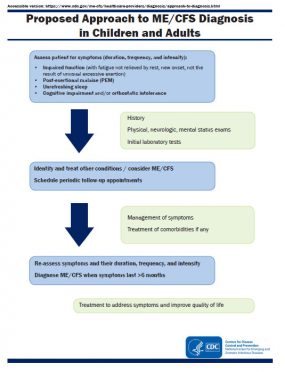
Proposed Approach to ME/CFS Diagnosis in Children and Adults
Assess patient for symptoms (duration, frequency, and intensity):
- Impaired function (with fatigue not relieved by rest, new onset, not the result of unusual excessive exertion)
- Post-exertional malaise (PEM)
- Unrefreshing sleep
- Cognitive impairment and/or orthostatic intolerance

History
Physical, neurologic, mental status exams
Initial laboratory tests
Identify and treat other conditions / consider ME/CFS
Schedule periodic follow-up appointments

Management of symptoms
Treatment of comorbidities if any
Re-assess symptoms and their duration, frequency, and intensity
Diagnose ME/CFS when symptoms last >6 months
Treatment to address symptoms and improve quality of life
The proposed approach to diagnosis of ME/CFS is outlined in the figure. When a patient presents with impaired function along with fatigue, PEM, unrefreshing sleep, and either one or both cognitive impairment or orthostatic intolerance, a thorough history, physical (including neurological) and mental health exam, and laboratory testing should be performed to evaluate for other conditions that may explain symptoms. During the evaluation period, healthcare providers can begin considering ME/CFS and schedule periodic follow-up appointments. The symptoms should be addressed and managed and any identified comorbidities treated to improve quality of life.
If symptoms persist for six months or longer, ME/CFS is diagnosed. Patients with ME/CFS should be re-evaluated periodically. Routine age-appropriate health monitoring/screening is important and should continue. In addition, healthcare providers should remain vigilant for illnesses that have symptoms similar to ME/CFS.
Getting a detailed medical history as well as social and occupational histories is critical to assessing the effects of the illness on patient’s daily functioning. PEM may be delayed after onset of other symptoms, and some patients may not recognize PEM at the start of their illnesses.
Healthcare providers can use questions similar to those below to elicit an accurate description of symptoms, including PEM and fatigue:
- What are you able to do now? How does it compare to what you were able to do before you became sick?
- How long have you felt this way?
- How do you feel after sleeping or resting?
- What makes you feel worse? What helps you feel better?
- What happens when you try to push to do activities that are now hard for you?
- Are you able to think as clearly as you did before becoming ill?
- What symptoms keep you from doing what you need or want to do?
- What symptoms do you have when you stand or sit upright?
- How much activity, either physical or mental, does it take for you to feel ill?
- How long does it take for you to feel better after such exertion?
- What types of activities do you now avoid because of what will happen if you do them?
- Do you ever feel dizzy or lightheaded? Have you been falling more often than before? Do you feel worse waiting in line, standing for more than 5 minutes, or when in warm environments?
Consider asking patients to document their activities and symptoms for a couple of weeks in a diary.
For children, the questions may need to be adapted and parents may be an important resource. Depending on the age of the child, the questions might be asked of the patient, parent/guardian, or both (together or independently).
If a patient has had impairment in function with severe fatigue for 6 months or longer but does not have all the required symptoms, the healthcare provider may make a diagnosis of idiopathic fatigue (fatigue with an unknown cause). In practice, patients with idiopathic fatigue are managed like patients with ME/CFS.
Disclaimer: The content of this ME/CFS website is for informational purposes only and does not represent a federal guideline or recommendation for the treatment of ME/CFS. The information provided on this website is not intended to be a substitute for the medical judgment of the healthcare provider and does not indicate an exclusive course of action or treatment.