At a glance
- Bites from mosquitoes and ticks can make you sick!
- They can spread germs that cause diseases like West Nile and Lyme disease.
- You can Fight the Bite and learn how to protect yourself and your loved ones from mosquitoes and ticks.

About the campaign
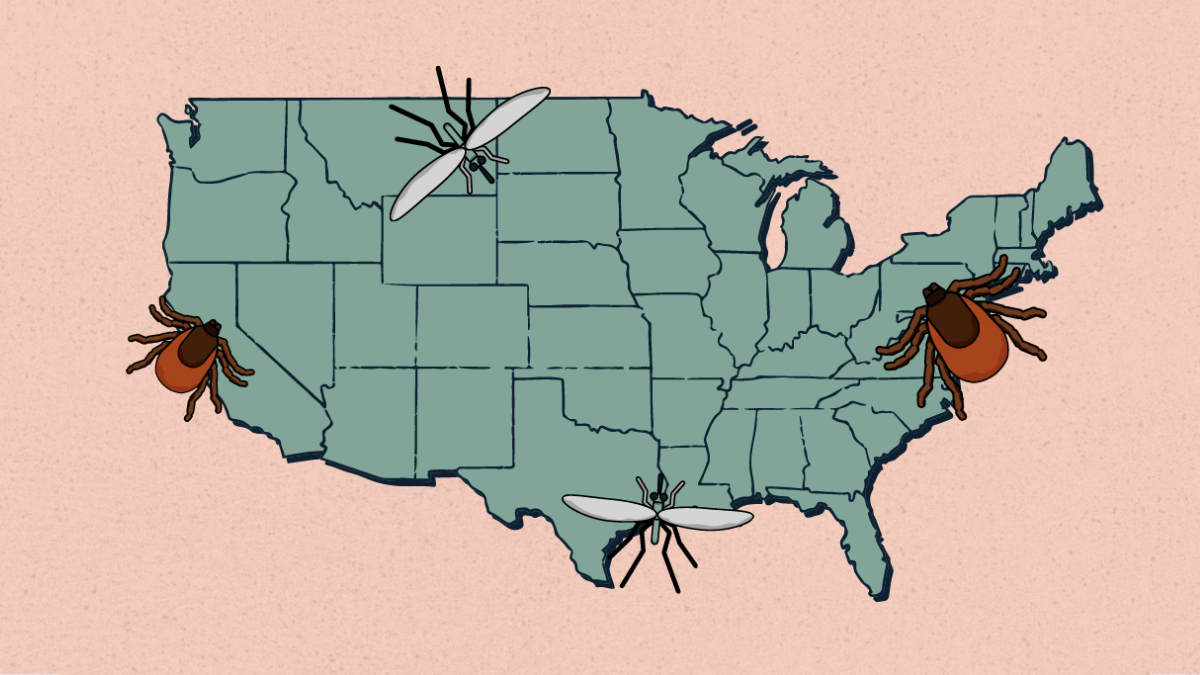
Vector-borne diseases (VBDs) are on the rise. Vectors, like mosquitoes and ticks, can spread germs through bites. Ranges of ticks are expanding, putting more people at risk for tick bites. Sporadic mosquito-borne disease outbreaks are an ongoing public health concern.
The Fight the Bite campaign was developed following a series of focus groups conducted with different at-risk audiences. Focus groups increased our understanding about which personal protective behaviors are being performed, how likely they will be performed, and how to best communicate prevention.
Learn about the development of this campaign and the resources provided below in our report, Results from Focus Groups with At-Risk Audiences.
Prevention tips and guidance
How to Prevent Mosquito and Tick Bites
Risk Factors for Vector-Borne Diseases
Risk and People Who Are Immunocompromised
Clinical Guidance for Immunocompromised Patients
Campaign resources
Help educate your community about their risk for vector-borne diseases and encourage people to prevent tick and mosquito bites.
Reach specific audiences by downloading tailored graphics for use on your own social media platforms. All graphics are in the public domain.
Logo graphics


Graphics showing key audiences

Personal protective behavior graphics for mosquitoes and ticks


Mosquito-related graphics
Tick-related graphics