis-associated deaths were attributed to the storm. During the hurricane response, Florida deployed public health messaging on storm preparedness statewide, advising residents of 1) the importance of not wading in flood waters or in standing water after a storm, especially persons with open wounds; 2) the potential life-threatening illness that can be caused by Vibrio vulnificus; and the importance of seeking prompt medical attention if symptoms* are experienced (2).
Vibrio bacteria thrive in warm salty or brackish waters such as those pushed ashore in a storm surge. These virulent gram-negative bacteria can result in gastrointestinal illness after consumption of raw or undercooked shellfish, or a skin infection following exposure of an open wound to salt or brackish water (a mixture of freshwater and seawater) (3). This data was obtained through routine investigation of vibriosis cases and follow- up using Florida’s reportable disease surveillance system Merlin. This activity was reviewed by CDC and was conducted consistent with applicable federal law and CDC policy.†
In the week preceding the hurricane (week 39), southwest Florida reported no vibriosis cases, which was below the 5-year median (three cases) for that week. Based on epidemiology from previous years, three vibriosis cases were expected to be reported in southwest Florida in the weeks during and after the storm (weeks 40 and 41). However, 38 culture-confirmed vibriosis cases determined to be associated with the impacts of Hurricane Ian occurred in Lee and Collier counties during September 29–October 23, representing an 1,100% increase over the 5-year median. These cases included 29 (76%) caused by V. vulnificus, three cases (8%) by Vibrio cholerae type non-O1, and two cases (5%) each by Vibrio parahaemolyticus, Vibrio fluvialis, and other Vibrio spp. One case occurred in a resident of another state who was exposed in Florida, and one patient was co-infected with V. vulnificus and V. parahaemolyticus. The median patient age was 80 years (range = 51–94 years), and 79% of the 38 cases occurred in men. Date of symptom onset ranged from September 28 to October 9; onset dates for two patients were unknown. Among 36 (95%) patients with known illness onset date, 34 (94%) cases occurred within 6 days of storm landfall (Figure).
Thirty-three (87%) patients had skin infections associated with exposure to storm surge or flood waters; two (5%) reported wounds with unclear exposures; two (5%) reported prolonged exposure to flood waters after being trapped in their homes or while evacuating; and one patient (3%) reported drinking flood waters. Thirty-six patients were hospitalized for a median of 10 days (range = 1–51 days), and eight (22%) were transferred to skilled nursing facilities or rehabilitation facilities after hospitalization. Eight patients required skin grafts, and three underwent lower extremity amputations. Among the 11 (29%) deaths that occurred, nine occurred in patients infected with V. vulnificus, and one death each occurred in patients infected with V. cholerae non-O1 and with some other Vibrio sp.
This outbreak is notable because of the large number of hurricane-attributable cases that occurred during a short period. The case fatality rate was 28.9%, which might be related to the age of many of the patients. In 2017, after Hurricane Irma, six storm-related vibriosis cases were documented in Florida, approximately one sixth the number documented after Ian, possibly because of the lower storm surge (5–6 ft [1.5–1.8 m]) during Irma. In 2005, Hurricane Katrina resulted in the highest storm surge in U.S. history (>25 ft [7.6 m]); 22 vibriosis cases were linked to that storm, all of which resulted in disease onset within 7 days of storm landfall (4). Communicating risk information to the public and to health care providers before an event with potential for significant storm surge, such as a major hurricane, might prevent cases and assist in the timely diagnosis and treatment of vibriosis. In hurricane-associated wound infections, V. vulnificus should be considered as a possible cause, aggressive wound care and prompt administration of antibiotics is essential to improving survival (5).
Corresponding author: Nicole Sodders, nicole.sodders2@flhealth.gov.
1Florida Department of Health; 2Florida Department of Health in Lee County, Fort Myers, Florida; 3Florida Department of Health in Collier County, Naples, Florida.
All authors have completed and submitted the International Committee of Medical Journal Editors form for disclosure of potential conflicts of interest. No potential conflicts of interest were disclosed.
* Signs and symptoms include fever, chills, decreased blood pressure (septic shock), and skin lesions.
† 45 C.F.R. part 46, 21 C.F.R. part 56; 42 U.S.C. Sect. 241(d); 5 U.S.C. Sect. 552a; 44 U.S.C. Sect. 3501 et seq.
References
- National Environmental Satellite Data and Information Service. Hurricane Ian’s path of destruction. Washington, DC: US Department of Commerce, National Oceanic and Atmospheric Administration; 2022. https://www.nesdis.noaa.gov/news/hurricane-ians-path-of-destruction
- Florida Health. Storm preparedness: Vibrio vulnificus. Tallahassee, FL: Florida Department of Health; 2022. https://www.floridahealth.gov/about/_documents/emergency-information-factsheet-vibrio.pdf
- CDC. Vibrio species causing vibriosis: questions and answers. Atlanta, GA: US Department of Health and Human Services, CDC; 2019. https://www.cdc.gov/vibrio/faq.html
- Engelthaler D, Lewis K, Anderson S, et al.; CDC. Vibrio illnesses after Hurricane Katrina—multiple states, August–September 2005. MMWR Morb Mortal Wkly Rep 2005;54:928–31. PMID:16177685
- CDC. Vibrio species causing vibriosis: information for health professionals and laboratorians. Atlanta, GA: US Department of Health and Human Services, CDC; 2023. https://www.cdc.gov/vibrio/healthcare.html
 FIGURE. Hurricane Ian–associated vibriosis cases* (N = 38) and deaths† (N = 11), by illness onset date and Vibrio species — Florida, September 28–October 9, 2022
FIGURE. Hurricane Ian–associated vibriosis cases* (N = 38) and deaths† (N = 11), by illness onset date and Vibrio species — Florida, September 28–October 9, 2022
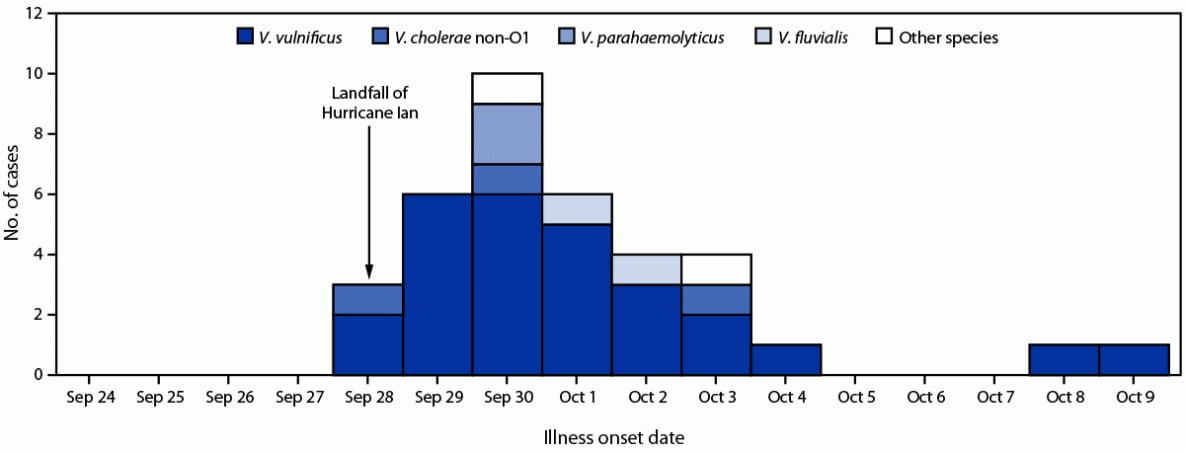
* Two cases not displayed because illness onset date was unknown.
† Nine V. vulnificus–associated deaths occurred in patients with illness onset dates of September 29 (three), September 30 (four), and October 9 (one); the onset date for one V. vulnificus–associated case was not known; one V. cholerae non-O1–associated death occurred in a patient with illness onset on September 28, and one death associated with another Vibrio sp. occurred in a patient with illness onset on September 30. One V. vulnificus–associated death was in a patient coinfected with V. parahaemolyticus.
Suggested citation for this article: Sodders N, Stockdale K, Baker K, Ghanem A, Vieth B, Harder T. Notes from the Field: Vibriosis Cases Associated with Flood Waters During and After Hurricane Ian — Florida, September–October 2022. MMWR Morb Mortal Wkly Rep 2023;72:497–498. DOI: http://dx.doi.org/10.15585/mmwr.mm7218a5.
MMWR and Morbidity and Mortality Weekly Report are service marks of the U.S. Department of Health and Human Services.
Use of trade names and commercial sources is for identification only and does not imply endorsement by the U.S. Department of
Health and Human Services.
References to non-CDC sites on the Internet are
provided as a service to MMWR readers and do not constitute or imply
endorsement of these organizations or their programs by CDC or the U.S.
Department of Health and Human Services. CDC is not responsible for the content
of pages found at these sites. URL addresses listed in MMWR were current as of
the date of publication.
All HTML versions of MMWR articles are generated from final proofs through an automated process. This conversion might result in character translation or format errors in the HTML version. Users are referred to the electronic PDF version (https://www.cdc.gov/mmwr) and/or the original MMWR paper copy for printable versions of official text, figures, and tables.
Questions or messages regarding errors in formatting should be addressed to mmwrq@cdc.gov.