
Feature Stories

LLS fellow Roxana Rodriguez Stewart, PhD (seated), trains lab staff at the Training Center for Excellence in Medical Sciences Training Laboratory in Thailand.
Fungi are everywhere, and the number of disease-causing fungi is rising worldwide. When laboratories can spot these harmful fungi, patients can quickly get the right diagnosis and treatment. Scientists at CDC’s Mycotic Diseases Branch (MDB) teach people across the United States and globe how to identify and test disease-causing fungi to improve public health.
In September 2023, LLS fellow, Roxana Rodriguez Stewart, PhD, working in CDC’s MDB, collaborated with CDC Thailand and Thailand’s Ministry of Public Health to train 26 lab staff on fungal laboratory tests. Trainees spent four days attending lectures each morning and applying those lessons in afternoon laboratory sessions. Staff learned to identify disease-causing fungi and test antifungal treatments. They worked through laboratory testing processes like those in real-life scenarios when the lab receives a specimen from a patient with an unknown cause of infection.
Roxana’s training was a success! Staff increased their knowledge of fungal lab tests by 31 percent. This training would not have been a success without all the hard work, months of planning, collaboration, and passion for public health ― all of which are needed in the continued effort for improving fungal diagnostics and treatment worldwide.
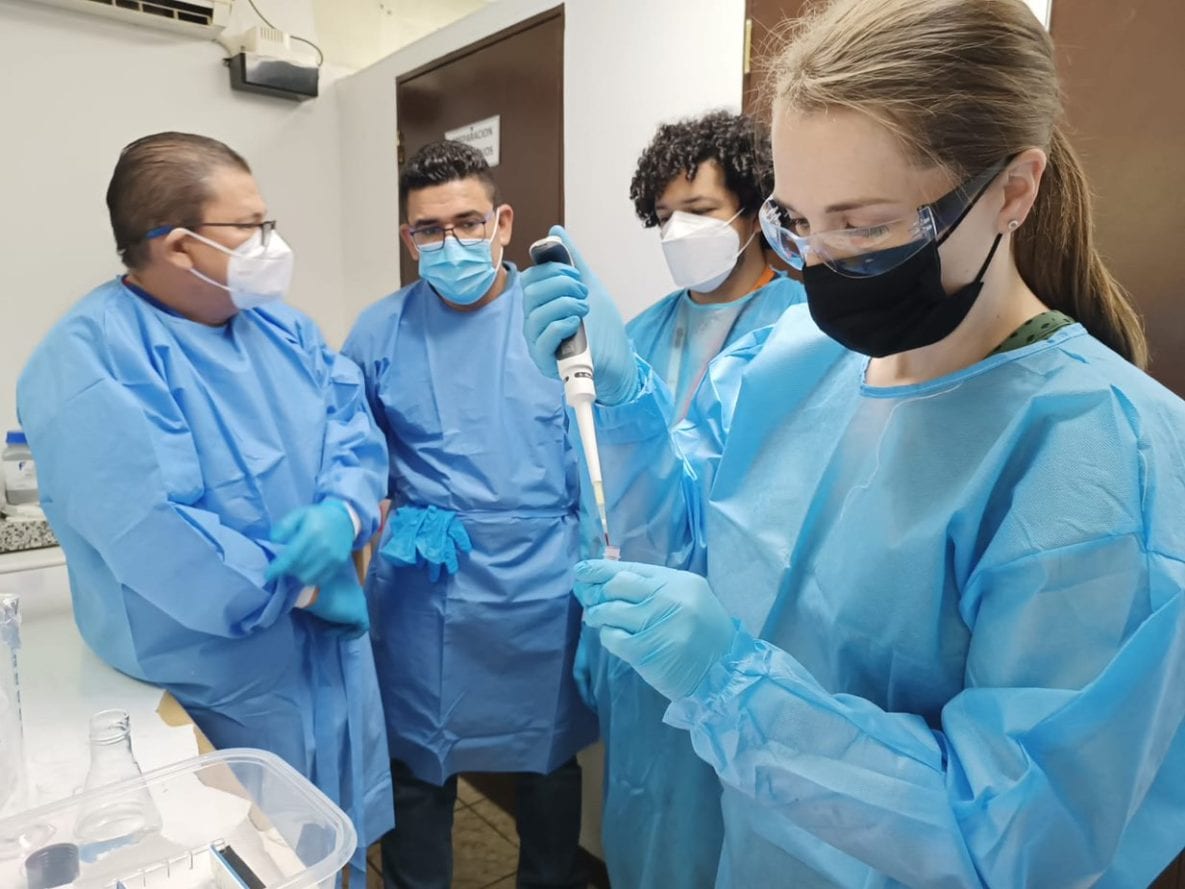
LLS fellow Megan Mickum (2022 class) trains National Public Health Laboratory scientists on a conventional PCR assay for Cholera surveillance in El Salvador. Image not from a CDC facility.
In light of multiple global outbreaks of cholera—many in regions where cases were not observed for a decade or more—laboratory preparedness for characterizing the causative agent of cholera, the bacterium Vibrio cholerae, is a high priority in Central America. El Salvador’s Ministry of Health (MOH) recognized an urgent need to strengthen in-country laboratory capacity. They were especially interested in being able to test for cholera more effectively. The MOH reached out to global partners COMISCA and CDC for assistance, and the CDC’s Enteric Diseases Laboratory Branch (EDLB) was invited to support this effort. Megan Mickum, PhD, a LLS fellow assigned to EDLB, was ready to lend a helping hand in the form of her laboratory expertise. Megan was invited to El Salvador to take part in a week of education and capacity building alongside partners from across Central America. As a lab expert from CDC, Megan gave educational lectures to audiences of 50–60 participants from El Salvador’s MOH. She educated the audience on culture and molecular methods for cholera detection, other lab testing methods, and how all these components play a pivotal role in cholera surveillance and outbreak investigations.
Besides the educational lectures in El Salvador, Megan spent four days working hands-on with six members of the Salvadorian National Public Health Laboratory (LNSP) to set up their own molecular testing laboratory. Prior to the visit, Megan worked closely with the team at SE-COMISCA to plan and prepare for this training. SE-COMISCA assisted with the necessary equipment and reagents, and the LNSP remodeled a previously unused room to serve as their new testing lab. Megan helped with making sure everything was in the right place, taught the steps of the assay, and taught everyone how to perform and interpret the tests. It was vitally important for the LNSP to learn the proper way to identify and characterize toxigenic Vibrio cholerae as the causative agent of cholera and how to optimize their protocol for their newly designed laboratory space and workflow. Megan recounted that working alongside these lab professionals was a once in a lifetime experience. “I would never have had an opportunity like this if not for being an LLS fellow. This was the most fun I’ve had in my professional career.”

LLS fellow Jessica Prince-Guerra packs leftover samples on dry ice for shipping to CDC laboratories. CDC evaluated the samples, which were positive by either the antigen or real-time RT-PCR test, for the presence of live virus.
LLS fellow Jessica Prince-Guerra (2020 class) deployed to Arizona and Georgia to provide laboratory expertise for CDC’s COVID-19 emergency response. She helped evaluate the widely distributed antigen test that received Emergency Use Authorization (EUA) from the Food and Drug Administration for use in people with symptoms. Jessica compared this test to real-time RT-PCR testing, the “gold standard” for detecting the virus. A CDC Morbidity and Mortality Weekly Report describes results from Arizona, where she led a team to test 3,400 residents in two weeks. In Georgia, her team tested more than 2,000 students and staff at a college over four-days. Read about Jessica and her team’s findings in this Virology Journal publication. Learn more about Jessica and her disease detective experience in this CDC responder story.

During CDC’s COVID-19 response, laboratory scientist Jesica Jacobs has helped with testing programs in four states and the Pacific Island of Saipan. Here she is on the Rosebud Sioux Reservation in South Dakota.
LLS fellow Jesica Jacobs (2019 class) led the charge by the Massachusetts Governor for the State Public Health Laboratory to determine how well the Abbott BinaxNOW rapid antigen COVID-19 tests could detect SARS-CoV-2 in people with and without symptoms. Jesica worked with the lab director to organize and execute the study, analyze the data, and publish the findings. Learn more about Jesica and her experiences as a disease detective in this CDC responder story.
LLS fellow David Lowe (2017 class) developed a new light-producing rabies animal model to help test new vaccines and therapeutics, which he presented at the 2019 Epidemic Intelligence Service (EIS) conference. CDC scientists work to develop and test new medical countermeasures (MCMs) that can be used to protect the public from diseases in an outbreak, natural disaster, or bioterrorism event. MCMs can include things like vaccines, medications, and diagnostic tests. Research on MCMs can include using animal models to test their effectiveness. Some pathogens, like Rabies lyssavirus (RABV), cause few signs of infection before death, which makes it hard to know if test animals survive because of effective MCM treatment, or because they were never infected.
David and his colleagues tested two RABV strains that had genes added to produce light when the viruses spread in infected animals. They found that these light-producing, or luminescent, rabies strains showed clear evidence of infection in mice, measured in “radiance” using a special laboratory imager. This meant they could detect rabies infection in living animals before clinical signs of rabies were detected. Luminescent rabies strains give clear and early signs of rabies virus in test animals. These new models could reduce the number of animals needed for testing, limit harm to test animals, and lower project times to develop and improve MCMs for rabies.
Medical countermeasures, or MCMs, are crucial to public health readiness in an emergency. Improving our animal models will allow future MCM research to be more targeted and efficient and can reduce the use of laboratory animals in developing and testing MCMs.
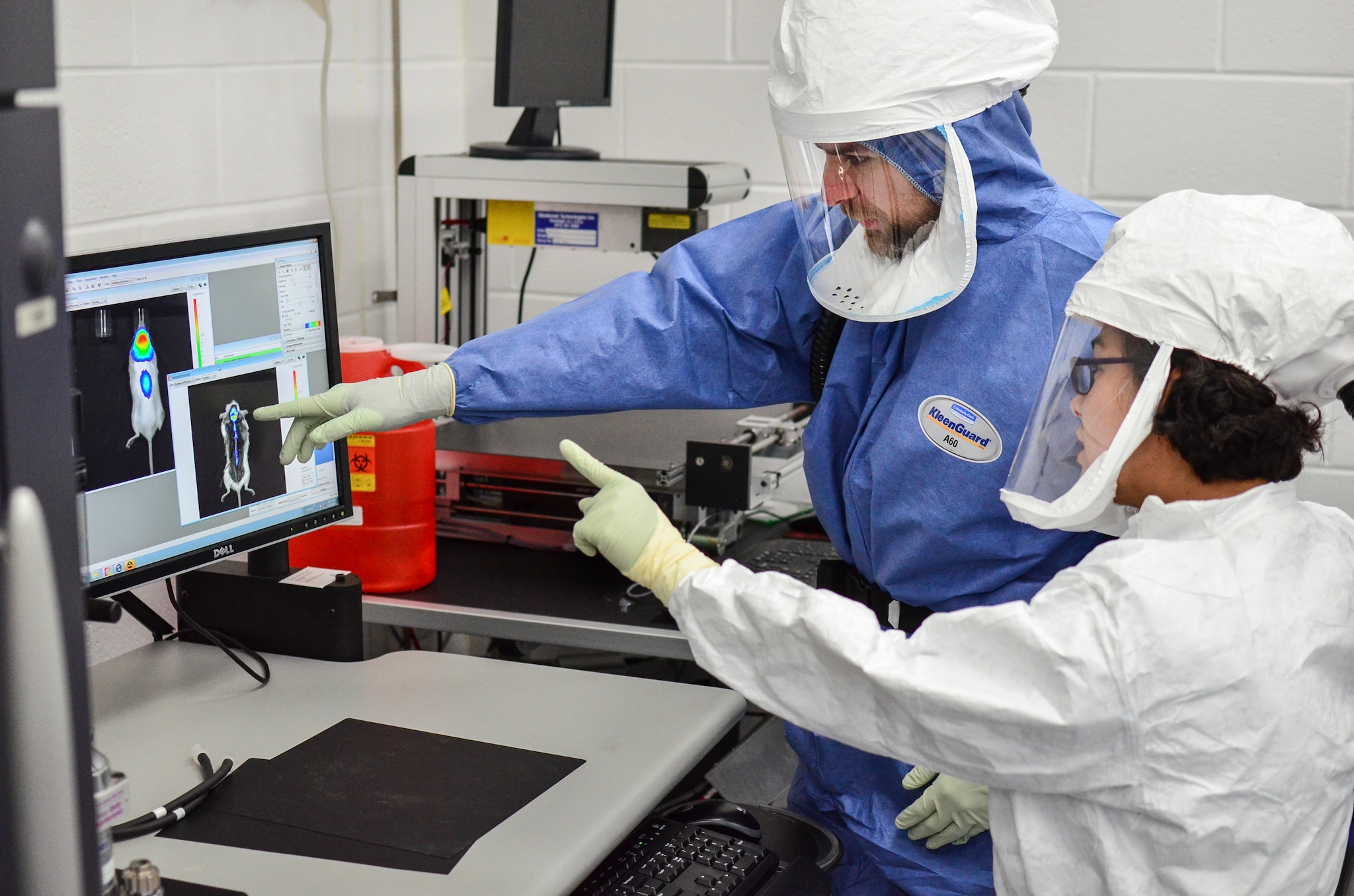
LLS Fellow David Lowe, PhD, and CDC’s Poxvirus and Rabies Animal Studies Unit lead Nadia Gallardo, DVM, discuss data from their new luminescent rabies model

LLS Fellow David Lowe, PhD, developed a new light-producing rabies animal model to help test new vaccines and therapeutics
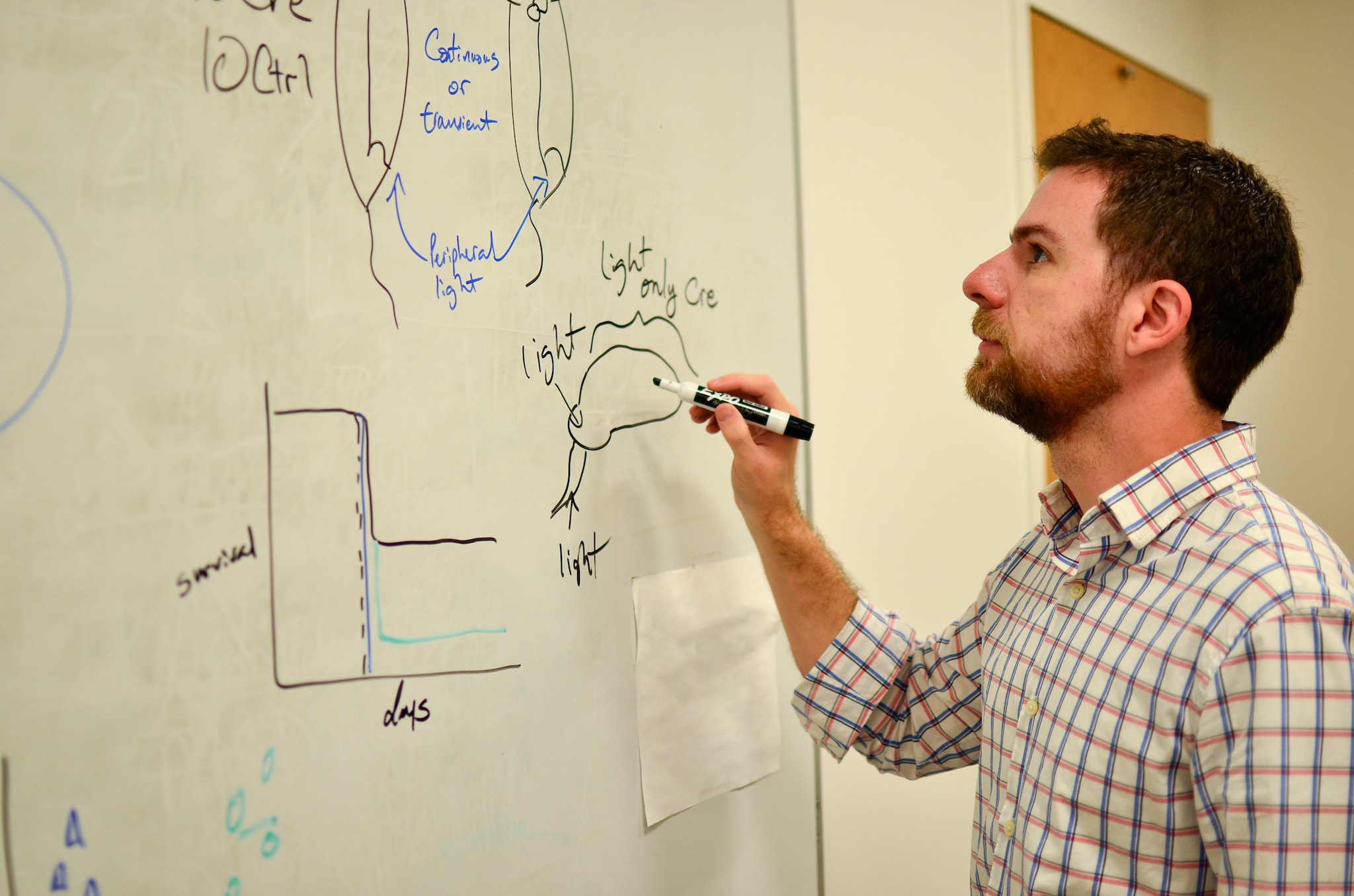
LLS fellow David Lowe, PhD, analyzes data from his new luminescent animal model that can lead to new treatments for rabies
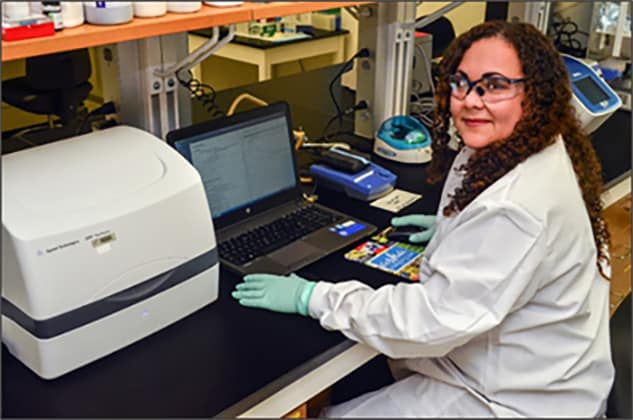
2016 Laboratory Leadership Service (LLS) fellow Brunie Burgos White, PhD, verifies the quality of RNA samples before building libraries for next generation sequencing in her fellowship assignment with CDC’s Division of STD Prevention Laboratory Branch.
LLS fellow Brunilis (Brunie) White (2016 class) worked with the Puerto Rico Department of Health to help re-establish lab operations after Hurricane Maria, which she presented during the 2018 Epidemic Intelligence Service (EIS) conference. Public services in Puerto Rico were severely affected by Hurricane Maria, including the operation of the Puerto Rico Department of Health (PRDOH) which provides critical laboratory testing and surveillance for diseases and other health hazards.
The PRDOH identified repair of the public health laboratories as a major priority during the post-hurricane response and requested assistance from CDC with clinical testing as well as with structural and safety assessments to help guide the restoration process. Brunie was among the CDC experts who worked closely with PRDOH and other federal, state, and non-governmental partners in providing technical support and aid in reestablishing laboratory operations during the emergency response.
Health departments may find it helpful to incorporate the practices used in Puerto Rico to help re-establish diagnostic testing and disease surveillance quickly after a natural disaster,” expressed Brunie.