Reduce Risk from Surfaces
Surfaces- A Key Component of Environmental Cleaning
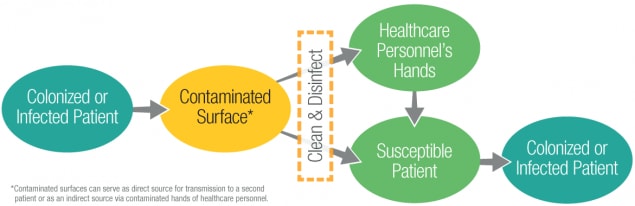
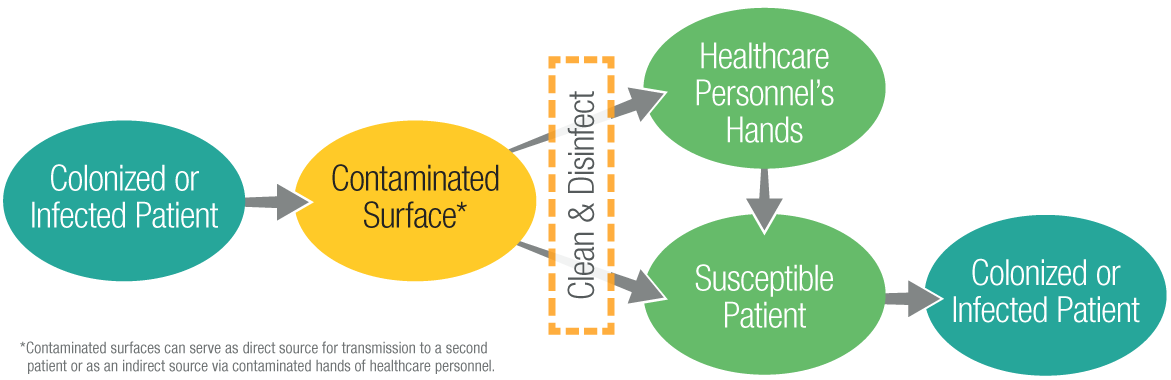
The healthcare environment contains a diverse population of microorganisms. Surfaces contaminated with microorganisms can serve as reservoirs of potential pathogens. Many of these microorganisms are continuously shed or spread by direct skin contact onto surrounding environment surfaces. Contamination of surfaces, including high-touch surfaces in the room (e.g., bedrails, over-bed tables, and call-buttons) and reusable patient care equipment that is moved between rooms, can lead to: (1) transmission to the next patient who occupies the room or uses the same equipment, or (2) contamination of the hands or clothing of healthcare personnel with transmission to other patients (Figure 1). Therefore, cleaning and disinfection of environmental surfaces is fundamental to reduce potential contribution to healthcare-associated infections. Inadvertent exposures to environmental opportunistic pathogens may result in infections with significant morbidity and/or mortality. The following are core components every healthcare facility should consider to ensure appropriate environmental cleaning and disinfection.
Figure 1: Transmission of Microorganisms through Contaminated Surfaces
Core Components of Environmental Cleaning and Disinfection in Hospitals
Introduction
To keep patients safe, hospitals must maintain a clean environment and minimize the presence of pathogens. No single “blueprint” exists for the best cleaning and disinfection method, but there are several foundational elements, or Core Components, that help establish and sustain a clean, safe environment that supports the safety of patients, healthcare personnel (HCP), and visitors.
Scope
The Core Components described in this document are intended for acute care hospitals. They can be applied to all healthcare facilities, including long-term care facilities and outpatient settings. However, special considerations may be needed to extend these components to these other healthcare settings.
The intended audience for this document includes:
- hospital executive leadership
- environmental services (EVS) managers and supervisors
- infection prevention and control (IPC) personnel
- quality leaders
- facilities engineering
- EVS personnel and HCP who are responsible for cleaning and disinfecting patient care areas (per facility protocol)
Core Components of Environmental Cleaning and Disinfection
- Integrate environmental services into the hospital’s safety culture.
- Educate and train all HCP responsible for cleaning and disinfecting patient care areas.
- Select appropriate cleaning and disinfection technologies and products.
- Standardize setting-specific cleaning and disinfection protocols.
- Monitor effectiveness and adherence to cleaning and disinfection protocols.
- Provide feedback on adequacy and effectiveness of cleaning and disinfection to staff and stakeholders.
This document addresses cleaning and disinfection of noncritical surfaces in hospitals. It does not address cleaning and disinfection of semi-critical or critical surfaces, devices, and equipment.
Descriptions and Examples of Activities in the Core Components
1. Integrate Environmental Services into the Hospital’s Safety Culture
Achieving and maintaining a clean patient care environment is a critical component of a hospital’s safety culture. In any hospital, EVS plays a pivotal role in IPC and in patient and HCP safety the patient care environment.
- Establish a hospital cleaning and disinfection program with a defined management structure and multidisciplinary participation and oversight.
- Include, at a minimum, representation from hospital leadership, quality, nursing, purchasing, facility management, IPC, and EVS.
- Hold regular meetings to review practices and quality measures and establish/review facility goals.
- Define program responsibilities, including but not limited to:
For more information on evaluating environmental cleaning, visit the CDC’s Options for Evaluating Environmental Cleaning.
- Implementing the Core Components described in this document.
- Evaluating effectiveness of the program using data from clinical surveillance, the environmental monitoring program, and the environmental cleaning and disinfection monitoring strategy (see Section 5 below).
- Establish and maintain a clear reporting and accountability structure for EVS personnel.
- Develop a performance evaluation and career advancement structure for EVS personnel and management that:
- Encourages excellence
- Rewards expertise and skills
- Optimizes retention
- Incorporate considerations for effective cleaning and disinfection into the design, structure, and layout of patient care areas.
2. Educate and Train All HCP Responsible for Cleaning and Disinfecting Patient Care Areas
All personnel who clean and disinfect patient care areas must understand their roles and responsibilities. This is critical for the ongoing success of the cleaning and disinfection program and for protecting the health of HCP, patients, and visitors. Because many HCP are responsible for cleaning and disinfecting reusable patient care equipment and environmental surfaces in patient care areas, appropriate education and training is required for a broad range of HCP.
- Focus education and training for HCP responsible for cleaning and disinfection on:
- Learning hospital cleaning and disinfection policies and following them (i.e., correct practices are observed by a trainer)
- Understanding the basic concepts of pathogen transmission
- Recognizing the impact of their work on infection control and patient safety
- Protecting themselves while working:
- Proper use of personal protective equipment (PPE)
- Safe use of chemicals [PDF – 1 Page] and cleaning technologies
- Infection control risks, including sharps safety
- Other aspects of worker safety as appropriate to the setting or situation
- Train all EVS personnel upon hire and at least annually, and when introducing new equipment or protocols.
- Keep records of training completion.
- If contracted services provide the training, make sure that it meets facility requirements.
- Re-train to address weaknesses discovered during routine monitoring activities or audits (see Section 5 below).
- Hold competency-based trainings that account for:
- staff turnover
- education levels
- language and cultural barriers
- multiple learning styles
- Keep a record of competency for all personnel responsible for disinfecting patient care areas and reusable equipment.
- Update EVS management and personnel on trends in facility infection rates and prevention priorities.
3. Select Appropriate Cleaning and Disinfection Technologies and Products
- Make sure that cleaning and disinfection technologies and products are tailored to the setting and standardized as much as possible.
- Use a systematic process to select technologies and products, including advanced technologies (e.g., no-touch disinfection devices), for patient care areas.
- Convene all stakeholders, including the facility cleaning and disinfection program, EVS management, IPC, Materials Management, and other relevant HCP in the decision-making process for factors such as:
- compatibility with device manufacturer’s instructions for use
- contact time
- possible health risks
- acceptability to HCP and patients
- effectiveness in decontaminating a surface
- impact on overall cleaning efficiency
- required expertise and training
- effect on surfaces or devices of repeated exposure to a product
4. Standardize Setting-Specific Cleaning and Disinfection Protocols
Identify standardized, setting-specific protocols for cleaning and disinfection, including use of technologies and products (See Section 3 above).
- Emphasize that surfaces, including high-touch surfaces, must be cleaned effectively, accounting for differences in room layout, equipment, and patient risk.
- Clearly define responsibilities for the cleaning and disinfection of noncritical equipment, shared medical equipment, and other electronics (e.g., ICU monitors, ventilator surfaces, bar code scanners, point-of-care devices, mobile workstations, code carts, airway boxes).
- Make sure that staff involved in cleaning and disinfection are aware of their responsibilities and are appropriately trained to fulfill them.
- Make sure that cleaning and disinfection supplies are easily accessible (e.g., cleaning cart and patient care areas are adequately stocked).
- Develop standardized protocols for routine (e.g., daily) and discharge/transfer (also known as terminal) cleaning and disinfection for each major patient care room type (i.e., intensive care unit or ward) or area type (i.e., operating room, emergency department, radiology suite).
- Make sure that the protocols are readily available (e.g., posted online or available in hard copy ) for review by staff.
- Include in the protocols:
- Appropriate PPE for EVS personnel
- Processes for routine and discharge/transfer cleaning and disinfection for specific pathogens (e.g., difficile, Candida auris, norovirus, MDROs) and other patient-level factors (e.g., wounds, diarrhea)
- Facility-specific cleaning and disinfection technologies, products, and methods
- Processes for easy identification of equipment and rooms that have been properly cleaned and disinfected and are ready for patient use (e.g., tagging system, placement in dedicated clean area)
- Develop policies and procedures for storage of patient and visitor personal items, which can make it difficult to properly clean a room.
- Make sure that the EVS team can identify which patient rooms are under transmission-based precautions, variations in cleaning and disinfection protocols that may be required, and necessary PPE.
- Establish the minimal cleaning time (MCT) for routine and discharge/transfer cleaning for each major patient care room type or area.
- Define a process to establish MCTs, for example by observing standardized cleaning protocols performed by experienced personnel.
- Align MCTs with staffing plans to ensure that effective cleaning and disinfection can be completed and sustained.
- Disseminate MCTs so that others who are responsible for patient flow, such as bed control and nursing, are aware of them for each patient care area.
- Enforce MCTs and empower EVS staff to require adherence to MCTs.
- Track cleaning times to:
- Identify factors that influence them
- Assess the need for mitigating those factors or revising the MCT
5. Monitor Effectiveness and Adherence to Cleaning and Disinfection Protocols
An environmental cleaning and disinfection monitoring strategy allows EVS personnel, other relevant HCP, and the facility cleaning and disinfection program to understand the current state of facility cleanliness and to identify areas for improvement.
- Develop and implement a monitoring strategy for adherence to, and effectiveness of, cleaning and disinfection procedures.
- Include in the protocols for monitoring:
- Who should do the monitoring
- What type of monitoring will be used (e.g., direct observation, fluorescent gel, adenoside triphosphate (ATP)
- How frequently the monitoring will occur
- How monitoring data will be validated
- Which rooms will be monitored
- Which surfaces will be assessed
- Incorporate methods for monitoring cleaning adherence and effectiveness in addition to direct observation (e.g., fluorescent markers, ATP assays).
- Perform routine audits of adherence to cleaning and disinfection procedures.
6. Provide feedback on adequacy and effectiveness of cleaning and disinfection to all responsible HCP as well as relevant stakeholders (e.g., infection control, hospital leadership)
- Use monitoring data to improve facility cleaning and disinfection policies and procedures and patient safety.
- Present audit data to EVS personnel regarding their adherence to cleaning and disinfection procedures. Determine the best method to disseminate the information and foster shared accountability (i.e., all staff, including EVS personnel, management, facility leadership, and clinical personnel take responsibility for consistent and successful adherence to protocols).
- Present audit data to leadership to:
- Identify active issues and strategies to mitigate these issues.
- Validate the effectiveness of the overall cleaning strategy.
Definitions
EVS personnel are responsible for cleaning and disinfection of reusable patient care equipment and environmental surfaces in patient care areas. They can be directly employed by the healthcare facility, a contractor, or another management structure. Additional HCP are also often responsible for cleaning and disinfection in patient care areas.
The safety culture of an organization is the individual and group values, attitudes, perceptions, competencies, and patterns of behavior that determine the commitment to health and safety management.
Noncritical environmental surfaces come into contact with intact skin, but not mucous membranes. They include:
- environmental surfaces (e.g., bed rails, bedside tables, countertops, patient furniture, and floors)
- patient care items and equipment (e.g., bedpans, blood pressure cuffs, IV poles, crutches, and computers)
Reusable patient care equipment are devices that HCP can reuse to diagnose and treat multiple patients (e.g., surgical forceps, endoscopes and stethoscopes).
Routine cleaning is the regular cleaning (and disinfection, when indicated) when the room is occupied to remove organic material, reduce microbial contamination, and provide a visually clean environment. Emphasis is on surfaces within the patient zone.
Critical patient care equipment are equipment and devices that enter sterile tissue or the vascular system, such as surgical instruments, cardiac and urinary catheters. They are not in the scope of this document.
Semi-critical patient care equipment are equipment, such as endoscopes, respiratory and anesthesia equipment, and vaginal ultrasound probes, that comes into contact with mucus membranes.. They are not in the scope of this document.
Terminal (discharge/transfer) cleaning is cleaning and disinfection that is performed after the patient is discharged or transferred. Includes the removal of organic material and significant reduction and elimination of microbial contamination.
Acronyms and Abbreviations
| Acronyms and Abbreviations | Expansion |
|---|---|
| EVS | Environmental Services |
| HCP | Healthcare Personnel |
| IPC | Infection Prevention and Control |
| MCT | Minimum Cleaning Time |
| MDRO | Multidrug-Resistant Organism |
| PPE | Personal Protective Equipment |
Guidelines and Toolkits
- Disinfection & Sterilization Guideline. 2008
- Environmental Infection Control Guideline, 2003
- How to Read A Label Infographic [PDF – 1 Page]
- More information on different monitoring strategies can be found here.
Supplemental documents, resources, and tools
- AHA. Using the Health Care Physical Environment to Prevent and Control Infection. ASHE Catalog #055196. A Best Practice Guide to Help Health Care Organizations Create Safe, Healing Environments. 2018.
- Association for the Healthcare Environment (AHE). Practice guidance for Healthcare environmental cleaning. 3rd Chicago, IL: AHA. 2019.
- AHE. Certified Health Care Environmental Services Technician Train-the-Trainer Program.
- AHE. Staffing Methodologies and Standards for Health Care.
- APIC. Environmental Services.
- CDC. Options for Evaluating Environmental Cleaning.
- Donskey CJ. Decontamination devices in healthcare facilities: practical issues and emerging applications. Am J Infect Control. 2019;47:A23-A28.
- Rutala WA, Weber DJ. Best practices for disinfection of noncritical environmental surfaces and equipment in health care facilities: a bundled approach. Am J Infect. 2019; 47:A96-105.
- Donskey CJ. Beyond high-touch surfaces: portable equipment and floors as potential sources of transmission of health care-associated pathogens. Am J Infect. 2019; 47:A90-95.
- Carling P, Herwaldt LA. The Iowa Disinfection Cleaning Project: Opportunities, Successes, and Challenges of a Structured Intervention Program in 56 Hospitals. Infect Control Hosp Epidemiol. 2017 Aug;38(8):960-965.
- Rock C, et al. Evaluating accuracy of sampling strategies for fluorescent gel monitoring of patient room cleaning. Infect Control Hosp Epidemiol. 2019 Jul;40(7):794-797.
- Rock C, et al. Using a human factors engineering approach to improve patient room cleaning and disinfection. Infect Control Hosp Epidemiol. 2016 Dec;37(12):1502-1506.