Behavioral Risk Factor Surveillance System (BRFSS) Cognitive Decline Module
Frequently Asked Questions
In 2007, the CDC Healthy Aging Program—in collaboration with national experts—developed a 10-question Behavioral Risk Factor Surveillance System (BRFSS) module to measure subjective cognitive decline (SCD) and its associated effects. CDC developed these survey questions because of the importance of cognitive impairment as a public health issue, and following the recommendation to develop population-based surveillance in The Healthy Brain Initiative: A National Public Health Road Map to Maintaining Cognitive Health [PDF – 3 MB], the first document in the public health Road Map series. The CDC consulted with a national panel of experts to develop the items. The CDC consulted with a national panel of experts to develop the items.
The CDC selected the BRFSS because it is a state-based surveillance system of US adults that askes respondents their health and a wide range of health behaviors. The primary focuses of the BRFSS are behaviors and conditions associated with the leading causes of death—heart disease, cancer, stroke, accidents, Alzheimer’s disease, and diabetes.
The CDC’s Alzheimer’s Disease Program is located within the Healthy Aging Branch. The Program’s focus on brain health ensures that data collection on cognitive decline continues to be a public health priority. As a result, the most recent update to the Healthy Brain Initiative’s Public Health Road Map series contains several actions that focus on data collected from the BRFSS Cognitive Decline module.
A multi-step process was used to develop the questions for the module. A scientific literature review was conducted to identify existing surveys and questions that measure cognitive decline and impairment. Next, a panel of subject matter experts reviewed questions used on other surveys, adapted existing questions, and developed a set of possible questions for the module. The module was finalized after four rounds of cognitive and field testing in California’s BRFSS survey during Fall 2008. In 2009, five states (California, Florida, Iowa, Louisiana, and Michigan) pilot-tested the module in their BRFSS surveys.
From 2011–2013, 47 states and territories added the Cognitive Impairment module (as it was then called) as an official optional module (in 2011) and as state-added questions (in 2012 and 2013).
The CDC revised the module in 2015 based on feedback from data users and a panel of experts. The Cognitive Decline module underwent two rounds of cognitive testing before it was finalized and approved by BRFSS coordinators to be included as an optional module starting in the 2015 BRFSS.
Beginning in 2015, the BRFSS Cognitive Decline optional module included the following revisions:
- The module was shortened from 10 to 6 questions in responses to concerns about the length of the module.
- The module is asked to BRFSS respondents aged 45 years or older. Data indicated that this age group was more likely to answer “yes” to the index question than those 44 years or younger.
- The name of the module was changed to the Cognitive Decline module to better reflect the measure.
- The introductory text was edited to provide greater clarity based on feedback from the cognitive testing.
The questions measure the BRFSS respondents’ perceptions about any confusion or memory loss that is happening more often or is getting worse:
- During the past 12 months, have you experienced confusion or memory loss that is happening more often or is getting worse?
This question captures symptoms of cognitive decline that are more frequent or worse over time, subjective cognitive decline (SCD). If a respondent answers “yes” to this question, other questions are asked to help understand the impact of SCD on functioning:
- During the past 12 months, as a result of confusion or memory loss, how often have you given up day-to-day household activities or chores you used to do, such as cooking, cleaning, taking medications, driving, or paying bills?
- As a result of confusion or memory loss, how often do you need assistance with these day-to-day activities?
- When you need help with these day-to-day activities, how often are you able to get the help that you need?
- During the past 12 months, how often has confusion or memory loss interfered with your ability to work, volunteer, or engage in social activities outside the home?
- Have you or anyone else discussed your confusion or memory loss with a health care professional?
These questions address how often SCD causes individuals to give up household chores or activities outside the home, whether they need assistance and can get the help they need, and whether anyone has discussed SCD with a health care professional.
Because the questions are not trying to measure whether the person has a medical condition or diagnosis, we encourage to refer to the measure as subjective cognitive decline (SCD) because it is a self-reported (subjective) measure of cognitive function that is worsening over time.
The module can provide the following state-level data leading to valuable insights:
- Percentage of adults aged 45 years or older who experience subjective cognitive decline (SCD).
- Percentage of adults aged 45 years or older who experience difficulties with daily activities due to SCD.
- Health conditions and behaviors of adults aged 45 years or older experiencing SCD (respondent-level data can be linked to other BRFSS measures such as health insurance and chronic conditions).
- Percentage of adults aged 45 years or older who experience SCD and live alone.
- Reported need for assistance with activities due to SCD and whether individuals receive the help they need.
- Relationship to other behavioral health factors from the BRFSS core or co-administered optional modules.
Declines in cognitive function vary among people and can include changes in attention, memory, learning, executive function (the ability to perform activities such as planning, organizing, paying attention, and remembering details), and language capabilities that negatively affect quality of life, personal relationships, activities of daily living, and the capacity for making informed decisions about health care and other matters. Changes in memory are typically one of the first warning signs of cognitive decline, possibly because of the development of Alzheimer’s disease or a related dementia. Some causes of cognitive decline are reversible (including, but not limited to, depression, infections, medication side effects, or nutritional deficiencies). These can be serious and should be treated by a health care provider as soon as possible.
There is increased attention and greater public health awareness about Alzheimer’s disease and related dementias. States and communities need to know about the burden of these conditions for planning of health care and long-term care needs as well as major caregiving and financial challenges.
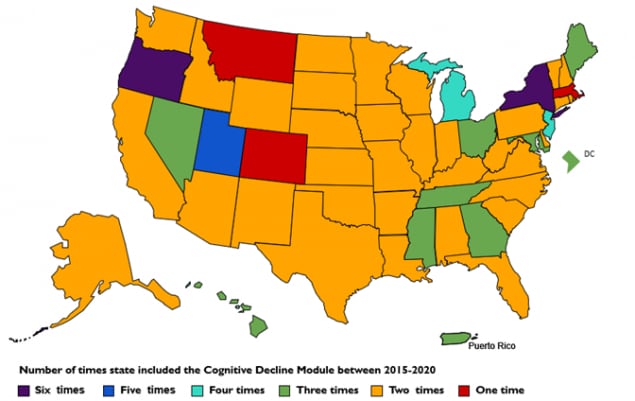
In 2015 and 2016, 49 states, the District of Columbia, and Puerto Rico administered the current Cognitive Decline module at least once. A report on the prevalence of SCD references the states that have used the module to date. Since 2016, states continue to administer this module to BRFSS respondents. States administering the current Cognitive Decline module varies by year. Information regarding states that administered the Cognitive Decline module by year are available on the BRFSS website and corresponding infographics are available.
This statistical brief [PDF – 2 MB] provides guidance for analyzing data from the current BRFSS Cognitive Decline Optional Module.
It is important to understand that any measure of subjective cognitive decline (SCD) obtained from the BRFSS is meant for public health purposes to help describe the burden associated with SCD in states.
Because questions are self-reported and not designed to assess whether the person has a medical condition or a medical diagnosis, the data are not intended to be reported as a prevalence measure of a medical condition, such as dementia or Alzheimer’s disease.
The BRFSS surveys community-dwelling adults and does not include residents of long-term care homes, group homes, or other facilities. In addition, if the selected respondent cannot respond to the survey because of physical or cognitive limitations, that respondent and their entire household are removed from the sample.
The CDC publishes various research papers using data from the BRFSS Cognitive Decline module data. A list of these and other papers can be found here.
Since 2015, CDC, in collaboration with the Alzheimer’s Association, developed a series of state-specific infographic for each year that a state collects BRFSS data using the Cognitive Decline module. Infographics presenting combined national data overall and by various demographic groups are also available. These infographics are available at https://www.cdc.gov/aging/data/index.htm. Data can also be queried using the Alzheimer’s Disease and Healthy Aging Data Portal and a series data briefs for action are available on select topics.
Researchers not familiar with BRFSS data analyses should familiarize themselves with the methods unique to BRFSS, including weighting and ranking methods. More information can be found at CDC’s BRFSS site. This statistical brief [PDF – 2 MB] provides an overview and guidance for analyzing data from the current BRFSS Cognitive Decline Optional Module