What to know
- Zika virus can be passed from a pregnant woman to her fetus.
- Infection during pregnancy can lead to congenital Zika syndrome and other birth defects.
- Zika virus infection does not impact future pregnancies.

Overview of Zika-associated birth defects
Zika virus infection during pregnancy can cause birth defects of the brain or eye. These birth defects can occur alone or with developmental problems in a particular pattern called congenital Zika syndrome. The following conditions can occur in a baby with congenital Zika virus infection:
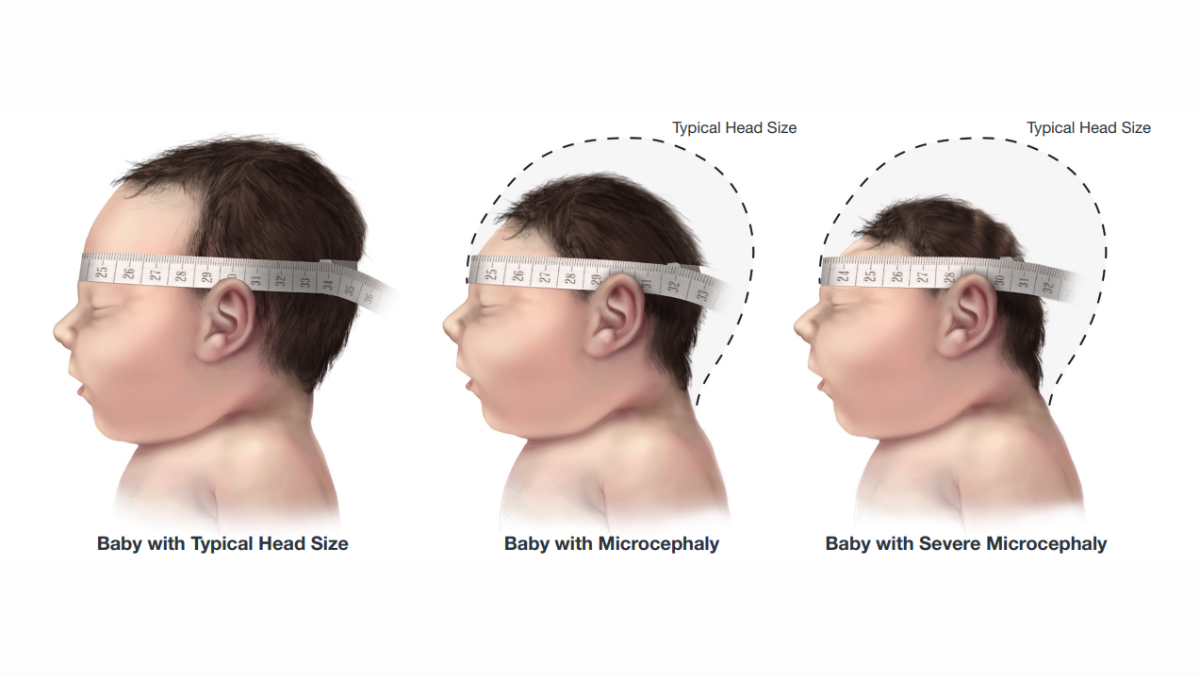
- Smaller than expected head size, called microcephaly
- Problems with brain development
- Feeding problems, such as difficulty swallowing
- Hearing loss and vision problems
- Seizures
- Decreased joint movement, called contractures
- Stiff muscles, making it difficult to move
Not all babies born with congenital Zika syndrome will have all of these conditions. Some infants who do not have microcephaly at birth may develop it later. In addition, some babies might look healthy at birth but can develop long-term health problems as they grow.
Recommended screenings
If your baby was born with congenital Zika infection, they should receive recommended screenings even if they appear healthy. Babies and children affected by Zika virus may have lasting special needs. They may require specialized care from many types of healthcare providers and caregivers as they age.
Frequency of Zika-associated birth defects
Zika virus does not cause birth defects for every baby exposed to the virus before birth (i.e., in utero). Infection with Zika virus during pregnancy simply increases the chances for these problems. Among women with confirmed or possible Zika infection during pregnancy in U.S. states and territories, Zika-associated birth defects occurred in about 5% of babies.1

Zika symptoms and birth defects
Zika-associated birth defects can occur whether or not the pregnant woman had symptoms of the infection during pregnancy. In the U.S. states and territories, about 1 in 20 (5.3%) people with symptoms of Zika virus infection during pregnancy had a baby with Zika-associated birth defects, compared with about 1 in 25 (4.2%) people infected with Zika virus but had no symptoms during pregnancy.1
Timing of Zika during pregnancy
Zika-associated birth defects are more common among infants born to women with exposure early in pregnancy. The highest risk of Zika-associated birth defects is with infection during the first and second trimesters. In the U.S. states and territories, about 2 in 25 (8%) pregnant women with confirmed Zika virus infection in the 1st trimester had babies with Zika-associated birth defects.1

Future pregnancies
Zika virus infection in a woman who is not pregnant does not pose a risk for future pregnancies. Like with other similar infections, once a person has been infected, they are likely to be protected from a future infection.
Support for families affected by Zika
Learn about Resources and Support Groups available to families living with birth defects.
- Roth NM, Reynolds MR, Lewis EL, et al. Zika-associated Birth Defects Reported in Pregnancies with Laboratory Evidence of Confirmed or Possible Zika Virus Infection — U.S. Zika Pregnancy and Infant Registry, December 1, 2015–March 31, 2018. MMWR Morb Mortal Wkly Rep 2022;71:73–79. DOI: http://dx.doi.org/10.15585/mmwr.mm7103a1external icon.
- Rice ME, Galang RR, Roth NM, et al. Vital Signs:Zika-Associated Birth Defects and Neurodevelopmental Abnormalities Possibly Associated with Congenital Zika Virus Infection — U.S. Territories and Freely Associated States, 2018. MMWR Morb Mortal Wkly Rep.2018;67:858-867. DOI: http://dx.doi.org/10.15585/mmwr.mm6731e1external iconexternal icon
- Smoots AN, Olson SM, Cragan J, et al. Population-Based Surveillance for Birth Defects Potentially Related to Zika Virus Infection — 22 States and Territories, January 2016–June 2017. MMWR Morb Mortal Wkly Rep 2020;69:67–71. DOI: http://dx.doi.org/10.15585/mmwr.mm6903a3.external icon
