Diagnose and Treat to Save Lives: Decreasing Deaths Among People with HIV
15,500
Around 15,500 people with HIV died from any cause in 2018.
↓37%
Death rates* among people with HIV decreased by about 37% from 2010 to 2018.
1 in 3
About 1 in 3 deaths among people with HIV were due to HIV-related causes in 2017.
Overview
About 1.2 million people are living with HIV in the United States. Improvements in HIV care and treatment have made it possible for people with HIV to live nearly as long as people who don’t have HIV. Yet, in 2017 HIV was among the 10 leading causes of death for some groups. To decrease HIV-related deaths, people need to know their HIV status so they can take medicine to treat HIV and get the virus under control† if they have it. People who have HIV and control the virus can live long, healthy lives and have effectively no risk of sexually transmitting HIV.
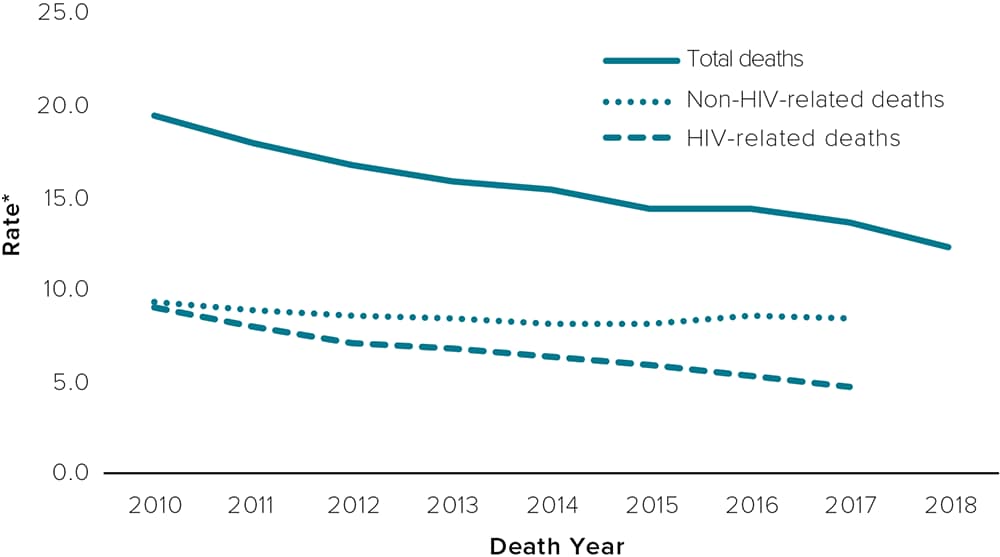
* Age-adjusted rates per 1,000 people with HIV were calculated using the US 2000 standard population.
† HIV that is under control or virally suppressed means less than 200 copies of HIV per milliliter of blood.
HIV-related deaths are preventable but persist.
- From 2010 to 2017, rates of HIV-related deaths decreased overall for people with HIV, yet differences continue to exist for certain populations.
- In 2017, by race/ethnicity, Black/African American people had a higher rate of HIV-related deaths compared to White and Hispanic/Latino people.
- In 2017, by US geographic region, rates of HIV-related deaths were higher among people in the South compared to other regions.
- In 2017, populations with higher rates of HIV-related deaths also had lower proportions of individuals with their virus under control.
- Other research suggests that social and structural factors, such as poverty, unemployment, lack of health insurance or access to care, and HIV-related stigma could affect timely diagnosis and access to treatment and contribute to higher rates of HIV-related deaths among Black/African American people and people in the South.
Among people with HIV, deaths from all causes decreased mainly because of declines in HIV-related deaths.
Racial and ethnic differences in HIV-related deaths continue to exist.
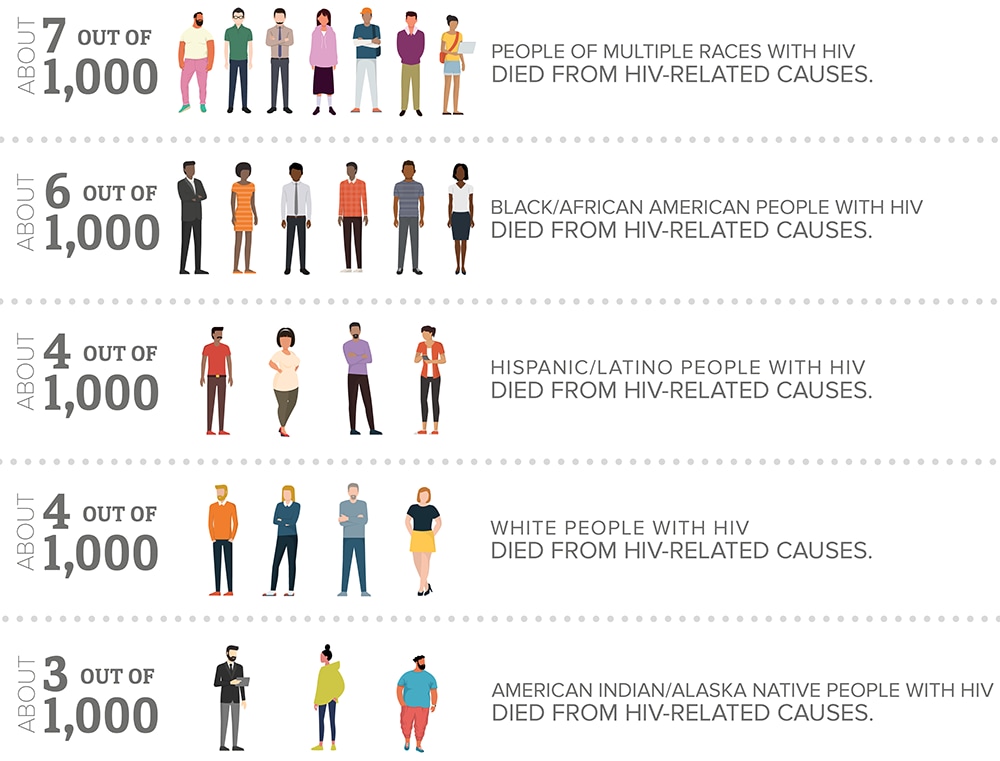
Note: Age-adjusted rates of HIV-related deaths per 1,000 people with HIV in 2017. Native Hawaiians and Other Pacific Islanders and Asians are excluded because less than 85% of deaths in 2017 had a known underlying cause of death. Rates calculated for American Indians/Alaska Natives are based on less than 12 deaths; these rates are considered unstable should be interpreted with caution.
Rates of HIV-related deaths were highest in the South. §
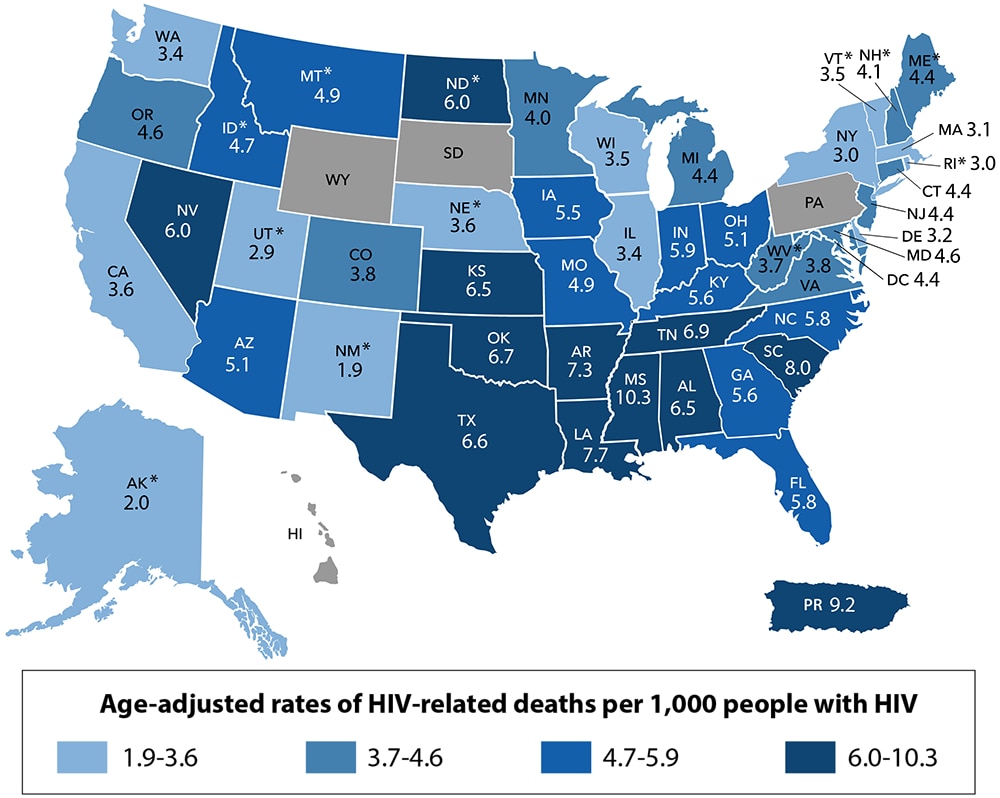
*Rates calculated based on less than 12 deaths are considered unstable and should be interpreted with caution.
Note: Age-adjusted rates of HIV-related deaths per 1,000 people with HIV in 2017.
Other US dependent areas are excluded because they do not report the underlying cause of death. HIV-related deaths include an ICD-10 code of B20-B24, O98.7, or R75 for the underlying cause of death. Non-HIV-related deaths include all other deaths with a known underlying cause. Deaths with an unknown underlying cause are excluded. Rates age-adjusted to use the US 2000 standard population.
§ Regions used in CDC’s National HIV Surveillance System:
Northeast: CT, ME, MA, NH, NJ, NY, PA, RI, VT
Midwest: IL, IN, IA, KS, MI, MN, MO, NE, ND, OH, SD, WI
South: AL, AR, DE, DC, FL, GA, KY, LA, MD, MS, NC, OK, SC, TN, TX, VA, WV
West: AK, AZ, CA, CO, HI, ID, MT, NV, NM, OR, UT, WA, WY
Jurisdictions with no shading are those with less than 85% of deaths in 2017 with a known underlying cause of death.
The Way Forward
Healthcare Providers Can:
- Test everyone for HIV once in their lifetime. Test people at higher risk at least annually.
- Discuss available HIV prevention options with patients, including pre-exposure prophylaxis (PrEP) and condoms.
- Link people with HIV to care as soon as possible after a diagnosis and help them stay in care.
Health Departments Can:
- Expand HIV testing, including the use of HIV self-tests.
- Raise awareness about prevention tools, such as PrEP for people at risk for getting the virus from sex or injection drug use.
- Quickly link people with HIV to care.
- Find and help relink people who fall out of HIV care.
People with HIV Can:
- Start HIV care immediately and take medicine as prescribed.
- Talk to their provider about problems taking their medicine.
- Learn more about living well with HIV.
Everyone Can:
- Learn their HIV status: gettested.cdc.gov
- Support family and friends who have HIV.
- Discuss HIV prevention options, including PrEP, with their healthcare provider.
- Help end HIV stigma to empower people with HIV to live long, healthy lives.
Diagnose and Treat
HIV treatment improves health outcomes.
Early diagnosis is the first step in helping people with HIV stay healthy. HHS guidelines recommend beginning treatment immediately after diagnosis to slow the progression of HIV and get the virus under control. Nearly all people in care can have their HIV under control within 6 months of diagnosis. Early diagnosis followed by prompt treatment controls the virus, prevents transmission, and helps people with HIV live long, healthy lives.