Rapid Evaluations of Telehealth Strategies to Address Hypertension
Telehealth is a promising strategy for providing care to patients with high blood pressure but raises a new set of barriers for health care access.
Telehealth and telemedicine existed long before the COVID-19 pandemic, but health systems’ use of telehealth changed significantly starting in March 2020.1
Growing interest in, accessibility of, and utilization of telehealth services within the United States, coupled with the high prevalence of cardiovascular disease (CVD) risk factors,2,3 indicated a need to rapidly generate practice-based evidence for telehealth interventions that focus on high blood pressure.
We conducted rapid evaluations of two Federally Qualified Health Centers (FQHCs) that demonstrated key organizational drivers for implementing telehealth.
Although telehealth is not a one-size fits all solution, both FQHCs that participated in the rapid evaluations expressed an interest in maintaining these services in the long term and noted that their patients want the same (Figure 1).
Evaluation Purpose and Methods

Figure 1: Key findings and early lessons learned for the use of telehealth to address health care needs for patients with high blood pressure. These include: Staff, training, and leadership support are key drivers for telehealth implementation; Telehealth addresses patients’ needs and also poses new barriers to care; Telehealth is not a one-size-fits-all solution; Health systems and their patients want access to telehealth services long term.
In fall 2020, CDC’s Division for Heart Disease and Stroke Prevention (DHDSP) identified health systems that were using telehealth to address the needs of patients with a diagnosis of high blood pressure.
After receiving nominations from health systems around the country, DHDSP selected ARcare Augusta and Terros Health—two Federally Qualified Health Centers (FQHCs)—to participate in rapid evaluations.
The rapid evaluations documented early telehealth implementation, outcomes, and impact on access to care, using a mixed-methods approach. Data sources included documents, interviews, and electronic health record (EHR) data.
Evaluation Findings: ARcare Augusta
Overview
ARcare is a Federally Qualified Health Center (FQHC) headquartered in Augusta, Arkansas, and provides primary care, chronic disease management, behavioral health, and pediatric services at 48 clinics. Within its network, 17 clinics serve rural medically underserved counties in Arkansas, Kentucky, and Mississippi.
Telehealth Implementation
ARcare began providing telehealth in 2018, using technology to connect clinicians with patients in satellite clinical or community sites. In March 2020, at the start of the COVID-19 pandemic, ARcare rapidly increased the scale of its telehealth services to accommodate patients’ needs and to address access to care.
From March 2019 – February 2020, there were a total of 9,904 encounters among patients with high blood pressure or high cholesterol, the of which 5% (n=489) occurred via telehealth.
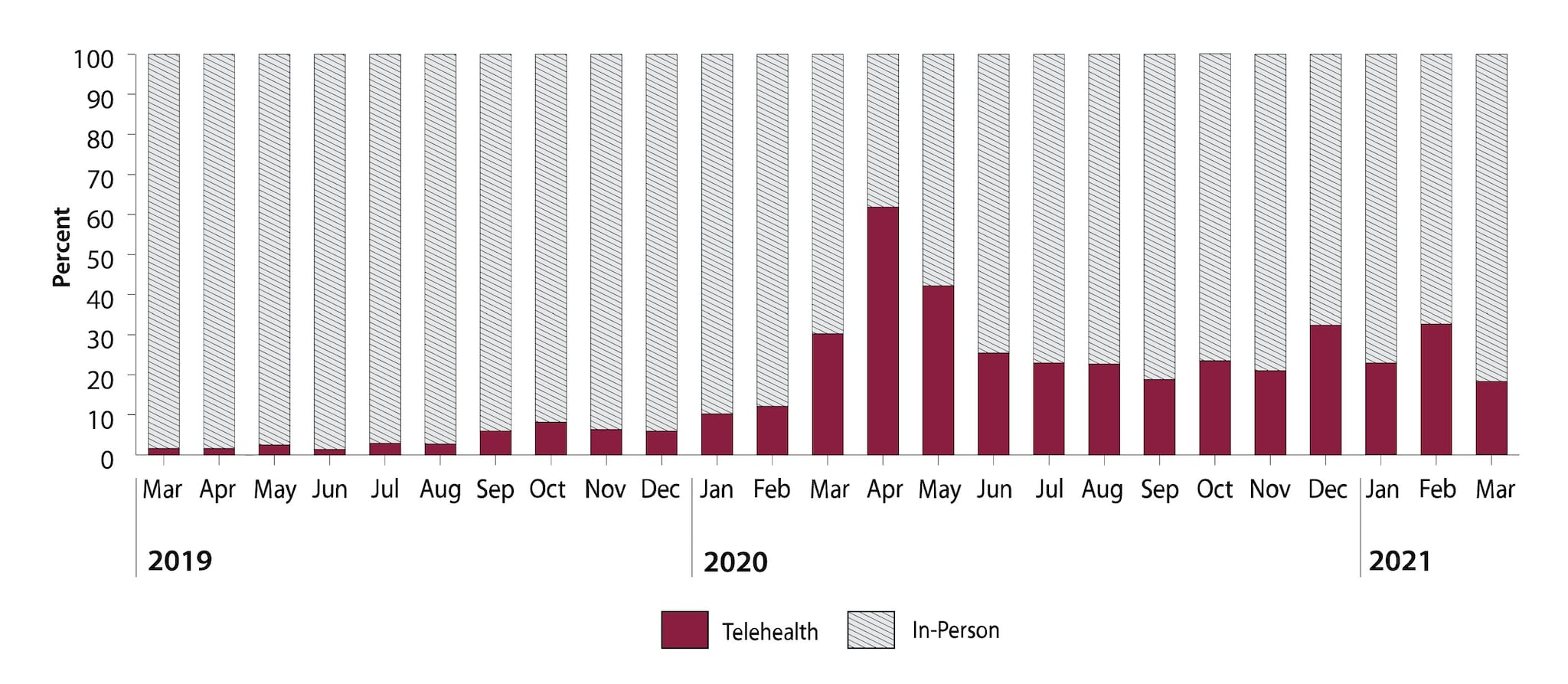
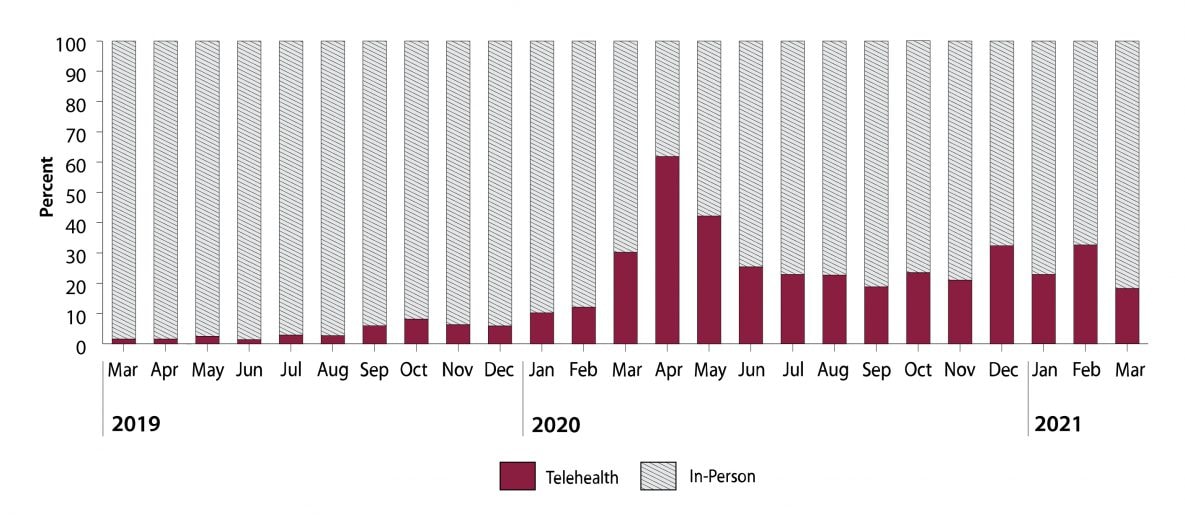
Following telehealth expansion, from March 2020 to March 2021, there were a total of 9,086 encounters of which 30% (n=2683) occurred via telehealth. The proportion of telehealth visits peaked in April 2020 (60%) and remained greater than 18% of all monthly visits through March 2021 (Figure 2).
Figure 2: Proportion of Clinic Encounters by Type at ARcare
Access to Care via Telehealth and Blood Pressure Control
- Barriers: ARcare staff observed that older adult patients were more resistant to using telehealth or lacked the necessary skills to use telehealth technologies. Additionally, some patients experienced barriers to accessing care via telehealth that were attributed to unreliable broadband internet access in rural areas.
- Facilitators: ARcare staff perceived that telehealth reduced no-show rates, increased medication adherence, and increased patient reach. At the same time, health care professionals perceived that telehealth helped some patients overcome transportation barriers that had previously limited their access to health care.
A lot of our patients in the more rural areas, of course, don’t have the technology. It’s the broadband, the internet connection, but it’s also their cell phone plans, because if you have a cell phone plan and you don’t have a lot of data, that telemed(icine) consult could eat up all the data they have for that month.
The evaluation assessed aggregate changes in blood pressure control rates among patients with a diagnosis of high blood pressure who sought telehealth services between March 2019 and March 2021.
There were no statistically significant differences in blood pressure control between the baseline period (53.4%, March 2019-February 2020) and following the rapid expansion of telehealth services during the COVID-19 pandemic (57.4%, March 2020-March 2021) (p=0.31).
This finding provides early evidence that blood pressure control rates remained relatively consistent during these time periods and that telehealth may be a suitable strategy for addressing the needs of ARcare patients with a diagnosis of high blood pressure during the time period observed.
Evaluation Findings: Terros Health
Health Overview
Terros Health is headquartered in Maricopa County, Arizona, and provides primary care, chronic disease management, and trauma-informed behavioral health services at 13 locations, including four FQHCs.
Telehealth Implementation
Prior to March 2020, Terros Health exclusively provided in-person health care services through their four FQHC primary care clinics. In March 2020, at the start of the COVID-19 pandemic, Terros rapidly adopted telehealth services to maintain continuity of health care while minimizing in-person visits.
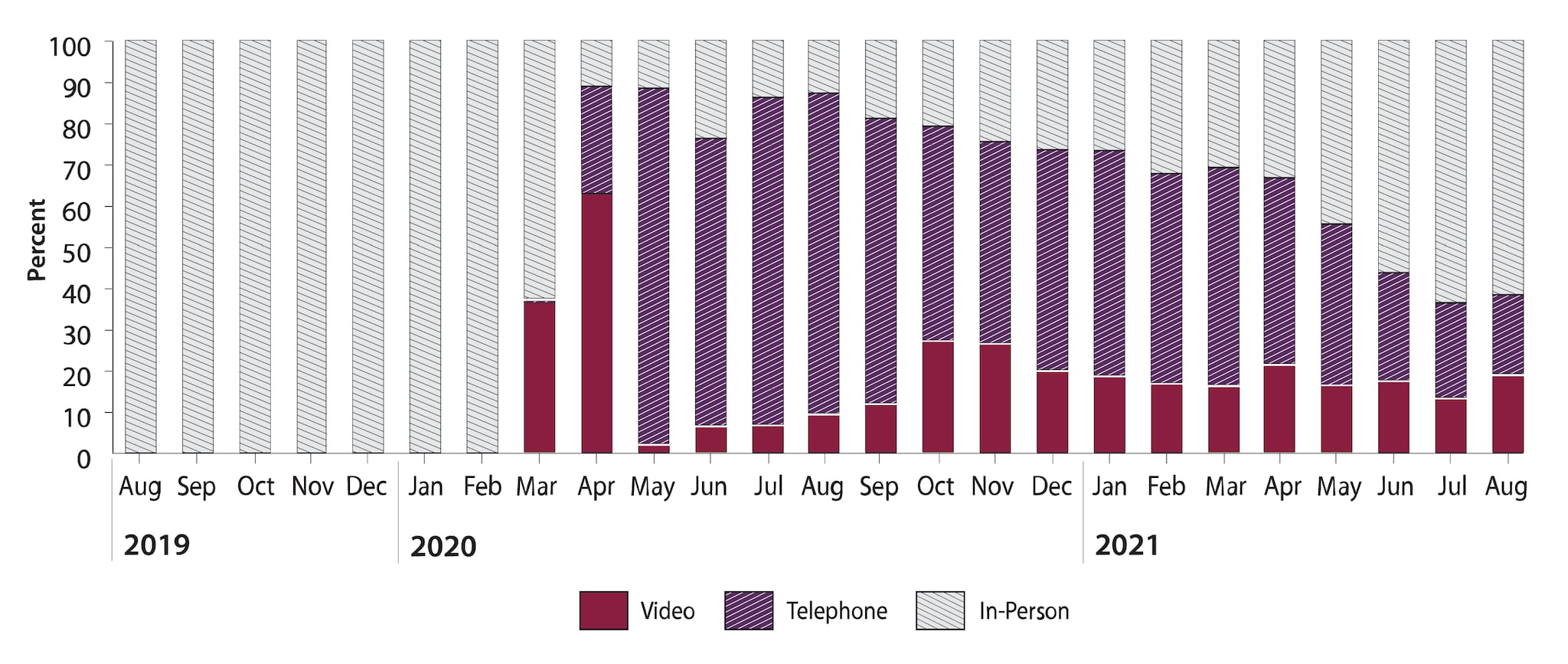
From March 2019 to August 2021, there were a total of 10,287 encounters across all patients, of which 58.9% (n= 6,063) occurred in person, 41.0% (n=4,224) occurred by telehealth using either video-based or telephone-only modalities.
The proportion of patients with a telehealth visit increased to 36.8% in March 2020, peaked at 89.1% in July 2020, and represented between 35.0% and 70.0% of visits between August 2020 and August 2021 (Figure 3).
Figure 3: Proportion of Clinic Encounters by Type at Terros Health
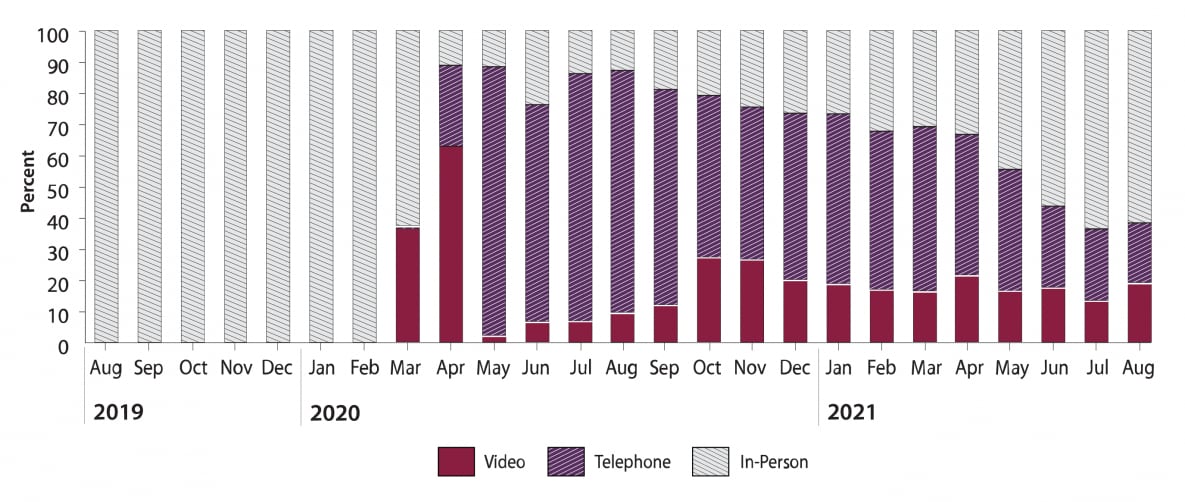
View HTML alternative description of this bar chart.
Access to Care via Telehealth and Blood Pressure Measurement
- Barriers: Terros staff and health care professionals perceived that broadband internet access, homelessness, and patient-preferred language were barriers for patients accessing care through telehealth. Additionally, Terros staff qualitative reported differences in telehealth adoption among patients according to patients’ race and ethnicity.
- Facilitators: Terros staff and health care professionals perceived that telehealth reduced no-show rates, maintained continuity of care and medication adherence during the pandemic, and increased reach and utilization of health care services specifically among patients who could not take time off work or needed to find childcare coverage for an in-person appointment. Additionally, Terros Health staff and health care professionals perceived that telehealth helped patients overcome transportation barriers that limited access to in-person health care.
There were a substantial number of missing blood pressure readings overall (39.4%, n = 4,062), differing significantly by encounter type (p < 0.001)—in-person visit, video, or telephone. From March 2019 through August 2021, more than 85% of blood pressure readings were missing for all telehealth visits, while only 8% of blood pressure readings were missing for in-person encounters, indicating that telehealth may present challenges for consistently recording blood pressure in a virtual setting.
The adoption rate for White non-Hispanic patients was almost immediate; it was very quick. It was like, ‘Okay, we’re good to go.’ For Black, White Hispanic, Native American, basically everybody else, it was a slow and very steady, and it remained disparate significantly.
Related Resources
- CDC: Telehealth Interventions to Improve Chronic Disease
- CDC: Evaluation Results and Lessons Learned
- CDC: Evaluation Guides & Toolkits
- Million Hearts® and CDC Foundation: COVID-19 and Cardiovascular Disease Partner Toolkit
- ARcare Augusta
- Terros Health
References
- Koonin LM, Hoots B, Tsang CA, Leroy Z, Farris K, Jolly T, et al. Trends in the use of telehealth during the emergence of the COVID-19 pandemic—United States, January–March 2020. MMWR Morb Mortal Wkly Rep. 2020;69(43):1595–1599.
- Demeke HB, Merali S, Marks S, Pao LZ, Romero L, Sandhu P, et al. Trends in use of telehealth among health centers during the COVID-19 pandemic—United States, June 26–November 6, 2020. MMWR Morb Mortal Wkly Rep. 2021;70(7):240–244.
- Virani SS, Alonso A, Aparicio HJ, Benjamin EJ, Bittencourt MS, Callaway CW, et al. Heart disease and stroke statistics—2021 update: a report from the American Heart Association. 2021;143(8):e254–e743.