Chronic Diseases and Military Readiness
Preventing and controlling chronic diseases is a matter of national security.
The nation’s armed forces depend on men and women who are fit, healthy, and able to perform at their peak on or off the battlefield. But active duty military members (service members) and potential recruits are not immune to the health problems that affect the rest of the US population, and the impact on military readiness is substantial.
Chronic diseases such as heart disease, cancer, and type 2 diabetes are the leading contributors to death, disability, and health care costs in the United States. They are mainly caused by a few common risk behaviors:
- Poor nutrition, including diets low in fruits and vegetables and high in sodium, saturated fats, and added sugars.
- Lack of physical activity.
- Tobacco use and exposure to secondhand smoke.
- Excessive alcohol use, including binge drinking.
These behaviors often start in youth and become more common and serious as people enter young adulthood. CDC’s National Center for Chronic Disease Prevention and Health Promotion funds programs to prevent or reduce these behaviors, starting in childhood, and works with the US Department of Defense (DOD) on projects to improve military health.
Promoting Better Nutrition and More Physical Activity

Poor nutrition and lack of physical activity can lead to obesity. More than 1 in 3 young adults are too heavy to serve in the US military. Among those who meet weight requirements, only 3 in 4 report physical activity levels that prepare them for challenges in basic training. Consequently, only 2 in 5 young adults are both weight-eligible and active enough for military service.
Obesity does not just limit the readiness of potential recruits. From 2008 to 2017, service members had more than 3.6 million musculoskeletal injuries. One study found that service members with obesity were 33% more likely to get this type of injury. In 2020, 19% of service members had obesity, up from 16% in 2015.
DOD spends about $1.5 billion a year in obesity-related health care costs for current and former service members and their families, as well as costs to replace unfit personnel. Lost workdays due to overweight and obesity costs DOD $103 million a year.
Increasing the Access of Healthy Foods

From 2016 to 2019, CDC’s Division of Nutrition, Physical Activity, and Obesity (DNPAO) offered a fellowship for DOD personnel. This fellowship led to increased opportunities and expertise for providing healthier foods and drinks on military bases and in surrounding communities. These fellows helped create an infographic on how obesity is affecting national security and promoted the use of food service guidelines in DOD facilities.
DNPAO staff also helped Jacksonville Naval Hospital in Jacksonville, Florida, create a food environment where healthy choices are easy to make—including setting up a healthy micromarket with automated access to food and drinks 24 hours a day. DNPAO continues to work with the Navy and other DOD branches and the Joint DOD Food & Nutrition and Dietary Supplement Subcommittees to determine how to make it easier for people to get and choose healthier foods.
In addition, DNPAO staff led the update of the 2017 Food Service Guidelines for Federal Facilities, working with nine federal agencies, including DOD. DNPAO, DOD, and other partners also participate in the Food Service Guidelines collaborative, which supports the purchasing and selling of healthier foods and drinks in government facilities, military bases, worksites, hospitals, universities, and other institutional settings.
Increasing Opportunities to be Physically Active
Only half of adults and about one-fourth of young people get recommended amounts of aerobic physical activity. Physical activity offers many performance and health benefits for current and future service members, including:
- Improved aerobic and muscular fitness.
- Improved balance and bone health.
- Improved joint mobility.
- Improved mental health.
- Reduced risk of falling.
- Extended years of active life.
DNPAO recommends the following strategies to increase physical activity, based on evidence from the Community Preventive Services Task Force:
- Activity-friendly routes to everyday destinations.
- Access to places for physical activity.
- School and youth programs.
- Community-wide campaigns.
- Social supports.
- Individual supports.
- Prompts to encourage physical activity.
Reducing Tobacco Use

Cigarette smoking is the leading cause of preventable death and disease in the United States. Over 16 million Americans have at least one disease from smoking, and 480,000 Americans die from smoking-related diseases each year. Commercial tobacco use harms military readiness by reducing service members’ physical fitness and strength. It also makes them more likely to become sick, get injured, and have delayed healing if wounded. Tobacco use also cost DOD nearly $1.8 billion in medical and nonmedical costs in 2014.
The percentage of service members who smoke cigarettes has historically been higher than that of the general adult population but has been dropping in recent years, along with declines in smoking in the general population. In 2018, more than 18% of active duty personnel reported that they currently smoke.
The percentage of service members who use smokeless tobacco (chewing tobacco, snuff, dip, or snus) is also higher than in the general population. In addition, e-cigarette use is increasing among service members. Data from 2018 show e-cigarette use remains high, with several service branches reporting e-cigarettes as the most commonly used product.
Helping Service Members Quit
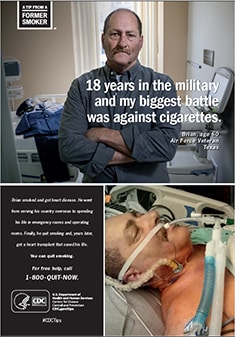
CDC’s Tips From Former Smokers® (Tips®) campaign focuses on motivating US adults who smoke to try to quit. Tips features real people—not actors—who are living with serious health conditions caused by smoking and secondhand smoke exposure. The newest Tips series adds compelling stories from family members who take care of loved ones affected by a smoking-related disease or disability.
The campaign connects people who smoke with resources to help them quit, including 1-800-QUIT-NOW, which directs people to free services available from their state quitlines. From 2012–2018, CDC estimates that more than 16.4 million people who smoke have attempted to quit and about 1 million have successfully quit because of the Tips campaign.
CDC’s Office on Smoking and Health (OSH) worked with DOD and the US Department of Veterans Affairs (VA) to develop a military-focused ad for the 2016 Tips campaign. The Tips website includes tailored content on dedicated cessation resources to help service members and veterans quit.
In the spring of 2021, CDC worked closely with DOD and the VA to develop and launch a Tips From Former Smokers Military Service Members & Veterans Media Outreach Kit. The kit contains materials that show the problem of tobacco use in the military and cessation resources that can be used for media outreach or shared with public on websites and during events. The resource is designed to reach CDC military and VA partners and their constituents.
Preventing Binge Drinking

Excessive alcohol use contributes to 95,000 deaths in the United States each year, including 1 in 10 deaths among working-age adults. Binge drinking (at least 5 drinks on an occasion for males or 4 drinks on an occasion for females) is responsible for almost half of these deaths. Binge drinking is also related to health and social problems, including alcohol-impaired driving, violence, unintended pregnancy, and alcohol use disorders.
Drinking too much lowers service members’ military readiness by impairing cognitive and motor function, including response time, decision making, and other critical combat skills, as well as workplace productivity. A 2013 report from the Institute of Medicine found that excessive alcohol use among service members “adversely affect[s] military readiness, family readiness, and safety, thereby posing a significant public health problem for the Department of Defense.”
According to a 2018 DOD health behavior survey, 1 in 3 active service members reported binge drinking in the past 30 days. That compares to 1 in 6 US adults in the overall population, According to a CDC survey conducted that same year. The CDC survey also found binge drinking was significantly higher among veterans than nonveterans. Increased combat exposure involving violence and trauma may increase the risk of excessive drinking. Alcohol use disorders are the most common form of substance use disorders among military personnel.
The Community Preventive Services Task Force recommends the following measures to reduce excessive alcohol use and related harms in communities:
- Regulating alcohol outlet density.
- Increasing alcohol taxes.
- Holding retailers accountable for harms that result from illegally serving or selling alcohol.
- Enforcing laws that prohibit alcohol sales to minors.
- Using electronic devices—such as computers, telephones, and mobile devices—to screen people for excessive alcohol use and deliver a brief intervention.
Connecting Military Communities With State and Local Public Health Resources
DNPAO and OSH are collaborating with DOD (Personnel and Readiness), the National Guard Bureau, and the National Association for Chronic Disease Directors to support DOD’s Total Force Fitness (TFF) framework. One TFF initiative is Building Healthy Military Communities (BHMC), which is working to coordinate and integrate DOD, federal, state, regional, and local efforts in support of service members and their families in seven states.
DNPAO and OSH have provided funding to the National Association for Chronic Disease Directors since October 2018 to:
- Connect military communities in BHMC pilot states with local and state support to prevent chronic disease associated with poor nutrition, lack of physical activity, obesity, and tobacco use.
- Identify opportunities to implement strategies that can help prevent health risk behaviors among service members and their families.
- Develop a toolkit for DOD service providers to better connect service members with national and state public health resources.



