Notes from the Field: Legionnaires Disease in a U.S. Traveler After Staying in a Private Vacation Rental House in the U.S. Virgin Islands — United States, February 2022
Weekly / May 19, 2023 / 72(20);564–565
Valerie V. Mac, PhD1,2,*; Katie Labgold, PhD1,2,*; Heidi L. Moline, MD1,3; Jessica C. Smith, MPH3; Jamaal Carroll2; Nakia Clemmons, MPH4; Chris Edens, PhD3; Brett Ellis, PhD2; Cosme Harrison, MPH2; Kelley C. Henderson, PhD3; Maliha K. Ishaq, MPH4; Natalia A. Kozak-Muiznieks, PhD3; Jasen Kunz, MPH5; Marlon Lawrence, PhD2; Claressa E. Lucas, PhD3; Heather L. Walker, DVM3; Melisa J. Willby, PhD3; Esther M. Ellis, PhD2 (View author affiliations)
View suggested citationOn February 1, 2022, the U.S. Virgin Islands (USVI) Department of Health (VIDOH) was notified of a confirmed case of Legionnaires disease in an adult U.S. resident (Figure). The patient, a man aged 55 years, returned to his U.S. state of residence from leisure travel in USVI on January 22 and developed a cough, shortness of breath, and fatigue on January 23. On January 29, he was hospitalized for shortness of breath and received a positive SARS-CoV-2 test result at admission. The combination of the patient’s symptoms and recent travel history prompted administration of a urinary antigen test (UAT) for Legionnaires disease specific to Legionella pneumophila serogroup 1 (Lp1); a positive result was returned on January 31. Inpatient treatment administered for COVID-19 pneumonia and Legionnaires disease included remdesivir, oral levofloxacin, oral and intravenous steroid therapy, and as-needed use of a bronchodilator inhaler and an expectorant. Remdesivir was discontinued during inpatient treatment because of elevated liver enzymes. The patient recovered and was discharged on February 2.
Interviews with the patient indicated that he had stayed at a privately owned vacation rental property during January 15–22. As is the case with most USVI residential properties, rainwater collected into a cistern under the home was the property’s potable water source (1), which supplies water for drinking, bathing, a swimming pool, and two hot tubs. Water is heated by a solar water heater, which does not allow for water temperature control. The property owner reported that no routine chlorine treatment or water filtration systems were used to maintain the potable water source during the patient’s stay.
On February 3, VIDOH requested assistance from CDC’s Legionella program to conduct environmental sampling and testing for Legionella bacteria. Twenty-five bulk water, swab, and cartridge filter samples were collected at the property. L. pneumophila nonserogroup 1 was detected in 11 locations, including one hot tub cartridge filter, all showers, the two sampled bathroom sinks, and two critical control points: the cistern and solar water heater. Lp1, the only strain detectable by UAT, was not detected in environmental samples.
No respiratory specimen was collected from the patient, which would have been needed to detect and directly link an L. pneumophila nonserogroup 1 infection to the property; however, L. pneumophila of any serogroup can infect humans, and any environment hospitable to L. pneumophila nonserogroup 1 is also hospitable to Lp1 (2,3). Thus, even without a direct linkage of the L. pneumophila strain detected in the patient to the property, the high prevalence (44%) of samples positive for L. pneumophila nonserogroup 1 in environmental samples collected at a single time point revealed favorable environmental conditions for widespread, uncontrolled Legionella growth of multiple serogroups at the property.
Given the detection of L. pneumophila nonserogroup 1 at multiple sampling locations on the same day, VIDOH provided recommendations to disinfect the property’s plumbing system and implement water system maintenance (installing a multistage ultraviolet filtration system and performing routine chlorination). The property owner completed remediation recommendations during February 5–6. However, a request by VIDOH for retesting in September was declined by the property owner, highlighting a gap in VIDOH’s ability to evaluate maintenance effectiveness.
Vacation rental properties represent a growing proportion of the accommodation types identified in U.S. travel-associated Legionnaires disease cases and outbreaks (4). In resource-constrained settings such as USVI, commonly recommended water quality maintenance strategies (e.g., controlled temperature water heating and multistage water filtration) are not easily implemented, highlighting territory-specific potable water maintenance and testing needs. In light of these maintenance challenges, and that an estimated 90% of USVI residences rely on cisterns as their potable water source, the environmental assessment and sampling results of this investigation underscore the potential for undetected Legionnaires disease cases among USVI residents and travelers (1). Patients with clinical signs consistent with Legionnaires disease such as shortness of breath, cough, fatigue, and a history of travel to USVI should be tested for Legionella, even if, as was the case for the patient described in this report, another respiratory virus test result is positive. When cases are identified, environmental assessment and sampling, remediation strategy implementation, and timely postremediation testing are central to ensuring treatment success. VIDOH continues to work with CDC’s Legionella program to improve territory Legionnaires disease case surveillance, Legionella environmental assessment and sampling practices, and educational outreach to vacation rental owners.
Corresponding author: Katie Labgold, tqo3@cdc.gov.
1Epidemic Intelligence Service, CDC; 2U.S. Virgin Islands Department of Health; 3Division of Bacterial Diseases, National Center for Immunization and Respiratory Diseases, CDC; 4Division of Environmental Health Science and Practice, National Center for Environmental Health, CDC; 5Division of Foodborne, Waterborne, and Environmental Diseases, National Center for Emerging and Zoonotic Infectious Diseases, CDC.
All authors have completed and submitted the International Committee of Medical Journal Editors form for disclosure of potential conflicts of interest. No potential conflicts of interest were disclosed.
* These authors have contributed equally to this report.
References
- USVI Hurricane Recovery and Resilience Task Force. Report 2018. Charlotte Amelie, USVI: USVI Hurricane Recovery and Resilience Task Force; 2018. https://cfvi.net/wp-content/uploads/2019/05/USVI_HurricaneRecoveryTaskforceReport_DIGITAL.pdf
- Nazarian EJ, De Jesus M, Musser KA. Legionella [Chapter 90]. In: Tang Y, Sussman M, Liu D, Poxton I, Schwartzman J, eds. Molecular medical microbiology. 2nd ed. Cambridge, MA: Academic Press; 2015.
- Yu VL, Plouffe JF, Pastoris MC, et al. Distribution of Legionella species and serogroups isolated by culture in patients with sporadic community-acquired legionellosis: an international collaborative survey. J Infect Dis 2002;186:127–8 https://doi.org/10.1086/341087 PMID:12089674
- CDC. Legionnaires’ disease prevention: providing a home for guests, not Legionella. Atlanta, GA: US Department of Health and Human Services, CDC; 2022. https://www.cdc.gov/legionella/downloads/fs-legionnairesvacationrental-508.pdf
 FIGURE. Time line of patient travel, illness onset, diagnosis, and environmental remediation for a case of Legionnaires disease in a U.S. traveler visiting the U.S. Virgin Islands — United States, January–February 2022
FIGURE. Time line of patient travel, illness onset, diagnosis, and environmental remediation for a case of Legionnaires disease in a U.S. traveler visiting the U.S. Virgin Islands — United States, January–February 2022
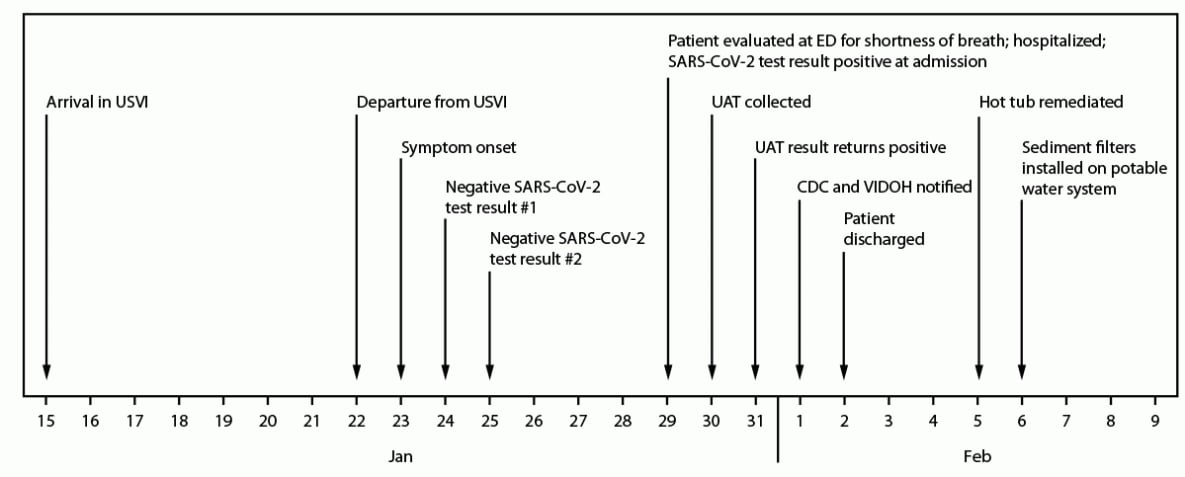
Abbreviations: ED = emergency department; UAT = urinary antigen test; USVI = U.S. Virgin Islands; VIDOH = Virgin Islands Department of Health.
Suggested citation for this article: Mac VV, Labgold K, Moline HL, et al. Notes from the Field: Legionnaires Disease in a U.S. Traveler After Staying in a Private Vacation Rental House in the U.S. Virgin Islands — United States, February 2022. MMWR Morb Mortal Wkly Rep 2023;72:564–565. DOI: http://dx.doi.org/10.15585/mmwr.mm7220a5.
MMWR and Morbidity and Mortality Weekly Report are service marks of the U.S. Department of Health and Human Services.
Use of trade names and commercial sources is for identification only and does not imply endorsement by the U.S. Department of
Health and Human Services.
References to non-CDC sites on the Internet are
provided as a service to MMWR readers and do not constitute or imply
endorsement of these organizations or their programs by CDC or the U.S.
Department of Health and Human Services. CDC is not responsible for the content
of pages found at these sites. URL addresses listed in MMWR were current as of
the date of publication.
All HTML versions of MMWR articles are generated from final proofs through an automated process. This conversion might result in character translation or format errors in the HTML version. Users are referred to the electronic PDF version (https://www.cdc.gov/mmwr) and/or the original MMWR paper copy for printable versions of official text, figures, and tables.
Questions or messages regarding errors in formatting should be addressed to mmwrq@cdc.gov.