About
CDC supports behavioral, biomedical, and structural interventions from the Compendium of Evidence-Based Interventions and Best Practices for HIV Prevention as well as public health strategies and social marketing campaigns to end the HIV epidemic. This page provides information and materials for CDC-supported interventions and strategies categorized by the Ending the HIV Epidemic in the U.S. pillars.

Diagnose
Great strides have been in made in HIV prevention, but about 1 in 8 (13%) of the estimated 1.2 million people with HIV in the United States still don't know they have HIV. Resources are available for the HIV prevention workforce to increase its capacity to test for HIV according to CDC guidelines and diagnose all people with HIV.
About HIV self-testing programs
HIVST programs are a way to reach more people who have HIV but are not yet diagnosed and represent a step forward to empowering individuals, diagnosing hard-to-reach populations earlier before they become sick, and bringing linkage-to-care services closer to populations where traditional testing locations are not easily accessible. While HIV self-tests are available for retail purchase by consumers, the CDC encourages health departments and CBOs to consider HIVST programs as an additional testing strategy to reach persons most affected by HIV.
A Rapid Self-Test is done entirely at home or in another private location. You can buy OraQuick, the only FDA-approved rapid self-test kit, at a pharmacy or online. This test can provide results within 20 minutes.
HIV self-testing training
Learning objectives
- Explain the intent of HIV self-testing as an HIV prevention strategy.
- Identify two (2) advantages of HIV self-testing for programs.
- Identify two (2) challenges of HIV self-testing for programs.
- Identify the key considerations for developing a framework for your HIV self-testing program.
- Determine strategies for engaging priority populations for HIV self-testing services.
- Identify key components of monitoring and evaluation plans for HIV self-testing programs.
This training has 1 component:
- 1-hour eLearning module
To access eLearning modules:
- Log-in to CDC TRAIN and access the HIV CBA Training Plan (step-by-step instructions are available).
- Select the module you wish to take.
- Launch the module or save the module for later.
If you have questions or need additional assistance, please contact HIVCBA@cdc.gov.
HIV self-testing program components
Program components to consider when building or strengthening an HIV self-testing program include:
- Priority population
- Methods of distribution
- Developing marketing materials
- Eligibility criteria
- Obtaining results
- Ways to incentivize the service
- Type of test
- Linkage to care
- Additional materials
- Requesting tests
- Data monitoring
- Training of staff
Technical assistance is available for the implementation of HIVST programs is available.
Implementation and marketing materials
Additional resources provided below may be helpful if you are considering offering HIVST programs:
- NASTAD HIV self-testing toolkit
- Let's Stop HIV Together self-testing page
- A Summary of HIV Self-Testing Program Models and Lessons Learned: In an effort to document HIVST program models in the United States, two capacity building assistance (CBA) providers funded by CDC, Denver Prevention Training Center and Washington University in St. Louis, contacted CDC-funded health departments and CBOs that were conducting HIVST. Between July and September 2020, the CBA providers had telephone discussions about program implementation with 42 agencies (23 state health departments and 19 CBOs) and collected HIVST standard operating procedures and training materials. Conversations covered topics such as: if/how agencies screen for eligibility; type of HIV test used; distribution methods; follow-up and linkage to prevention/care resources; data collection and management; and incentives. The two CBA providers summarized the discussions to produce this executive summary and a descriptive table.
- OraQuick HIV self-test: OraSure Technologies provides detailed information about their HIV self-test product, OraQuick HIV Self-Test. On this site, consumers can find information about the product, written and video instructions of how to use the test, help on how to interpret a result, and the 24/7 customer support phone number.
About HIV testing in nonclinical settings
HIV testing in nonclinical settings is a key public health strategy under the Ending the HIV Epidemic in the U.S. (EHE) Diagnose Pillar. A nonclinical setting is defined as a location not offering routine HIV treatment. Examples of nonclinical settings for HIV testing may include community-based organizations (CBOs), retail and community pharmacies, mobile units, and places a population of interest congregates and is accessible (e.g., parks, bridge underpasses, bars, community festivals).
Nonclinical settings should be easy to access and useful for reaching people who might not be willing or able to access medical services regularly. They typically provide same-day rapid HIV testing results and support based on the wholistic needs and desires of the individual.
About the HIV testing in nonclinical settings training
HIV Testing in Nonclinical Settings is the Centers for Disease Control and Prevention's (CDC's) latest HIV testing training for nonclinical settings. This training is influenced by CDC's guidance Implementing HIV Testing in Nonclinical Settings: A Guide For HIV Testing Providers (2016), as well as advancements in the field since its publish date. Key influences on this curriculum have been shifts in HIV prevention, care, and treatment that have occurred since the previous training called Fundamentals of HIV Prevention Counseling training, and the policies that followed.
The HIV Testing in Nonclinical Settings course has a streamlined Six-Step Protocol with greater emphasis on meeting a client where they are, sex-positive messages, retesting recommendations, and active referrals based on current circumstances.
This course is being offered virtually, with live instructors and utilizes a variety of adult learning methodologies inclusive of lectures, group discussions, video forums, and role-plays.
About the Fundamentals of Rapid HIV Testing training
The Fundamentals of Rapid HIV Testing E-learning course provides foundational training to rapid HIV testing staff working in nonclinical community-based settings such as health departments, community-based organizations, and other nonclinical HIV testing sites.
This course prepares rapid HIV testing staff to conduct the key steps of rapid HIV testing: setting up workspace, conducting the rapid HIV test, preparing clients for the test and delivering test results, and conducting quality assurance activities.
Trainings
HIV Testing in Nonclinical Settings training has one component:
- 3-day (5 hours per day) virtual, instructor-led training; or
- 2 days (8 hours per day) in a live classroom setting
Fundamentals of Rapid HIV Testing training has one component:
- 5-module self-paced eLearning training
To view and register for scheduled instructor-led virtual or classroom training:
- Access the National HIV Classroom Learning Center training calendar hosted on Cicatelli Associates, Inc.'s (CAI's) website.
- Pre-register for your selected course via the link provided in the training calendar.
- Complete your registration on CDC TRAIN as directed when you receive an email from the National HIV Classroom Learning Center. You must join the HIV CBA Learning Group and locate the HIV CBA Training Plan in order to complete your CDC TRAIN registration for a specific classroom training session (step-by-step instructions are available).
To access eLearning training:
- Log-in to CDC TRAIN and access the HIV CBA Training Plan (step-by-step instructions are available).
- Select the module you wish to take.
- Launch the module or save the module for later.
To request technical assistance or that a training session be scheduled:
- CDC's directly funded health department and CBO partners may request delivery of a CDC-supported training or technical assistance by submitting a request in the CBA Tracking System.
- Organizations not directly funded by CDC may contact their local health department for assistance in submitting a training or technical assistance request.
If you have questions or need additional assistance, please contact HIVCBA@cdc.gov.
Implementation and marketing materials
The materials and resources listed below support the implementation and/or marketing of HIV Testing in Nonclinical Settings by health departments, community-based organizations, and health care or other organizations. The resources are evidence-based and designed for cost-effective, scalable implementation.
About HIV testing in retail pharmacies
The accessibility of pharmacies for HIV testing presents a unique opportunity for pharmacists to contribute to the identification of undiagnosed HIV. It is estimated that 70% of rural consumers live within 15 miles of a pharmacy, and 90% of urban consumers live within 2 miles of a pharmacy. A Centers for Disease Control and Prevention (CDC)-funded feasibility study offering rapid, point-of-care testing in community pharmacies and retail clinics stated: "Pharmacies and retail clinics represent a vast, largely untapped potential for the delivery of HIV testing in settings that are more accessible and, for some people, less stigmatizing than traditional testing."
Based on these findings, CDC developed the HIV Testing in Retail Pharmacies training that reflects scientific advances and evidence-informed updates as expressed in CDC's guidance: Implementing HIV Testing in Nonclinical Settings: A Guide For HIV Testing Providers (2016).
Note: This training does not teach participants how to collect blood or oral samples
HIV testing in retail pharmacies training
This training has two components:
- 1-hour eLearning pre-course module
- 1-day (5 hour) virtual, instructor-led training
To view and register for scheduled virtual, instructor-led trainings:
- Access the National HIV Classroom Learning Center training calendar hosted on Cicatelli Associates, Inc.'s (CAI's) website.
- Pre-register for your selected course via the link provided in the training calendar.
- Complete your registration on CDC TRAIN as directed when you receive an email from the National HIV Classroom Learning Center. You must join the HIV CBA Learning Group and locate the HIV CBA Training Plan in order to complete your CDC TRAIN registration for a specific classroom training session (step-by-step instructions are available).
To access eLearning modules, including training prerequisite courses:
- Log-in to CDC TRAIN and access the HIV CBA Training Plan (step-by-step instructions are available).
- Select the module you wish to take.
- Launch the module or save the module for later.
To request technical assistance or that a training session be scheduled:
- CDC's directly funded health department and CBO partners may request delivery of a CDC-supported training and technical assistance by submitting a request in the CBA Tracking System.
- Organizations not directly funded by CDC may contact their local health department for assistance in submitting a training or technical assistance request.
If you have questions or need additional assistance, please contact HIVCBA@cdc.gov.
Implementation and marketing materials
The materials and resources listed below support the implementation and/or marketing of HIV Testing in Retail Pharmacies by health departments, community-based organizations, and health care or other organizations. The resources are evidence-based and designed for cost-effective, scalable implementation.
About partner services
DIS are usually health department personnel who are specifically trained to provide Partner Services. Some health departments, however, use different titles for persons providing partner services. In addition, in certain jurisdictions, other persons (e.g., HIV counselors or clinicians), either inside or outside of the health department, provide certain or all elements of partner services.
An important job of Partner Services is partner notification, a process through which infected persons are interviewed to elicit information about their partners, who can then be confidentially notified of their possible exposure or potential risk. Other roles of partner services include prevention counseling, testing for HIV and other types of STDs (not necessarily limited to syphilis, gonorrhea, and chlamydial infection), hepatitis screening and vaccination, treatment or linkage to medical care, linkage or referral to other prevention services, and linkage or referral to other services (e.g., reproductive health services, prenatal care, substance use treatment, social support, housing assistance, legal services, and mental health services).
CDC strongly recommends that all persons with newly diagnosed or reported HIV infection or early syphilis receive Partner Services with active health department involvement. Persons diagnosed with gonorrhea or chlamydial infection are also suitable candidates for Partner Services; however, disease burden and resource limitations may prevent direct health department involvement.
Core elements
The following serve as the foundation for providing partner services:
- Client centered.
- Confidential.
- Voluntary and non-coercive.
- Free.
- Evidence based.
- Culturally, linguistically, and developmentally appropriate.
- Accessible and available to all.
- Comprehensive and integrative.
Passport to Partner Services: Principles, Practices, and Pathways to Disease Intervention (3PDI)
Passport to Partner Services has been the comprehensive national curriculum that provides training for DIS and other Partner Services providers. All Passport to Partner Services modules are available on CDC TRAIN. To access these modules, log into CDC TRAIN and search "Passport to Partner Services" or enter course ID# 4299. The instructor-led Passport to Partner Services course is not currently being offered.
In 2022, Passport to Partner Services curriculum will be replaced by the Principles, Practices, and Pathways to Disease Intervention (3PDI) modules. DIS and others who perform partner services will need to complete the 3PDI training to become certified disease investigation providers. Watch for announcements on CDC TRAIN and through other CDC announcements for more information.
To request technical assistance:
- CDC's directly funded health department and CBO partners may request technical assistance by submitting a request in the CBA Tracking System.
- Organizations not directly funded by CDC may contact their local health department for assistance in submitting a request.
If you have questions or need additional assistance, please contact HIVCBA@cdc.gov.
References
On October 31, 2008, CDC issued the Recommendations for Partner Services Programs for HIV Infection, Syphilis, Gonorrhea, and Chlamydial Infection to guide the delivery of Partner Services.
- CDC. Recommendations for partner services programs for HIV infection, syphilis, gonorrhea, and chlamydial infection. MMWR 2008;57(No. RR-9):1-62.
- CDC. HIV Partner Service Delivery Among Blacks or African Americans — United States, 2016. MMWR 2019;58(4):81-86.
- CDC. HIV Testing, Linkage to HIV Medical Care, and Interviews for Partner Services Among Black Men Who Have Sex with Men — Non–Health Care Facilities, 20 Southern U.S. Jurisdictions, 2016. MMWR 2018;67(28):778-781.
- CDC. HIV Testing, Linkage to HIV Medical Care, and Interviews for Partner Services Among Youths — 61 Health Department Jurisdictions, United States, Puerto Rico, and the U.S. Virgin Islands, 2015. MMWR 2017; 66(24):629-635.
- CDC. HIV Testing, Linkage to HIV Medical Care, and Interviews for Partner Services Among Women — 61 Health Department Jurisdictions, United States, Puerto Rico, and the U.S. Virgin Islands, 2015. MMWR 2017;66(41);1100-1104.
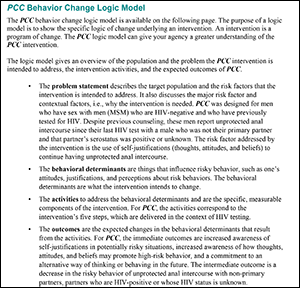
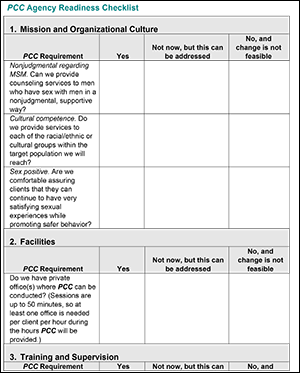
About Personalized Cognitive Counseling
Personalized Cognitive Counseling (PCC) is a 30- to 50-minute individual-level, single-session intervention. PCC encourages HIV test clients to identify thoughts and feelings from a recent episode of unprotected anal sex reduce to the risk behavior in future situations.
Intervention goal
To reduce unprotected anal sex among repeat HIV testing, HIV negative MSM.
Intervention core elements
- Provide one-on-one counseling focusing on a recent, memorable episode of unprotected anal sex.
- Provide the service within the context of HIV testing and counseling, prevention case management, primary medical care, or mental health services.
- Direct the client to review the PCC Checklist of Thoughts.
- Explore the circumstances and context of the episode of unprotected anal sex in detail before, during, and after the event.
- Identify specific self-justifications used by the client in making the decision to engage in the specific event and then, in relation to each self-justification heard, clarify how they are linked to the decision to have unprotected sex.
- Guide the clients to reexamine their thoughts and identify ways they might think differently in the future.
Intervention population
To be eligible for PCC, the client must:
- be a man who has sex with men;
- have previously tested HIV-negative and not on PrEP;
- does not have a chronic substance use;
- have had unprotected anal sex since their last HIV test with a non-primary partner who was HIV-positive or whose status was unknown;
- be able to recall the unprotected anal sex event; and
- know about HIV risk behavior.
Personalized Cognitive Counseling training
This training has one prerequisite and two components:
Fundamentals of Motivational Interviewing for HIV virtual instructor-led training is a prerequisite for this training.
- 3-day virtual instructor-led training intended for frontline staff who will conduct PCC with the following experience:
- A 1-day virtual instructor-led mini-training intended for frontline staff who will conduct PCC may be offered only if the 3-day training is not available. This mini-training is also available in Spanish.
To view and register for scheduled virtual instructor-led trainings:
- Access the National HIV Classroom Learning Center training calendar hosted on Cicatelli Associates, Inc.'s (CAI's) website.
- Pre-register for your selected course via the link provided in the training calendar.
Complete your registration on CDC TRAIN as directed when you receive an email from the National HIV Classroom Learning Center. You must join the HIV CBA Learning Group and locate the HIV CBA Training Plan in order to complete your CDC TRAIN registration for a specific classroom session (step-by-step instructions are available).
To access eLearning modules, including training prerequisite courses:
- Log-in to CDC TRAIN and access the HIV CBA Training Plan (step-by-step instructions are available).
- Select the module you wish to take.
- Launch the module or save the module for later.
Technical assistance for the implementation of PCC is available.
To request technical assistance or that a training session be scheduled:
- CDC's directly funded health department and CBO partners may request technical assistance or a training session by submitting a request in the CBA Tracking System.
- Organizations not directly funded by CDC may contact their local health department for assistance in submitting a training or technical assistance request.
If you have questions or need additional assistance, please contact HIVCBA@cdc.gov.
Implementation and marketing materials
The materials and resources listed below support the implementation and/or marketing of Personalized Cognitive Counseling by health departments, community-based organizations, and health care or other organizations. The resources are evidence-based and designed for cost-effective, scalable implementation.
About SNS for HIV testing recruitment
With SNS for HIV testing recruitment, agencies identify persons with HIV or have risk factors for HIV and enlist them to become recruiters. Unlike peer advocates or peer educators, recruiters are short-term volunteers and require little training and supervision. With the support of an SNS manager, recruiters identify their network associates—people in their social networks (e.g., friends, sex or drug use partners, family members, etc.) who are at increased risk of getting or transmitting HIV. Recruiters then speak with their NAs and refer or accompany them to an agency where they can receive HIV testing services.
Recruiters and network associates receive compensation for their participation in the program.
Core elements of SNS

SNS training
This training has one component:
- 2-day virtual, instructor-led training; or
- 2-day live classroom training
- Español language, 2-day, virtual, instructor-led training also available.
To view and register for scheduled trainings:
- Access the National HIV Classroom Learning Center training calendar hosted on Cicatelli Associates, Inc.'s (CAI's) website.
- Pre-register for your selected course via the link provided in the training calendar.
- Complete your registration on CDC TRAIN as directed when you receive an email from the National HIV Classroom Learning Center. You must join the HIV CBA Learning Group and locate the HIV CBA Training Plan in order to complete your CDC TRAIN registration for a specific training session (step-by-step instructions are available).
To request that a training session be scheduled:
- CDC's directly funded health department and CBO partners may request delivery of a CDC-supported training by submitting a request in the CBA Tracking System.
- Organizations not directly funded by CDC may contact their local health department for assistance in submitting a training request.
If you have questions or need additional assistance, please contact HIVCBA@cdc.gov.
Implementation and marketing materials
The materials and resources listed below support the implementation and/or marketing of Social Network Strategy for HIV Testing Recruitment by health departments, community-based organizations, and health care or other organizations. The resources are evidence-based and designed for cost-effective, scalable implementation.
Treat
People who have HIV and who take medicine as prescribed and maintain an undetectable viral load can live long, healthy lives and will not sexually transmit HIV to their partner(s). Resources are available for the HIV prevention workforce to increase its capacity to link, retain, and re-engage people to care and treatment.
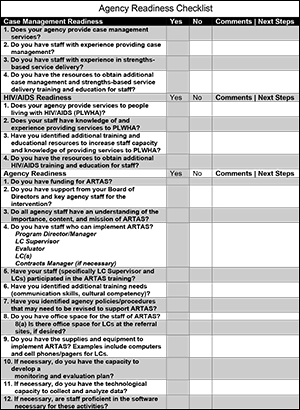
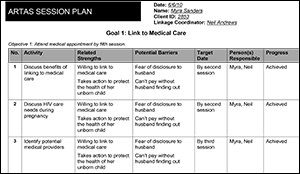
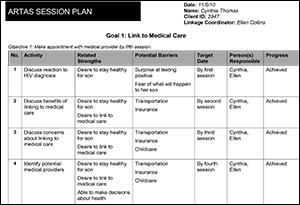
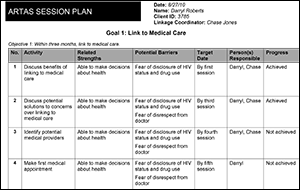
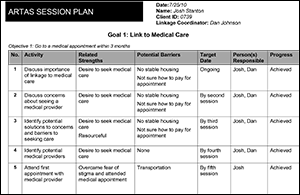
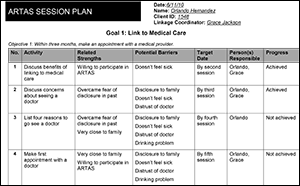
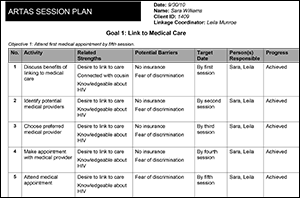
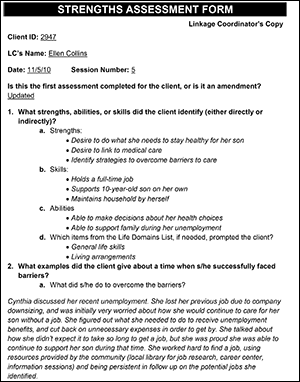
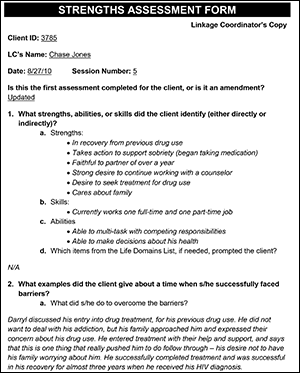
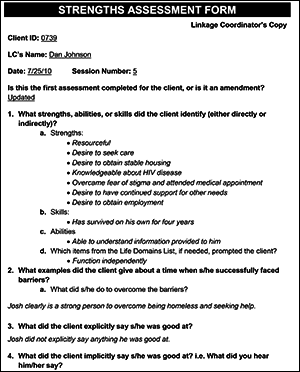
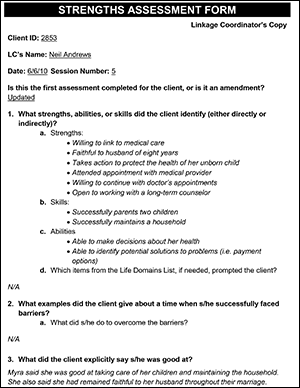
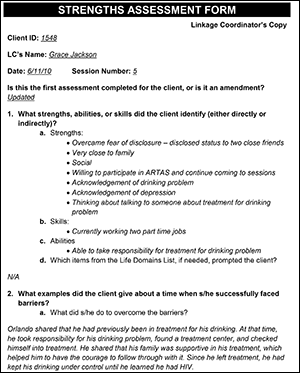
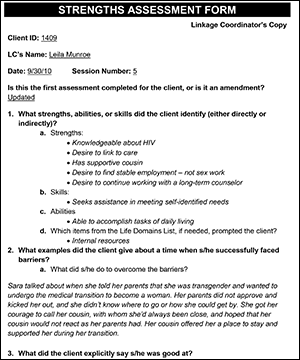
About ARTAS
Anti-Retroviral Treatment and Access to Services (ARTAS) is an individual-level, multi-session, time-limited intervention designed to link individuals with recently diagnosed HIV to medical care. ARTAS supports early access to HIV medical care and helps clients to address barriers by emphasizing the client's abilities rather than inabilities through use of the strengths-based approach. The setting of objectives and goals is driven by the client who must implement these changes. Finally, the mutually respectful and cooperative relationship between the client and linkage coordinator supports the client in their efforts to implement changes and overcome barriers.
ARTAS consists of up to five client sessions conducted over a 90-day period or until the client links to medical care – whichever comes first. ARTAS views the community as a resource for the client and client sessions are encouraged to take place outside the office or wherever the client feels most comfortable. Following the final client session, the client may be linked to a long-term/Ryan White case manager and/or another service delivery system to address his/her longer-term barriers to remaining in care, such as substance use treatment or mental health services.
Intervention goals
The goal of ARTAS is to support people with HIV in linking to medical care soon after receiving a positive HIV test result.
- ARTAS helps clients overcome barriers to being successfully linked to medical care.
- ARTAS aims to create a trusting, effective relationship between client and Linkage Coordinator.
- ARTAS helps to facilitate a client's ability to create an action plan for being linked to medical care.
Intervention core elements
- Build an effective working relationship between the Linkage Coordinator and each client
- Focus on a client's strengths by:
- conducting a strengths-based assessment; and
- encouraging each client to identify and use strengths, abilities, and skills to link to medical care and accomplish other goals.
- Facilitate a client's ability to:
- identify and pursue their own goals; and
- develop a step-by-step plan to accomplish those goals.
- Maintain a client-driven approach by:
- conducting one to five structured sessions with each client;
- conducting active, community-based case management;
- coordinating and linking each client to available community resources; and
- advocating on a client's behalf.
Intervention population
Persons with HIV who are not in medical care and willing to participate in the intervention.
ARTAS training
This training has three components:
- 1-hour eLearning pre-course module
- 1-hour Strengths-based Case Management eLearning module (English and Español language versions available)
- 3-day (15-hour) virtual, instructor-led training; or
- 2 -day (16-hour) in a live classroom setting
Training also available in Español.
This training is intended for persons who will conduct ARTAS sessions with clients, also known as the Linkage Coordinators. Ideally, Linkage Coordinators should have experience providing case management or social services and can include experienced case managers, social workers, and/or HIV test counselors.
Participants must complete the ARTAS Pre-Course Online Module and ARTAS Strengths-Based Case Management eLearning module located in CDC TRAIN before they can attend the instructor-led training.
To view and register for scheduled training:
- Access the National HIV Classroom Learning Center training calendar hosted on Cicatelli Associates, Inc.'s (CAI's) website.
- Pre-register for your selected course via the link provided in the training calendar.
- Complete your registration on CDC TRAIN as directed when you receive an email from the National HIV Classroom Learning Center. You must join the HIV CBA Learning Group and locate the HIV CBA Training Plan in order to complete your CDC TRAIN registration for a specific classroom session (step-by-step instructions are available).
To access eLearning modules, including training prerequisite courses:
- Log-in to CDC TRAIN and access the HIV CBA Training Plan (step-by-step instructions are available).
- Select the module you wish to take.
- Launch the module or save the module for later.
To request that a training session be scheduled:
- CDC's directly funded health department and CBO partners may request delivery of a CDC-supported training by submitting a request in the CBA Tracking System.
- Organizations not directly funded by CDC may contact their local health department for assistance in submitting a training request.
If you have questions or need additional assistance, please contact HIVCBA@cdc.gov.
Implementation and marketing materials
The materials and resources listed below support the implementation and/or marketing of ARTAS by health departments, community-based organizations, and health care or other organizations. The resources are evidence-based and designed for cost-effective, scalable implementation.
References
- Gardner LI, Metsch LR, Anderson-Mahoney P, Loughlin AM, del Rio C, Strathdee S, Sansom SL, Siegal HA, Greenberg AE, Holmberg SD; Antiretroviral Treatment and Access Study Study Group. Efficacy of a brief case management intervention to link recently diagnosed HIV-infected persons to care. AIDS 2005;19(4):423-431.
- Craw JA, Gardner LI, Marks G, Rapp RC, Bosshart J, Duffus WA, Rossman A, Coughlin SL, Gruber D, Safford LA, Overton J, Schmitt K. Brief strengths-based case management promotes entry into HIV medical care: Results of the antiretroviral treatment access study-II. J Acquir Immune Defic Syndr 2008;47(5):597-606.
- Neduzhko O, Postnov O, Sereda Y, Kulchynska R, Bingham T, Myers JJ, Flanigan T, Kiriazova T. Modified Antiretroviral Treatment Access Study (MARTAS): A randomized controlled trial of the efficacy of a linkage-to-care intervention among HIV-positive patients in Ukraine. AIDS and Behavior 2020;24:3142-3154.
About Data to Care
D2C approaches may vary and range in scope and design. Some examples of D2C activities include using HIV surveillance data routinely collected by state and local health departments and other data sources to:
- identify persons who are not in care (NIC) and then link or re-engage them in care;
- identify persons who are in care but not virally suppressed and work with these clients and their providers to achieve viral suppression; and
- identify pregnant women or mothers and their exposed infants who may need coordinated services (perinatal HIV services coordination).
Considerations for implementing D2C
D2C should be implemented as part of a comprehensive strategy for linkage to and re-engagement in care activities. It is a collaborative effort between the health department, HIV medical providers, and essential support service providers.
When implemented as part of a comprehensive strategy, D2C programs can result in:
- Successful linkage to or re-engagement in care for persons with HIV;
- Expanded partner services for persons with HIV not newly diagnosed, including an opportunity to re-interview individuals out of care, conduct partner notification, and offer testing and other prevention services;
- Identification of and follow-up with persons with HIV who may be in care, but are not virally suppressed, and need adherence support or other services;
- Improved surveillance data quality; and
- Better collaboration among surveillance, prevention, care, and treatment staff.
Data to Care training
There is no CDC-supported training currently available for Data to Care. Technical assistance for the implementation of Data to Care is available.
To request technical assistance:
- CDC's directly funded health department and CBO partners may request technical assistance by submitting a request in the CBA Tracking System.
- Organizations not directly funded by CDC may contact their local health department for assistance in submitting a request.
If you have questions or need additional assistance, please contact HIVCBA@cdc.gov.
Implementation and marketing materials
The National Alliance for State and Territorial AIDS Directors (NASTAD), a capacity building assistance (CBA) provider funded by the Centers for Disease Control and Prevention (CDC), offers two resources on D2C implementation for health departments:
- Data Points: A Health Department Roadmap for Enhancing Data to Care Programs: a digi-book intended to help health departments lay the foundation for successful D2C implementation; and
- The Data to Care Hub: a supplement to Data Points that is intended to help health departments strengthen and expand their D2C programs.
The additional materials and resources listed below support the implementation and/or marketing of Data to Care by health departments, community-based organizations, and other healthcare organizations. The resources are evidence-based and designed for cost-effective, scalable implementation.
References
The following are published articles on the various elements of D2C that health departments may find useful when implementing and improving their D2C programs.
Overview
- Mokotoff ED, Green Ruth K, Benbow N, Sweeney P, Nelson Sapiano T, McNaghten AD. Data to Care: Lessons Learned From Delivering Technical Assistance to 20 Health Departments. J Acquir Immune Defic Syndr 2019;82(suppl 1):S74-79.
- Sweeney P, DiNenno EA, Flores SA, Dooley S, Shouse RL, Muckleroy S, Margolis AD. HIV Data to Care—Using Public Health Data to Improve HIV Care and Prevention. J Acquir Immune Defic Syndr 2019;82(suppl 1):S1-S5.
- Williams KM, Taylor RD, Painter T, Jeffries WL 4th, Prather C, Spikes P, Mulatu MS, Henny K, Hoyte T, Flores SA. Learning by Doing: Lessons From the Care and Prevention in the United States Demonstration Project. Public Health Rep 2018;133(2_suppl):18S-27S.
Implementation
- Lewis S, Morrison M, Randall LM, Roosevelt K. The Partnerships for Care Project in Massachusetts: Developing Partnerships and Data Systems to Increase Linkage and Engagement in Care for Individuals Living With HIV. J Acquir Immune Defic Syndr 2019;82(suppl 1):S47-S52.
- Neblett Fanfair R, Shrestha RK, Randall L, Lucas C, Nichols L, Camp NM, Brady K, Jenkins H, Altice F, Villanueva M, DeMaria A. Implementing Data to Care—What Are the Costs for the Health Department? J Acquir Immune Defic Syndr 2019;82 (suppl 1):S57-S61.
Demonstration Projects
- Beltrami J, Dubose O, Carson R, Cleveland JC. Using HIV Surveillance Data to Link People to HIV Medical Care, 5 U.S. States, 2012-2015. Public Health Rep 2018;133(4):385-391.
- Bove JM, Golden MR, Dhanireddy S, Harrington RD, Dombrowski JC. Outcomes of a Clinic-Based Surveillance-Informed Intervention to Relink Patients to HIV Care. J Acquir Immune Defic Syndr 2015;70(3):262-268.
- Buchacz K, Chen MJ, Parisi MK, Yoshida-Cervantes M, Antunez E, Delgado V, Moss NJ, Scheer S. Using HIV surveillance registry data to re-link persons to care: The RSVP Project in San Francisco. PLoS One 2015;10(3):e0118923.
- Dombrowski JC, Bove J, Roscoe JC, Harvill J, Firth CL, Khormooji S, Carr J, Choi P, Smith C, Schafer SD, Golden MR; Northwest Health Department Centers for AIDS Research (CFAR) Consortium. "Out of Care" HIV Case Investigations: A Collaborative Analysis Across 6 States in the Northwest U.S. J Acquir Immune Defic Syndr 2017;74(suppl 2):S81-S87.
- Hague JC, John B, Goldman L, Nagavedu K, Lewis S, Hawrusik R, Rajabiun S, Cocoros N, Fukuda HD, Cranston K. Using HIV Surveillance Laboratory Data to Identify Out-of-Care Patients. AIDS Behav 2019;23(suppl 1):78-82.
- Hart-Malloy R, Brown S, Bogucki K, Tesoriero J. Implementing data-to-care initiatives for HIV in New York state: Assessing the value of community health centers identifying persons out of care for health department follow-up. AIDS Care 2018;30(3):391-396.
- Sweeney P, Hoyte T, Mulatu MS, Bickham J, Brantley AD, Hicks C, McGoy SL, Morrison M, Rhodes A, Yerkes L, Burgess S, Fridge J, Wendell D. Implementing a Data to Care Strategy to Improve Health Outcomes for People With HIV: A Report From the Care and Prevention in the United States Demonstration Project. Public Health Rep 2018;133(2_suppl):60S-74S.
- Wohl AR, Dierst-Davies R, Victoroff A, James S, Bendetson J, Bailey J, Daar E, Spencer L, Kulkarni S, Pérez MJ. Implementation and Operational Research: The Navigation Program: An Intervention to Reengage Lost Patients at 7 HIV Clinics in Los Angeles County, 2012-2014. J Acquir Immune Defic Syndr 2016;71(2):e44-50.
Collaborations
- Davies C, Klein PW, Okoye ID, Heitgerd J, Shapatava E, Ihiasota I, Browne MNC, Viall A, Stockmann D, Hauck H. Short-Term Outcomes and Lessons Learned From the Federal HIV Health Improvement Affinity Group for State Medicaid/Children's Health Insurance Program Agencies and State Health Departments. J Acquir Immune Defic Syndr 2019;82(suppl 1):S62-S68.
- Harrison TP, Williams KM, Mulatu MS, Edwards A, Somerville GG, Cobb-Souza S, Dunbar E, Barskey A. Integrating Federal Collaboration in HIV Programming: The CAPUS Demonstration Project, 2012-2016. Public Health Rep 2018;133(2_suppl):10s-17s.
- Hart-Malloy R, Rajulu DT, Johnson MC, Shrestha T, Spencer EC, Anderson BJ, Tesoriero JM. Cross-Jurisdictional Data to Care: Lessons Learned in New York State and Florida. J Acquir Immune Defic Syndr 2019;82:S42-S46.
- Macomber KE, Viall A, Ramakrishnan V, Wilson J, Brandt MG, Kinsinger L, Kreiner M, Curtis T, Copeland R, Staudacher A, Neff D. Operationalizing a Data to Care Strategy in Michigan Through Cross-Agency Collaborations. J Acquir Immune Defic Syndr 2019;82:S69-S73.
- Ocampo JMF, Smart JC, Allston A, Bhattacharjee R, Boggavarapu S, Carter S, Castel AD, Collmann J, Flynn C, Hamp A, Jordan D, Kassaye S, Kharfen M, Lum G, Pemmaraju R, Rhodes A, Stover J, Young MA. Improving HIV Surveillance Data for Public Health Action in Washington, DC: A Novel Multiorganizational Data-Sharing Method. JMIR Public Health Surveill 2016;2(1):e3.
Community Engagement
- Evans D, Van Gorder D, Morin SF, Steward WT, Gaffney S, Charlebois ED. Acceptance of the use of HIV surveillance data for care engagement: National and local community perspectives. J Acquir Immune Defic Syndr 2015;69 (suppl 1):S31-S36.
Data Sources
- Arey AL, Cassidy-Stewart H, Kurowski PL, Hitt JC, Flynn CP. Evaluating HIV Surveillance Completeness Along the Continuum of Care: Supplementing Surveillance With Health Center Data to Increase HIV Data to Care Efficiency. J Acquir Immune Defic Syndr 2019;82:S26-S32.
- Beer L, Bosh KA, Chowdhury PP, Craw J, Nyaku MA, Luna-Gierke RE, Sanders CC, Shouse RL. Informing Data to Care: Contacting Persons Sampled for the Medical Monitoring Project. J Acquir Immune Defic Syndr 2019;82:S6-S12.
- Byrd KK, Camp NM, Iqbal K, Weidle PJ. Pharmacy Data as an Alternative Data Source for Implementation of a Data to Care Strategy. J Acquir Immune Defic Syndr 2019;82:S53-S56.
- Christopoulos KA, Scheer S, Steward WT, Barnes R, Hartogensis W, Charlebois ED, Morin SF, Truong HM, Geng EH. Examining clinic-based and public health approaches to ascertainment of HIV care status. J Acquir Immune Defic Syndr 2015;69 (suppl 1):S56-S62.
- Enns EA, Reilly CS, Virnig BA, Baker K, Vogenthaler N, Henry K., Potential Impact of Integrating HIV Surveillance and Clinic Data on Retention-in-Care Estimates and Re-Engagement Efforts. AIDS Patient Care STDS 2016;30(9):409-415.
- Kunzweiler C, Kishore N, John B, Roosevelt K, Lewis S, Klevens RM, Morrison M, Randall LM, DeMaria A Jr. Using HIV Surveillance and Clinic Data to Optimize Data to Care Efforts in Community Health Centers in Massachusetts: The Massachusetts Partnerships for Care Project. J Acquir Immune Defic Syndr 2019;82:S33-S41.
- Lubelchek RJ, Finnegan KJ, Hotton AL, Hazen R, Murphy P, Prachand NG, Benbow N. Assessing the use of HIV surveillance data to help gauge patient retention-in-care. J Acquir Immune Defic Syndr 2015;69 (suppl 1):S25-S30.
- Padilla M, Mattson CL, Scheer S, Udeagu CN, Buskin SE, Hughes AJ, Jaenicke T, Wohl AR, Prejean J, Wei SC. Locating People Diagnosed With HIV for Public Health Action: Utility of HIV Case Surveillance and Other Data Sources. Public Health Rep 2018;133(2):147-154.
Data Quality
- Dombrowski JC, Bove J, Roscoe JC, Harvill J, Firth CL, Khormooji S, Carr J, Choi P, Smith C, Schafer SD, Golden MR; Northwest Health DepartmentCenters for AIDS Research (CFAR) Consortium. "Out of Care" HIV Case Investigations: A Collaborative Analysis Across 6 States in the Northwest U.S. J Acquir Immune Defic Syndr 2017;74(suppl 2):S81-S87.
- Ocampo JMF, Hamp A, Rhodes A, Smart JC, Pemmaraju R, Poschman K, Hess KL, Bhattacharjee R, Flynn C, Anderson BJ, Dowling JE, Maccormack F, Doshi R, Lum G, Maddox L, Moncur B, Barnhart JE, Maxwell J, Aurand SB, Hogan V, Wills D, Prowell S, Kassaye SG, Karn HE, Laffoon BT, Collmann J. Improving HIV Surveillance Data by Using the ATra Black Box System to Assist Regional Deduplication Activities. J Acquir Immune Defic Syndr 2019;82:S13-S19.
- Ocampo JMF, Smart JC, Allston A, Bhattacharjee R, Boggavarapu S, Carter S, Castel AD, Collmann J, Flynn C, Hamp A, Jordan D, Kassaye S, Kharfen M, Lum G, Pemmaraju R, Rhodes A, Stover J, Young MA. Improving HIV Surveillance Data for Public Health Action in Washington, DC: A Novel Multiorganizational Data-Sharing Method. JMIR Public Health Surveill 2016;2(1):e3.
Partner Services
- Hart-Malloy R, Shrestha Tarak, Pezzulo MC, Patterson W, Gunn JKL, Johnson MC, Tesoriero JM. Data to Care Opportunities: An Evaluation of Persons Living With HIV Reported to Be "Current to Care" Without Current HIV-Related Labs. J Acquir Immune Defic Syndr 2019;82:S20-S25.
- Tesoriero JM, Johnson BL, Hart-Malloy R, Cukrovany JL, Moncur BL, Bogucki KM, Anderson BJ, Johnson MC. Improving Retention in HIV Care Through New York's Expanded Partner Services Data-to-Care Pilot. J Public Health Manag Pract 2017;23(3):255-263.
Evaluation
- Dombrowski JC, Hughes JP, Buskin SE, Bennett A, Katz D, Fleming M, Nunez A, Golden MR. A Cluster Randomized Evaluation of a Health Department Data to Care Intervention Designed to Increase Engagement in HIV Care and Antiretroviral Use. Sex Transm Dis 2018;45(6):361-367.
About Fundamentals of Motivational Interviewing for HIV training course
The "Fundamentals of Motivational Interviewing for HIV" training course will introduce learners to the foundational content and skills of MI. This course describes motivational interviewing, explores its effectiveness, and reviews the elements and skills necessary to utilize MI. It gives learners the opportunity to practice the fundamental skills necessary for applying MI during client interactions. This course is offered in two formats—virtual, instructor-led course and live, classroom course.
Course Learning Objectives
- Define motivational interviewing and how the MI approach helps healthcare providers build their relationship with their clients
- Discuss the effectiveness of MI and how it has been applied in HIV prevention and care
- Describe the "spirit" of MI, which communicates compassion, acceptance, partnership, and respect
- Describe and practice the four processes of MI
- Use the core communication skills of MI: open-ended questions, affirmations, reflective listening, and summarizing
- Describe the foundational content of MI
- Build skills to use MI in your client encounters
Intended learners
- Healthcare providers and clinic staff that implement HIV programs and services
- Community-based organizations (CBOs) workforce
- Health department workforce
Fundamentals of motivational interviewing for HIV training
This training has one component:
- 2 five-hour days in a virtual, instructor-led training setting; or
- 2 eight-hour days in a live classroom setting
To view and register for trainings:
- Access the National HIV Classroom Learning Center training calendar hosted on Cicatelli Associates, Inc.'s (CAI's) website.
- Pre-register for your selected course via the link provided in the training calendar.
- Complete your registration on CDC TRAIN as directed when you receive an email from the National HIV Classroom Learning Center. You must join the HIV CBA Learning Group and locate the HIV CBA Training Plan in order to complete your CDC TRAIN registration for a specific training session (step-by-step instructions are available).
Technical assistance for the implementation of Fundamentals of Motivational Interviewing for HIV is available.
To request technical assistance:
- CDC's directly funded health department and CBO partners may request technical assistance support by submitting a request in the CBA Tracking System.
- Organizations not directly funded by CDC may contact their local health department for assistance in submitting a training request.
If you have questions or need additional assistance, please contact HIVCBA@cdc.gov.
References
- Miller WR, Rollnick S. Motivational Interviewing: Helping People Change (3rd ed.). New York City: Guilford Press; 2013.
- Centers for Disease Control and Prevention-Cicatelli Associates, Inc. Fundamentals of Motivational Interviewing for HIV: Trainer Manual; 2020.
About HIV Navigation Services – STEPS to Care
HIV Navigation Services – STEPS to Care (HNS–STEPS to Care) includes guiding clients to health care systems, assisting with health insurance and transportation, identifying and reducing barriers to care, and tailoring health education to the client to support their full engagement in care.HNS–STEPS to Care guides persons at high risk to and retains them in HIV services such as:
- HIV care and treatment
- nPEP;
- PrEP; and
- Services and interventions dealing with other major risk-complicating factors including substance use, violence, stigma, mental health, homelessness, and other health disparities.
HNS–STEPS to Care also includes:
- Client identification,
- Health education,
- Motivation,
- Guidance to services,
- Appointment assistance,
- Payer identification,
- Cultural sensitivity,
- Guidance while in services for retention,
- Adherence support, and
- Transportation.
HNS–STEPS to Care training
This training has two components:
- 30-minute eLearning pre-course module
- 3-day virtual, instructor-led training
Training is also available in Español.The HNS-STEPS to Care course is designed to improve navigation skills for those delivering prevention services to persons with HIV and HIV-negative persons at risk. This comprehensive course package is for service providers who want to know more about navigation skills, how navigation fits in the overall field of HIV prevention, structural components of a navigation program, and professional conduct.The recommended training audience includes staff from:
- Community-Based Organizations (CBOs);
- Health Departments;
- Health Care Organizations implementing HIV programs and services; and
- General navigation programs that seek to enhance their existing navigation services.
HNS-STEPS to Care virtual, instructor-led trainings are conducted over a 3-day period. Participants are required to complete the HNS-STEPS to Care pre-course online module prior to attending the virtual, instructor-led training.
To view and register for scheduled virtual, instructor-led trainings:
- Access the National HIV Classroom Learning Center training calendar hosted on Cicatelli Associates, Inc.'s (CAI's) website.
- Pre-register for your selected course via the link provided in the training calendar.
- Complete your registration on CDC TRAIN as directed when you receive an email from the National HIV Classroom Learning Center. You must join the HIV CBA Learning Group and locate the HIV CBA Training Plan in order to complete your CDC TRAIN registration for a specific training session (step-by-step instructions are available).
To access eLearning modules, including training prerequisite courses:
- Log-in to CDC TRAIN and access the HIV CBA Training Plan (step-by-step instructions are available).
- Select the module you wish to take.
- Launch the module or save the module for later.
To request technical assistance or that a training session be scheduled:
- CDC's directly funded health department and CBO partners may request delivery of a CDC-supported training or technical assistance by submitting a request in the CBA Tracking System.
- Organizations not directly funded by CDC may contact their local health department for assistance in submitting a technical assistance or training request.
If you have questions or need additional assistance, please contact HIVCBA@cdc.gov.
Implementation and marketing materials
The materials and resources listed below support the implementation and/or marketing of HIV Navigation Services – STEPS to Care by health departments, community-based organizations, and health care or other organizations. The resources are evidence-based and designed for cost-effective, scalable implementation.
References
- Bradford JB, Jones A, Coleman S. HIV system navigation: An emerging model to improve HIV care access. AIDS Patient Care STDS 2007;21(suppl 1):S49-S58.
- Centers for Disease Control and Prevention, Health Resources and Services Administration, National Institutes of Health, American Academy of HIV Medicine, Association of Nurses in AIDS Care, International Association of Providers of AIDS Care, the National Minority AIDS Council, and Urban Coalition for HIV/AIDS Prevention Services. Recommendations for HIV Prevention with Adults and Adolescents with HIV in the United States, 2014.
- Zuniga JM, International Association of Providers of AIDS Care (IAPAC). IAPAC guidelines for optimizing the HIV care continuum for adults and adolescents. J Int Assoc Provid AIDS Care 2015;14(suppl 1):S3-S34.
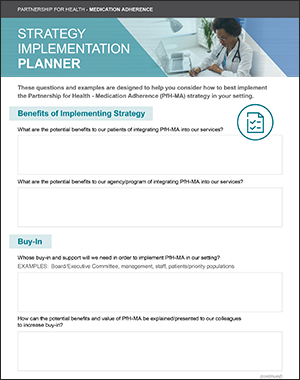
About Partnership for Health-Medication Adherence
Partnership for Health-Medication Adherence (PfH-MA) helps establish a partnership between the provider and patient to increase the knowledge, self-efficacy, and behaviors of the patient associated with adherence to antiretroviral therapy (ART). The relationship between the provider and patient provides an underlying trust that facilitates behavior change. The provider fosters an open and honest relationship through active listening skills and engaging the patient to discuss concerns around their treatment regimen. The provider and patient develop an individualized adherence plan together during the clinic visit by problem solving barriers to adherence and identifying solutions.
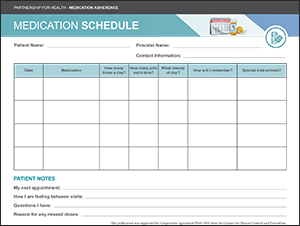
Intervention core elements
- A trusting relationship between provider and patient to increase the patient's knowledge and self-efficacy, address patient concerns, and problem solve barriers to medication adherence;
- Adherence support tools such as adherence messaging displayed in posters and brochures and the medication schedule to track the individualized adherence plan; and
- A seven-step approach to structure short conversations with patients about medication adherence at every visit.
Intervention goals
- Improve adherence to antiretroviral therapy.
- Achieve an undetectable viral load.
Intervention population
- Persons with HIV in outpatient clinics
Partnership for Health-Medication Adherence training
This training has one component:
- 1-hour and 45-minute eLearning module
A 1-hour and 45-minute Partnership for Health–Medication Adherence eLearning module is located in CDC TRAIN. The primary target audience for this course is physicians who treat people living with HIV; however, anyone providing medical care or other support services to this population may find the information in the eLearning module to be useful.
To access eLearning modules, including training prerequisite courses:
- Log-in to CDC TRAIN and access the HIV CBA Training Plan (step-by-step instructions are available).
- Select the module you wish to take.
- Launch the module or save the module for later.
Technical assistance for the implementation of Partnership for Health-Medication Adherence is available.
To request technical assistance:
- CDC's directly funded health department and CBO partners may request technical assistance by submitting a request in the CBA Tracking System.
- Organizations not directly funded by CDC may contact their local health department for assistance in submitting a request.
If you have questions or need additional assistance, please contact HIVCBA@cdc.gov.
Implementation and marketing materials
The materials and resources listed below support the implementation and/or marketing of Partnership for Health – Medication Adherence by health departments, community-based organizations, and health care or other organizations. The resources are evidence-based and designed for cost-effective, scalable implementation.
References
- Milam J, Richardson JL, McCutchan A, Stoyanoff S, Weiss J, Kemper C, Larsen RA, Hollander H, Weismuller P, Bolan R. Effect of a brief antiretroviral adherence intervention delivered by HIV care providers. J Acquir Immune Defic Syndr 2005;40(3):356-363.
About PROMISE for HIP
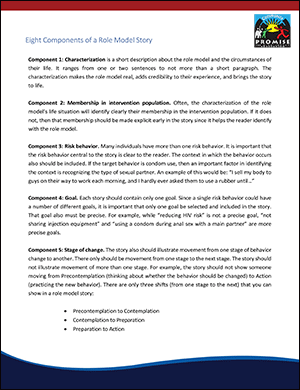
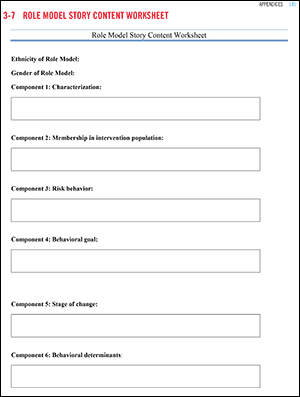
PROMISE for HIP is based on several behavioral theories, including Stages of Change Theory, the Theory of Reasoned Action, and Social Cognitive Theory. PROMISE for HIP begins with a community identification process to collect and analyze information about the risk networks, sex and drug risk behaviors, indicators related to the HIV continuum of care, and identification of determinants of risk. This helps agencies identify and intervene with the intervention populations and appropriately tailor the intervention to specific network needs.
Members of the intervention population who have made positive behavior change and/or engage in HIV care, including medication adherence, are interviewed and role models' stories are written based upon the interviews. The stories are personal accounts of positive behavior change about how and why the participants took steps to reduce risk, engage in HIV care, be adherent to medication, and the resulting positive effects on their lives. The stories can be presented as printed materials via face-to-face community outreach or in video format using social media platforms.
Peer advocates from the intervention population are recruited and trained to distribute the role model stories and prevention materials within their social networks. New role model stories are written based on continuous formative research that reflects behavior change within the intervention population. Intervention Goals1890
- To disseminate positive messages to intervention populations about condom use, HIV testing, accessing pre-exposure prophylaxis (PrEP) and post-exposure prophylaxis (PEP), engaging and/or re-engaging in care, and adhering to anti-retroviral therapy (ART) regimens.
- To encourage significant movement by community members toward consistent condom use with their main and non-main partner.
- To significantly increase condom carrying among members of the communities.
Intervention core elements
- Community identification process to collect information about the network, including HIV/STD risk behaviors and HIV care continuum.
- Create role model stories based on personal accounts from individuals in the intervention population who have made positive behavior change.
- Recruit and train peer advocates from the intervention population to distribute role model stories and prevention materials.
- Continuous evaluation to capture behavior change within the intervention population.
PROMISE for HIP training
This training has two components:
- 1-hour eLearning pre-course
- 2-day virtual instructor-led training
To access eLearning modules, including training prerequisite courses:
- Log-in to CDC TRAIN and access the HIV CBA Training Plan (step-by-step instructions are available).
- Select the module you wish to take.
- Launch the module or save the module for later.
To view and register for scheduled virtual instructor-led trainings:
- Access the National HIV Classroom Learning Center training calendar hosted on Cicatelli Associates, Inc.'s (CAI's) website.
- Pre-register for your selected course via the link provided in the training calendar.
Complete your registration on CDC TRAIN as directed when you receive an email from the National HIV Classroom Learning Center. You must join the HIV CBA Learning Group and locate the HIV CBA Training Plan in order to complete your CDC TRAIN registration for a specific classroom session (step-by-step instructions are available).
Technical assistance for the implementation of PROMISE for HIP is available.
To request technical assistance:
- CDC's directly funded health department and CBO partners may request technical assistance by submitting a request in the CBA Tracking System.
- Organizations not directly funded by CDC may contact their local health department for assistance in submitting a request.
If you have questions or need additional assistance, please contact HIVCBA@cdc.gov.
Implementation and marketing materials
The materials and resources listed below support the implementation and/or marketing of PROMISE for HIP by health departments, community-based organizations, and health care or other organizations. The resources are evidence-based and designed for cost-effective, scalable implementation.
References
- CDC AIDS Community Demonstration Projects Research Group. Community-level HIV intervention in 5 cities: Final outcome data from the AIDS community demonstration projects. Am J Public Health 1999;89(3):336-345.
About Stay Connected for Your Health
Stay Connected for Your Health is a clinic-wide intervention that uses posters, brochures, and brief verbal messages delivered to patients by clinic staff. Additionally, patients who are new or inconsistent in appointment attendance are offered meetings with a Retention Specialist. This intervention combines strategies from two research studies that demonstrated improvement in retention in HIV care. Stay Connected for Your Health is delivered to patients who are newly diagnosed with HIV, re-engaging in care, or at risk of falling out of care.
Intervention goals
- Improve retention in care and attendance of clinic visits
Intervention essential elements
- Warm, positive greetings and retention messages during patient visits that are incorporated by all staff;
- Brochures and posters displayed in the waiting room and exam rooms to reinforce the importance of staying in care;
- Meetings between the patient and the Retention Specialist during routine visits to build rapport, address challenges to remaining in care, and assist patients in coming up with strategies to overcome challenges to retention; and
- Referrals provided for auxiliary services such as mental health, substance use, housing, and others.
Intervention audience
- Clinics that provide care for patients with HIV
Stay Connected for Your Health training
This intervention has 2 trainings:
- All Staff virtual instructor-led training delivered over one half-day.
- Retention Specialist virtual instructor-led training delivered over three half-days. Retention Specialists are also required to take 1) Stay Connected for Your Health: All Staff Virtual Instructor-led Training; 2) Fundamentals of Motivational Interviewing for HIV, Virtual Instructor-led Training; and 3) Stay Connected for Your Health: Retention Specialists Online Pre-Course.
The goals of these trainings are as follows:
All Staff Training Goals
- Provide information on Stay Connected for Your Health and its role in care retention;
- Improve the ability of all clinic staff to deliver brief, positive, welcoming messages to patients; and
- Equip clinical staff with skills to deliver Stay Connected for Your Health messages to people with HIV.
Retention Specialist Training Goals
- Describe the roles and responsibilities of the Retention Specialist in improving retention among patients in the clinic; and
- Equip the Retention Specialist with the skills and strategies of Motivational Interviewing to provide face-to-face personalized meetings and interim phone calls to patients to improve retention in care.
To view and register for scheduled virtual, instructor-led trainings:
- Access the National HIV Classroom Learning Center training calendar hosted on Cicatelli Associates, Inc.'s (CAI's) website.
- Pre-register for your selected course via the link provided in the training calendar.
- Complete your registration on CDC TRAIN as directed when you receive an email from the National HIV Classroom Learning Center. You must join the HIV CBA Learning Group and locate the HIV CBA Training Plan in order to complete your CDC TRAIN registration for a specific training session (step-by-step instructions are available).
To access eLearning modules, including training prerequisite courses:
- Log-in to CDC TRAIN and access the HIV CBA Training Plan (step-by-step instructions are available).
- Select the module you wish to take.
- Launch the module or save the module for later.
To request technical assistance or that a training session be scheduled:
- CDC's directly funded health department and CBO partners may request delivery of a CDC-supported training or technical assistance by submitting a request in the CBA Tracking System.
- Organizations not directly funded by CDC may contact their local health department for assistance in submitting a training or technical assistance request.
If you have questions or need additional assistance, please contact HIVCBA@cdc.gov.
Implementation and marketing materials
The materials and resources listed below support the implementation and/or marketing of Stay Connected for Your Health by health departments, community-based organizations, and health care or other organizations. The resources are evidence-based and designed for cost-effective, scalable implementation.
References
- Gardner LI, Marks G, Craw JA, Wilson TE, Drainoni M, More RD, Mugavero MJ, Rodriguez AE, Bradley-Springer LA, Holman S, Keruly JC, Sullivan M, Skolnik PR, Malitz F, Metsch LR, Raper JL, Giordano TP; Retention in Care Study Group. A low-effort, clinic-wide intervention improves attendance for HIV primary care. Clin Infect Dis 2012;55(8):1124-1134.
- Gardner LI, Giordano TP, Marks G, Wilson TE, Craw JA, Drainoni M, Keruly JC, Rodriguez AE, Malitz F, Moore RD, Bradley-Springer LA, Holman S, Rose CE, Girde S, Sullivan M, Metsch LR, Saag M, Mugavero MJ; Retention in Care Study Group. Enhanced personal contact with HIV patients improves retention in primary care: A randomized trial in 6 U.S. HIV clinics. Clin Infect Dis 2014;59(5):725-734.
About
The STEPS to Care Toolkit supports three key strategies of HIV care coordination:
- Patient navigation
- Care team coordination
- HIV self-management
Dashboard
Learn about the three STEPS strategies, how they work together, and to find related tools, templates, and guidance.
STEP 1: Start with the basics
Preview Guide and FAQs
This preview guide addresses many of the common questions Program Directors have when considering or preparing to implement STEPS to Care at their agency. The questions and answers highlight both the strengths of STEPS to Care and some of the challenges that agencies may face during planning and start-up, implementation, and maintenance. This guide also provides information on how the STEPS to Care online tools and resources can be used to support agencies during each of these phases.
STEPS Strategies
In the Patient navigation sessions, navigators build a strong relationship with their clients and teach HIV self-management skills through educational information and counseling. Regularly scheduled care team coordination meetings ensure the interdisciplinary team—including navigators, care coordinators, program directors, physicians, and nurses—remains informed and responsive to the client's changing needs.
Client Pathway and Relevant Provider Forms: This chart provides an overview of the client experience and shows how the three strategies work together to create the STEPS to Care program. The chart also shows which staff member is responsible for each step along the path, and lists the forms and protocols needed to deliver HIV services.
Key Components Checklist: This checklist contains an overview of agency practices involved in implementing each of the three STEPS to Care strategies and the tools that are designed to support them. Program Directors can use this checklist to determine if and how these activities align with what their agency is already doing and which tools they can use or adapt. As the agency prepares for implementation, the checklist can be used to create a "training curriculum" for individual staff members. For example, Program Directors can place a checkmark next to the tools that a patient navigator should complete or read prior to meeting with clients, as well as a targeted completion date for each. Program Directors should meet at least once a month (more frequently at first) to discuss staff progress in using these tools.
STEP 2: Prepare for clients
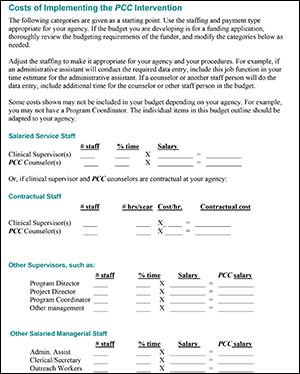
Budgeting
Program Directors must allocate the proper resources and funds to implement the STEPS to Care program.
Creating a systematic budget for your agency's STEPS program ensures the costs of staff pay, direct service implementation, non-direct service implementation, administration, and overhead are accounted for and managed.
This section includes a budgeting toolkit to help you plan your budget for STEPS and keep track of agency funding during implementation.
After using the budget resources below, you will know how to:
- Create and maintain a budget for STEPS to Care
- Identify cost categories associated with implementation of STEPS
Budget toolkit
Creating a system for budgeting is an important way for Program Directors to stay on top of all budget needs.
Use the Budget Toolkit to:
- Report to partner organizations and agencies
- Inform your future implementation by helping you estimate the costs of carrying out each service
The Toolkit is a single Microsoft Excel spreadsheet with a glossary and three separate calculation sheets that can be used to generate an overall budget:
Staff pay: Use this sheet to track the pay for the Program Director, patient navigator, care coordinator, and other staff members of the STEPS program. This includes both salaried employees and hourly rate employees.
Implementation costs: Use this sheet to estimate the costs (with the staff pay information entered on the "Staff Pay" sheet) for the following categories and calculate the percent of contribution from different staff member types and the cost of implementing each service type:
- Direct service implementation with clients, which includes:
- Intake assessment
- Outreach for re-engagement
- Care plan
- Other assessment/reassessment
- Accompaniment
- Assistance with health care
- Assistance with entitlements/benefits
- Assistance with social services
- Assistance with housing
- Logistics planning
- Care team meetings
- Case finding
- HIV Self-Management
- Administrative, which includes:
- Establishing policies and procedures
- Budgeting
- Staffing
- Non-direct service implementation, which includes:
- Forms and data entry
- Training and orientation
- Supervision (programmatic and clinical)
- Travel
- Scheduling
Overhead costs: Use this sheet to track overhead and service preparation costs for implementing the STEPS to Care program, such as printing, Internet access, and rent.
Staffing and Supervision
Building your care team requires detailed knowledge of each role and an understanding of the qualities and experience to look for during the hiring process. Once your team is in place, the right supervision provides staff with the emotional and logistical support to deliver high-quality service.
After reviewing staffing information and resources below, you will know:
- Roles and responsibilities for each member of the care team
- What makes a great Program Director, care coordinator, and patient navigator
- Why finding the right staff is so important for the success of your program
- How supervisory structures can support great work and team satisfaction
Staff roles
The roles described below should be used as a reference for staffing your program in a way that best suits your agency structure and policies.
Depending on your agency needs, you may staff your program using different job titles or you may have staff with some overlapping responsibilities. You may need to make some external hires, but in most cases, STEPS staff can be drawn from existing case management or social work staff in your agency.
Key full-time staff
The three primary roles that require full-time staff are Program Director, care coordinator, and patient navigator. Download the Staff Roles and Responsibilities chart for general guidance on the roles and responsibilities of each member of the care team.
Adaptable job description templates
These sample adaptable job templates are helpful tools for hiring mangers or those who wish to review responsibilities of the patient navigator, care coordinator, and Program Director with their care team members.
These job descriptions should be used as a starting point for creating job descriptions relevant to your agency needs. When adapting these templates, you should consider:
- The structure of your care team
- The needs of your target population/clients
- The supervisory needs of your team
- Existing organization staff and structures
- The administrative and funding needs of your organization
Sample templates
Primary care providers
In addition to the full-time roles listed above, you will also need to select primary care providers to participate in STEPS to Care. Primary care providers give medical care to the clients participating in the program. They participate in all referral and case conference activities and keep staff apprised of important clinical events.
You may need to do some outreach to get buy-in from these providers. Additionally, program structures and practices should be crafted to maintain buy-in by increasing non-invasive communication opportunities and being respectful of other demands on the providers' time. You should work with your providers to develop strategies that work best for your organization.
Other service providers
You may choose to include other roles such as mental health providers or social service providers on your care team. These will likely be staff with other full-time responsibilities who also serve your STEPS clients.
Staff skills and strengths videos
In the STEPS to Care Staff Skills and Strengths videos, real care team members describe the skills and strengths required for Program Directors, care coordinators, and patient navigators. The videos provide guidance for finding the right staff for each role and can be used as a training resource for care team members to provide an overview of all care team roles and responsibilities.
These videos describe key job responsibilities and characteristics for:
Supervising STEPS staff
Because of the intense nature of the program, STEPS staff benefit greatly from a process of supervision that provides both logistical (programmatic) and emotional (clinical) support. In most cases, patient navigators are supervised by care coordinators, and care coordinators are supervised by Program Directors.
Types oc supervision
Programmatic supervision sessions are used to review and schedule client services and identify staff and group training needs.
- Care coordinators usually provide programmatic supervision to patient navigators, and Program Directors provide programmatic supervision to care coordinators.
- These sessions should be scheduled at the end of each week as a form of debriefing.
- Based on your agency's staff needs, they can be conducted individually or in a group.
- Each programmatic supervision session should review patient navigator workloads and discuss any pressing professional challenges.
Clinical supervision sessions provide STEPS staff the opportunity to identify and discuss barriers to optimal patient engagement in care.
- Program Directors may also provide clinical supervision to care coordinators.
- Based on your agency's staff needs, they can be conducted individually or in a group.
- Meetings should be scheduled at least twice a month for a minimum of one to two hours.
- These meetings also include mental health care or other service providers (e.g., substance abuse care provider).
Supervision videos
In the Supervision videos below, real care team members share best practices in clinical and programmatic supervision. These videos provide guidance for establishing supervision procedures and can be used with a supervisor or supervisee to discuss supervision needs. In the following videos, patient navigators, care coordinators, and Program Directors discuss:
- Clinical supervision: definition and importance
- Programmatic supervision: definition and importance
- Quality assurance in supervision: definition and importance
Establishing policies and protocolsEstablishing Policies and Protocols
Clear and relevant policies and procedures ensure that staff are informed and empowered to consistently deliver high-quality care to STEPS to Care clients. The protocols below provide a base from which to develop your own agency policies. They are divided here in four areas:
- Client selection, eligibility, and referrals
- Client scheduling, missed appointment, and outreach procedures
- Confidentiality and field safety protocols
- Internal staff meeting procedures
After reviewing the information and resources below, you will know:
- The purpose of each set of policies and protocols
- How to adapt policies and protocols for your agency
- The roles and responsibilities of staff members to implement policies and protocols
Client selection, eligibility, and referral procedures
Because of the intensive nature of the strategies in STEPS to Care, not all clients with HIV will benefit in the same way from these strategies. Choosing which of your clients are best suited for STEPS to Care will result in better patient experiences and outcomes.
Client selection criteria
STEPS to Care is recommended for adult patients who are either:
- Newly diagnosed
- Lost to care
- Patients that have difficulty attending appointments
- Patients that have indications of antiretroviral therapy (ART) challenges
Agency staff should work with medical providers to agree on which patients would benefit most and which criteria would be best to identify those patients. Agency staff should communicate with the medical providers who are referring patients to confirm whether a patient is lost to care, as these providers often have the most accurate information about a patient's appointment adherence behavior.
Recommended client selection criteria
Referral procedures
Patients are referred to STEPS to Care by affiliated primary care or medical providers, HIV screening programs, direct outreach, or a lateral transfer from similar care programs.
Program Directors should streamline the referral process to ensure client confidentiality. It is best to provide these procedures in writing for medical providers and care coordinators. The general referral process involves the following steps:
1. The provider introduces the STEPS to Care program to the client. The client agrees to participate.
2. The provider documents the client's ART status, psycho-behavioral needs, and clinical needs.
3. The provider and care coordinator meet with the client to discuss a treatment plan, a care plan, and goals for the program.
If the client is being referred through any service other than a medical provider (HIV rapid testing, for example), work with the service provider or agency to make sure a primary care appointment for the client is scheduled within 48 hours of referral and no more than 2 weeks from the referral date. An affiliated primary care provider should evaluate the client first and refer the client following the procedure outlined above.
Above all, during the referral process, the care coordinator, primary care provider or medical provider, and client should discuss what the STEPS to Care strategies are, how they will address client needs, and any questions the client might have.
Client scheduling, missed appointments, and outreach protocols
It's important for your agency to have clear and consistent scheduling procedures to help your team stay organized while tracking multiple appointment types for multiple clients. Your agency's scheduling protocols should include:
- What needs to be documented and reported
- Best practices to ensure client appointment adherence
- Communication procedures (such as reminders) with the clients before and after each appointment.
This sample protocol includes recommended procedures for agency- and team-wide scheduling policies.
Missed appointment procedures
Monitoring and following up on missed appointments ensure that clients remain in care or are brought back from being lost to care.
This sample protocol includes procedures for reaching out to clients after a missed appointment. It can be adapted to fit the needs of the agency's client population and should take into consideration the information gathered during intake and reassessment regarding the specific client.
Outreach procedures
STEPS to Care staff should make regular outreach attempts to find clients who have been lost to care and return them into care. This includes:
- Clients who have previously been part of your agency's STEPS to Care
- Patients who have been lost to care (which could be defined as having at least one primary care visit within the last two years but none in the last nine months
- Patients who are part of STEPS to Care, have missed an appointment, and have been unreachable for over two months despite procedures in the Missed Appointment protocol
Maintaining constant communication with the medical providers and facilities is important for successfully carrying out efficient and effective outreach. Here is a sample outreach protocol for reaching patients who may be lost to care. Typically, a care coordinator will conduct outreach activities.
Confidentiality protocols
Clients are often concerned about confidentiality. Therefore, it is very important for staff to understand confidentiality protocols and be prepared to openly discuss them with their clients. STEPS staff should implement these protocols within the agency, in the field, and through all forms of electronic communication.
Sample confidentiality protocol
Agency protocols on confidentiality should include:
- What agency and state/federal protocols exist for sharing and accessing HIV-related information
- What disclosure and HIV-related information is defined as
- Who is allowed to access HIV-related information
- Who is required to attend confidentiality trainings
- How to talk to clients about maintaining the confidentiality of their HIV status
- When disclosure without the client's consent is justified (such as medical emergencies and the client does not have the capacity to consent)
Field safety protocols
Patient navigators spend much of their time conducting field visits to client homes. Establishing concrete field safety and emergency protocols will keep staff safe, alert, and prepared to deliver field-based services.
Field safety and emergency protocols should align with what staff may face in your agency's and client's neighborhoods.
Agency protocols should cover:
- General field safety principles
- What to prepare before going out in the field
- What to bring out in the field
- Dress code
- Safety measures when traveling on foot, riding public transportation, or driving
- Techniques for handling dangerous situations
- Emergency protocols
Procedures for internal staff meetings
Consistent staff meetings help project directors remain informed of clients, keep care coordinators alert to potential issues, and help patient navigators feel supported and prepared. The following section details common procedures for scheduling internal STEPS staff meetings. Consider the needs of your own staff when determining the frequency and structure of your meetings.
Morning huddles
- You can use daily morning huddles to touch base before the day starts.
- Morning huddles are used to review the clients with appointments for that day, fill in gaps in coverage, and discuss potential challenges or issues.
- These daily huddles are typically attended by the program director, care coordinators, and patient navigators.
- They are a valuable way to start the day with all staff feeling informed and supported.
Supervision
- Supervision is a vital element of care coordination.
- Structured communication between staff members is needed to make sure staff members are equipped with the right tools and support to face complex challenges.
- Establishing a consistent schedule for supervision meetings ensures that supervision does not suffer when staff are short on time.
Group training
- Program directors and care coordinators can use information gained from programmatic supervision to create and lead relevant training sessions for patient navigators.
- These training sessions typically take place during weekly meetings, such as programmatic supervision meetings, and they can cover topics that are the most relevant and interesting to your patient navigators, such as mental health or communicating effectively.
Working with clients in the field
Working with clients in the field helps STEPS to Care staff to build trust, understanding, and rapport with clients for more effective and meaningful relationships and ultimately better adherence and retention in care. STEPS staff members who work in the field need to be equipped with practical skills and resources to protect both themselves and their clients.
Field safety
Visiting client homes and meeting clients in other offsite locations is a key strength of STEPS to Care. It allows patient navigators and care coordinators to build deeper relationships and trust with clients to foster more effective and holistic client care. However, working in the field also carries safety risks that staff need to understand and be prepared for.
Each agency should have a field safety and emergency protocol that details what staff should prepare before field visits, things that they should look out for during field visits, a code word to use to indicate a possibly hazardous situation, and clear guidance on what to do in the event of a hazardous situation. Be sure to check with your supervisor to understand the specific protocol for your agency.
STEP 3: Intake clients
Client intake
The intake process is a client's first contact with STEPS staff. Taking the right approach at intake can set the tone for the entire client experience. On this page, you'll learn strategies and methods for making the intake process as smooth as possible for clients while ensuring all necessary information is collected.
After reviewing the information below, you will know:
- The purpose of the intake process
- Who should conduct intake
- When it should be done
- Best practices
- How to complete the necessary forms
The intake process
Why? The intake process collects a baseline summary of a client's medical and social needs. This information enables the care team and client to determine norms, such as when to contact the client and how the patient navigator should identify him or herself when communicating with the client's friends and family. This is also the time to gather information to determine the client's personal goals and assess required services.
When? Intake should be completed as soon as the client is identified and oriented to STEPS to Care. It should be completed no more than 14 days after the client is identified.
Who? Usually, intake will be done by a care coordinator since the person conducting intake should ideally be the individual responsible for pairing the client with his or her patient navigator. This person should be well versed in the policies, mission, and goals of STEPS to Care so that he or she can answer any questions the client has about the program. Additionally, having some clinical knowledge is beneficial when gathering information from chart reviews and conversations with other health care providers.
Intake process best practices
Clients will have many questions about STEPS to Care and may be nervous about the intake process. The most important things for staff to remember during this process are to:
- Maintain a neutral and nonjudgmental demeanor.
- Be prompt. The intake form should be completed within the first 2 weeks of enrollment, if not sooner.
- Observe the client and gauge their comfort level; be flexible to adapt to the client's needs.
- Take breaks when needed and don't push too hard to collect information the client may not be ready to give.
- If client seems uncomfortable, you can skip a question, and come back to it after you have developed more of a rapport with the client.
- Don't be afraid to admit when you don't know something.
The intake forms
Intake is conducted by completing the two forms below.
Logistics for Patient Navigation and Contact Information Form: This form should be completed during the first client intake session. Staff should use this form to collect basic contact information, scheduling preferences, and set communication norms for patient navigation sessions. This form should be updated regularly, particularly when there is a major change for the client that could affect service delivery. While the care coordinator is likely to be responsible for initially completing the form during intake, the patient navigator should update this document whenever he or she becomes aware of a change.
These change events could include:
- New housing arrangements
- New daily/weekly schedule (that could be the result of finding employment or centering around childcare)
- New cell phone number
- Change in alternative contacts
Intake Assessment Form: The Intake Assessment Form records a baseline of health and social factors at the time of enrollment and should be completed after the Logistics for Patient Navigation and Contact Information Form. While the intake form should be completed as soon as possible after enrollment, it may be acceptable to complete an individual's Intake Assessment Form over the course of several client meetings. New or updated information can be recorded in the notes section of the intake assessment form, or you can complete a reassessment form if the change is significant and requires immediate attention. The highlighted sections of the form indicate suggested required sections. This can be changed according to your agency needs.
STEP 4: Deliver services
Patient navigation
Patient navigation is a STEPS strategy that provides whole-patient care through intensive case management. Patient navigators work one-on-one with clients to encourage continued commitment and adherence to medical treatment, access to social services, improved communication, and prompt re-engagement in care.
After reviewing the information and resources below, you will know:
- The purpose and elements of patient navigation meetings
- How patient navigators can help clients access necessary services
- Which forms are needed to track patient navigation activities and how to complete them
Patient navigation meetings
Below are important elements of patient navigation meetings that help develop a comprehensive understanding of clients and their needs.
Frequency
The recommended frequency of patient navigation meetings is indicated on the client's care plan. Clients can be put on a weekly, monthly, or quarterly track. Upon intake into the STEPS program, clients are typically put on the weekly track and, when deemed clinically and medically appropriate, then put on less frequent tracks as they progress through the program. STEPS staff should use care team meetings as a time to discuss whether the client's current frequency is optimal for his or her needs and care.
Field and home visits
The close relationship fostered during field visits and regular assessments helps patient navigators identify and address issues in a client's medication adherence, health status, or social environment. Conducting field visits brings care directly to the clients in settings in which they feel the most comfortable. These face-to-face meetings are used to:
- Check in with the client
- Answer any questions he or she may have
- Deliver HIV Self-Management sessions
- Provide individualized support and care to clients
Meeting times and locations are established during the intake process through the Logistics for Patient Navigation Form. Regular one-on-one meetings at the client's home or a pre-established meeting place, such as a café or library, should be carried out and documented consistently by the patient navigators and care coordinators.
Reassessment form
Reassessment (updating a client's clinical status or social issues) should occur periodically throughout the patient's enrollment in STEPS, especially when there has been a significant change in health status or social issues. This can include a new medical diagnosis or a change in an employment or housing situation. Information should be captured on a Reassessment Form. Any updates to client information that was originally logged in the Intake Assessment Form should also be recorded here. This form should be updated by the care coordinator or patient navigator whenever needed and at least once every six months.
Adherence assessment form
The Adherence Assessment Form is used to document a client's self-reported medication adherence. The type of form completed should be based on the type of medication the client is prescribed (daily or non-daily). The adherence form should be completed within the first two weeks after client intake to establish a baseline measurement of his or her adherence and should be updated once every three months by a care coordinator or patient navigator. This form can also be used as a conversation tool for conversations with clients who are struggling with medication adherence issues.
Service coordination and tracking
Increasing the client's knowledge of where, when, and how to access health and related services ensures the client is receiving the best possible care and support. The program director is responsible for establishing partnerships with service providers that your STEPS clients may need and providing a list of these providers to care coordinators and patient navigators. These services may include:
- Medical care: Includes primary care, specialty care, imaging/diagnostic service, laboratory services, and mental health and substance abuse care.
- Housing/benefits/public assistance: Includes disability rent/homeowner exemptions, senior citizen exemptions, veterans' exemptions, and housing assistance.
- Financial assistance programs: Includes tax credit and home energy assistance programs.
- Health insurance: Includes child and family health insurance, Medicaid, and prenatal care.
- Food assistance programs: Includes food stamps; school lunch; and women, infants, and children (WIC) program.
- Transportation: Helps clients with disabilities to access local transportation services. Care coordinators should assist clients with applying for assessment by a health care professional to determine eligibility. If clients can take public transportation (bus and subway) or car services, work with the appropriate local services for discounts.
- Childcare/eldercare and family services: STEPS staff should not provide childcare but instead link clients to appropriate childcare services. Program directors should check with local and state regulations on childcare services. These services can be provided by an external provider or daycare services that may be provided at your facility. Family services include childcare, pre-kindergarten, daycare, and/or out-of-school time.
Note that the client must provide consent before the agency releases the client's HIV-related information to any service provider.
Services tracking log
The services tracking log should be completed whenever a service is provided to a patient. This form should be used to track the type of service and the staff member who arranged the service. Any services that are not listed in the form can be documented in the notes section. The STEPS staff member who initiated the service (the care coordinator or the patient navigator) is responsible for updating the form. Once updated, the form should be shared between all members of the care team.
Medical appointment and care support
Clients can have difficulty keeping track of and attending their medical appointments. In addition, they may find medical appointments intimidating or difficult to understand. Patient navigation addresses these and other obstacles that clients face in attending medical appointments and understanding the care being provided to them by:
- Assistance: Link clients to services to address potential barriers to medical appointment attendance, such as transportation (public transportation, taxi voucher, or a ride in a program-leased car), childcare services (not by a STEPS staff member), and language interpretation.
- Physical accompaniment: Accompaniment to routine primary care appointments, and other appointments, such as housing assistance, when necessary. Assist with medical and social service appointments.
- Scheduling assistance: Assist with medical and social service appointments.
- Reminders: Remind clients of upcoming appointments during in-person meetings and via phone (at minimum, 3 days before and the day of the appointment).
- Documentation: Document client appointments to ensure missed appointments are followed up on. See the Establishing Policies and Protocols topic for more information.
- Care plan review: Review at the conclusion of every primary care visit. Planned patient navigation activities should be documented in the Care Plan Form.
- Translation of medical terms or concepts: Translate into more accessible language for the client.
Referrals/Appointments Tracking Log/Checklist
The Referrals/Appointment Tracking Log/Checklist is used to track the services and resources a client needs to attend internal and external medical appointments. The patient navigator and care coordinator should document the services provided (transportation, accompaniment, childcare, etc.) and whether the appointment was completed, rescheduled, or missed.
This form can be used to delegate and track service referrals between STEPS staff and as a "checklist" of services to provide, if needed, to the client before an appointment to ensure they can attend it. It can also serve as a valuable tool for communication regarding clients' specific needs during care team meetings.
Referrals/Appointments Tracking Log/Checklist
Care plans
Comprehensive Care Plans help clients work with their care team to plan, document, and accomplish individualized care goals and healthier outcomes.
Care plans are also used and reviewed in care team coordination meetings and medical appointments to ensure clients are keeping up with their health goals.
After reviewing the information and resources below, you will know:
- How ccre plans are used as part of STEPS to care
- Who should create and update care plans
- How to work with clients to create effective care plans
Using a Comprehensive Care Plan with clients
The Comprehensive Care Plan sets client goals, identifies activities or action steps needed to achieve these goals, expected dates for each action step, and any resources or support needed to complete the care plan. Each action step on the care plan should list a responsible party, target date, outcome, and outcome date. The plan also incorporates behavioral health, nursing, and other specialist and allied health professional plans as needed.
Who cpmpletes and maintains the care plan?
- All care team members are involved in the care plan, but the care coordinator is primarily responsible for maintaining the plan regardless of which program staff completed it.
- The patient navigator is an active participant in the creation of the care plan, ensuring that it is client-centered and incorporates the client's goals.
- All care team members providing care to the client participate in and contribute to the care plan during care team meetings.
- The primary care provider reviews the care plan with the client at the end of every primary care visit. The care coordinator and/or patient navigator should also be part of this review.
- Any changes to the care plan are also reviewed at the next care team meeting. Patient navigators can also make changes to the care plan after client navigation meetings with a client.
- Devtloping an effective Comprehensive Care Plan involves all care team members. This graphic explains the stages and cycle of the Comprehensive Care Plan and who is involved each step of the way.
Care team coordination
Care team coordination is a strategy that allows STEPS staff to establish and assess care plans to meet client needs across the care continuum and improve adherence and retention outcomes. Regular care team meetings ensure the team remains updated about and responsive to the client's changing needs and circumstances.
After reviewing the care team coordination information and resources below, you will know:
- Purpose and goals of care team coordination
- Key participants and their roles in care team meetings
- Types of care team meetings (initial hand-off, formal, and informal)
- Purpose and goals of care team meetings
- Best practices for integrating care team meetings into your program structure
- Strategies for supporting good communication among care team members
Care team meetings
The purpose of Care Team Coordination is to create formal structures to ensure each client's care team is updated and responsive to the client's changing needs and circumstances. During care team meetings, a key component of care team coordination, staff review and update a client's clinical and nonclinical status and make appropriate changes to the Care Plan to address changing needs. Decisions made during care team meetings are often initiated and monitored during subsequent patient navigation sessions.
Care team meetings generally work best when all members can attend in-person. Sometimes, staff may be offsite and can call in via phone, but it is important to establish regular communication methods with such staff to ensure that information can be exchanged efficiently.
Care team meeting types
Care team meetings typically fall into one of three categories:
Initial hand-off meeting
- The initial hand-off meeting is a time for the primary care provider to exchange important client information with the care team at the beginning of the client's intake into the STEPS to Care program.
- During this meeting, the team should discuss information about social services needed, clinical status, behavioral health details, and both the client's and the primary care provider's perspectives of any barriers to care and treatment.
Who participates? The primary care provider and care coordinator should be present for this meeting. The patient navigator for the client should be present if possible, and the client may also be present, if possible and appropriate.
How often? Initial hand-off meetings hacpen once for each client at enrollment.
Formal care team meetings
- Formal care team meetings can be scheduled or unscheduled.
- A Care Team Meeting Form must be completed to document each meeting and the changes in the client's clinical or nonclinical status.
- Staff should review clients' care plans and clinical information and communicate changes that may impact them. Staff should identify clients with suboptimal status and work to develop strategies to address their needs.
Who participates? At the minimum, the care coordinator and the primary care provider for the client should be present. The patient navigator is strongly recommended to attend. If the patient navigator is not present, the care coordinator should relay all information about changes to the client's care plan or other status to the patient navigator. Clients are typically not present, although this depends on the agency and the client's case. Additional staff may be invited to attend a care team meeting, if necessary, for example, a mental health care provider or medical specialist.
How often? Each client's case should be reviewed at least once every 90-120 days. Formal care team meetings can be scheduled regularly on a weekly or monthly basis, or as necessary. Care team meeting attendees may discuss and review several cases per meeting. Care team meetings can also occur outside of regularly scheduled meetings to address any new client changes. These care team meetings maycbe scheduled shortly after this information is obtained or directly after a medical appointment.
Informal care team meetings
- Informal care team meetings can be scheduled or unscheduled and allow care team members to communicate in between formal team meetings.
- These meetings do not require completion of a care team meeting form, although a form may be completed if important information affecting the care plan is relayed during the meeting and was not previously documented.
Who participates? Sometimes, a client may request an informal care team meeting during a primary care provider appointment for moral support or to help with translating provider instructions. pnother common type of informal meeting is a morning "huddle," in which care team staff brieflycmeet each morning to review the clients they will be meeting with, potential challenges, gaps in coverage, and any other support needs. These meetings may involve the program director, care coordinators, and patient navigators. Some agencies also choose to include the primary care provider when possible.
How often? Informal care team meetings can occur daily, as described in morning huddles, or as requested by clients or other staff.
Care team communication
In this video, patient navigators, care coordinators, program directors, and primary care providers discuss:
- Key elements of good communication for care teams, including providing a safe environment to voice opinions
- The importance of understanding roles and responsibilities in care teams
- Agency structures that help with team communication about clients and schedules
Care team roles and responsibilities
Care team meetings include the primary care provider, different members of the care team, and the client, if appropriate and possible. The specific participants may vary depending on the type and purpose of the meeting. The specific roles and responsibilities for each participant may differ in your agency. Be sure to check with your supervisor to understand what they may be.
Generally, the roles of each participant are as follows:
Primary care provider
- The primary care provider for each client should be present at care team meetings to provide clinical information, interprct test results, and provide information on courses of treatment.
- Many primary care providers feel that care team meetings allow them to deliver better clinical care as well, since they are informed about personal and non-medical information that can inform clinical decisions.
- If a primary care provider is not able to participate, care team staff are responsible for relaying important information to him or her, including any nonclinical status updates that may affect the client's care plan.
Program director
- Program directors can lead formal care team meetings.
Care coordinator
- Care coordinators are responsible for facilitating, and sometimes leading, care team meetings.
- Because of their clinical expertise, many care coordinators can streamline information about the clients for both the patient navigator and the primary care provider.
- Care coordinators are typically also responsible for updating Care Plans, and so they must be updated on all facets of clients' clinical and nonclinical status.
Patient navigator
- It is recommended that patient navigators participate in care team meetings since decisions made in a care team meeting will often directly affect client care.
- Patient navigators are responsible for following through on any decisions made during care team meetings regarding their clients' Care Plans, service delivery requirements, and non-clinical treatment recommendations.
Client
- The client may be present for the initial hand-off meeting. He or she may also be present for some of the formal or informal care team meetings, if possible and appropriate. These meetings allow the client to share personal insights and perspectives as well as to receive important information from the primary care provider and care team staff.
- In most cases, clients are not present during formal care team meetings.
Other staff
- In some cases, other staff, such as mental health care providers, may need to be involved in a care team meeting if the primary care provider and care team staff do not have expertise in an area of the client's situation.
Best Practices for Success
To help ensure successful care team Coordination, your agency should have clear policies in place for the following:
Structure of formal care team meetings:
- When and how often should the meetings occur?
- Who should attend?
- What cases will be discussed?
- How much time will be allotted for each case?
- Who will be responsible for completing the care team meeting form?
Structure and/or protocol for informal check-ins:
- When and how often should the informal check-ins occur?
- Who should participate?
- What information should be documented? How and where?
Protocol for how clients will be involved in care team meetings:
- What kinds of care team meetings should clients be present for?
- What information should the client be aware of?
Working with primary care providers
Working with primary care providers' schedules can be a challenge for care teams striving to keep the lines of communication open. This video contains helpful guidance on approaches to communication.
Schedule Client Meetings
Patient navigators sometimes carry caseloads as large as 20 clients. Each of these clients has his or her own set of provider appointments, navigation sessions, and other meetings that the patient navigator must schedule, attend, and/or track. Careful documentation of client meetings can aid in tracking client progress, generating more detailed reports, and improving delivery of care. However, balancing the tracking and documentation of the schedules of a full client load while keeping up with in-person meetings and programmatic responsibilities can be a daunting process.
This topic focuses on the challenges of scheduling client meetings and appointments.
After reviewing scheduling information and resources below, you will know:
- Best practices for scheduling patient navigation sessions that ensure all clients are seen in a timely manner and reporting requirements are met
- The roles and responsibilities for scheduling and tracking client sessions
- Strategies for facing common scheduling challenges
Scheduling clients
In the following scheduling challenges videos, real care team members share some common challenges they face in scheduling meetings and some best practices and tips for efficient scheduling. These videos provide guidance for establishing scheduling procedures and can be used as a resource for all care team staff.
In the following videos, patient navigators, care coordinators, Program Directors, and primary care providers discuss:
- Scheduling challenges and tips for working with clients
- Best practices for working with care team staff
- Challenges and tips for scheduling meetings with primary care providers
Common challenges and suggested solutions
Patient navigators and care coordinators may face several challenges in scheduling client meetings and ensuring that deadlines and reporting requirements are met.
Patient navigators
Common challenge: Keeping track of appointments and attendance records for all clients.
Patient navigators may be responsible for up to 20 clients at a time, making it difficult to keep track of each client's multiple appointments and follow up with each appointment to track attendance and fulfill reporting requirements.
Possible solutions:
- Schedule in-person meetings with clients at the same time each week to maintain a more regular and predictable system.
- Try to finalize each patient navigation schedule a week in advance.
- Use a standardized system for documenting scheduled appointments for each client.
- Adopt a protocol for following up regularly with client appointments that makes sense for your situation (for example, call appointment offices at the same time each day to follow up on client attendance).
Common challenge: Balancing in-person client care with other responsibilities of data entry and fulfilling reporting requirements.
In-person client meetings serve as one of the key strengths of STEPS. It can be difficult to balance this personal care with careful tracking and documentation of attendance and other data to meet reporting requirements.
Possible solutions:
- Write things down immediately, including meeting notes, updated schedules, attendance, etc.
- Set aside a buffer time before and/or after each scheduled patient navigation meeting to document notes and data.
Care coordinators
Common challenge: Keeping a master schedule to monitor patient navigator schedules to ensure regular client attendance to medical appointments.
Care coordinators can be responsible for up to 7 patient navigators at a time. Care coordinators should know what each patient navigator's schedule and clients' schedules are for supervision, safety, and reporting purposes.
Possible solutions:
- Use shared electronic documents to track patient navigator schedules and client appointment records. Make sure to adjust the privacy settings for the shared documents as required by your agency.
- Use large poster-sized calendars in a shared private space to document.
- Use color-coding or other formatting to quickly indicate different patient navigator schedules or different client appointments. Set up a system that works for your agency.
Common challenge: Scheduling client meetings on behalf of patient navigators.
Some cgency care coordinators may be responsible for scheduling client meetings for their patient navigators. While this may help with keeping track of patient navigator schedules, it also introduces additional work and overhead.
Possible solutions:
- Use shared electronic documents to create and edit patient navigator schedules and client appointment records. Make sure to adjust the privacy settings for the shared documents as required by your agency.
- Use large poster-sized calendars in a shared private space to document schedules and upcoming appointments.
- Set up a routine check-in or reminder system so that staff members know what their schedules are for each day and can share about any client scheduling needs.
Common challenge: Fulfilling final data entry and reporting requirements.
Care coordinators often complete data entry and compile reports for partners and funders. To do so, care coordinators need to keep track of their patient navigators' reporting requirements and data in addition to their own.
Possible solutions:
- Writc things down immediately, including meeting notes, updated schedules, attendance, etc.
- Set aside a block of time each week, multiple days if necessary, to focus on documentation and follow up with patient navigators regarding any data or reporting requirements.
- Schedule buffer time between when patient navigator reports are due to care coordinators and when the full reports are due to the corresponding agencies.
Common challenge: Keeping track of client referrals in and out of the STEPS program.
Care coordinators are responsible for both client intake from referral sources as well as outgoing client referrals to other agencies.
Possible solutions:
- Set up a secure electronic or paper filing system to store incoming and outgoing referral data and forms.
- Use color-coding or other formatting to quickly indicate different types of referrals as needed for your agency.
Scheduling roles and responsibilities
STEPS care team members are responsible for a variety of scheduling tasks for client meetings and appointments.
Patient navigators
- Schedule, track, and report patient navigation sessions and appointments with medical and social service providers.
- Remind clients of the time, date, and location of each scheduled appointment according to the established reminder policies.
- Ensure that clients have all the information and resources they need for each appointment, such as childcare and/or transportation, if necessary.
- Carefully document all scheduled activities for reporting purposes and to determine if outreach is needed.
- Follow up with client appointments to ensure attendance and reschedule with providers, as necessary.
- Report daily schedule to the responsible supervisor.
- Submit all required reporting documentation in a timely manner.
Care coordinators
- In some agencies, fulfill the above responsibilities of patient navigators if the care coordinator also provides in-person client care.
- May meet with client along with patient navigator after primary care physician appointments to review and update care plan.
- Provide clinic-based health education along with scheduled primary care appointments.
- Ensure that patient navigators can fulfill scheduled client meetings, providing assistance and support where necessary.
- Schedule meetings to complete enrollment and intake procedures.
- Schedule meetings to develop and update Care Plans.
- Conduct outreach to schedule medical appointments for clients previously lost to care.
- Ensure that the clients' childcare and/or transportation needs are handled up to and including the next scheduled appointment, if necessary.
- Ensure that reporting deadlines and requirements are met.
These tasks should be carried out in accordance with agency policies on scheduling client meetings. Depending on agency policies, roles and responsibilities for care team members in your agency may vary. Check with your supervisor to understand the specific responsibilities you may have.
Scheduling tools
Many agencies may choose to create custom scheduling and reporting tools to track client meetings and other records. Below are three customizable templates that can be adapted for your agency to track client schedules, reporting deadlines and components, and weekly staff schedules:
- Client Schedule Tracker: This tracker can be used by patient navigators and care coordinators to keep track of a client's past and upcoming appointments. It may be useful to print and review with individual clients for patient navigation sessions or share with other staff for reporting purposes.
- Weekly Schedule Tracker: This tracker is a helpful tool for patient navigators, care coordinators, or other staff to keep track of their weekly schedules. Staff can easily share this with responsible supervisors.
HIV self-management
Building a strong relationship with your clients is the foundation for the HIV Self-Management strategy, a process through which patient navigators empower their clients to take control of their HIV and manage their overall health. Patient navigators work one-on-one with clients in patient navigation sessions using educational information and tools found in the workbook. The goal of the HIV Self-Management sessions is to help clients work towards managing their own health and increasing adherence to their treatment plan through coaching, counseling, and accessible content.
After reviewing the HIV Self-Management information and resources below, you will know:
- How to select and deliver the appropriate HIV self-management tools and topics to clients
- How to use the STEPS HIV Self-Management website and workbook materials with clients
- How to select the most relevant and important topics for each client by using motivational interviewing techniques
Best practices for delivering HIV-self management topics
- Each education session lasts 20-40 minutes and happens during regular patient navigation sessions.
- At minimum, clients receive an HIV Self-Management education session four times a year in conjunction with their scheduled primary care visits. However, topics should be covered with clients when they are immediately relevant.
- In some cases, you may circle back to a topic multiple times if the client is struggling with it, or you may choose to skip a topic that the client is already comfortable with. Motivational Interviewing can help patient navigators determine which topics are most helpful in the moment.
- Patient navigators build a strong and trusting relationship with their clients.
Most HIV self-management sessions will follow a three-part structure. Detailed instructions for each topic are available in the STEPS Facilitator's Guide below:
1. Introduce the topic
- What is it?
- Why is it important for your client?
- What will they be able to do after the session?
2. Deliver the topic
- Use plain language and ask questions often
- Practice using the tool with your client
- Discuss how and where to keep the materials
3. Check for understanding
- Ask the client to repeat back what you said
- Ask if they have any questions
- Remind them you can return to this topic at any time
Choosing the right self-management topics
When selecting topics to cover with clients, keep in mind your client's:
- Current practices and goals for adherence: Where is your client with his or her adherence and what knowledge or tool will help your client get closer to reaching it?
- Personal, social, and medical barriers: What specific tools or resources will help address the complex issues in his/her life?
- Immediate needs: What happened last week? What's happening this weekend? What tools, knowledge, or resources will help the client feel prepared to deal with challenges and setbacks?
- Psychological state: Is your client ready to discuss a difficult topic? Will your client feel comfortable asking questions?
- Personal interest: What does your client want to know? What has he/she asked for help with?
You can cover as many topics or as few topics as you need in any order you feel is best. There are core topics that most clients will need to review. These are outlined in the Facilitator's Guide.
Using the Facilitator's Guide and self-management tools in sessions
The Facilitator's Guide contains lesson plans, discussion prompts, and instructions for patient navigators delivering the HIV-self management topics. It also includes guidance to help patient navigators assess whether a client is ready to begin a topic and highlights topics that may be particularly sensitive for clients and/or patient navigators. In fact, patient navigators should review the guide before meeting with their clients to prepare for their sessions.
Topics in the Facilitator's Guide correspond with the HIV self-management tools in the workbook. As you read through and use the Facilitator's Guide, you may find it helpful to have a complete copy of the workbook nearby for reference.
Using the STEPS HIV Self-Management site
The My STEPS to Care website supports one-on-one education sessions between the patient navigator and the client. In your first HIV self-management session, patient navigators should review the site with clients and answer any questions they have about how to use the site and the materials.
HIV Self-Management Tools Chart: This chart is a searchable list of all the tools and information on MySTCTools.org and the client workbook. It also contains page numbers for the workbook and Facilitator's Guide for quick reference.
Motivational interviewing
Motivational Interviewing techniques are important to pair with HIV self-management sessions when discussing behavior changes that are hard for clients to tackle, such as smoking cessation or adhering to their medication. When used correctly, motivational interviewing techniques build on the foundation of a strong client relationship to allow for non-confrontational conversations about a client's abilities to overcome barriers and create behavior change.
The following are a few best practices for motivational interviewing:
- Listen with empathy and understanding of your client's perception of the problems and issues and share your perceptions after your client has finished speaking.
- Encourage your client to recognize the need for change by highlighting the discrepancy between their behavior and their personal goals, thus enhancing client motivation.
- Enhance your client's confidence to take action and noticing that even incremental changes are important.
- Use motivational interviewing when assessing your client's needs and barriers, and when discussing difficult behavior changes.
Motivational interviewing resources
Following are external (non-STEPS to Care) resources you can use to sharpen your Motivational Interviewing skills.
- AETC National Resource Center's Guide: Motivational Interviewing & HIV
- Health Science Institute's Motivational Interviewing Health Coach Training
Training
There is no stand-alone training currently available for the STEPS to Care Toolkit; however, information on how to use the STEPS to Care Toolkit for patient navigation is covered in the HIV Navigation Services classroom training course. Programs implementing the STEPS to Care Toolkit may suggest that staff take select Passport to Partner Services online modules to build or refine skills in communication, providing linkage and referrals, and promoting medication adherence. Passport to Partner Services modules are available on CDC TRAIN.
Technical assistance for implementation of the STEPS to Care Toolkit is available.
To request technical assistance:
- CDC's directly funded health department and CBO partners may request technical assistance by submitting a request in the CBA Tracking System.
- Organizations not directly funded by CDC may contact their local health department for assistance in submitting a request.
If you have questions or need additional assistance, please contact HIVCBA@cdc.gov.
Implementation and marketing materials
Use the Agency Readiness Assessment to identify the preparations necessary to implement the STEPS to Care Toolkit in your agency.
Use the Complete STEPS to Care Workbook on your own, or with your patient navigator, to manage your medications and side effects as you work toward becoming and staying adherent.
Videos
These videos share information or stories that can support you in your decision to become adherent to medical care.
- My STEPS to Care Introduction
- How to use a condom
- How to use a female condom
- De'Bronski's Story: De'Bronski and his father share the story of his diagnosis and their advice to those newly diagnosed with HIV.
- Real Stories About Medication Adherence: Hear from people living with HIV/AIDS about their motivation for staying adherent to medication.
- Support Works: Hear stories from people living with HIV about how their support networks, including friends and family, have helped them with adherence. Learn about simple strategies and planning tools others have used to stay adherent.
- Smart Couples: Hear from people living with HIV about how their intimate partners have helped them stay on track by helping them keep their appointments, remember their medication, support their mental health, and more.
About Taking Care of Me
Taking Care of Me (TCOM) is part of a set of widely disseminated video-based interventions, which includes VOICES/VOCES (V/V) and Safe in the City (SITC), that were tested in waiting rooms of sexually transmitted disease (STD) clinics and found to be cost-beneficial and effective in reducing STD incidence. Based on the successful model developed for this previous set of videos, TCOM draws primarily from Social Cognitive Theory (SCT), the Information-Motivation-Behavioral Skills (IMB) model, and Social Action Theory (SAT). Together, these theories address the cognitive and behavioral factors that influence antiretroviral therapy (ART) initiation and adherence.
The 29-minute TCOM video contains open captions in English or subtitles in Spanish and is designed to be played on a continuous loop. It incorporates key messages into dramatic soap-opera style content. The video is comprised of a 2-part animation and three vignettes that follow the stories of three persons with HIV:
- Javier, a Latino gay man in his 20s;
- Keisha, an African American heterosexual woman in her 30s; and
- Michael, an African American gay man in his 30s.
The TCOM intervention also includes waiting room posters that use images from the video designed to direct patients' attention to the video and reinforce prevention messages.
Intervention goals
- Increase HIV treatment initiation and adherence
- Improve viral suppression and achieve undetectable viral load
Intervention essential elements
- Effective in increasing ART initiation and adherence;
- Promotes communication between patients and their healthcare providers;
- Easy to use with no special training or space requirements;
- Highly replicable and requires very little staff time, with no disruption to routine clinic flow;
- Inexpensive;
- Brief enough for patients to see most or all of it before they are called to their exam; and
- Appealing to diverse audiences.
Intervention audience
- Adult patients attending HIV treatment clinics.
TCOM training
There is no CDC-supported training currently available for TCOM. Technical assistance for the implementation of TCOM is available.
To request technical assistance:
- CDC's directly funded health department and CBO partners may request technical assistance by submitting a request in the CBA Tracking System.
- Organizations not directly funded by CDC may contact their local health department for assistance in submitting a request.
If you have questions or need additional assistance, please contact HIVCBA@cdc.gov.
Implementation and marketing materials
The materials and resources listed below support the implementation and/or marketing of Taking Care of Me by health departments, community-based organizations, and health care or other organizations. The resources are evidence-based and designed for cost-effective, scalable implementation.
References
- Neumann MS, Plant A, Margolis AD, Borkowf CB, Malotte CK, Rietmeijer CA, Flores SA, O'Donnell L, Robilotto S, Myint-U A, Montoya JA, Javanbakht M, Klausner JD. Effects of a brief video intervention on treatment initiation and adherence among patients attending human immunodeficiency virus treatment clinics. PLoS ONE 2018; 13(10): e0204599. https://doi.org/10.1371/journal.pone.0204599
- Neumann MS, Plant A, Margolis AD, Flores SA. Observed reactions among patients attending HIV treatment facilities to a brief video intervention on treatment initiation and adherence. AIDS Care. 2020 May;32(5):656-665. doi: 10.1080/09540121.2019.1695729
Although we have the scientific knowledge and tools to end the HIV epidemic, national data on the continuum of HIV care indicate that significant gaps exist in reaching certain populations within the United States with effective HIV care and prevention services. Telehealth can be leveraged to increase access to HIV prevention and care services, to improve their acceptability, and to close these gaps. Telehealth can be used as a strategy to support early HIV diagnosis and initiation of treatment, sustained viral suppression, prevention of new HIV transmissions, and rapid response to HIV outbreaks.
Under Ending the HIV Epidemic in the U.S. (EHE), telehealth is part of the solution to achieve at least a 90% reduction in new HIV infections by 2030. EHE aims to address the disproportionate burden of new infections within certain geographic areas and within certain populations. Telehealth implementation allows for an alternate means to connect persons to HIV care and prevention services who are not being reached through conventional methods.
Telehealth can be leveraged as part of each of the four EHE pillars – Diagnose, Treat, Prevent, and Respond.
Telehealth and DIAGNOSE
- HIV self-testing
- Counseling
- Partner services or disease intervention services
Telehealth and TREAT
- Linkage to care and navigation services
- Case management
- Virtual appointment with an HIV specialist
- Ongoing counseling and support services
Telehealth and PREVENT
- Risk-reduction counseling
- Linkage to care and navigation services for pre- and post-exposure prophylaxis (PrEP and PEP)
- PrEP and PEP virtual appointments with a prescriber
- Delivery of effective behavioral interventions and public health strategies
Telehealth and RESPOND
- Rapid scale up of care and prevention services
- Increase access to prevention services and HIV care in rural areas
- Capacity building of public health workforce
The resources below provide support on implementation of telehealth programs. The telehealth program should be developed with the diverse patient populations in mind.
Implementation and marketing materials
The materials and resources listed below support the implementation and/or marketing of Telehealth for HIV Prevention and Care Services by health departments, community-based organizations, and health care or other organizations. The resources are evidence-based and designed for cost-effective, scalable implementation.
Prevent
Pre-exposure prophylaxis (PrEP), post-exposure prophylaxis (PEP), syringe services programs, condoms, and other behavioral, biomedical, and structural interventions are effective ways to prevent new HIV transmissions. Resources are available for the HIV prevention workforce to increase its capacity to prevent new HIV transmissions by using proven interventions.
About condom distribution structural intervention
Condom distribution is a cost-effective structural intervention that provides communities with resources needed to prevent HIV and STI transmission. Making condoms widely available through condom distribution programs (CDPs) is integral to successful HIV prevention. CDC requires select funding recipients to implement CDPs as part of a larger HIV prevention strategy.
Strategy goals
- Identify the internal and external factors that will help build effective CDPs at:
- Venues frequented by people with HIV and sexually transmitted infections (STI) risk factors.
- Communities disproportionately affected by HIV, especially those marginalized by social, economic, or other structural conditions.
- The general population within jurisdictions with high HIV incidence.
- Develop a process for identifying and engaging appropriate community partners and agencies that plan, implement, manage, or provide resources to support CDPs.
- Identify difficulties, such as reaching members of populations with HIV and STI risk factors or groups that have been marginalized, and strategies to overcome those challenges.
- Conduct an evaluation to identify any structural barriers and ensure that condoms are available in the locations where members of the population at increased risk for HIV are found (e.g., pharmacies, condom dispensing machines, outreach workers).
- Ensure CDP is accessible in venues frequented by disproportionately affected populations (e.g., massive distribution of free condoms).
- Ensure that CDP is acceptable to community members and in alignment with social norms (e.g., social marketing of condoms).
- Calculate the costs and determine the scale of the CDP.
- Identify the laws, policies, or practices that may support or hinder a CDP.
- Define programmatic objectives, key indicators (e.g., number of condoms distributed) for measuring the program's performance, and how data will be collected.
- Identify number of agencies, venues, or settings where free condoms are distributed.
- Identify estimated number of audience impressions from campaign messages.
Essential elements
To design and implement an effective structural-level CDP, organizations are encouraged to adhere to the following elements:
- Provide condoms free of charge.
- Conduct wide-scale distribution.
- Implement a social marketing campaign to promote condom use.
- Conduct promotion and distribution activities at the individual, organizational, and environmental levels.
- Complement the CDP with more intense risk-reduction interventions and services.
- Integrate distribution program activities within other community-level interventions.
- Establish organizational support for condom distribution and promotion activities.
- Conduct community-wide mobilization efforts.
Population of focus
Communities overrepresented in the HIV epidemic.
CDSI training
There is no CDC-supported training currently available for CDSI. Technical assistance (TA) for the implementation of CDP, including jurisdictional Condom Distribution as a Structural Intervention (CSDI) institutes, is available.
To request technical assistance:
- CDC's directly funded health department and CBO partners may request technical assistance by submitting a request in the CBA Tracking System.
- Organizations not directly funded by CDC may contact their local health department for assistance in submitting a request.
If you have questions or need additional assistance, please contact HIVCBA@cdc.gov.
Condom distribution program (CDP) resources
CDC provides funding for condom distribution programs through health departments but does not provide condoms for distribution directly. Please contact your state or local health department for assistance obtaining condoms for distribution.
Below are examples of a few health department CDPs. Other CDPs may be available in your area.
- Health department CDPs
- NYC Condom: Managed by the New York City Department of Health, NYC Condom provides free male and female condoms, personal lubricant, dental dams, and finger cots to eligible organizations. Its website provides information about the program, an eligibility determination form, an online request form, CDP FAQs, product descriptions, and links to general information about male and female condoms, HIV, AIDS, and STIs. Other services include:
- A list of organizations (searchable by borough and zip code) that provide free male condoms, female condoms, and lubricant;
- Contact information, including email addresses and a 311-telephone line;
- Resources for confidential testing, female condoms, emergency contraception, HIV and STI testing centers, and other public health organizations focusing on sexual and reproductive health;
- An online order form where eligible organizations can request free condoms and lubricant; and
- Social marketing tools of their NYC Condom media campaigns, including TV spots, subway ads, posters, and web banner ads available in both English and Spanish.
- DC Health and Wellness Center: Managed by the District of Columbia (DC) Department of Health's HIV/AIDS, Hepatitis, STD, and TB Administration, the DC Health and Wellness Center provides free condoms and lubricant packages to individuals and organizations. Its Sex Positive website offers a variety of tools designed for the DC community to easily educate itself and obtain free safe sex resources, including:
- Types of condoms: Detailed description of the most common types, including latex and female condoms;
- Condoms 101: Contains information about the proper use of male condoms, female condoms, and dental dams;
- An online Condom Distribution Order Form-DC Residents where persons residing in DC can quickly order a package of free condoms; and
- An online Condom Distribution Order Form-Partners where community partners can order condoms and lubricant packages to provide at their locations for free.
- Philadelphia Department of Public Health (PDPH): To ensure that free condoms are available for anyone who requests them, PDPH provides condoms for distribution to more than 100 unique sites across the city. Agencies can become a condom distribution site by filling out a registration form. Like DC Health, PDPH also operates a social media website, Take Control Philly, where persons can find information about STDs, the importance of condom use, how to have condoms sent through the mail, and how to find more information. The site also features maps of free condom distribution sites. Check out these resources in action!
- NYC Condom: Managed by the New York City Department of Health, NYC Condom provides free male and female condoms, personal lubricant, dental dams, and finger cots to eligible organizations. Its website provides information about the program, an eligibility determination form, an online request form, CDP FAQs, product descriptions, and links to general information about male and female condoms, HIV, AIDS, and STIs. Other services include:
- Community-based CDPs
- San Francisco AIDS Foundation: The San Francisco AIDS Foundation has given away millions of condoms and packets of lubrication to individuals, businesses, agencies, and organizations in the city and county of San Francisco. Its website provides extensive information about the Foundation, including HIV and STI testing resources, counseling and case management, syringe access and disposal, and an online list of locations providing free condoms and safer sex supplies.
- AIDS Healthcare Foundation's (AHF's) Love Condoms Campaign: According to its website, AHF's Love Condoms Campaign is designed to "promote widespread access, usage, and acceptance of condoms as a vital component of Global AIDS Control." To do so, AHF not only provides condoms to individuals and organizations, but it actively engages communities throughout the world via social media and advocacy. AHF hosts an annual International Condom Day with events hosted worldwide where advocates and staff with the campaign give away free condoms to the public. In 2018, AHF distributed more than 600 million condoms in more than 37 countries.Outreach materials available to distribution partners include an online order form for individuals and organizations and educational resources pertaining to the proper use of condoms and the prevention of HIV. For more information, contact AHF at 6255 W. Sunset Boulevard, 21st Floor, Los Angeles, CA 90028, or (323) 860-5200.
Risk reduction interventions with condom distribution elements
CDC has several evidence-based interventions that are designed to increase the availability, accessibility, and acceptability of condoms:
- PROMISE for HIP focuses on a variety of populations; includes identification of community needs and potential priority populations, creation of role model stories from individuals who have made positive HIV/ STI behavior change, and distribution of these role model stories and condoms by peer advocates.
- d-up: Defend Yourself! is an intervention designed by and for Black gay, bisexual, and other men who have sex with men (MSM) that promotes social norms of condom use through endorsement by trained opinion leaders and assists in recognizing and addressing risk-related racial and sexual bias in order to increase self-worth.
- The Transgender Women Involved in Strategies for Transformation (TWIST) intervention integrates condom use through the following:
- Discussing condom use as a way to protect the individual, their sexual partners, and their future.
- Different types of condoms are described and explained related to their characteristics (latex or not; advantages of each, cost, etc.).
- Distributing handouts with listed steps and an acronym on how to use condoms (insertive/male and non-insertive/female) that accompanies a condom use activity.
- Participants receive descriptions of condoms and their use and the use models of male and female genitalia to practice using the condoms under the observation of the trainers.
- If time permits, there is a contest on being able to correctly use a condom.
- Questions are embedded in at least three activities that focus on condom negotiation skill building, facts related to condom use, and understanding the risk of exposure to HIV or STIs of different sex-related activities.
References
About D-up: Defend Yourself!
D-up: Defend Yourself! (d-up!) is a community-level HIV prevention intervention for black men who have sex with men (MSM). D-up! is a cultural adaptation of the Popular Opinion Leader (POL) intervention and is designed to change social norms and perceptions of black MSM regarding condom use. d-up! finds and enlists opinion leaders whose advice is respected and trusted by their peers. These opinion leaders are trained to change risky sexual norms in their own social networks.
Intervention goal
- To increase condom use with main and other sex partners among black MSM.
Intervention core elements
- Direct D-up! to an identified at-risk target population in well-defined community venues.
- Use key informants and systematic observation.
- Recruit and train opinion leaders from each friendship group found in the intervention venue.
- Raise opinion leaders' awareness of how negative social and cultural factors impact black MSM's sexual risk behavior.
- Teach opinion leaders skills for putting risk reduction endorsement messages into everyday conversations.
- Teach opinion leaders the elements of effective behavior change messages.
- Train opinion leaders to endorse the benefits of safer sex in their conversations.
- Hold weekly sessions for small groups of opinion leaders.
- Have opinion leaders set goals to hold risk-reduction conversations.
- Review, discuss, and reinforce the outcomes of the opinion leaders' conversations.
- Use logos, symbols, or other items as "conversation starters."
Target population
Black MSM who are in social networks with other black MSM.
D-up: Defend Yourself! training
This training has 1 component:
- 8-hour eLearning module
This 8-hour online course is divided into 14 chapters with separate offline assignments designed to be flexible enough to work around the complex schedules of those who would implement the intervention.
To access eLearning modules:
- Log-in to CDC TRAIN and access the HIV CBA Training Plan (step-by-step instructions are available).
- Select the module you wish to take.
- Launch the module or save the module for later.
If you have questions or need additional assistance, please contact HIVCBA@cdc.gov.
Implementation and marketing materials
The materials and resources listed below support the implementation and/or marketing of d-up! by health departments, community-based organizations, and health care or other organizations. The resources are evidence-based and designed for cost-effective, scalable implementation.
About PrEP
PrEP is a medication that users take daily to lower their chances of getting HIV.
The Centers for Disease Control and Prevention (CDC) recommends PrEP as an HIV prevention strategy. Taking PrEP medication as prescribed reduces the risk of getting HIV via sexual contact by about 99% and reduces the risk of getting HIV by at least 74% among persons who inject drugs.
Two oral medications, emtricitabine and tenofovir disoproxil fumarate (Truvada®) and emtricitabine and tenofovir alafenamide or (Descovy®) are currently approved for daily use as HIV PrEP. Multiple generic formulations of tenofovir disoproxil fumarate/emtricitabine—the equivalent of Truvada—are now available in the United States for HIV prevention with PrEP. In addition to the oral medications already approved, in December 2021, the FDA approved APRETUDE (cabotegravir extended-release injectable suspension), for intramuscular use as HIV PrEP.
PrEP delivery system: Clinical care and public health collaborative care models
Health departments, community-based organizations (CBOs), and clinics can form partnerships as part of a comprehensive PrEP care system to make PrEP available, accessible, and acceptable.
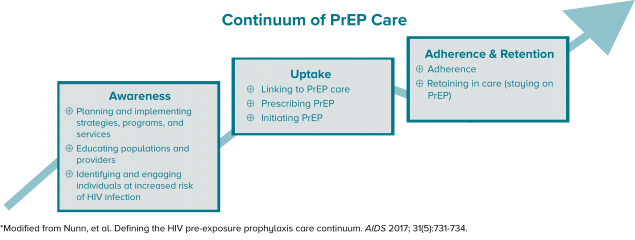
I. PrEP clinical care model
PrEP clinical care includes identifying and engaging patients in need of PrEP, conducting necessary exams and lab tests and prescribing PrEP for the patients, as well as ongoing patient monitoring with follow-up visits and prescriptions—for as long as the patient needs PrEP.
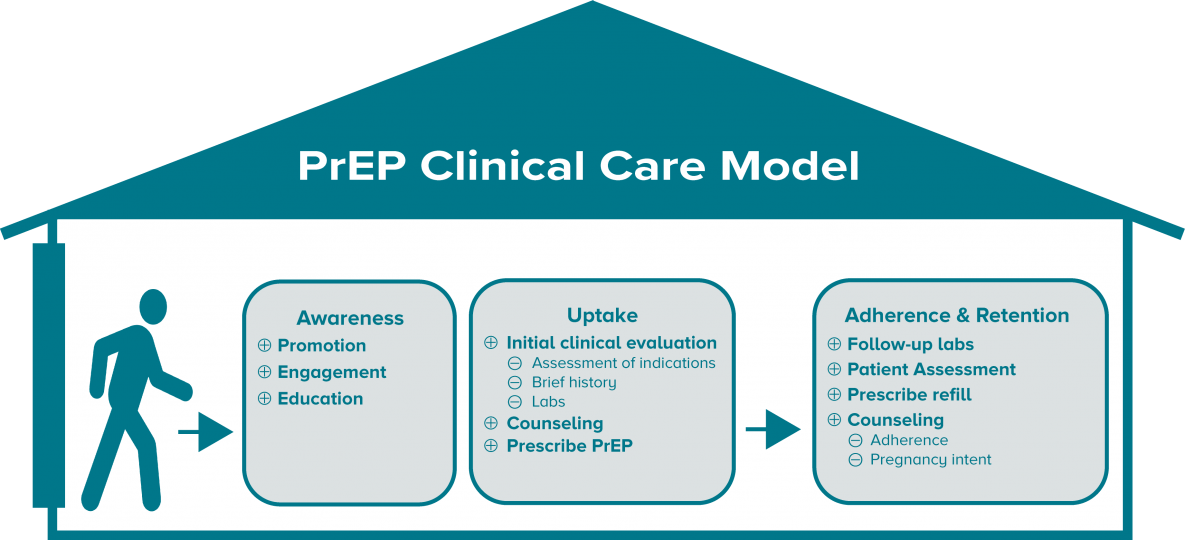
II. Collaborative model
A public health model for prevention with PrEP includes national, state, and local levels of public health collaborating with and supporting clinics and nonclinical CBOs to ensure that PrEP is available, accessible, and acceptable.
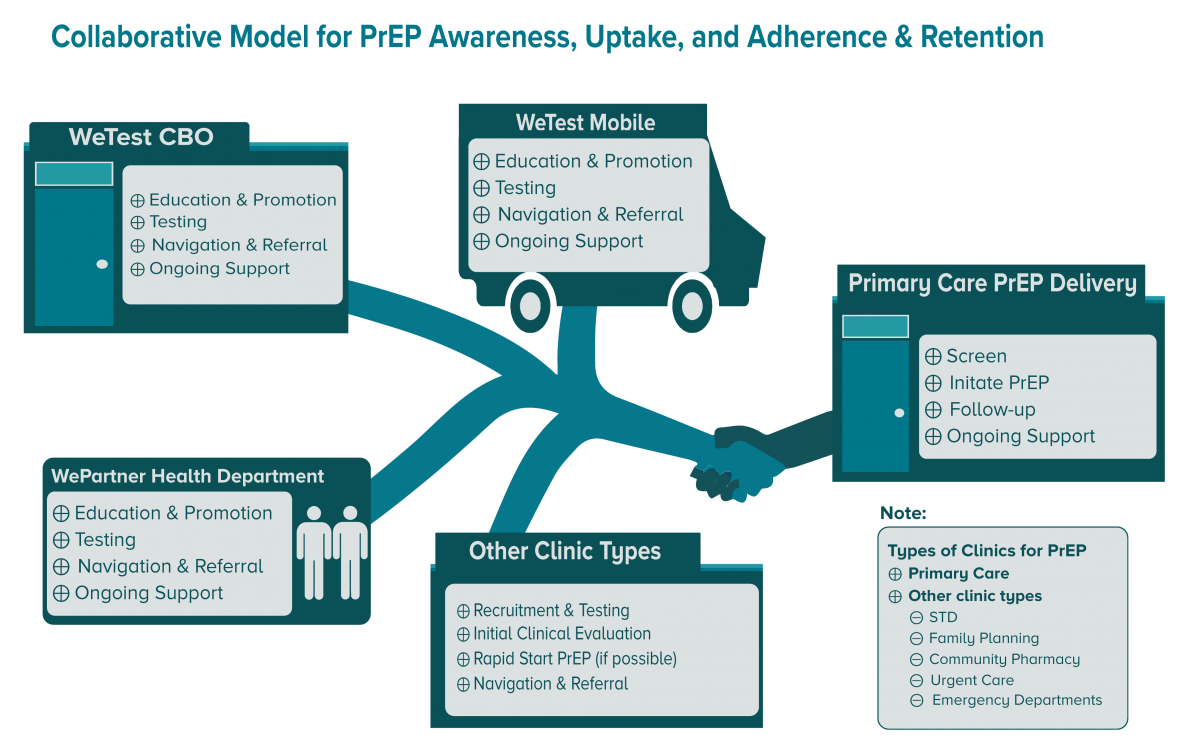
III. Public health resources for PrEP: Awareness, uptake, adherence, and retention
Increase consumer and provider knowledge
Community-wide education on PrEP happens in a variety of complementary ways, including:
- Visuals, brochures, and pamphlets;
- Media campaigns, including the use of social media;
- Radio and television public service announcements; and
- Partnering with community members, key stakeholders, and peers to build trust and credibility.
Some examples include:
- Let's Stop HIV Together-PrEP includes a PrEP brochure, graphic button with link, and an interactive widget to locate HIV prevention Services that can be embedded in your website.
- Building Healthy Online Communities (BHOC) is intended to help providers conduct HIV prevention online. The site contains useful resources like a clearinghouse of PrEP publicity campaigns.
There are several community-level interventions that use effective strategies for promoting PrEP.
- PROMISE for HIP promotes PrEP by creating and distributing community- and population-specific role model stories to spread educational messages and modeling community member experiences and endorsements.
- D-up: Defend Yourself! is based on a cultural adaptation of the Popular Opinion (POL) intervention and is intended to reach black gay, bisexual, and other men who have sex with men (MSM). D-up: Defend Yourself! includes skills building for coping with community- and individual-level stigma.
Enhance provider knowledge and support of PrEP
Health departments can develop their own PrEP educational materials and provide training for clinicians.
- HIV NEXUS- CDC Resources for Clinicians are appropriate for clinical detailing or for use in clinician education.
Identification, recruitment and navigation of people in need of PrEP
Persons at risk for HIV can be identified in clinics, through outreach, community testing, and other community program services and interventions. Integrating PrEP education and referrals into program services is an effective way to promote PrEP to likely candidates.
Testing and risk assessment resources
- HIV Testing in Nonclinical Settings- Program guidance for HIV testing providers
- Discussing Sexual Health with Patients (brochure)
Uptake
Linkage and navigation
Those at risk of HIV often encounter barriers, such as stigma, medical mistrust, and perceived payment barriers, that prevent them from receiving health services. PrEP navigation includes identifying and linking persons in need of PrEP-to-PrEP care, assisting with health insurance, identifying and reducing barriers to care, and tailoring education to the client to influence his or her health-related attitudes and behaviors. This may also include retention—supporting the person to stay on PrEP.
CBOs that do not provide clinical services may develop working relationships with PrEP clinicians to facilitate linkage of community members to PrEP services. Clinical programs may also involve staff from CBOs to help to support PrEP patients. Working relationships with behavioral health clinics, substance abuse treatment clinics, and other clinical service providers may be beneficial for providing services to persons in need of PrEP.
- PrEP Clinic Locator Find PrEP providers whether insured or uninsured.
- Find a Community Health Center Use this HRSA locator to find local health centers.
- The Toolkit for Technology-based Partner Services The toolkit serves as a general resource for health departments, community-based organizations, and others on how to use the internet and other technologies to trace and contact persons potentially exposed to STIs including HIV.
Clinical/prescribing PrEP
- The U.S. Public Health Service's Clinical Practice Guideline [PDF – 2 MB], updated in 2021, provides the framework for clinical prevention with PrEP. Also see: Clinical Provider's Supplement, 2021 [PDF – 809 KB].
- National Clinician Consultation Center for PrEP. National Clinician Consultation Center provides direct guidance on all aspects of PrEP management. This service includes guidance on assessing indications for PrEP, prescribing practices, PrEP-related laboratory protocols, and assistance with adherence issues. Via telephone: The PrEP Warmline: (855) 448-7737 or (855) HIV-PrEP, Monday – Friday, 9 a.m.- 8 p.m. EST.
- Materials for Your Practice and Patients (HIV NEXUS- CDC Resources for Clinicians)
- Screening for HIV
- Telehealth for HIV Prevention and Care Services
Financing PrEP
Jurisdictions may have local funds and leverage existing patient assistance program resources to establish their own PrEP patient assistance program. Providers may be able to leverage other public health resources such as:
- 340B Drug Pricing Program
- Diversifying PrEP Financing: Strategies to Leverage Funding across the PrEP Care Continuum
PrEP candidates may need assistance with transportation, communication with clinicians, and other services, such as navigating payment coverage. Here are some resources to help with the cost of PrEP:
Continuing Education (CE)
eLearning modules on CDC TRAIN
- HIV PrEP: Engaging Patients in U.S. Clinics (TRAIN Course ID 1085296)
- HIV PrEP: Prescribing PrEP (TRAIN Course ID 1087417)
- HIV PrEP: PrEP and Pregnancy (TRAIN Course ID 1086182)
Classroom (or virtual, synchronous learning) on CDC TRAIN
- Implementing PrEP in Your Clinic: A Course for Decision Makers(TRAIN Course ID 1095262)
Adherence and persistence
PrEP users should be provided all the information and support needed to ensure they take PrEP daily as directed. Health departments can support clinics and CBOs with adherence-related activities by providing PrEP education to clinical providers and providing resources for patients.
Compendium of Evidence-Based Interventions and Best Practices for HIV Prevention- PrEP Chapter
Continuing Education (CE)
eLearning modules on CDC TRAIN
- Strengthening Strategies that Support PrEP Adherence (TRAIN Course ID 1105465)
Training and Continuing Education Online (TCEO)
A comprehensive directory of HIV and other health services should support navigation and guidance of clients. The health department, local CBOs, or jurisdictional planning groups may have created such a directory. If none are available in your jurisdiction, you may want to create one that includes online resources, programs, and services. Compiling, using, and maintaining a directory for PrEP providers and PrEP-related services is a great way to provide information to the community and collaborate with others on prevention with PrEP.
PrEP training
To view and register for scheduled virtual, instructor-led trainings:
- Access the National HIV Classroom Learning Center training calendar hosted on Cicatelli Associates, Inc.'s (CAI's) website.
- Pre-register for your selected course via the link provided in the training calendar.
- Complete your registration on CDC TRAIN as directed when you receive an email from the National HIV Classroom Learning Center. You must join the HIV CBA Learning Group and locate the HIV CBA Training Plan in order to complete your CDC TRAIN registration for a specific classroom session (step-by-step instructions are available).
To access eLearning modules, including training prerequisite courses:
- Log-in to CDC TRAIN and access the HIV CBA Training Plan (step-by-step instructions are available).
- Select the module you wish to take.
- Launch the module or save the module for later.
To request technical assistance or that a training session be scheduled:
- CDC's directly funded health department and CBO partners may request delivery of technical assistance or a CDC-supported training by submitting a request in the CBA Tracking System.
- Organizations not directly funded by CDC may contact their local health department for assistance in submitting a technical assistance or training request.
If you have questions or need additional assistance, please contact HIVCBA@cdc.gov.
References
- Centers for Disease Control and Prevention. U.S. Public Health Service: Preexposure prophylaxis for the prevention of HIV infection in the United States—2021 Update: A Clinical Practice Guideline. Published 2021.
Transgender people, in particular transgender women, are disproportionately impacted by HIV. Providing high quality capacity building assistance to support HIV prevention programs and reduce disparities for transgender persons is an HIV prevention priority.
CDC collects and analyzes epidemiological data to support HIV prevention partners in focusing prevention efforts, allocating resources, monitoring trends, and determining gaps and successes in HIV prevention for transgender persons.
- HIV and Transgender People
- HIV Infection, Risk, Prevention, and Testing Behaviors Among Transgender Women – National HIV Behavioral Surveillance: 7 U.S. Cities, 2019-2020
- Issue Brief: HIV and Transgender Communities, 2022
CDC provides resources and offers capacity building assistance to improve HIV prevention programs and services for transgender persons.
- Toolkit for Providing HIV Prevention Services to Transgender Women of Color
- Implementing HIV Prevention Programs for Transgender Women Training
- Transgender Women Involved in Strategies for Transformation (TWIST)
- Transgender Status-Neutral Community to Clinic Models to End the HIV Epidemic (TRANSCEND) Learning Collaborative
Toolkit for providing HIV prevention services to transgender women of color
The Toolkit for Providing HIV Prevention Services to Transgender Women of Color supports implementation of HIV prevention services for transgender women of color. Authors of the toolkit included transgender women of color with extensive experience working in HIV prevention. Six transgender women from across the country who work in HIV prevention and advocate for transgender women's health critically reviewed the toolkit. The following topics are covered in the toolkit:
- Assessing community needs
- Providing client-centered care and services
- Hiring and supporting transgender women of color staff
- Creating transgender-affirming environments
- Developing outreach, recruitment, and retention systems and services
- Implementing evidence-based interventions and homegrown programs
- Conducting program evaluation and improvement
- Engaging transgender women of color in HIV prevention and testing
- Providing primary care (including HIV care) to transgender women of color
- Addressing mental and behavioral health needs of transgender women of color
- Building community partnerships and referrals
The toolkit may be of use for staff at all levels of an organization, including those at the executive level, program managers, and frontline staff such as those working in HIV testing, linkage, outreach, and programs. It is also intended for clinical providers and staff that provide the range of social support services needed by transgender women of color.
A version of this toolkit is available in Spanish.
Implementing HIV prevention programs for transgender women training
Implementing HIV Prevention Programs for Transgender Women is an 8-hour virtual instructor-led training designed to equip managers from community-based organizations with promising practices for planning and implementing HIV prevention programs and HIV care services for transgender women, including but not limited to the Transgender Women Involved in Strategies for Transformation (TWIST) intervention. This course provides tools and resources to support agencies during each of the program planning phases, from pre-implementation to implementation and maintenance.
This course is intended for executive directors, supervisors, and program managers who are working in community-based organizations and who are planning to build, expand, and improve programs that meet the needs of transgender women.
Transgender Status-Neutral Community to Clinic Models to End the HIV Epidemic (TRANSCEND) Learning Collaborative
CDC's Division of HIV Prevention launched the Transgender Status-Neutral Community to Clinic Models to End the HIV Epidemic (TRANSCEND) Learning Collaborative in 2023 as part of a CDC-funded project, PS22-2209, and welcomes all healthcare and other service providers who work with or are interested in expanding services to transgender persons in clinics and community-based organizations (CBOs), including those who are not funded for this project, to participate.
The TRANSCEND Learning Collaborative is hosted by the National Prevention Information Network (NPIN) and provides both an NPIN community forum and quarterly meetings for TRANSCEND Learning Collaborative members to dialog with one another and share best practices, lessons learned, and program-related materials and resources.
To learn more and join the TRANSCEND Learning Collaborative:
- Visit NPIN at https://npin.cdc.gov.
- Select the "NPIN Community" tab.
- Join NPIN, using the invitation code: TRANSCEND.
- Look for an email indicating that you have been approved to join NPIN and the TRANSCEND Community Page.
Trainings
To view and register for scheduled virtual, instructor-led or classroom trainings:
- Access the National HIV Classroom Learning Center training calendar hosted on Cicatelli Associates, Inc.'s (CAI's) website.
- Pre-register for your selected course via the link provided in the training calendar.
- Complete your registration on CDC TRAIN as directed when you receive an email from the National HIV Classroom Learning Center. You must join the HIV CBA Learning Group and locate the HIV CBA Training Plan in order to complete your CDC TRAIN registration for a specific training session (step-by-step instructions are available).
To request that a training session be scheduled or to request technical assistance:
- CDC's directly funded health department and CBO partners may request delivery of a CDC-supported training or technical assistance by submitting a request in the CBA Tracking System.
- Organizations not directly funded by CDC may contact their local health department for assistance in submitting a training or technical assistance request.
If you have questions or need additional assistance, please contact HIVCBA@cdc.gov.
Implementation and marketing materials
About Safe in the City
Safe in the City is part of a set of widely disseminated video-based interventions, which includes Sin Buscar Excusas (No Excuses) and Taking Care of Me (TCOM), that were tested in sexually transmitted disease (STD) clinics and found to be cost-beneficial and effective in reducing STD incidence. Safe in the City is a 23-minute, video-based HIV and STD prevention intervention designed for adult patients in STD clinic waiting rooms. Safe in the City aims to increase condom use and other safer sex behaviors, and thereby reduce infections among patients who view the video.
Safe in the City can be easily integrated into the clinic waiting room, requires very little staff time to set up with no disruption to clinic flow, and requires no counseling or small-group facilitation. Safe in the City was designed as a looping video where multiple playback options allow users to customize the intervention delivery.
Intervention essential elements
- Increase knowledge and perception of HIV/STD risk.
- Promote knowledge of correct condom use.
- Promote positive attitudes toward condom use.
- Increase intentions to use condoms.
- Build self-efficacy for testing, facilitating partner testing and treatment.
- Build self-efficacy for practicing safer sex, and the acquisition, negotiation, and use of condoms.
- Build skills for facilitating partner testing and treatment, including PrEP and PeP for prevention.
- Build skills for practicing safer sex, and the acquisition, negotiation, and use of condoms.
- Model appropriate behaviors around practicing safer sex.
Intervention audience
- Adult STD clinic patients from diverse cultural backgrounds and sexual orientations.
Safe in the City training
There is no CDC-supported training currently available for Safe in the City. Technical assistance for the implementation of Safe in the City is available.
To request technical assistance:
- CDC's directly funded health department and CBO partners may request technical assistance support by submitting a request in the CBA Tracking System.
- Organizations not directly funded by CDC may contact their local health department for assistance in submitting a training request.
If you have questions or need additional assistance, please contact HIVCBA@cdc.gov.
Implementation and marketing materials
The materials and resources listed below support the implementation and/or marketing of Safe in the City by health departments, community-based organizations, and health care or other organizations. The resources are evidence-based and designed for cost-effective, scalable implementation.
About Sin Buscar Excusas/No Excuses
Sin Buscar Excusas/No Excuses is a 60-minute, single-session, small-group, video-based behavioral intervention that aims to increase sexual safety and HIV testing and care among adult Hispanic/Latino gay, bisexual, and other men who have sex with men (MSM). Sexual safety includes having fewer partners, using condoms consistently, engaging in less risky sexual behaviors, using pre-exposure prophylaxis (PrEP) or post-exposure prophylaxis (PEP) as needed, and communicating with one's partner about monogamy or HIV status.
Sin Buscar Excusas/No Excuses can be implemented in various settings, including clinics and community agencies.
Intervention core elements
- Viewing of a Spanish- or English-language video in a small-group setting that ensures privacy and confidentiality.
- Structured, small-group, brief discussion about barriers and strategies to increase sexual safety and HIV testing and care.
- Condom distribution, the offer of an HIV test, and referrals for services (including PrEP, PEP, medication adherence, substance use/harm reduction programs, case management, and additional services in linking to care).
Intervention population
- Hispanic/Latino gay and bisexual men and other MSM who are ages 18 and older.
Sin Buscar Excusas/No Excuses training
This training has one component:
- 2 eight-hour days in a virtual, instructor-led training; or
- 2 eight-hour days in a live classroom setting
- Training also available in Español.
To view and register for scheduled trainings:
- Access the National HIV Classroom Learning Center training calendar hosted on Cicatelli Associates, Inc.'s (CAI's) website.
- Pre-register for your selected course via the link provided in the training calendar.
- Complete your registration on CDC TRAIN as directed when you receive an email from the National HIV Classroom Learning Center. You must join the HIV CBA Learning Group and locate the HIV CBA Training Plan in order to complete your CDC TRAIN registration for a specific training session (step-by-step instructions are available).
To request that a training session be scheduled:
- CDC's directly funded health department and CBO partners may request delivery of a CDC-supported training by submitting a request in the CBA Tracking System.
- Organizations not directly funded by CDC may contact their local health department for assistance in submitting a training request.
If you have questions or need additional assistance, please contact HIVCBA@cdc.gov.
Implementation and marketing materials
The materials and resources listed below support the implementation and/or marketing of Sin Buscar Excusas/No Excuses by health departments, community-based organizations, and health care or other organizations. The resources are evidence-based and designed for cost-effective, scalable implementation.
References
- O'Donnell L, Stueve A, Joseph HA, Flores S. Adapting the VOICES HIV behavioral intervention for Latino men who have sex with men. AIDS Behav 2014;18(4):767–775.
About
Sister to Sister: Take Control of Your Health (TCYH) is an adaptation of the 1993 original intervention, Sister to Sister: Respect Yourself! Protect Yourself! Because You Are Worth It! This adaptation incorporates advancements in HIV prevention, such as inclusion of education on PrEP and post-exposure prophylaxis (PEP). The intervention also uses CDC's #ShesWell assets, part of the Let's Stop HIV Together campaign to reinforce a variety of healthful messages.
Intervention objectives
Women who participate in this program will be able to:
- Identify the ways HIV can be transmitted and the ways it cannot
- Understand their personal vulnerability to HIV
- Identify three highly effective methods to prevent HIV
- Demonstrate the correct steps for using a condom
Intervention core elements
- Helping the patient understand her own vulnerability to HIV and how HIV affects women like her
- Helping the patient understand that condoms work and can be a healthy and sexy addition to her sex life
- Helping the patient learn how to properly use a condom
- Helping the patient practice negotiating condom use with her partner and responding to her partners' reactions to condom use
- Helping the patient understand PrEP and how it can help her take control of her health
- Building the patient's self-efficacy by helping her acknowledge that she is in control of her health, and she is worth it
- Demonstrating a caring attitude toward the patient
- Ensuring women providers are trained to deliver this intervention
Sister to Sister: TCYH training
This training of facilitators course is designed for a variety of women who provide HIV care and education services in clinics and primary health care settings, including community health workers, health educators, nurses, social workers, HIV case managers, and patient navigators.
Training Objectives:
- Identify at least 5 of the core elements of Sister to Sister: TCYH
- List at least 3 of the key characteristics of Sister to Sister: TCYH
- List the 9 activities of Sister to Sister: TCYH and describe how the activities help providers build patients' self-efficacy
- Practice delivering the Sister to Sister: TCYH intervention
This training has two components:
- A one-hour self-paced prerequisite eLearning module
- A two-day live, instructor-led virtual training
To view and register for scheduled trainings:
- Access the National HIV Classroom Learning Center training calendar hosted on Cicatelli Associates, Inc.'s (CAI's) website.
- Pre-register for your selected course via the link provided in the training calendar.
- Complete your registration on CDC TRAIN as directed when you receive an email from the National HIV Classroom Learning Center. You must join the HIV CBA Learning Group and locate the HIV CBA Training Plan in order to complete your CDC TRAIN registration for a specific classroom training session (step-by-step instructions are available).
To request that a training session be scheduled:
- CDC's directly funded health department and CBO partners may request delivery of a CDC-supported training by submitting a request in the CBA Tracking System.
- Organizations not directly funded by CDC may contact their local health department for assistance in submitting a training request.
After you have completed the course, you may request technical assistance:
- CDC's directly funded health department and CBO partners may request technical assistance by submitting a request in the CBA Tracking System.
- Organizations not directly funded by CDC may contact their local health department for assistance in submitting a request.
If you have questions or need additional assistance, please contact HIVCBA@cdc.gov.
Implementation and marketing materials
The materials and resources listed below support the implementation and/or marketing of Sister to Sister: Take Control of Your Health by state and local health departments, community-based organizations, and health care or other organizations. The resources are evidence-based and designed for cost-effective, scalable implementation.
References
- Aaron E, Blum C, Seidman D, et al. Optimizing delivery of HIV preexposure prophylaxis for women in the United States. AIDS Patient Care STDs 2018;32(1):16-23. doi:10.1089/apc.2017.0201.
- Bandura A. Social Foundations of Thought and Action: A Social Cognitive Theory. Upper Saddle River, NJ: Prentice Hall; 1986.
- Jemmott LS, Jemmott JB, O'Leary A. Effects on sexual risk behavior and STD rate of brief HIV/STD prevention interventions for African American women in primary settings. Am J Public Health 2007;97(6):1034-1040.
- Lambert CC, Marrazzo J, Amico RK, Mugavero MJ, Elopre L. PrEParing women to prevent HIV: An integrated theoretical framework to PrEP Black women in the United States. J Assoc Nurses AIDS Care 2018;29(6):835-848. doi:10.1016/j.jana.2018.03.005.
About status neutral HIV prevention and care
Status neutral HIV prevention and care was first introduced by the New York City Department of Health and Mental Hygiene as a comprehensive system of prevention that includes all people affected by HIV, regardless of their HIV status. With a status neutral approach, engaging and assessing the client's needs begins before an HIV test is conducted. Considered a whole person approach to health care and service delivery, status neutral HIV prevention and care focuses on the needs of the person through provision of comprehensive services that meet people where they are regardless of their HIV status.
Status neutrality seeks to address social and structural barriers to engagement in biomedical prevention (e.g., PrEP) and HIV care and treatment (e.g., ART). A status neutral approach prioritizes opportunities to address the needs of everyone in a community by providing or linking to comprehensive, state-of-the-art sexual health and supportive services. Ultimately, status neutral approaches promote health equity by putting client needs above HIV status to improve care and eliminate stigma.
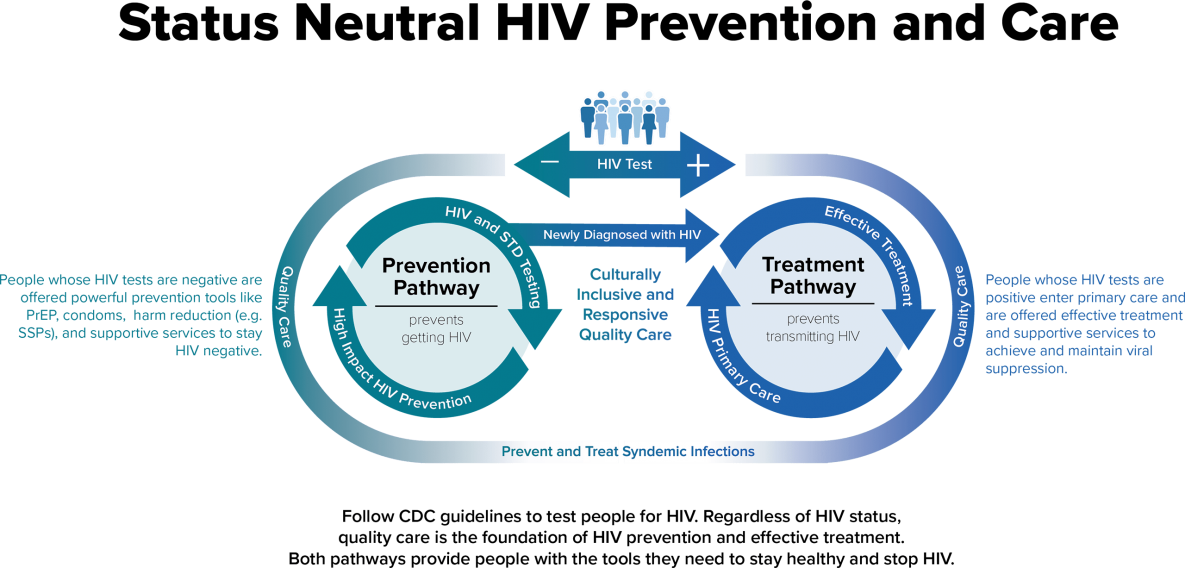
The status neutral approach to HIV prevention and care defines the entry point to care as the time of an HIV test. At this entry point, clients' needs are assessed, and they are engaged and linked to appropriate services based on these needs, regardless of whether their HIV test is positive or negative. This status neutral approach modifies the step-by-step care continuum from a disease-specific, linear approach to a whole person, needs-based approach.
Social determinants of health impact risk of acquiring HIV. The status neutral approach aims to provide "comprehensive support and care to address the social determinants of health that create disparities, especially as they relate to HIV." Working in communities to expand availability of and access to interventions and services that address the needs of all community members reflects a status neutral approach. Such offerings might include safe, stable housing, mental health services, food security, legal support, and syringe services programs.
Individuals from communities disproportionately affected by HIV should be able to access or easily navigate priority services without requiring an HIV test first. Status neutral approaches recognize the influence of social determinants of health and prioritize innovative, person-focused care to address not only HIV prevention and treatment, but also to address all barriers to staying healthy. The Status Neutral Health and Social Services graphic, from ETR, highlights the holistic offerings consistent with a status neutral approach.
o learn more about status neutral HIV prevention and care, please view the CDC Issue Brief: Status Neutral HIV Care and Service Delivery Eliminating Stigma and Reducing Health Disparities.
Intervention Goals
Minimizing stigma by taking a whole person approach to prevention and care
- Eliminating Stigma
- Making Services More Accessible
- Helping People Achieve Optimal Health and Well-being
- Efficiencies in Service Delivery
- Greater Health Equity
Status Neutral HIV Prevention and Care Core/Essential Elements
- Offer whole person, holistic services
- Provide prevention, care, and treatment services regardless of HIV status
Status Neutral HIV Prevention and Care Priority Population
- All persons affected by HIV
Status Neutral HIV Prevention and Care Training
This training has 1 component:
- 20-minute eLearning module
To access eLearning modules, including training prerequisite courses:
- Log-in to CDC TRAIN and access the HIV CBA Training Plan (step-by-step instructions are available).
- Select the module you wish to take.
- Launch the module or save the module for later.
Technical assistance for the implementation of Status Neutral HIV Prevention and Care is available.
To request technical assistance:
- CDC's directly funded health department and CBO partners may request technical assistance support by submitting a request in the CBA Tracking System.
- Organizations not directly funded by CDC may contact their local health department for assistance in submitting a training request.
If you have questions or need additional assistance, please contact HIVCBA@cdc.gov.
References
- Achieving Together Texas. A Status Neutral Approach: Achieving Together to End the HIV Epidemic. AchievingtogetherTexas.org. Published June 18, 2020. Accessed September 7, 2022.
- DC Beings. HIV Status Neutral. Published May 27, 2021. Accessed September 7, 2021.
- District of Columbia Department of Health. Status Neutral. Sex Positive. Published August 31, 2021. Accessed September 7, 2021.
- Dubin S. 'If We Do This Right' Maybe H.I.V. Will Be Forgotten. The New York Times. Published June 12, 2019. Accessed September 7, 2022.
- Mayer K, Nelson L, Hightow-Weidman L, et al. The persistent and evolving HIV epidemic in American men who have sex with men. The Lancet 2021;397: 1116–26.
- Myers JE, Braunstein SL, Xia Q, et al. Redefining prevention and care: A status-neutral approach to HIV. Open Forum Infect Dis. 2018;5(6). doi:10.1093/ofid/ofy097.
- New York City Department of Health and Mental Hygiene. New York City: Ending the HIV Epidemic: A Plan for America Plan. NYhiv.org. Published March 29, 2021. Accessed September 7, 2021.
- Rangel JC, Crath R. Managing risk, managing affects: The emerging biopolitics of HIV neutrality. Health Risk Soc. 2021;23(5-6):251-271. doi:10.1080/13698575.2021.1972088.
About syringe services programs
Syringe Services Programs (SSPs) are associated with an estimated 50% reduction in HIV and hepatitis C virus (HCV) incidence. When combined with medications that treat opioid dependence (also known as medication-assisted treatment), HIV and HCV transmission is reduced by over two-thirds, according to research.
SSPs serve as a bridge to other health services, including HIV and HCV testing and treatment, HIV pre-exposure prophylaxis (PrEP), and medication-assisted treatment.
In some jurisdictions, PWID can access sterile needles and syringes and other injection paraphernalia through SSPs and through pharmacies without a prescription.
SSPs can also prevent overdose by teaching people how to recognize, respond to, and reverse a drug overdose (e.g., naloxone). Many SSPs distribute and train clients to administer naloxone along with other harm reduction measures, such as safer injection practices.
SSPs have partnered with law enforcement and other first responders, such as EMT workers and fire fighters, to provide lifesaving naloxone if someone is experiencing overdose. SSPs also protect first responders and the public by providing safe needle disposal and reducing the presence of discarded needles in the community.
Strategy goals
- Prevent transmission of blood-borne infections
- Reduce or stop substance use
- Prevent overdose deaths
- Reduce publicly discarded needles
- Increase HIV/STD treatment initiation and retention
Strategy essential elements
- Provide onsite access to and disposal of syringes and injection equipment
- Provide onsite vaccination and testing services
- Offer referrals to medicated-assisted treatment, medical and psychosocial care, food, housing, and other services
- Provide onsite wound care, safer injection instruction, and training on administering the overdose prevention medication, i.e., naloxone
- Provide onsite sexual HIV/STD prevention (e.g., condoms, lubricant, PrEP)
SSP training
There is no CDC-supported training currently available for SSP. Technical assistance for the implementation of SSPs, including jurisdictional SSP institutes, is available.
To request technical assistance:
- CDC's directly funded health department and CBO partners may request technical assistance by submitting a request in the CBA Tracking System.
- Organizations not directly funded by CDC may contact their local health department for assistance in submitting a request.
If you have questions or need additional assistance, please contact HIVCBA@cdc.gov.
SSP resources
CDC has information and program guidance on SSPs.
- Syringe Services Programs (SSPs)
- Summary of Information on The Safety and Effectiveness of Syringe Services Programs (SSPs)
- Determination of Need for Syringe Services Programs
- Federal Funding for Syringe Services Programs
- Peer-Delivered Syringe Exchange Toolkit
Implementation and marketing materials
The materials and resources listed below support the implementation and/or marketing of SSPs by health departments, community-based organizations, and health care or other organizations. The resources are evidence-based and designed for cost-effective, scalable implementation.
References
- CDC. 2020 Viral Hepatitis Surveillance Report.
- CDC. Estimated HIV incidence and prevalence in the United States, 2010–2015. HIV Surveillance Supplemental Report. 2018;23(No. 1). Published March 2018.
- Broz D, Carnes N, Chapin-Bardales J, Des Jarlais DC, Handanagic S, Jones CM, Paul McClung RP, Asher AK. Syringe services programs' role in ending the HIV epidemic in the U.S: Why we cannot do it without them. Am J Prevent Med 2021 Nov;61(5 Suppl 1):S118-S129.
- Chahal HS, Marseille EA, Tice JA, Pearson SD, Ollendorf DA, Fox RK, Kahn JG. Cost-effectiveness of early treatment of hepatitis C virus genotype 1 by stage of liver fibrosis in a US treatment-naive population. JAMA Intern Med 2016 Jan;176(1):65-73.
- Aspinall EJ, Nambiar D, Goldberg DJ, Hickman M, Weir A, Van Velzen E, Palmateer N, Doyle JS, Hellard ME, Hutchinson SJ. Are needle and syringe programmes associated with a reduction in HIV transmission among people who inject drugs: A systematic review and meta-analysis. Int J Epidemiol Feb 2014;43(1):235-48. doi: 10.1093/ije/dyt243. Epub 2013 Dec 27. PMID: 24374889.
- Platt L, Minozzi S, Reed J, Vickerman P, Hagan H, French C, Jordan A, Degenhardt L, Hope V, Hutchinson S, Maher L, Palmateer N, Taylor A, Bruneau J, Hickman M. Needle syringe programmes and opioid substitution therapy for preventing hepatitis C transmission in people who inject drugs. Cochrane Database Syst Rev 2017;9:CD012021. doi:10.1002/14651858.CD012021.pub2.
- Fernandes RM, Cary M, Duarte G, Jesus G, Alarcão J, Torre C, Costa S, Costa J, Carneiro AV. Effectiveness of needle and syringe programmes in people who inject drugs – An overview of systematic reviews. BMC Public Health 2017;17(1):309. doi:10.1186/s12889-017-4210-2.
- HIV and Injection Drug Use – Vital Signs – CDC. Centers for Disease Control and Prevention. Published December 2016.
- Des Jarlais DC, Nugent A, Solberg A, Feelemyer J, Mermin J, Holtzman D. Syringe service programs for persons who inject drugs in urban, suburban, and rural areas — United States, 2013. MMWR Morb Mortal Wkly Rep 2015;64(48):1337-1341. doi:10.15585/ mmwr.mm6448a3.
- Seal KH, Thawley R, Gee L. Naloxone distribution and cardiopulmonary resuscitation training for injection drug users to prevent heroin overdose death: A pilot intervention study. J Urban Health 2005;82(2):303-311. doi:10.1093/jurban/jti053.
- Galea S, Worthington N, Piper TM, Nandi VV, Curtis M, Rosenthal DM. Provision of naloxone to injection drug users as an overdose prevention strategy: Early evidence from a pilot study in New York City. Addict Behav 2006;31(5):907-912. doi:10.1016/j. addbeh.2005.07.020.
- Tobin KE, Sherman SG, Beilenson P, Welsh C, Latkin CA. Evaluation of the Staying Alive programme: Training injection drug users to properly administer naloxone and save lives. Int J Drug Policy 2009;20(2):131-136. doi:10.1016/j.drugpo.2008.03.002.
- Doe-Simkins M, Walley AY, Epstein A, Moyer P. Saved by the nose: Bystander-administered intranasal naloxone hydrochloride for opioid overdose. Am J Public Health 2009;99(5):788-791. doi:10.2105/ajph.2008.146647.
- Bennett AS, Bell A, Tomedi L, Hulsey EG, Kral AH. Characteristics of an overdose prevention, response, and naloxone distribution program in Pittsburgh and Allegheny County, Pennsylvania. J Urban Health 2011;88(6):1020-1030. doi:10.1007/s11524-011-9600-7.
- Leece PN, Hopkins S, Marshall C, Orkin A, Gassanov MA, Shahin RM. Development and implementation of an opioid overdose prevention and response program in Toronto, Ontario. Can J Public Health 2013;104(3):e200-204.
- Childs R. Law Enforcement and Naloxone Utilization in the United States. North Carolina Harm Reduction Coalition; 2016.
- Tookes HE, Kral AH, Wenger LD, et al. A comparison of syringe disposal practices among injection drug users in a city with versus a city without needle and syringe programs. Drug Alcohol Depend 2012;123(1-3):255-259. doi:10.1016/j.drugalcdep.2011.12.001.
- Riley ED, Kral AH, Stopka TJ, Garfein RS, Reuckhaus P, Bluthenthal RN. Access to sterile syringes through San Francisco pharmacies and the association with HIV risk behavior among injection drug users. J Urban Health 2010;87(4):534-542. doi:10.1007/s11524- 010-9468-y.
- Klein SJ, Candelas AR, Cooper JG, et al. Increasing safe syringe collection sites in New York State. Public Health Rep 2008;123(4):433-440. doi:10.1177/003335490812300404.
- de Montigny L, Vernez Moudon A, Leigh B, Kim SY. Assessing a drop box programme: A spatial analysis of discarded needles. Int J Drug Policy 2010;21(3):208-214. doi:10.1016/j.drugpo.2009.07.003.
- Doherty MC, Junge B, Rathouz P, Garfein RS, Riley E, Vlahov D. The effect of a needle exchange program on numbers of discarded needles: A 2-year follow-up. Am J Public Health 2000;90(6):936- 939.
- Bluthenthal RN, Anderson R, Flynn NM, Kral AH. Higher syringe coverage is associated with lower odds of HIV risk and does not increase unsafe syringe disposal among syringe exchange program clients. Drug Alcohol Depend 2007;89(2-3):214-222.
- HIV Infection, Risk, Prevention, and Testing Behaviors among Persons Who Inject Drugs—National HIV Behavioral Surveillance: Injection Drug Use, 20 U.S. Cities, 2018. HIV Infection, Risk, Prevention, and Testing Behaviors among Persons who Inject Drugs (cdc.gov). Published February 2020. Accessed February 6, 2023.
- Marx MA, Crape B, Brookmeyer RS, et al. Trends in crime and the introduction of a needle exchange program. Am J Public Health 2000;90(12):1933–1936.
- Galea S, Ahern J, Fuller C, Freudenberg N, Vlahov D. Needle exchange programs and experience of violence in an inner city neighborhood. J Acquir Immune Defic Syndr 2001;28(3):282-288.
About TRANSFORM
TRANSFORM (Transforming from HIV Prevention Practice to Prevention Innovation): Comprehensive HIV Care Delivery for MSM of Color is a curriculum designed for HIV prevention or care staff working in health departments, community-based organizations (CBOs), and behavioral or social service agencies serving men who have sex with men (MSM) of color at risk for or living with HIV. TRANSFORM includes culturally and linguistically appropriate trainings that address behavioral health, HIV prevention and care, and social services.
Curriculum goal
To provide training and technical assistance (TA) to health departments and their community partners to increase their capacity to address the holistic health needs of MSM of color at risk for or living with HIV.
Curriculum objectives
HIV prevention staff who complete the TRANSFORM curriculum will:
- Increase their knowledge, skills, and abilities to provide comprehensive HIV prevention and care services to MSM of color at risk for or living with HIV.
- Improve recruitment, retention, and adherence to care services for their patients and clients who are MSM of color.
Intended audience
HIV prevention or care staff working in health departments, CBOs, and behavioral or social service agencies serving MSM of color at risk for or living with HIV.
TRANSFORM training
This training has one component:
- 12 (60- to 90-minute) eLearning modules (E)
Prevention Services
- HIV Testing for Men Who Have Sex with Men (MSM) of Color
- PrEP Module: Implementation for Health Departments
Behavioral Health Modules
- Developing Public Health and Behavioral Health Partnerships
- Defining Behavioral Health Opportunities for MSM of Color
- Evidence-Based Behavioral Health Engagement Strategies for MSM of Color
- Sustaining Behavioral Health through Insurance Coverage
- The Urgency to Advance Trauma Informed Behavioral Health Approaches in Services for MSM of Color (E)
- Building Integrated Public and Behavioral Health Systems
Clinical Services
- Sexual History Taking in the Clinical Engagement with Men Who Have Sex with Men (MSM) Of Color
Social Services
- Employment as a Determinant of Health for MSM of Color
Health Systems
- Peer Navigation for Men Who Have Sex with Men (MSM) of Color
- Community Mobilization for MSM of Color
To access eLearning modules, including training prerequisite courses:
- Log-in to CDC TRAIN and access the HIV CBA Training Plan (step-by-step instructions are available).
- Select the module you wish to take.
- Launch the module or save the module for later.
If you have questions or need additional assistance, please contact HIVCBA@cdc.gov.
About TWIST
Transgender Women Involved in Strategies for Transformation (TWIST) is a behavioral intervention developed by transgender women for transgender women and aims to reduce HIV and STD transmission behaviors among participants. The TWIST intervention consists of four, 3-hour educational and skills-building sessions designed to be facilitated by transgender women to transgender women in small groups. The sessions of TWIST address specific needs and issues faced by transgender women regardless of HIV status, including gender affirmation, building their social support networks, increasing self-efficacy to set goals, identifying characteristics of healthy and unhealthy relationships, learning behaviors that can lower the chances of getting HIV, and coping with stress.
The TWIST intervention is an extensive adaptation of the WILLOW intervention guided by social cognitive theory, transgender theory, and gender affirmation theory. The TWIST intervention underwent extensive updating in 2022 and was piloted between November 2022 and March 2023. TWIST has not yet been formally evaluated for its impact on HIV and STD transmission behaviors.
TWIST Training
Agencies implementing TWIST must be ready to provide HIV prevention services and services to address the needs of transgender women.
- Implementing HIV Prevention Programs for Transgender Women
- A virtual instructor-led training designed to equip program managers with best practices for planning and implementing HIV prevention programs and HIV care services for transgender women. This course provides tools and resources to support agencies during each of the program planning phases, from pre-implementation to implementation and maintenance.
- Intended for executive directors, supervisors, and program managers who are planning to build, expand, and improve programs that meet the needs of transgender women in an inclusive, affirming, and respectful way.
- Request technical assistance
- Agencies implementing TWIST are expected to have the following capacities before conducting the TWIST intervention with clients:
- Ability to hire and retain transgender women on staff
- Complete a community assessment
- Develop a Community Resource Directory
- Engage with transgender persons in the community and recruit to agency services
- Have a plan and process to assess and identify the needs of transgender women and to link these clients to services
- Train staff who will serve as TWIST facilitators in the following topics:
- Fundamentals of HIV and STIs
- Basic facilitation skills
- Agencies implementing TWIST are expected to have the following capacities before conducting the TWIST intervention with clients:
It is highly recommended that TWIST is facilitated by transgender women. To prepare to facilitate the course, TWIST facilitators must take the following trainings:
- TWIST Training of Facilitators
- A live classroom training that prepares transgender women to serve as facilitators of the TWIST intervention.
- Intended for transgender women who will be facilitating the TWIST intervention in their community.
- Fundamentals of Motivational Interviewing (MI) for HIV
- Provides a versatile skill set that can be used to assist clients as they work through challenges with behavioral change. This classroom training introduces learners to the foundational skills of MI.
- Benefits many audiences, including TWIST facilitators by providing participants with skills that can be leveraged while facilitating TWIST.
To view and register for scheduled training:
- Access the National HIV Classroom Learning Center training calendar hosted on Cicatelli Associates, Inc.'s (CAI's) website.
- Pre-register for your selected course via the link provided in the training calendar.
- Complete your registration on CDC TRAIN as directed when you receive an email from the National HIV Classroom Learning Center. You must join the HIV CBA Learning Group and locate the HIV CBA Training Plan in order to complete your CDC TRAIN registration for a specific classroom session (step-by-step instructions are available).
To request that a training session be scheduled:
- CDC's directly funded health department and CBO partners may request delivery of a CDC-supported training by submitting a request in the CBA Tracking System.
- Organizations not directly funded by CDC may contact their local health department for assistance in submitting a training request.
To request technical assistance:
- CDC's directly funded health department and CBO partners may request technical assistance by submitting a request in the CBA Tracking System.
- Organizations not directly funded by CDC may contact their local health department for assistance in submitting a request.
If you have questions or need additional assistance, please contact HIVCBA@cdc.gov.
Implementation and marketing materials
Materials and resources that support the implementation of TWIST are coming soon.
Respond
Cutting-edge HIV prevention technologies and strategies now allow CDC to help local public health officials identify where HIV prevention and treatment services are most urgently needed. CDC can assess and address gaps in staffing, expertise, and data management systems that prevent states and local areas from being able to fully investigate and respond to increases in HIV transmission and outbreaks. Resources are available for the HIV prevention workforce to increase its capacity to identify, investigate, and respond to potential HIV outbreaks.
About HIV cluster detection and response
CDR is a critical component of the federal initiative to End the HIV Epidemic by 2030. CDR uses data routinely reported to health departments to identify communities where HIV may be spreading rapidly. This information can then be used to identify gaps in prevention and care services to ensure that services reach the populations that need them quickly. Considerations for Implementing HIV Cluster Detection and Response6690When a growing cluster of HIV cases and the associated risk network is detected, whether through molecular surveillance or partner services, community partners can work together to prevent ongoing transmission. Learn more about CDR.
For additional information on CDR, please see:
- Public Health Response to Clusters and Outbreaks 101
- Public Health Response to HIV Clusters and Outbreaks 201
- Public Health Response to HIV Clusters and Outbreaks 301
HIV cluster detection and response training
There is no CDC-supported training currently available for HIV Cluster Detection and Response. Technical assistance for HIV Cluster Detection and Response is available.
To request technical assistance:
- CDC's directly funded health department and CBO partners may request technical assistance by submitting a request in the CBA Tracking System.
- Organizations not directly funded by CDC may contact their local health department for assistance in submitting a request.
If you have questions or need additional assistance, please contact HIVCBA@cdc.gov.
About social marketing
The Centers for Disease Control and Prevention's (CDC's) Division of HIV Prevention (DHP) has developed guidelines and best practices for implementing its health communication campaigns, activities, and emergency response efforts. Although these materials were developed for CDC staff, they may be useful for health departments, community-based organizations, healthcare and other organizations, and technical assistance providers when strategizing to develop social and digital media communication messages to reach a target audience:
- CDC HIV provides current, scientifically accurate HIV content and resources for the general public, public health professionals, and clinicians.
- Let's Stop HIV Together provides access to campaign resources for distinct audiences.
- The HIV Risk Reduction Tool helps people learn about the risk of getting HIV or transmitting HIV to someone else, and how to lower that risk.
Key projects developed by DHP include social marketing campaigns for consumers and health care providers through Let's Stop HIV Together, and:
- Partnership activities and community engagement
- Web development
- Content development and inquiry response
- Conference exhibits
DHP also engages with the general public, partners, and healthcare providers through social media, including Facebook CDCHIV and Start Talking. Stop HIV, X (formerly Twitter) @CDC_HIV, Instagram (@stophivtogether and @starttalkinghiv and CDC's YouTube HIV playlist.