West Africa Comes Together to Confront Monkeypox
April 30, 2019

Clint Morgan and Jeffrey Doty of CDC guide the One Health team in laboratory techniques at Afi Mountain.
Photo: Muhammed Saleh
On September 22, 2017, the Nigeria Center for Disease Control (NCDC) sprang into action when a suspected case of monkeypox was reported in the southern part of Nigeria, almost 40 years after the rare virus was last detected in the country.
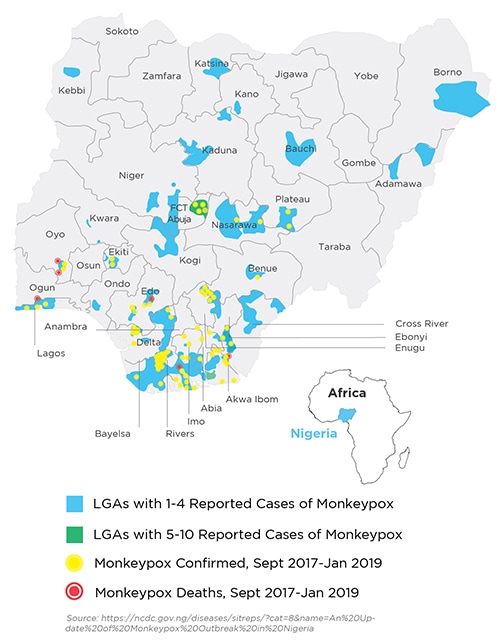
The outbreak spread rapidly. Within two weeks, 33 suspected cases were identified. As cases were confirmed in the early stages of the outbreak and evidence of possible human-to-human transmission emerged, the fear that the outbreak could spread rapidly throughout the country and across borders grew. Given the scope of the outbreak, the response required a collaborative approach with regional partners and international organizations to accurately detect, track, and stop the virus.

When NCDC noticed the sudden appearance of monkeypox symptoms in one community, it immediately activated its multiagency and multi-partner emergency operations center (EOC) for coordination of the outbreak response. The response took a One Health approach, recognizing that human health is closely connected to the health of animals and the environment. Experts from Nigeria’s health, agriculture, and environmental sectors, in collaboration with international partners including the U.S. Centers for Disease Control and Prevention (CDC), the World Health Organization, Africa Centres for Disease Control and Prevention (Africa CDC), and the African Field Epidemiology Training Network, set to work to identify and address diagnostic and surveillance gaps for both human and animal infections. CDC contributed its expertise to the response by training 10 healthcare professionals on the EOC team using the One Health approach. This training helped the EOC team analyze the latest disease surveillance data, improve Nigeria’ laboratory capacity to diagnose new cases, and develop national guidelines for NCDC. In neighboring Cameroon, Equatorial Guinea, Togo, and Central African Republic, border health authorities were also on alert and ready to investigate if people presented with fever, headache, muscle aches, swollen lymph nodes, exhaustion, and rash—the usual signs and symptoms of monkeypox.
IMPROVING LAB CAPACITY
“Regional and global collaboration were essential to contain this monkeypox outbreak,” explained Muhammad Saleh, a senior public health specialist for emergency management at CDC’s office in Nigeria. “Within a few days of the EOC’s activation, Africa CDC deployed an expert to provide technical assistance in the coordination of the EOC’s daily operations and how to follow the International Health Regulations (2005), which aim to strengthen reporting and communication among neighboring nations in potential cross-border outbreaks.”
At the time of the outbreak, Nigeria did not have the laboratory capacity to test for monkeypox. As a result, NCDC had to dispatch initial specimens to laboratories in neighboring Senegal and to CDC in Atlanta for quick and accurate diagnosis. To strengthen Nigeria’s local capacity to confirm suspected animal and human monkeypox cases, CDC trained seven frontline laboratory staff to test samples in-country using polymerase chain reaction (PCR) testing. CDC deployed poxvirus experts to work closely with staff at NCDC, providing technical assistance in outbreak coordination, surveillance, and laboratory diagnosis. CDC also provided reagents, equipment, and other essential laboratory supplies needed to identify specimens accurately.
Collaboration with CDC, Africa CDC, and other partners helped improve NCDC’s laboratory surveillance and testing methods to quickly and accurately test for monkeypox and other diseases like Lassa fever. CDC poxvirus ecologists trained local staff in how to trap small animals that may carry monkeypox virus. Almost 120 animal samples are banked for PCR and genetic testing at the National Veterinary Research Laboratory, a local collaborating institution for outbreak response in Nigeria. These samples, when tested and analyzed, may provide information about the source of the outbreak and any additional monkeypox disease reservoirs, critical details needed to improve the country’s ability to detect and prevent future outbreaks.
Regional and international collaborations strengthened NCDC’s outbreak response capabilities, building the foundation for faster in-country disease diagnosis and a One Health approach that can be applied to future outbreaks. The outbreak included more than 300 cases (132 of them confirmed) and seven deaths by the end of January 2019. However, the coordinated response stopped the monkeypox outbreak before it spread more widely, demonstrating that collaboration and a regional approach to global health security can save lives.