STEPS to Care: Care Team Coordination
Care Team Coordination is a strategy that allows STEPS staff to establish and assess Care Plans to meet client needs across the care continuum and improve adherence and retention outcomes. Regular Care Team meetings ensure the team remains updated about and responsive to the client’s changing needs and circumstances.
After reviewing the Care Team Coordination information and resources below, you will know:
- Purpose and goals of Care Team Coordination
- Key participants and their roles in Care Team meetings
- Types of Care Team meetings (initial hand-off, formal, and informal)
- Purpose and goals of Care Team meetings
- Best practices for integrating Care Team meetings into your program structure
- Strategies for supporting good communication among Care Team members
Care Team Meetings
The purpose of Care Team Coordination is to create formal structures to ensure each client’s Care Team is updated and responsive to the client’s changing needs and circumstances. During Care Team meetings, a key component of Care Team Coordination, staff review and update a client’s clinical and nonclinical status and make appropriate changes to the Care Plan to address changing needs. Decisions made during Care Team meetings are often initiated and monitored during subsequent patient navigation sessions.
Care Team meetings generally work best when all members can attend in-person. Sometimes, staff may be offsite and can call in via phone, but it is important to establish regular communication methods with such staff to ensure that information can be exchanged efficiently.
Care Team Meeting Types
Care Team meetings typically fall into one of three categories:
Initial hand-off meeting
- The initial hand-off meeting is a time for the primary care provider to exchange important client information with the Care Team at the beginning of the client’s intake into the STEPS to Care program.
- During this meeting, the team should discuss information about social services needed, clinical status, behavioral health details, and both the client’s and the primary care provider’s perspectives of any barriers to care and treatment.
Who participates? The primary care provider and Care Coordinator should be present for this meeting. The Patient Navigator for the client should be present if possible, and the client may also be present, if possible and appropriate.
How often? Initial hand-off meetings happen once for each client at enrollment.
Formal care team meetings
- Formal Care Team meetings can be scheduled or unscheduled
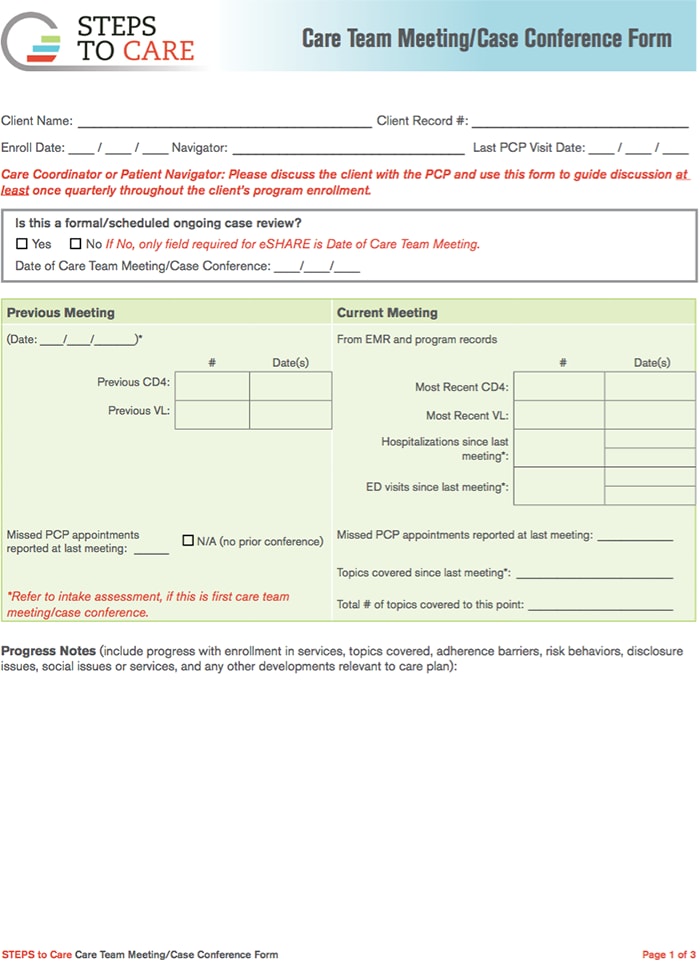
- A Care Team meeting form [PDF – 169 KB] must be completed to document each meeting and the changes in the client’s clinical or nonclinical status.
- Staff should review clients’ Care Plans and clinical information and communicate changes that may impact them. Staff should identify clients with suboptimal status and work to develop strategies to address their needs.
Who participates? At the minimum, the Care Coordinator and the primary care provider for the client should be present. The Patient Navigator is strongly recommended to attend. If the Patient Navigator is not present, the Care Coordinator should relay all information about changes to the client’s Care Plan or other status to the Patient Navigator. Clients are typically not present, although this depends on the agency and the client’s case. Additional staff may be invited to attend a Care Team meeting if necessary, for example, a mental health care provider or medical specialist.
How often? Each client’s case should be reviewed at least once every 90-120 days. Formal Care Team meetings can be scheduled regularly on a weekly or monthly basis, or as necessary. Care Team meeting attendees may discuss and review several cases per meeting. Care Team meetings can also occur outside of regularly scheduled meetings to address any new client changes. These Care Team meetings may be scheduled shortly after this information is obtained or directly after a medical appointment.
Informal care team meetings
- Informal Care Team meetings can be scheduled or unscheduled and allow Care Team members to communicate in between formal team meetings.
- These meetings do not require completion of a Care Team meeting form, although a form may be completed if important information affecting the Care Plan is relayed during the meeting and was not previously documented.
Who participates? Sometimes, a client may request an informal Care Team meeting during a primary care provider appointment for moral support or to help with translating provider instructions. Another common type of informal meeting is a morning “huddle,” in which Care Team staff briefly meet each morning to review the clients they will be meeting with, potential challenges, gaps in coverage, and any other support needs. These meetings may involve the Program Director, Care Coordinators, and Patient Navigators. Some agencies also choose to include the primary care provider when possible.
How often? Informal Care Team meetings can occur daily, as described in morning huddles, or as requested by clients or other staff.
Care Team Communication
In the video below, Patient Navigators, Care Coordinators, Program Directors, and primary care providers discuss:
- Key elements of good communication for Care Teams, including providing a safe environment to voice opinions
- The importance of understanding roles and responsibilities in Care Teams
- Agency structures that help with team communication about clients and schedules
Care Team Roles and Responsibilities
Care Team meetings include the primary care provider, different members of the Care Team, and the client, if appropriate and possible. The specific participants may vary depending on the type and purpose of the meeting. The specific roles and responsibilities for each participant may differ in your agency. Be sure to check with your supervisor to understand what they may be. The Staffing and Supervision topic page also provides more information about STEPS roles and responsibilities.
Generally, the roles of each participant are as follows:
| Roles | Responsibilities |
|---|---|
| Primary care provider |
|
| Program director |
|
| Care coordinator |
|
| Patient navigator |
|
| Client |
|
| Other staff |
|
Best Practices for Success
To help ensure successful Care Team Coordination, your agency should have clear policies in place for the following:
| Structure and responsibilities for intake: For more information, visit the Client Intake page. |
Structure of formal Care Team meetings:
|
Structure and/or protocol for informal check-ins:
|
Protocol for how clients will be involved in Care Team meetings:
|
Working with Primary Care Providers
Working with Primary Care Providers’ schedules can be a challenge for Care Teams striving to keep the lines of communication open. The video below contains helpful guidance on approaches to communication.