Technical Report 2: Multi-National Mpox Outbreak, United States, 2022
Mpox Archive Content
You are viewing an archived web page, collected from CDC’s Mpox website. The information on this web page may be out of date.
Report reflects data and terms used as of August 26, 2022, prior to the World Health Organization’s decision to adopt the term “mpox”.
This is a technical report intended for scientific audiences. Additional information, including materials targeted to the general public, are available on the mpox site.
The purpose of this report is to provide timely updates regarding CDC’s ongoing response to the mpox outbreak in the United States, and to share preliminary results of new analyses that can improve understanding of the outbreak and inform further scientific inquiry. This report is intended for a technical audience; each report features a combination of standing topics and the results of special analyses.
U.S. Case Data
On May 17, 2022, the United States confirmed the first monkeypox case in Massachusetts. As of August 26, there are 17,432 cases in all 50 states, the District of Columbia, and Puerto Rico (Figure 1). These case counts include those who tested positive for either monkeypox virus or orthopoxvirus as described in the 2022 Monkeypox Response case definition. An epidemiological curve of all monkeypox cases reported to CDC through August 26, 2022, is depicted in Figure 2. A 14-day rolling average has been included in the epidemiological curve to help account for fluctuations in daily reporting. Additionally, a cumulative case count curve of monkeypox cases by report date is provided in Figure 3. Case data are voluntarily reported by states.
The median age of cases reported into CDC’s Data Collection and Integration for Public Health Event Response (DCIPHER) platform is 35 years (range: <1 year to 89 years). We are aware of 7 total confirmed pediatric cases, defined as those under 18 years of age, which presented clinical compatible disease and tested positive with a monkeypox virus specific testing. Currently, all pediatric cases are subject to in-depth interview and confirmatory molecular testing for monkeypox virus to eliminate the possibility of false positive test results. As of this report, investigations were initiated for a total of 45 probable pediatric cases. There were 21 cases aged 13-17 years, 3 of whom were confirmed cases and 18 of whom are under investigation or pending additional test results. Of 24 cases aged 12 years or younger, 16 are under investigation or pending additional test results, and 8 had completed interviews and testing, 4 of whom were confirmed cases.
Data on sex assigned at birth are available for 52.2% (n=9,071) of cases reported to CDC. Among those with available data, 8,907 (98.2%) report male sex at birth and 164 (1.8%) report female sex at birth. Gender identity data are available for 70.8% (n=12,289) of cases reported into DCIPHER. Among those for whom gender identity is available, 11,988 (97.6%) are men, 182 (1.5%) are women, 42 (<1%) are transgender women, 17 (<1%) are transgender men, and 60 (<1%) are another gender identity.
Gender or sex data are available for 76.9% (n=13,369) of cases reported to CDC. People whose reported sex differed from their reported gender were classified as transgender. Among people for whom reported gender was not available, but sex was reported, sex was used to categorize people as female or male. While the case report form specifies sex assigned at birth, there are variations in how jurisdictions collect sex, and in some cases, this may represent current gender. Recognizing these limitations, among those with available gender or sex data, 12,959 (96.9%) are men, 215 (1.6%) women, 54 (<1%) transgender men, 70 (<1%) transgender women, and 71 (<1%) another sex or gender.
Race and ethnicity data are available for 59.2% (n=10,297) of cases reported to CDC. Approximately 33.1% (n=3,413) of cases with known race/ethnicity are Non-Hispanic White, 31.1% (n=3,218) are Hispanic (of any race), 31.1% (n=3,205) are non-Hispanic Black, and 3.7% (n=381) are non-Hispanic Asian. Less than 1% of cases with available race/ethnicity data report being American Indian or Alaska Native (n=34), or Native Hawaiian or other Pacific Islander (n=12), or multiple races (n=34).
Recent sexual history was defined as any sex and/or close intimate contact in the three weeks preceding symptom onset. Among 7,378 people with data on both recent sexual history and gender, 78.9% (n=5,820) reported man-to-man sexual contact (Figure 4). We note this proportion is lower than values previously reported for “male-to-male sexual contact” because this updated proportion better accounts for data variations by jurisdictions and is based on more complete data, resulting in more accurate estimates. Some jurisdictions also report sexual orientation to the CDC. Among 4,460 cases with known sexual orientation and gender, 4,159 (93.3%) were gay or bisexual men, 242 (5.4%) were straight or heterosexual men, and 59 (1.3%) were straight, lesbian, or bisexual women (Figure 5).
Symptom data are available for 38.3% (n=6,664) of cases reported to CDC. Among cases for which symptom data were available, nearly all reported rash (97.8%) and a majority reported non-specific prodromal symptoms such as malaise (70.7%), fever (83.8%), chills (66.5%), headache (62.8%), lymphadenopathy (62.0%), myalgia (59.8%), and pruritis (58.0%).
As of August 31, a total of 87,363 specimens have been tested for non-variola orthopoxvirus or monkeypox virus in the United States, including testing at public health and select commercial laboratories. Among those specimens, some of which may have come from the same patient, 30.9% were positive.
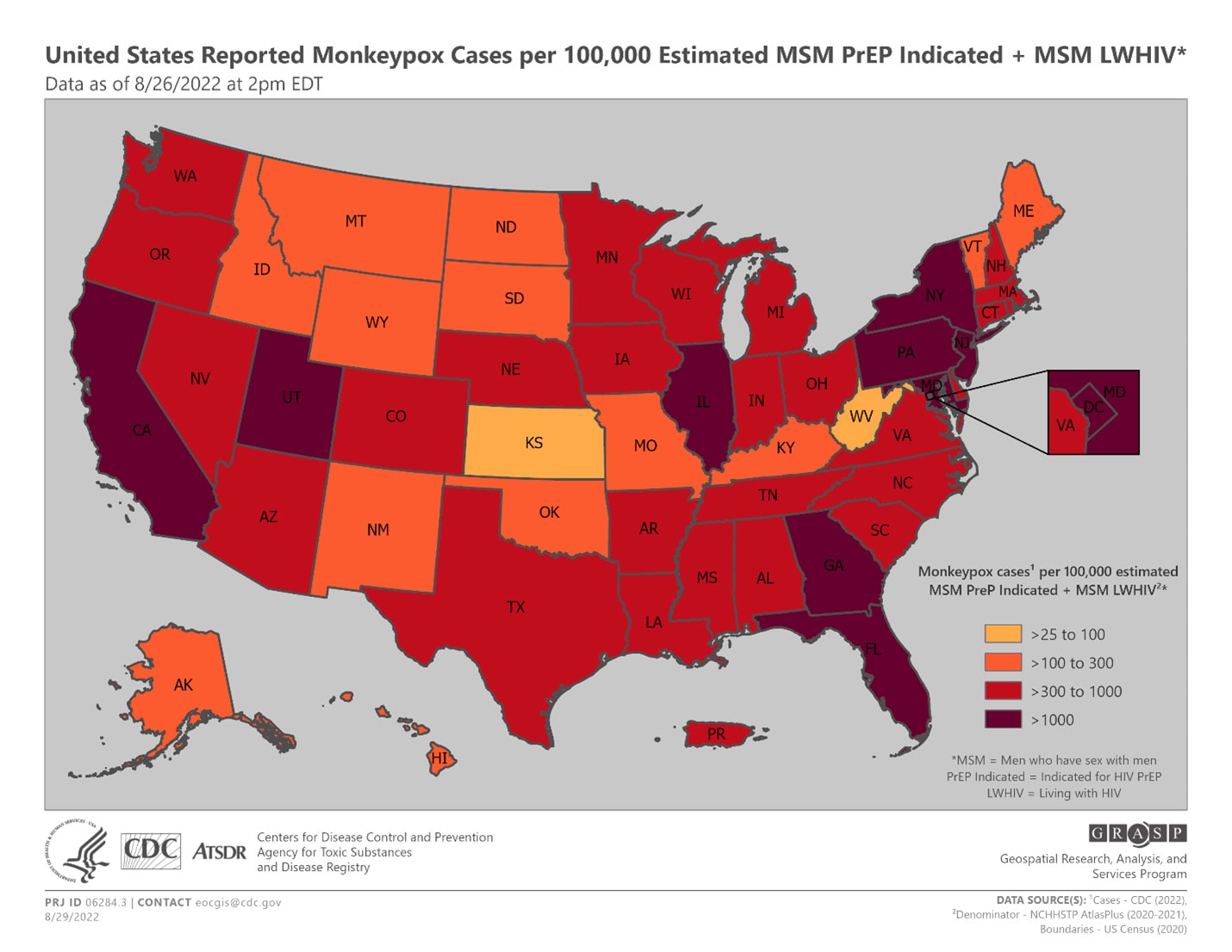
Figure 1. Monkeypox Case incidence/diagnosis rate per 100,000 estimated MSM PrEP Indicated + MSM living with HIV (LWHIV) by state or jurisdiction as of August 26, 2022.
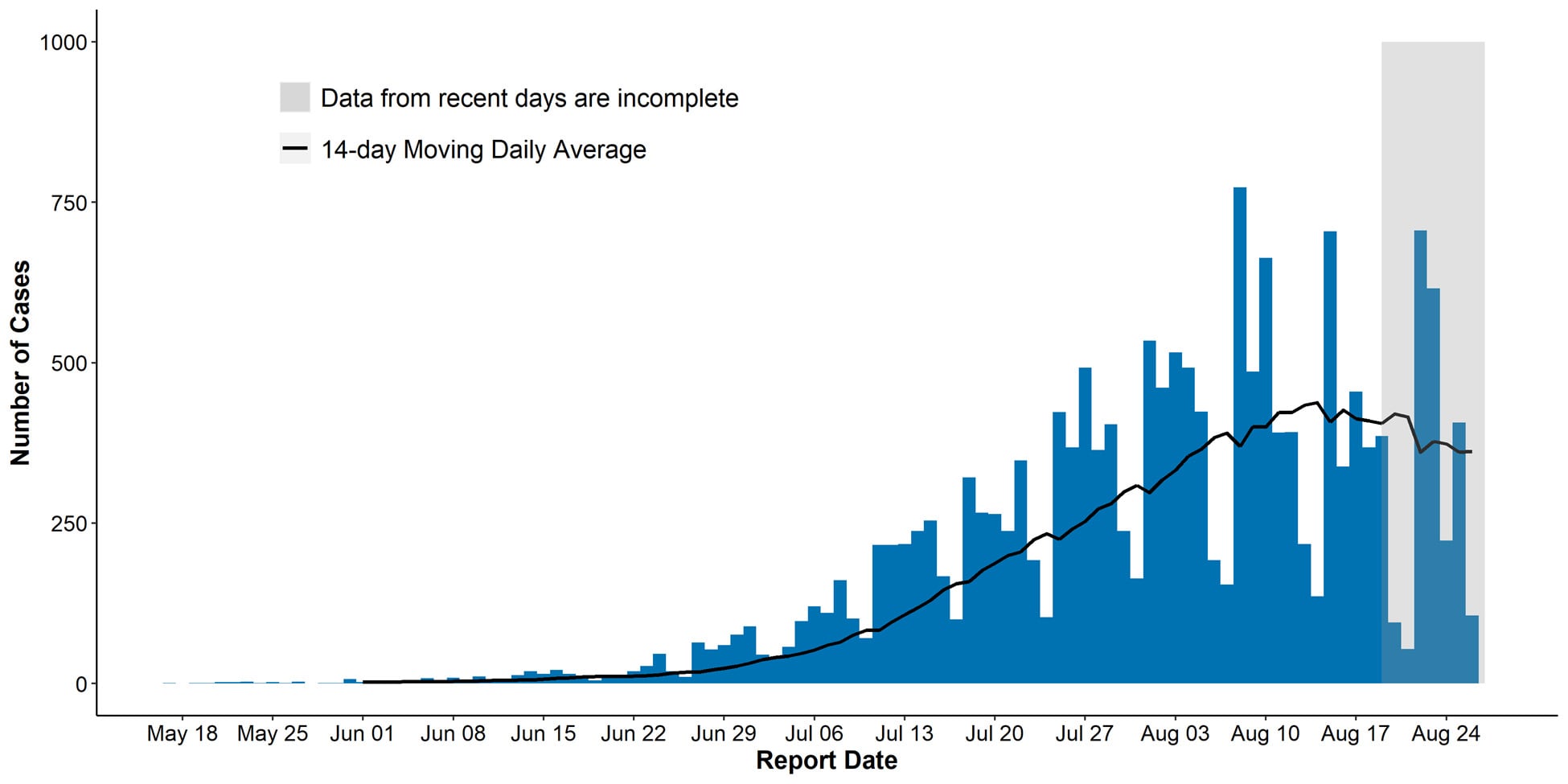
Figure 2. Epidemiological curve of monkeypox cases by report date (defined as the positive laboratory test report date, CDC call center reporting date, or case data entry date into CDC’s emergency response common operating platform, DCIPHER) as of August 26, 2022. Data for some cases may be updated when additional information is provided to CDC via DCIPHER.
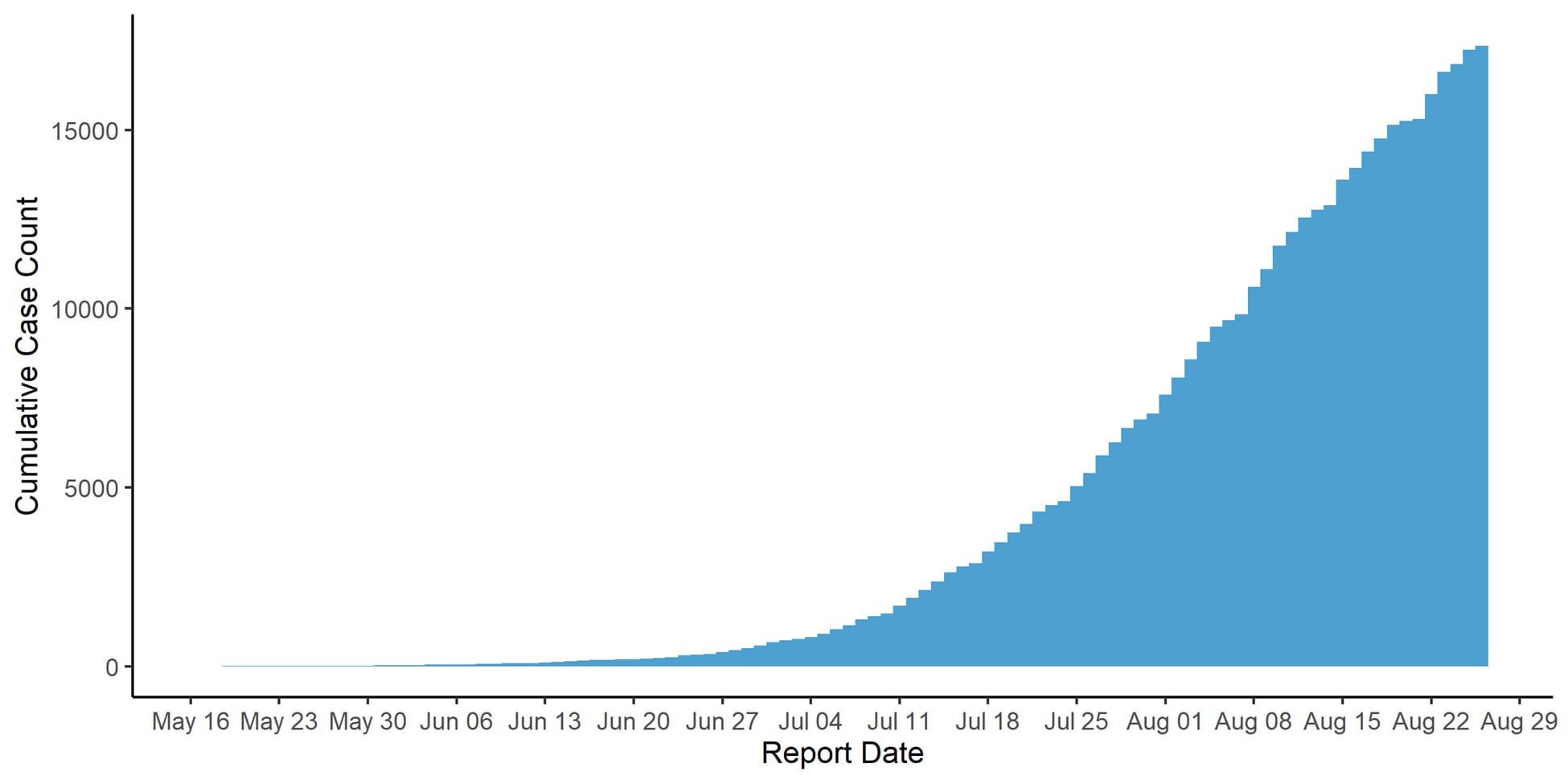
Figure 3. Cumulative count of monkeypox cases by report date (defined as the positive laboratory test report date, CDC call center reporting date, or case data entry date into CDC’s emergency response common operating platform, DCIPHER) as of August 26, 2022. Data for some cases may be updated when additional information is provided to CDC via DCIPHER.
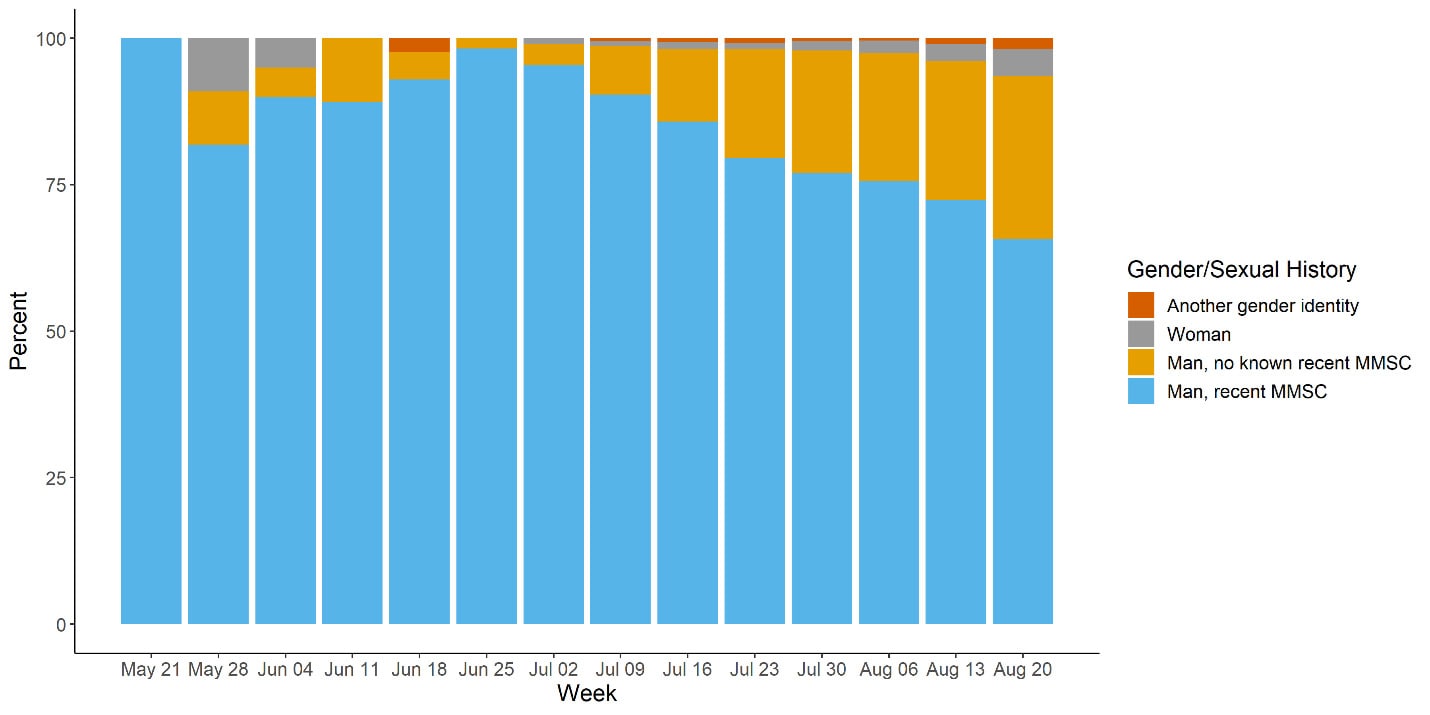
Figure 4. Proportion of cases with known data on sexual history and gender reporting recent man-to-man sexual contact (MMSC) by the week in which monkeypox case was reported (reporting date defined as the positive laboratory test report date, CDC call center reporting date, or case data entry date into CDC’s emergency response common operating platform, DCIPHER) as of August 26, 2022. Data for some cases may be updated when additional information is provided to CDC via DCIPHER. Due to the small number of cases in women and those with another gender identify, we did not further break these groups down by sexual history.
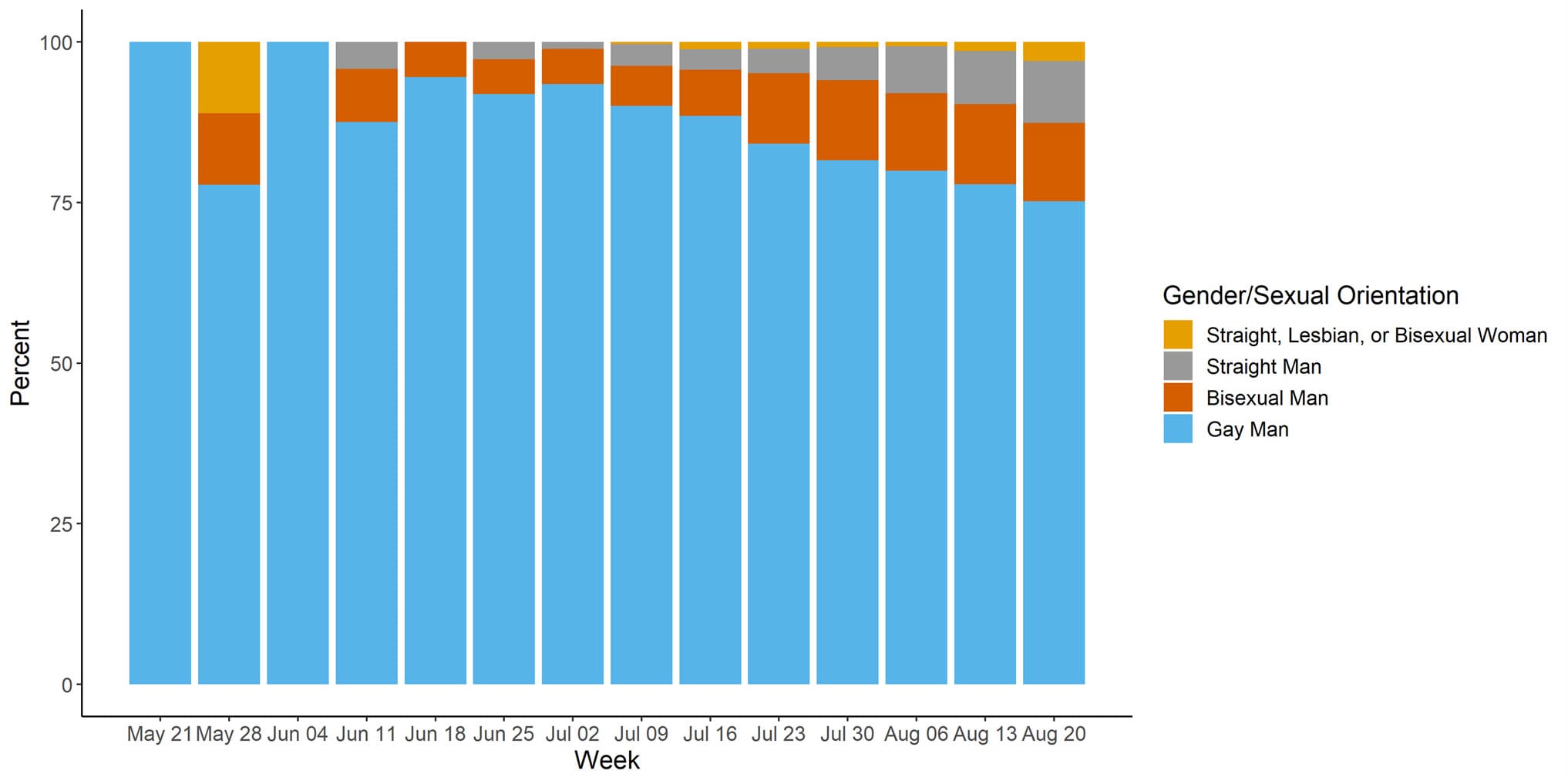
Figure 5. Proportion of sexual orientation and gender combination by the week in which monkeypox case was reported (reporting date defined as the positive laboratory test report date, CDC call center reporting date, or case data entry date into CDC’s emergency response common operating platform, DCIPHER) as of August 26, 2022. Data for some cases may be updated when additional information is provided to CDC via DCIPHER.
Global Outbreak
As of August 28, 2022 CDC is tracking 47,206 confirmed cases of monkeypox in 92 non-endemic countries, territories, and areas associated with the 2022 multinational outbreak (Figure 6). This count may include confirmed cases not yet reported in World Health Organization (WHO) official counts. In some countries, such as the United Kingdom and Portugal, daily case growth has slowed (Figure 7).
2022 Monkeypox and Orthopoxvirus Global Outbreak Map
Additional data on the global situation is available on the WHO and European Centre for Disease Prevention and Control ECDC
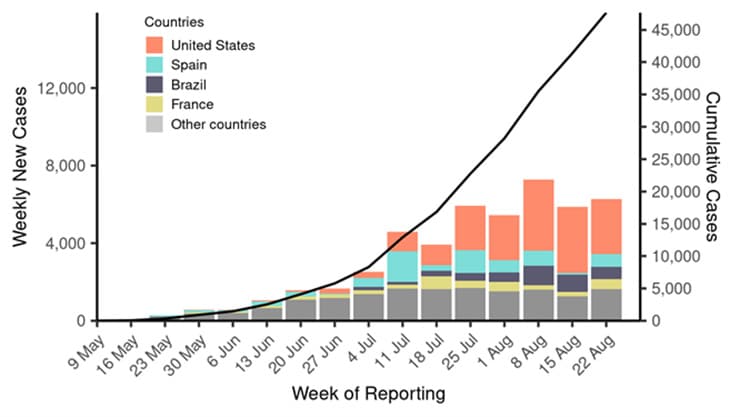
Figure 6. New and cumulative monkeypox cases by week globally as of August 28, 2022.
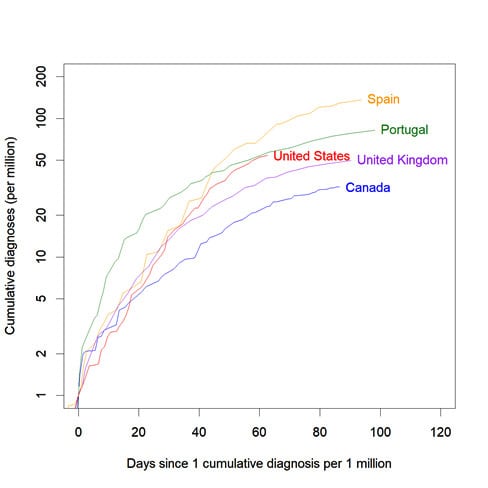
Figure 7. Cumulative incidence of monkeypox per million population for select countries, by day since reporting 1 cumulative diagnosis per million population. Data obtained from https://www.global.health as of August 30, 2022 at 9:40 AM.
Dynamics of U.S. Outbreak
Current Transmission Level
CDC is closely monitoring the nature of monkeypox transmission dynamics in the United States. Following levels defined by the UK Health Security Agency, the outbreak could fall into one of the following four transmission categories:
- Imported cases with limited onward transmission
- Spread within a defined sub-population
- Spread within multiple sub-populations or larger sub-population
- Significant, community-wide transmission
We assess the United States is likely experiencing spread within a defined sub-population, currently among gay, bisexual, and other men who have sex with men (MSM); we have moderate confidence1 in this assessment.
We base this assessment on epidemiological data indicating that the vast majority of cases have thus far occurred in adult men reporting sexual contact with other men, both in the United States and globally. We have also observed few cases of transmission to household contacts and non-sexual contacts to date, although we note the declining portion of cases reporting recent man-to-man sexual contact in the United States (Figure 4) and declining proportion of MSM globally could be signs that transmission through these routes is increasing. Finally, the potential for sustained spread among heterosexual networks is likely low, based on relatively lower partnership formation rates, extrapolating from modeling work from the United Kingdom (Endo et al. 2022; Brand et al. 2022).
Outbreak Growth Rate Estimates
Based on estimates from the first half of August, the monkeypox outbreak in the United States continued to grow exponentially, although there are recent signs the rate of growth is slowing. We estimated the outbreak doubling time is approximately 25 days, which has slowed from earlier estimates of doubling times of around 8 days throughout most of July (Figure 8). Our growth rate estimates are uncertain, and recent trend changes should be interpreted cautiously, given reporting delays and missing data. We have attempted to adjust for reporting delays, as shown in Figure 9 below, however adjustment is particularly sensitive to temporal changes in reporting delays. There are recent signs that case growth may have slowed further, but changes in data reporting processes have made it difficult to update this analysis with the most recent data.
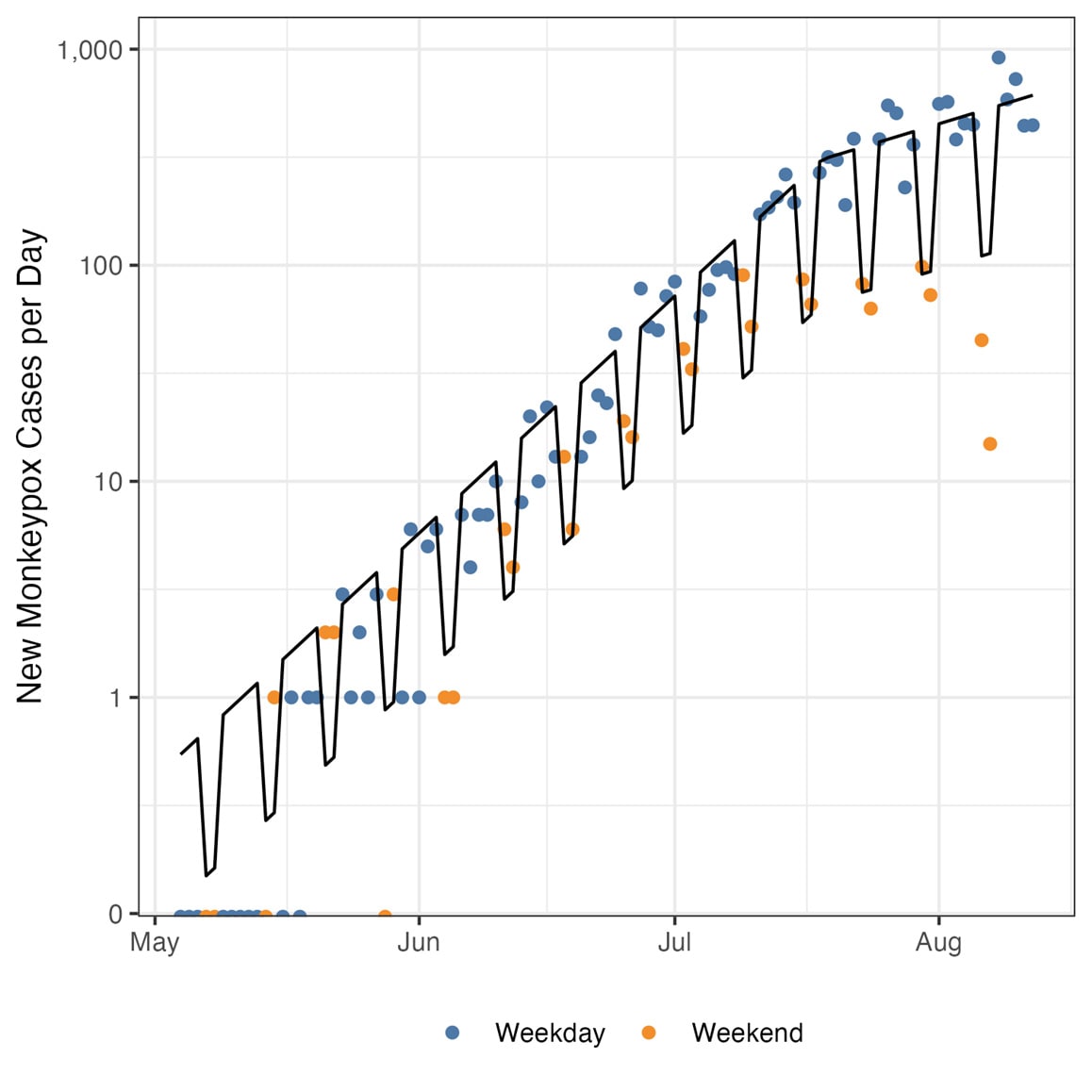
Figure 8. Daily monkeypox cases reported in the United States on weekdays (blue) and weekends (orange), corrected for reporting delays. The black line shows an exponential growth model fit to the adjusted case data, with a single rate changepoint and weekend effect adjustment. Data are visualized on a log scale to illustrate the decline in growth rate around mid-July. Data as of August 16, 2022.
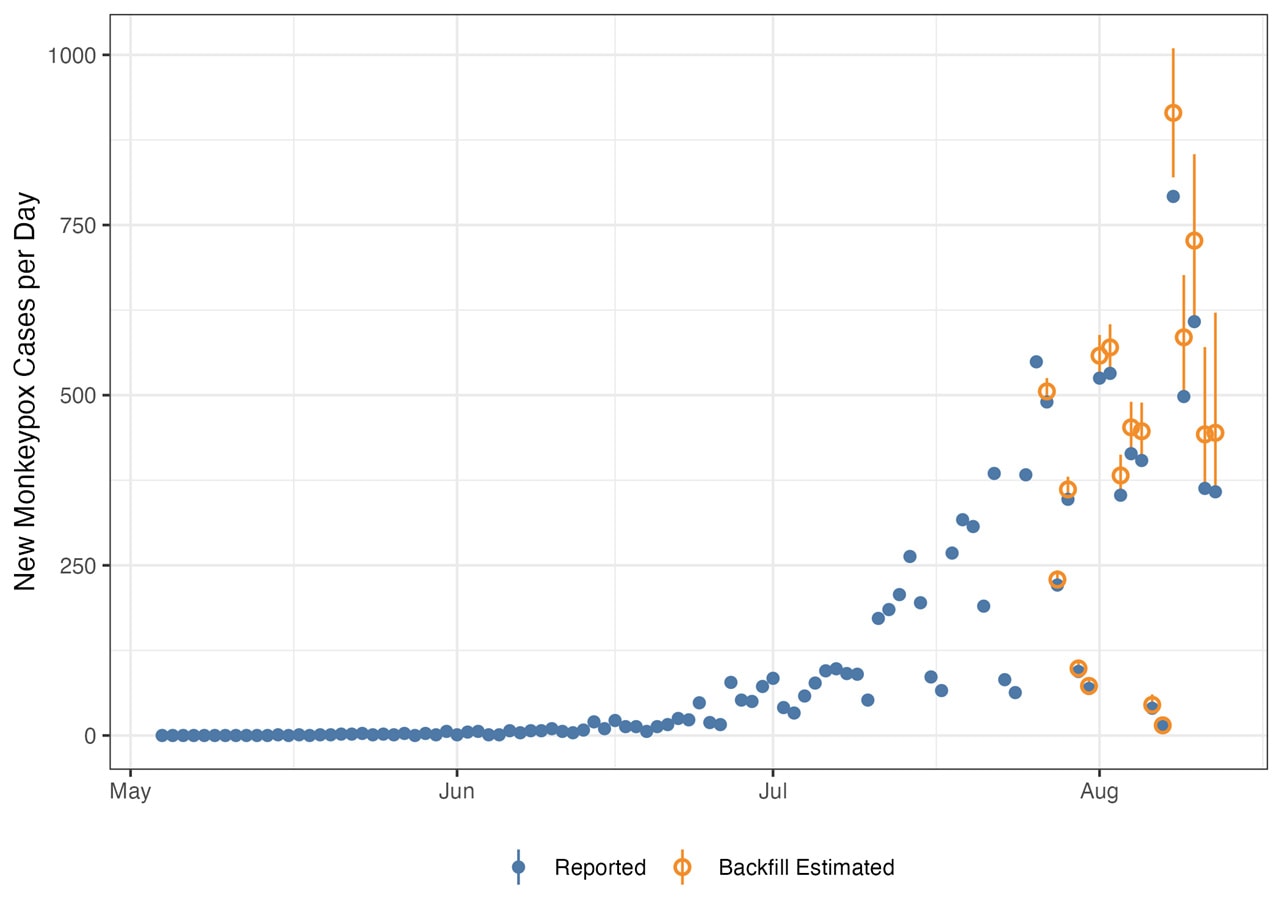
Figure 9. Daily monkeypox cases reported in the United States (blue) with estimated number of cases adjusted for reporting delays (orange). Orange ranges indicate 95% credible intervals for the backfilled data. Data as of August 16, 2022.
We have observed heterogeneity in growth rates across states and regions of the United States (Figures 10, 12). While many states with larger outbreaks have slowing growth, some jurisdictions are experiencing accelerating growth, for example Indiana, Virginia, Massachusetts, and the District of Columbia, as shown in Figure 11 below. Across U.S. Department of Health and Human Services (HHS) regions, as shown in Figure 13, Region 1 has shown the highest growth rate, while Region 2 exhibited faster growth early in the outbreak, which has since slowed.
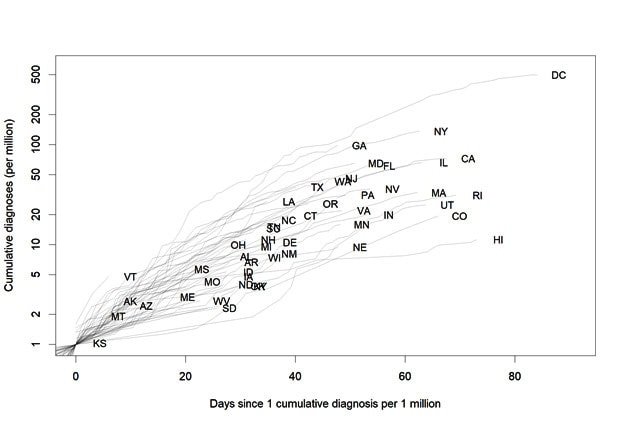
Figure 10. Cumulative monkeypox cases per million by state, by day since 1 cumulative diagnosis per million population using data as of August 16, 2022.
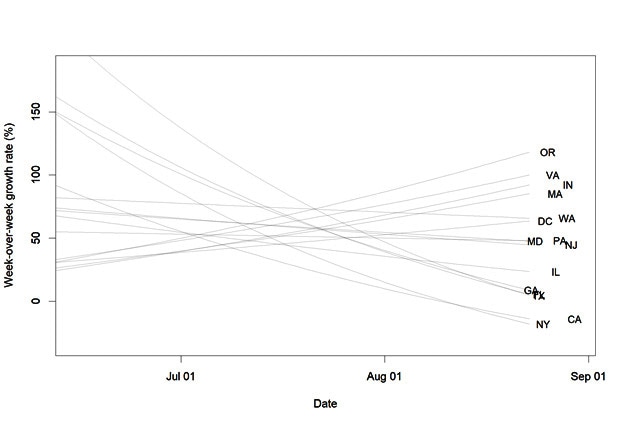
Figure 11. Modelled week-over-week growth rates for states, excluding states with fewer than 100 diagnoses by August 16, 2022, due to instability in estimates from small numbers.
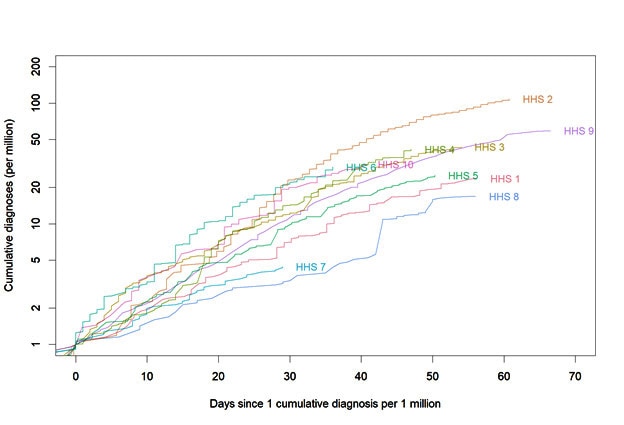
Figure 12. Cumulative monkeypox cases per million for HHS regions of the United States, by day since 1 cumulative diagnosis per million population using data as of August 16, 2022.
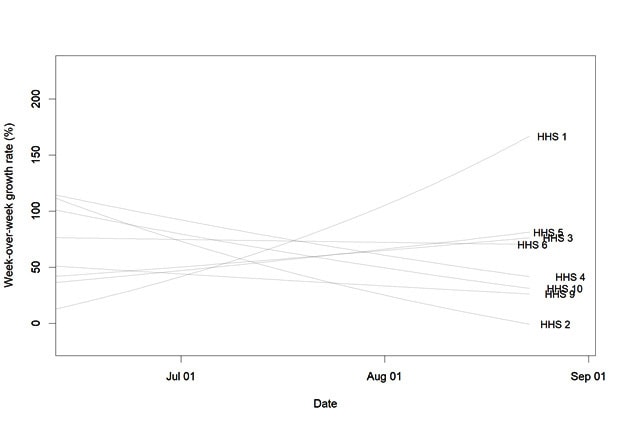
Figure 13. Modelled week-over-week growth rate for HHS regions of the United States, excluding regions with fewer than 200 diagnoses by August 16, 2022, due to instability in estimates from small numbers.
Potential Future Outbreak Trajectory
Likely Short-Term Scenarios
We believe the most likely outbreak growth scenarios for the United States over the next two to four weeks are the following:
- Continued exponential growth with daily cases rising significantly
- Very slow or zero growth with daily cases rising slowly or roughly plateauing
- Daily cases declining significantly
Among these scenarios, we assess the monkeypox outbreak in the United States will most likely continue to grow very slowly over the next two to four weeks, likely with a declining growth rate. We have low confidence in this assessment. Given the estimated doubling time above, in this scenario cumulative cases could double to approximately 35,000 over the next month.
Our rationale for this assessment is that, based on the current growth rate, we expect some level of continued growth over this short time horizon. However, we note daily cases are declining in several large U.S. states and European countries and that our growth rate estimates are based on trends observed through mid-August, so the outbreak growth rate could slow further in the coming weeks. Because the causes of cases slowing in U.S. and other countries are not well understood and patterns have not been uniform, we cannot predict the timing and precise trajectory of case declines in the United States.
Longer-Term Considerations
We have even greater uncertainty over the longer-term trajectory for the monkeypox outbreak in the United States, owing to a range of unknowns including the following:
- Detailed characteristics of sexual networks involving gay, bisexual, and other men who have sex with men (MSM) and the impact of behavior change on outbreak trajectory among MSM
- Impact of vaccines and other interventions on outbreak trajectory among MSM
- Vaccine effectiveness for infection prevention, versus minimizing severe disease
- Potential for sustained transmission among non-MSM populations and via non-sexual routes, particularly in special populations such as:
- Highly connected heterosexual transmission networks
- Congregate settings such as daycares, schools, colleges, and prisons
- Extent and impact of asymptomatic spread of infection
- Potential impact of viral mutation on transmission dynamics
Our current assessment for the most likely longer-term scenario is that the outbreak will remain concentrated in MSM, with cases increasing over the coming weeks, but falling significantly over the next several months. We have low confidence in this assessment. We note that low-level transmission could continue indefinitely, and the cumulative number of cases that could occur among MSM is unknown.
We believe this scenario is most likely because the outbreak to date has remained concentrated among MSM, and monkeypox spread in other subpopulations has so far not been intensive, although the declining portion of cases reporting recent man-to-man sexual contact in the United States (Figure 4) and among MSM globally could signal potential for non-sexual spread in other sub-populations. We also make this assessment assuming monkeypox infection provides strong immunity to subsequent infection, as is the case for other orthopoxviruses, which will eventually lead to a depletion of susceptible individuals among populations disproportionately affected.
We note that mathematical models have shown considerable variability in predicted levels of cumulative incidence among MSM (Endo et al. 2022; van Dijck et al. 2022; personal communication and internal modeling results). The duration of the intense transmission phase for this outbreak is also highly uncertain. If spread is concentrated among a fixed subset of MSM with the highest numbers of sexual partners, and vaccination is well targeted toward this exposure group and strongly protective against infection, a more rapid decline and lower cumulative number of cases could occur (Badham and Stocker 2010). If, however, spread is less concentrated among a fixed subset of MSM with the highest numbers of partners, or vaccination and behavior change only gradually slow spread, a cumulatively high number of MSM infections and a long outbreak tail are possible.
Given our uncertainty over how the monkeypox outbreak may unfold in the United States, we acknowledge several other less likely but possible scenarios that could transpire, some of which could require major shifts in our outbreak response posture.
Containment: The monkeypox outbreak could be contained in the United States sometime over the next 6 months, with domestic transmission eliminated. The United States would still likely experience imported cases with potential for some additional onward spread. This scenario would be most likely to occur if monkeypox is and remains concentrated in a subset of MSM with the highest number of sexual partners, and the vaccine targets this exposure group and prevents infection, both factors which would cause faster declines in transmission.
Acceleration: The monkeypox outbreak could accelerate in the United States over the next several months and affect an increasingly wider segment of the United States population. This scenario is most likely to transpire if transmission occurs more readily than expected among non-MSM populations including potentially among highly connected heterosexual networks or by non-sexual routes, including in congregate or other special settings such as daycares.
Establishment in animal populations: There is a possibility that the monkeypox virus establishes itself in one or more animal populations in the United States, although this scenario would require that a suitable reservoir animal host exists, which is currently unknown. If such a reservoir host exists, this scenario could become more likely as case numbers rise. Several animal species in North America, both wild and domestic, may be susceptible to monkeypox infection and may be able to transmit the virus to other animals or species.
1In this report, we use the following definitions for confidence levels associated with analytic judgments: High confidence judgments are based on high-quality information from multiple sources, although such judgments are not a certainty and still carry a risk of being wrong. Moderate confidence judgments are based on credibly sourced and plausible information, but the information is not of sufficient quality or corroboration to warrant a high level of confidence. Low confidence judgments are based on information that is fragmented or poorly corroborated or upon data sources for which there are significant concerns or problems.
Special Studies
Social and Behavioral Health
In an online survey of gay, bisexual, and other men who have sex with men conducted during August 5-15, respondents reported changing their behavior because of the monkeypox outbreak. Among respondents, 48% reported reducing their number of sex partners, 50% reported reducing one-time sexual encounters, and 50% reported reducing sex with partners met on dating apps or at sex venues.
Source: American Men’s Internet Survey, 2022 Monkeypox Supplemental Survey. https://emoryamis.org/
Ongoing Investigations
CDC has initiated several studies to answer key unknowns related to monkeypox, including seroprevalence studies, clinical studies, and lab studies. Other studies will be included in this report once staff needs are allocated and protocols for investigations are approved.
Serosurvey
Investigation: Three-week prospective study with certain public health clinics in San Francisco that predominantly care for MSM. The study involves collection of serum samples and answers to specific questions about exposures and behaviors among a racially and ethnically diverse population with a broad range of socio-economic status. The goal is to determine the prevalence of monkeypox.
Collaborating Institutions: CDC, San Francisco Department of Public Health
Status: Serum collection is complete. The laboratory has tested 181 serum samples and found 4 of these had significant IgG positive results, with 2 of those 4 IgM positive. One individual was likely IgG positive due to childhood smallpox vaccination. A second had no history of rash like disease; this individual was IgM negative but also less than age 50 and no reported smallpox vaccination history. The source of this antibody response is uncertain. The final two IgM positive results were reported in individuals which had a history of rash like disease but were not tested by PCR for monkeypox virus (MPXV) or orthopoxvirus; these were likely previously undiagnosed MPXV infections. The study has concluded enrollment and we anticipate ~30-50 additional serum specimens to be received and tested.
Testing of residual nucleic acid material
Investigation: Banked nucleic acid and ongoing (prospective) collection from a commercial laboratory. These residual specimens are from clinics across the country and were targeted based on ICD-10 codes relevant to outbreak.
Collaborating Institutions: CDC, HealthTrackRX
Status: Two out of 213 specimens (collected from late May-July) tested positive for MPXV DNA at the CDC. 421 additional specimens collected from late July-middle of August were screened by the company and 36 tested positive for MPXV. These specimens are being sent to the CDC for confirmatory testing. All 38 MPXV positive specimens were from male patients. Additional analysis of the zip codes and ICD-10 codes are currently underway and a manuscript to describe results is being planned.
Presence of MPX DNA in throat, rectal swabs, and blood and immune response against the JYNNEOS vaccine among persons at elevated risk of MPX exposure but without lesions
Investigation: To determine if MPX DNA can be detected in throat, rectal swabs, and/or blood prior to lesion/rash presence among persons at elevated risk of MPX exposure, i.e., persons presenting for post-exposure prophylaxis (PEP) or PEP++ (people with certain risk factors and recent experiences that might make them more likely to have been recently exposed to monkeypox). To assess the immune response against JYNNEOS from the US population after at least one dose of vaccine.
Collaborating Institutions: CDC, Washington D.C. PHL
Status: Collection is ongoing. Initial specimens have arrived at CDC.
Technical Assistance
Investigation: Three-to-four-week technical assistance to improve understanding of monkeypox cases through network analysis and characterizing transmission dynamics, including processing through detailed partner services/contact tracing data to better understand secondary attack rates, delays between exposure and symptom onset, characterization exposure types, and identifying common venues associated with transmission.
Collaborating Institutions: CDC, DC Department of Health
Status: Ongoing virtually since July 12, 2022.
Priority Research Topics
The following is a list of topics that CDC is interested in studying in more depth given resources to do so. For some of these topics, CDC is planning research or has begun studying some aspect of the topic, including for particular geographic areas or time periods, however the broader topics remain priorities for future investigation.
Gaps and Potential Areas of Focus:
- Medical Countermeasure Effectiveness
- Effectiveness of vaccine to prevent or ameliorate disease when administered as pre- or post-exposure prophylaxis
- Effectiveness of antivirals to prevent disease if given as postexposure prophylaxis or to improve clinical outcomes when given for treatment (e.g., prevention of severe disease/complications, decreased lesion burden, hastening of lesion resolution)
- Decentralized trials, remote case monitoring, and improved access to interventions
Comparing effectiveness and safety of 1 vs. 2 dose vaccine regimens; possible use of “ring” vaccine strategy - Novel methods for evaluating medical countermeasures during an outbreak
- Epidemiology, pathogenesis, and clinical characteristics
- Modeling transmission dynamics
- Clinical presentation (particularly of the rash), risk factors, and associated outcomes, as well as similarities and differences in non-US cases
- Disease pathogenesis and relationship to clinical presentation and transmission route
- One Health – transmission to animals, including pets, domestic animals, and wildlife
- Social and behavioral factors associated with transmission
- Diagnostic Tools and Surveillance
Validation and strategic deployment of pre-existing and novel diagnostics- Viral detection across specimen types
- Levels of undetected transmission, especially in populations and regions with less access to MPX testing
- Serosurveys and improved serologic assays
- Community and wastewater surveillance
- Sequencing to identify changes in circulating viruses
- Sensitivity analysis to test for anti-viral resistant strains
- Communications
- Understand knowledge, attitudes, and practices of key communities and impacted populations.
- Monitor mis/disinformation and implement actions to address
- Health Equity and Stigma Reduction during Public Health Emergency
- Equitably balancing resources for outbreak response in non-endemic countries with control in endemic countries (e.g., access and distribution of vaccines and therapeutics)
- Evaluate the equitable distribution of testing, treatment, prevention measures and other resources; and evaluate measures to improve access for underserved groups
- Social and Behavioral Science
- Gather qualitative and quantitative data directly from affected communities to guide implementation of testing, vaccination, and other prevention strategies.
Limitations of the Report
All data are preliminary and may change as additional data are obtained.
Due to the limited availability of detailed data from case reports and contact tracing, we continue to have knowledge and data gaps related to monkeypox transmission dynamics, case ascertainment, clinical characteristics, and other key features of this outbreak. CDC is working with state, local, tribal, and territorial partners, as well as clinical and laboratory partners, on obtaining improved case and contact tracing data to better understand this rapidly changing outbreak. CDC is also working with other federal partners and academic partners to improve our ability to respond to this outbreak.
Use of trade names and commercial sources is for identification only and does not imply endorsement by HHS or CDC.
References to non-CDC sites on the Internet are provided as a service to readers and do not constitute or imply endorsement of these organizations or their programs by CDC or the U.S. Department of Health and Human Services. CDC is not responsible for the content of pages found at these sites.
Acknowledgements
Authors of and contributors to this report are members of CDC’s 2022 Multi-National Monkeypox Outbreak Response and the Center for Forecasting and Outbreak Analytics.
References to non-CDC sites are provided as a service and do not constitute or imply endorsement of these organizations or their programs by CDC or the U.S. Department of Health and Human Services. CDC is not responsible for the content of pages found at these sites. URL addresses listed were current as of the date of publication.