Surveillance for Viral Hepatitis – United States, 2017
Entire report in a printable format pdf icon[PDF – 1.8MB – 65 pages]
*This summary replaces the version released on September 10, 2019. Please refer to Appendix B for a summary of changes.
SUMMARY
Each week, health departments report cases of hepatitis A, hepatitis B, and hepatitis C to the Centers for Disease Control and Prevention (CDC) through the National Notifiable Diseases Surveillance System (NNDSS). CDC aggregates the information to conduct ongoing viral hepatitis surveillance nationwide.
Hepatitis A is an acute infection that can result in mild illness or be severe enough to result in hospitalization or, in rare cases, death. Hepatitis A has been a vaccine preventable disease since the hepatitis A vaccine first became available in 1995. Incidence rates decreased more than 95% from 1995 to 2011, then increased by 140% from 2011 to 2017. Until 2017, US incidence rates were influenced by occasional outbreaks, often linked to imported food, and from time-to-time among non-immune persons. In 2017, large person-to-person outbreaks began occurring among persons who use drugs and persons experiencing homelessness.
Hepatitis A Tables and Figures
Hepatitis B often occurs as an acute infection that may or may not be identified or reported. Later, a chronic infection may develop. Hepatitis B is a vaccine preventable disease and reported cases of acute hepatitis B declined from 1990–2014 after routine vaccination of children was recommended. Injection drug use is a major risk factor associated with acute hepatitis B cases in the US. Chronic hepatitis B infections primarily occur among persons born outside the US in countries with intermediate or high rates of hepatitis B prevalence. Chronic hepatitis B infection can be treated and managed clinically but cannot be cured.
Hepatitis B Tables and Figures
Hepatitis C occurs as an acute infection that is most often asymptomatic and frequently develops into a chronic infection. New cases of acute hepatitis C have increased rapidly in the US since 2010, and have most often been associated with injection drug use. There is no vaccine against hepatitis C, but short-term treatment for chronic hepatitis C can clear the virus and cure the infection.
Hepatitis C Tables and Figures
BACKGROUND
Viral hepatitis A, B, and C are transmitted in different ways. Main transmission routes and risk factors are summarized in the table below. Hepatitis B and C may be transmitted from a mother to her baby, known as perinatal transmission. Perinatal hepatitis C cases were not reportable to the CDC in 2017. This report contains only perinatal hepatitis B cases, which have been reported to the CDC since 1995.
| Hepatitis A | Hepatitis B | Hepatitis C | |
|---|---|---|---|
| Main transmission | Fecal-oral | Blood Sexual |
Blood |
| Perinatal transmission | No | Yes | Yes |
| Risk factors (1-4) |
Direct contact with someone with hepatitis A
Traveling to or adopting a child from countries where hepatitis A is common Men who have sex with men Injection or non-injection drug use Homelessness Clotting factor disorders Working with nonhuman primates |
Born to infected mother
Sexual partners or household contacts of infected persons Men who have sex with men Injection drug use Health care and public safety workers at risk for exposure to blood Hemodialysis patients |
Injection drug use
Specific types of health care exposures HIV-positive Born to infected mother |
| Number of acute infections reported in 2017 | 3,366 | 3,409 | 3,216 |
| Adjusted number of acute infections in 2017 (5)* | 6,700 (4,700-7,400) | 22,200 (12,600-54,200) | 44,700 (35,400-152,400) |
| Estimated prevalence of chronic infections (6,7) | Not applicable | 862,000 (668,000-1,056,000) in 2011–2016 | 2.4 million (2.0-2.8 million) in 2013–2016 |
| Vaccine | Yes | Yes | No |
| Treatment of Chronic Infections | Not applicable | Yes, not curative | Yes, curative |
* The adjusted number accounts for under-ascertainment and under-reporting based on data from 2011. The methods are documented in Klevens, et al. (5) with corrected multipliers and confidence intervals developed by the CDC.
After the hepatitis virus is transmitted to an uninfected person, it can cause acute infection. It is not possible to diagnose every acute case, because symptoms may be so mild that the person does not seek care or too vague to prompt a health care provider to suspect and test for viral hepatitis.
An acute infection can either resolve or, for hepatitis B and hepatitis C, the infection can become chronic. Not every chronic infection is diagnosed because the infection can last for many years without signs and symptoms, gradually causing damage to the liver and other organs. Without treatment, chronic viral hepatitis can lead to liver fibrosis or liver cancer; either of which can lead to liver failure or death.
VACCINATION
Vaccines are the best way to prevent infectious diseases, including viral hepatitis; and there are vaccines to prevent both hepatitis A and hepatitis B infections. No vaccine is available for hepatitis C. To learn more about vaccines, for hepatitis A visit https://www.cdc.gov/hepatitis/hav/havfaq.htm#B1 and for hepatitis B visit https://www.cdc.gov/hepatitis/hbv/hbvfaq.htm#vaccFAQ.
For surveillance, it is important to remember that certain populations have higher levels of immunity, whether from vaccination or prior infection. In general, young people have been vaccinated at a higher rate because of childhood vaccine recommendations issued in 1991 for hepatitis B and starting in 1996 for hepatitis A.
SCREENING
For chronic hepatitis B and hepatitis C, certain groups at high risk should receive appropriate blood tests in order to detect the disease before the virus causes liver damage. The CDC recommends screening for current hepatitis B and hepatitis C infection based on patient characteristics (e.g., born from 1945–1965 for hepatitis C, and birth in countries with intermediate to high endemic hepatitis B) and risk behaviors. To learn more about testing, for hepatitis B visit https://www.cdc.gov/hepatitis/hbv/hbvfaq.htm#b5 and for hepatitis C visit https://www.cdc.gov/hepatitis/hcv/hcvfaq.htm#c1.
In addition to testing based on risk behaviors, hepatitis B screening recommendations for all pregnant women were introduced in 2007, and hepatitis C screening recommendations for persons born from 1945 to 1965 were introduced in 2012. For surveillance, it is important to remember that if certain populations and settings are prioritized for testing, more cases will be detected within those populations and settings.
TREATMENT
If a person develops acute viral hepatitis, supportive treatment and even hospitalization may be required. Antiviral therapies are typically effective and recommended for chronic hepatitis B or hepatitis C infections.
New drugs that can reliably cure hepatitis C have been available since 2013. To learn more about hepatitis B treatment, visit https://www.cdc.gov/hepatitis/hbv/hbvfaq.htm#b13 and for chronic hepatitis C visit https://www.cdc.gov/hepatitis/hcv/hcvfaq.htm#d3. As more people living with chronic hepatitis C infection are cured, mortality rates are expected to decline even for those with advanced liver damage due to chronic infection. In the context of public health surveillance, hepatitis C treatment will have an effect on the number and prevalence of chronic hepatitis C infections and the proportion of resolved cases versus currently infected
CASE DEFINITIONS
To ensure consistent reporting across states, the Council for State and Territorial Epidemiologists (CSTE) developed case definitions for viral hepatitis A, B, and C. The case definitions serve as a way to standardize reporting using uniform criteria and differentiate between acute and chronic cases. When new technologies are developed for laboratory testing or better clinical data becomes available, the case definitions are updated. Changes to case definitions should be considered when examining trends over time. For more information on 2017 case definitions, visit https://wwwn.cdc.gov/nndss/conditions/notifiable/2017/infectious-diseases/. There were no changes to case definitions for acute or chronic viral hepatitis; however, the case definition for perinatal hepatitis B was updated in 2017.
DATA SOURCES
In order for a health department to report diagnosed cases of viral hepatitis to the CDC, they must have systems in place that ensure each diagnosed case is detected. Due to varying state laws and infrastructure, not all health departments report all cases of acute or newly reported chronic viral hepatitis to the CDC.
Case reporting generally begins when a local or state health department receives a positive laboratory report, indicating an individual has one or more viral hepatitis infections. Since initial reporting provides limited information and clinical symptoms are frequently needed to classify cases as acute, reported cases may require extensive follow-up to obtain full information for establishing case status and case classification. Health departments prioritize cases for follow-up using their own protocols and may submit cases to CDC with incomplete or missing information. Additionally, the volume of laboratory reports for chronic viral hepatitis infections is so large that not all health departments are able to consistently detect and report all chronic cases to the CDC. This under-reporting translates into underestimation of chronic viral hepatitis cases when using state reports based on data from NNDSS. NNDSS data on chronic hepatitis B and hepatitis C are in this report where available; however these are newly identified chronic cases and do not measure prevalence.
To account for under-estimation, a probabilistic model to estimate the true incidence (symptomatic and asymptomatic cases) of acute hepatitis A, B, and C from reported (symptomatic) cases has been published previously (5). The model includes the probabilities of symptoms, referral to care and treatment, and rates of reporting to local and state health departments. The published multipliers have since been corrected by CDC to indicate that each reported case of acute hepatitis A represents 2.0 estimated cases (95% bootstrap confidence interval [CI], 1.4-2.2), each reported case of acute hepatitis B represents 6.5 estimated cases (95% CI, 3.7-15.9), and each reported case of acute hepatitis C represents 13.9 estimated cases (95% CI 11.0-47.4).
In 2017, the CDC provided funding to 14 states to perform enhanced surveillance of hepatitis B and hepatitis C through a cooperative agreement. Previously, only five states and two cities were funded from 2013–2016. Funding states for enhanced surveillance improves detection of cases and completeness of reports.
Cases of viral hepatitis that are submitted to CDC by health departments are collected in NNDSS, for which information on acute cases in this report are based.
Deaths due to viral hepatitis among reported acute cases are submitted by states to CDC through NNDSS. Data entered on death certificates are also available to the CDC through the National Vital Statistics System (NVSS). Both data sources are used in this report and more information on NVSS mortality data is provided.
Figure 1.1. Actual number of acute viral hepatitis cases submitted to CDC by states and estimated* number of acute viral hepatitis cases — United States, 2010–2017.
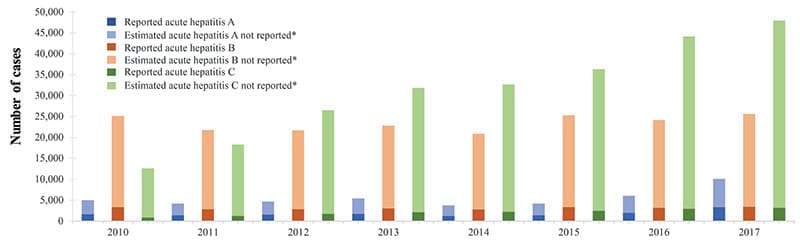
Source: CDC, National Notifiable Diseases Surveillance System.
* The number of estimated viral hepatitis cases was determined by multiplying the number of reported cases by a factor that adjusted for under-ascertainment and under-reporting (5). Corrected multipliers and confidence intervals developed by the CDC are shown in the Appendix A. In this visual representation, the sum of reported and estimated not reported total the estimated number of acute cases.
HEPATITIS A
The number of reported hepatitis A cases declined after 2013 to 2015; however, person-to-person hepatitis A outbreaks in 2016 and 2017 among persons who used drugs and persons experiencing homelessness caused the number of cases to increase.
Figure 2.1. Actual number of hepatitis A cases submitted to CDC by states and estimated* number of hepatitis A cases — United States, 2013–2017.
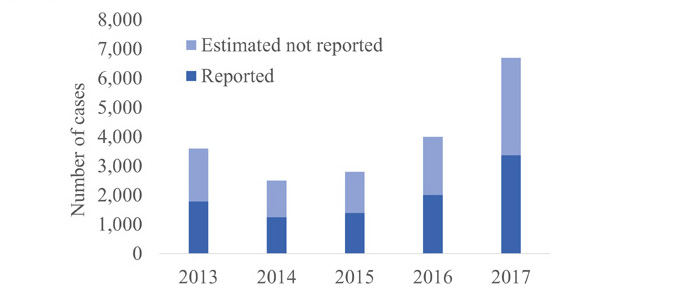
Source: CDC, National Notifiable Diseases Surveillance System.
* The number of estimated viral hepatitis cases was determined by multiplying the number of reported cases by a factor that adjusted for under-ascertainment and under-reporting (5). Corrected multipliers and confidence intervals developed by the CDC are shown in the Appendix A. In this visual representation, the sum of reported and estimated not reported total the estimated number of acute cases.
Downloads of this slide: PDFpdf icon PowerPointppt icon
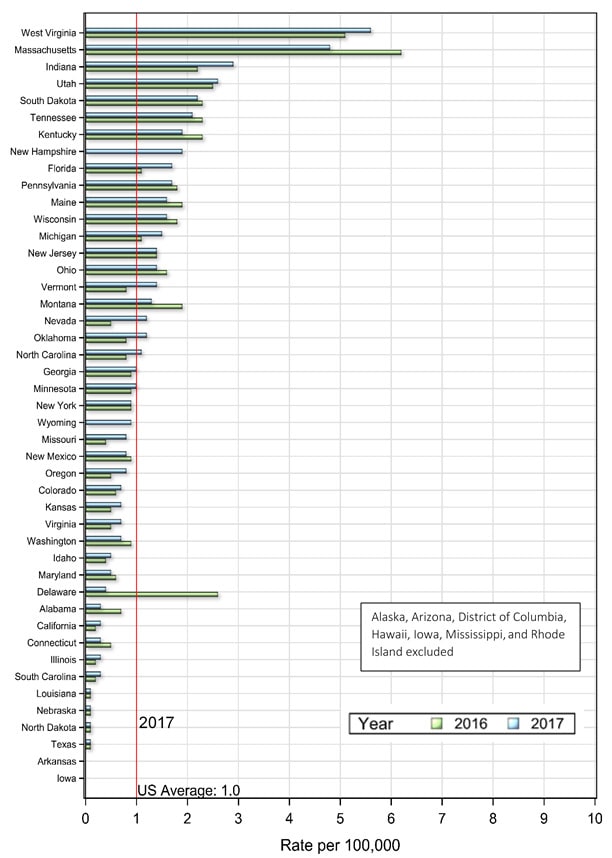
HEPATITIS A: ACUTE CASES BY STATE
Acute hepatitis A cases fluctuate when states experience outbreaks.
- Hawaii reported fewer cases of acute hepatitis A in 2017 compared to 2016, after a large foodborne outbreak occurred in 2016.
- California, Kentucky, Michigan, and Utah reported outbreaks of hepatitis A in 2017 (8). Epidemiologic investigations revealed that these were not common source or foodborne outbreaks, but instead person-to-person transmission among persons who use drugs and persons experiencing homelessness.
Table 2.1. Number and rate* of reported cases† of hepatitis A, by state or jurisdiction and nationally ― United States, 2013–2017.
| State | 2013 No. |
2013 Rate* |
2014 No. |
2014 Rate* |
2015 No. |
2015 Rate* |
2016 No. |
2016 Rate* |
2017 No. |
2017 Rate* |
|---|---|---|---|---|---|---|---|---|---|---|
| Alabama | 10 | 0.2 | 15 | 0.3 | 23 | 0.5 | 19 | 0.4 | 23 | 0.5 |
| Alaska | 1 | 0.1 | 1 | 0.1 | 4 | 0.5 | 2 | 0.3 | — | — |
| Arizona | 66 | 1.0 | 29 | 0.4 | 54 | 0.8 | 32 | 0.5 | 59 | 0.8 |
| Arkansas | 9 | 0.3 | 2 | 0.1 | 10 | 0.3 | 13 | 0.4 | 7 | 0.2 |
| California | 255 | 0.7 | 142 | 0.4 | 179 | 0.5 | 229 | 0.6 | 947 | 2.4 |
| Colorado | 51 | 1.0 | 23 | 0.4 | 25 | 0.5 | 22 | 0.4 | 65 | 1.2 |
| Connecticut | 19 | 0.5 | 23 | 0.6 | 9 | 0.3 | 16 | 0.4 | 17 | 0.5 |
| Delaware | 4 | 0.4 | 1 | 0.1 | 2 | 0.2 | 1 | 0.1 | 6 | 0.6 |
| District of Columbia | — | — | U | U | U | U | 4 | 0.6 | 3 | 0.4 |
| Florida | 115 | 0.6 | 90 | 0.5 | 108 | 0.5 | 115 | 0.6 | 261 | 1.2 |
| Georgia | 36 | 0.4 | 24 | 0.2 | 30 | 0.3 | 44 | 0.4 | 24 | 0.2 |
| Hawaii | 16 | 1.1 | 5 | 0.4 | 6 | 0.4 | 285 | 20 | 8 | 0.6 |
| Idaho | 8 | 0.5 | 7 | 0.4 | 9 | 0.5 | 7 | 0.4 | 4 | 0.2 |
| Illinois | 79 | 0.6 | 82 | 0.6 | 57 | 0.4 | 71 | 0.6 | 73 | 0.6 |
| Indiana | 32 | 0.5 | 20 | 0.3 | 19 | 0.3 | 18 | 0.3 | 21 | 0.3 |
| Iowa | 17 | 0.6 | 12 | 0.4 | 16 | 0.5 | 16 | 0.5 | 9 | 0.3 |
| Kansas | 11 | 0.4 | 7 | 0.2 | 7 | 0.2 | 5 | 0.2 | 6 | 0.2 |
| Kentucky | 24 | 0.5 | 19 | 0.4 | 16 | 0.4 | 9 | 0.2 | 71 | 1.6 |
| Louisiana | 14 | 0.3 | 5 | 0.1 | 5 | 0.1 | 12 | 0.3 | 8 | 0.2 |
| Maine | 10 | 0.8 | 8 | 0.6 | 8 | 0.6 | 8 | 0.6 | 7 | 0.5 |
| Maryland | 29 | 0.5 | 27 | 0.5 | 19 | 0.3 | 37 | 0.6 | 29 | 0.5 |
| Massachusetts | 43 | 0.6 | 43 | 0.6 | 34 | 0.5 | 64 | 0.9 | 52 | 0.8 |
| Michigan | 83 | 0.8 | 45 | 0.5 | 51 | 0.5 | 112 | 1.1 | 670 | 6.7 |
| Minnesota | 32 | 0.6 | 19 | 0.3 | 21 | 0.4 | 15 | 0.3 | 30 | 0.5 |
| Mississippi | 5 | 0.2 | 3 | 0.1 | 2 | 0.1 | 2 | 0.1 | 3 | 0.1 |
| Missouri | 8 | 0.1 | 20 | 0.3 | 9 | 0.1 | 16 | 0.3 | 27 | 0.4 |
| Montana | 6 | 0.6 | 5 | 0.5 | 2 | 0.2 | 3 | 0.3 | 3 | 0.3 |
| Nebraska | 13 | 0.7 | 9 | 0.5 | 6 | 0.3 | 21 | 1.1 | 4 | 0.2 |
| Nevada | 19 | 0.7 | 5 | 0.2 | 11 | 0.4 | 14 | 0.5 | 19 | 0.6 |
| New Hampshire | 9 | 0.7 | 5 | 0.4 | 2 | 0.2 | 8 | 0.6 | 7 | 0.5 |
| New Jersey | 68 | 0.8 | 59 | 0.7 | 59 | 0.7 | 74 | 0.8 | 71 | 0.8 |
| New Mexico | 20 | 1.0 | 8 | 0.4 | 6 | 0.3 | 4 | 0.2 | 4 | 0.2 |
| New York | 167 | 0.8 | 84 | 0.4 | 123 | 0.6 | 99 | 0.5 | 218 | 1.1 |
| North Carolina | 46 | 0.5 | 38 | 0.4 | 45 | 0.4 | 52 | 0.5 | 29 | 0.3 |
| North Dakota | 9 | 1.2 | 9 | 1.2 | 5 | 0.7 | 2 | 0.3 | — | — |
| Ohio | 59 | 0.5 | 32 | 0.3 | 36 | 0.3 | 36 | 0.3 | 45 | 0.4 |
| Oklahoma | 14 | 0.4 | 17 | 0.4 | 11 | 0.3 | 11 | 0.3 | 9 | 0.2 |
| Oregon | 29 | 0.7 | 13 | 0.3 | 28 | 0.7 | 15 | 0.4 | 20 | 0.5 |
| Pennsylvania | 53 | 0.4 | 48 | 0.4 | 43 | 0.3 | 62 | 0.5 | 69 | 0.5 |
| Rhode Island | 4 | 0.4 | 8 | 0.8 | 4 | 0.4 | 4 | 0.4 | 6 | 0.6 |
| South Carolina | 14 | 0.3 | 6 | 0.1 | 16 | 0.3 | 21 | 0.4 | 21 | 0.4 |
| South Dakota | 4 | 0.5 | 3 | 0.4 | 2 | 0.2 | 1 | 0.1 | 1 | 0.1 |
| Tennessee | 20 | 0.3 | 12 | 0.2 | 14 | 0.2 | 7 | 0.1 | 6 | 0.1 |
| Texas | 109 | 0.4 | 124 | 0.5 | 147 | 0.5 | 139 | 0.5 | 129 | 0.5 |
| Utah | 12 | 0.4 | 8 | 0.3 | 8 | 0.3 | 12 | 0.4 | 159 | 5.1 |
| Vermont | 7 | 1.1 | 1 | 0.2 | 3 | 0.5 | 5 | 0.8 | 2 | 0.3 |
| Virginia | 36 | 0.4 | 27 | 0.3 | 50 | 0.6 | 190 | 2.3 | 46 | 0.5 |
| Washington | 45 | 0.6 | 26 | 0.4 | 26 | 0.4 | 31 | 0.4 | 28 | 0.4 |
| West Virginia | 4 | 0.2 | 12 | 0.6 | 8 | 0.4 | 15 | 0.8 | 6 | 0.3 |
| Wisconsin | 37 | 0.6 | 7 | 0.1 | 9 | 0.2 | 7 | 0.1 | 16 | 0.3 |
| Wyoming | — | — | 1 | 0.2 | 3 | 0.5 | — | — | 18 | 3.1 |
| U.S. | 1,781 | 0.6 | 1,239 | 0.4 | 1,390 | 0.4 | 2,007 | 0.6 | 3,366 | 1.0 |
Source: CDC, National Notifiable Diseases Surveillance System.
* Rate per 100,000 population.
† For case definition, see https://wwwn.cdc.gov/nndss/conditions/hepatitis-a-acute/
—: No reported cases. The reporting jurisdiction did not submit any cases to CDC.
U: Unavailable. The data are unavailable.
Figure 2.2. Rates of reported hepatitis A cases, by state compared to the 2017 overall rate of hepatitis A — United States, 2016 and 2017.
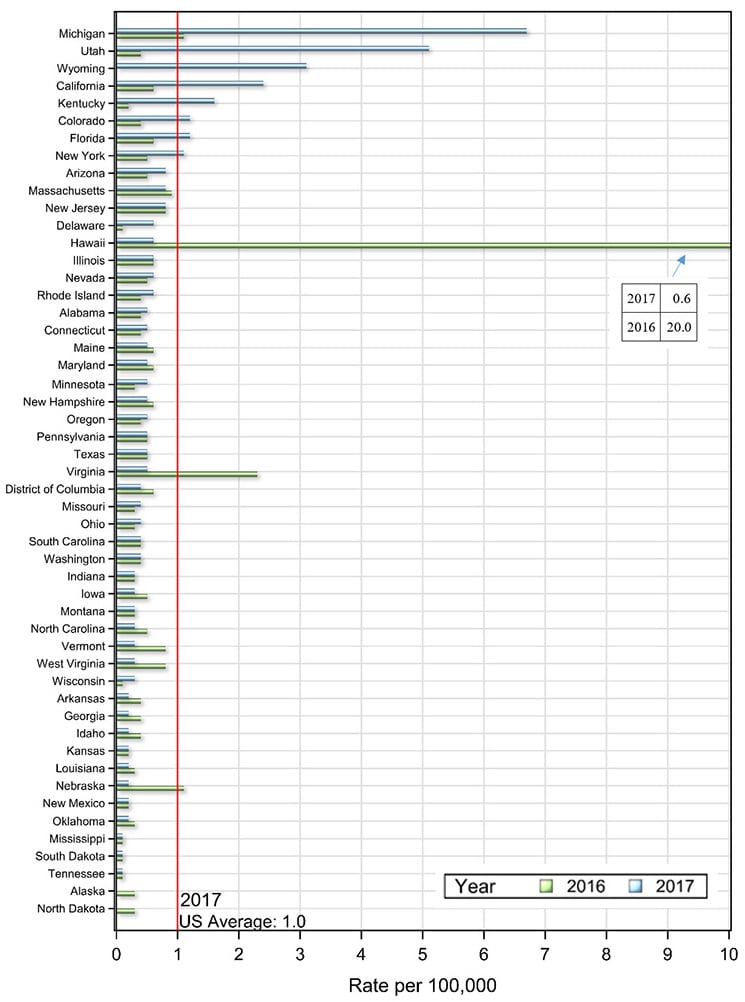
Source: CDC, National Notifiable Diseases Surveillance System.
Downloads of this slide: PDFpdf icon
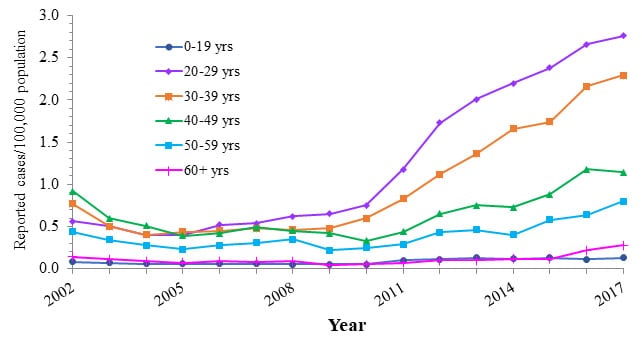
HEPATITIS A: SUBGROUP TRENDS
Adult age groups influence the trend in reported hepatitis A cases per 100,000 population for two main reasons:
- Rates of hepatitis A infection remain low in children and adolescents due to childhood vaccination recommendations for hepatitis A starting in 1996.
- Change in the epidemiology including population-level immunity, source of infection, and affected populations.
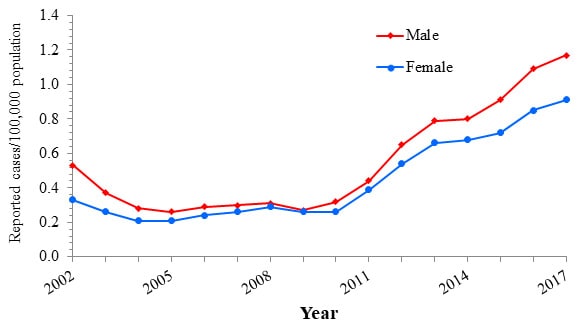
In 2017, rates of reported hepatitis A cases increased more markedly for males than for females, consistent with higher rates of drug use among men compared to women (9).
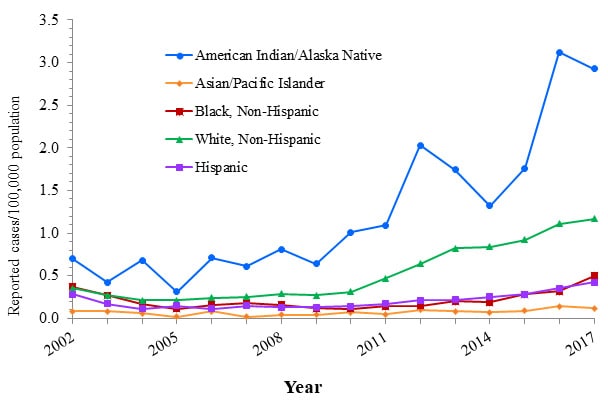
Trends by race/ethnicity revealed the following:
- The incidence among Asian/Pacific Islanders returned to the 2015 rate following an uptick in 2016 that was likely due to the ending of a large foodborne outbreak that occurred in Hawaii.
- The incidence among all other race/ethnicity groups increased from 2016 to 2017.
Figure 2.3. Rates of reported hepatitis A, by age group — United States, 2002–2017.
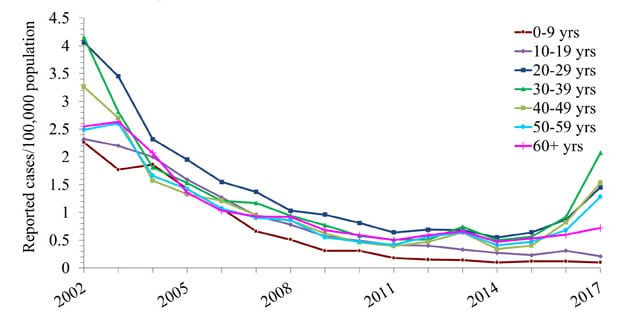
Source: CDC, National Notifiable Diseases Surveillance System.
Downloads of this slide: PDFpdf icon PowerPointppt icon
Figure 2.4. Rates of reported hepatitis A, by sex — United States, 2002–2017.
Source: CDC, National Notifiable Diseases Surveillance System.
Downloads of this slide: PDFpdf icon PowerPointppt icon
Figure 2.5. Rates of reported hepatitis A, by race/ethnicity — United States, 2002–2017.
Source: CDC, National Notifiable Diseases Surveillance System.
Downloads of this slide: PDFpdf icon PowerPointppt icon
Table 2.2. Number and rate* of reported cases† of hepatitis A, by selected characteristics — United States 2013–2017.
| 2013 No. |
2013 Rate* |
2014 No. |
2014 Rate* |
2015 No. |
2015 Rate* |
2016 No. |
2016 Rate* |
2017 No. |
2017 Rate* |
|
|---|---|---|---|---|---|---|---|---|---|---|
| Total§ | 1,781 | 0.6 | 1,239 | 0.4 | 1,390 | 0.4 | 2,007 | 0.6 | 3,366 | 1.0 |
| Age group | ||||||||||
| 0 – 9 years | 57 | 0.1 | 41 | 0.1 | 48 | 0.1 | 47 | 0.1 | 40 | 0.1 |
| 10 – 19 years | 138 | 0.3 | 114 | 0.3 | 97 | 0.2 | 131 | 0.3 | 86 | 0.2 |
| 20 – 29 years | 299 | 0.7 | 246 | 0.5 | 287 | 0.6 | 392 | 0.9 | 659 | 1.4 |
| 30 – 39 years | 302 | 0.7 | 207 | 0.5 | 233 | 0.6 | 391 | 0.9 | 893 | 2.1 |
| 40 – 49 years | 267 | 0.6 | 139 | 0.3 | 164 | 0.4 | 333 | 0.8 | 621 | 1.5 |
| 50 – 59 years | 278 | 0.6 | 182 | 0.4 | 205 | 0.5 | 297 | 0.7 | 554 | 1.3 |
| 60+ years | 415 | 0.7 | 304 | 0.5 | 353 | 0.5 | 409 | 0.6 | 509 | 0.7 |
| Sex | ||||||||||
| Male | 864 | 0.6 | 645 | 0.4 | 726 | 0.5 | 1,107 | 0.7 | 2,209 | 1.4 |
| Female | 914 | 0.6 | 591 | 0.4 | 662 | 0.4 | 897 | 0.5 | 1,149 | 0.7 |
| Race/ethnicity | ||||||||||
| American Indian/Alaskan Native | 7 | 0.3 | 4 | 0.2 | 5 | 0.2 | 3 | 0.1 | 13 | 0.5 |
| Asian/Pacific Islander | 101 | 0.6 | 135 | 0.7 | 114 | 0.6 | 299 | 1.5 | 124 | 0.6 |
| Black, Non-Hispanic | 75 | 0.2 | 82 | 0.2 | 71 | 0.2 | 137 | 0.3 | 303 | 0.7 |
| White, Non-Hispanic | 962 | 0.5 | 566 | 0.3 | 701 | 0.3 | 865 | 0.4 | 1,979 | 1.0 |
| Hispanic | 278 | 0.5 | 211 | 0.4 | 219 | 0.4 | 293 | 0.5 | 471 | 0.8 |
| HHS Region¶ | ||||||||||
| Region 1 | 92 | 0.6 | 88 | 0.6 | 60 | 0.4 | 105 | 0.7 | 91 | 0.6 |
| Region 2 | 235 | 0.8 | 143 | 0.5 | 182 | 0.6 | 173 | 0.6 | 289 | 1.0 |
| Region 3 | 126 | 0.4 | 115 | 0.4 | 122 | 0.4 | 309 | 1.0 | 159 | 0.5 |
| Region 4 | 270 | 0.4 | 207 | 0.3 | 254 | 0.4 | 269 | 0.4 | 438 | 0.7 |
| Region 5 | 322 | 0.6 | 205 | 0.4 | 193 | 0.4 | 259 | 0.5 | 855 | 1.6 |
| Region 6 | 166 | 0.4 | 156 | 0.4 | 179 | 0.4 | 179 | 0.4 | 157 | 0.4 |
| Region 7 | 49 | 0.4 | 48 | 0.3 | 38 | 0.3 | 58 | 0.4 | 46 | 0.3 |
| Region 8 | 82 | 0.7 | 49 | 0.4 | 45 | 0.4 | 40 | 0.3 | 246 | 2.1 |
| Region 9 | 356 | 0.7 | 181 | 0.4 | 250 | 0.5 | 560 | 1.1 | 1,033 | 2.0 |
| Region 10 | 83 | 0.6 | 47 | 0.4 | 67 | 0.5 | 55 | 0.4 | 52 | 0.4 |
Source: CDC, National Notifiable Diseases Surveillance System.
* Rate per 100,000 population.
† For the case definition, see https://wwwn.cdc.gov/nndss/conditions/hepatitis-a-acute/
§ Numbers reported in each category may not add up to the total number of reported cases in a year due to cases with missing data or, in the case of race/ethnicity, cases categorized as “Other”.
¶ Health and Human Services Regions were categorized according to the grouping of states and US territories assigned under each of the ten Department of Health and Human Services regional offices (https://www.hhs.gov/about/agencies/iea/regional-offices/index.htmlexternal icon). For the purposes of this report, regions with US territories (Region 2 and Region 9) contain data from states only.
HEPATITIS A: RISK FACTORS
Risk data were missing for 46.6% of reported hepatitis A cases reported to CDC in 2017, up slightly from 45.7% in 2016.
The most common risk factors reported in 2017 were injection drug use, person-to-person and foodborne outbreaks, and sexual/household contact with a hepatitis A patient.
Figure 2.6. Availability of information on risk behaviors/exposures* associated with reported cases of hepatitis A — United States, 2017.
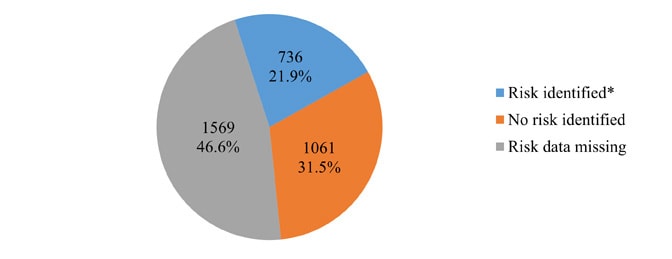
Source: CDC, National Notifiable Diseases Surveillance System.
* Includes case reports indicating the presence of at least one of the following risks 2–6 weeks prior to onset of symptomatic hepatitis A: 1) traveled to hepatitis A-endemic regions of Mexico, South/Central America, Africa, Asia/South Pacific, or the Middle East; 2) sexual/household or other contact with suspected/confirmed hepatitis A patient; 3) a child/employee in day-care center/nursery/preschool or having had contact with such persons; 4) involved in a foodborne/waterborne outbreak; 5) being a man who has sex with men; and 6) injection drug use.
Downloads of this slide: PDFpdf icon PowerPointppt icon
Figure 2.7. Reported cases of hepatitis A*, by risk behavior/exposure† — United States, 2017.
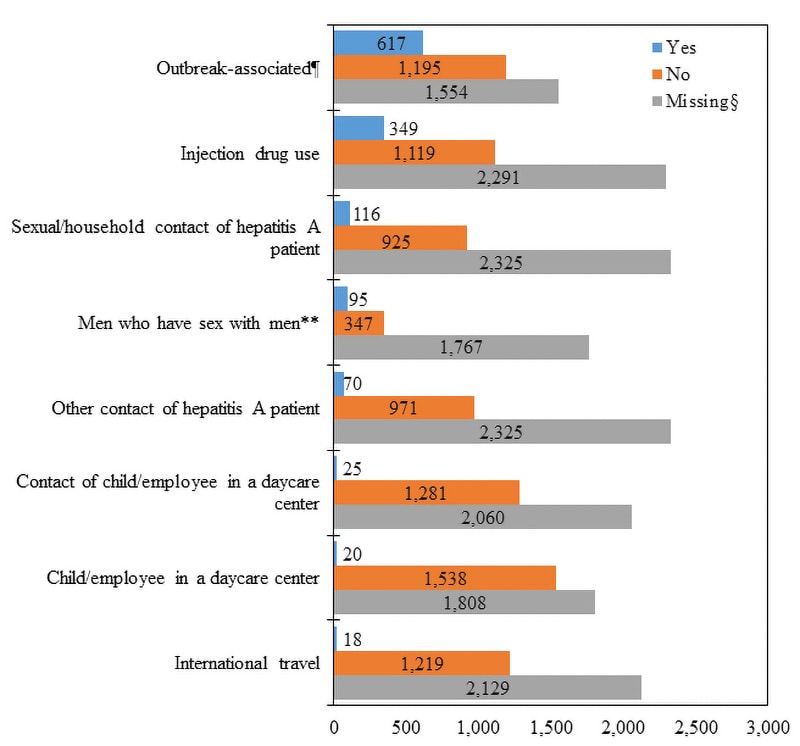
Source: CDC, National Notifiable Diseases Surveillance System.
* A total of 3,366 case reports of hepatitis A were received in 2017.
† More than one risk behavior/exposure may be indicated on each case report.
§ No risk data reported.
¶ Associated with person-to-person or foodborne outbreak.
** A total of 2,209 hepatitis A cases were reported among males in 2017.
Downloads of this slide: PDF pdf icon[PDF – 138 KB] PowerPointppt icon
HEPATITIS A: HOSPITALIZATION
Hospitalization data were missing for 49.0% of hepatitis A cases reported to CDC in 2017, up from 45.3% in 2016.
Of those with hospitalization data, 67.2% (1,154 of 1,717) were hospitalized in 2017, which was substantially higher than 41.6% in 2016.
HEPATITIS A: MORTALITY
In 2017, there were 91 death certificates among US residents that listed hepatitis A as the underlying or a contributing cause of death.
- While the rates did not change over time, the number of death certificates with hepatitis A listed increased from 70 in 2016 to 91 in 2017.
- The increase in the number of deaths in 2017 was likely due to the increasing number of cases associated with outbreaks.
Only 24 hepatitis A deaths were reported through NNDSS. No additional information, including US resident status, was submitted through NNDSS.
Table 2.3. Number and rate* of deaths with hepatitis A listed as a cause of death† among US residents, by demographic characteristic and year – United States, 2013-2017.
| Demographic characteristic | 2013 No. |
2013 Rate (95% CI)§ |
2014 No. |
2014 Rate (95% CI) |
2015 No. |
2015 Rate (95% CI) |
2016 No. |
2016 Rate (95% CI) |
2017 No. |
2017 Rate (95% CI) |
|---|---|---|---|---|---|---|---|---|---|---|
| Age Group (years) | ||||||||||
| 0–44 | 4 | – | 4 | – | 5 | – | 6 | – | 9 | – |
| 45–64 | 43 | 0.05 (0.04-0.07) |
35 | 0.04 (0.03-0.06) |
25 | 0.03 (0.02-0.04) |
33 | 0.04 (0.03-0.06) |
35 | 0.04 (0.03-0.06) |
| 65+ | 33 | 0.07 (0.05-0.10) |
37 | 0.08 (0.06-0.11) |
37 | 0.08 (0.05-0.11) |
31 | 0.06 (0.04-0.09) |
47 | 0.09 (0.07-0.12) |
| Race/ethnicity | ||||||||||
| White, non-Hispanic | 63 | 0.02 (0.02-0.03) |
51 | 0.02 (0.02-0.03) |
45 | 0.01 (0.00-0.01) |
50 | 0.02 (0.01-0.02) |
69 | 0.02 (0.02-0.03) |
| Other | 17 | – | 25 | – | 22 | – | 20 | – | 21 | – |
| Sex | ||||||||||
| Male | 50 | 0.03 (0.02-0.04) |
42 | 0.02 (0.01-0.03) |
38 | 0.02 (0.01-0.03) |
38 | 0.01 (0.01-0.02) |
63 | 0.03 (0.02-0.03) |
| Female | 30 | 0.01 (0.00-0.01) |
34 | 0.01 (0.01-0.02) |
29 | 0.01 (0.00-0.01) |
32 | 0.01 (0.01-0.02) |
28 | 0.00 (0.00-0.00) |
| Overall | 80 | 0.02 (0.02-0.03) |
76 | 0.02 (0.02-0.03) |
67 | 0.01 (0.01-0.02) |
70 | 0.01 (0.00-0.01) |
91 | 0.02 (0.02-0.03) |
Source: CDC, National Center for Health Statistics, Multiple Cause of Death 1999–2017 on CDC WONDER Online Database. Data are from the 2013–2017 Multiple Cause of Death files and are based on information from all death certificates filed in the vital records offices of the fifty states and the District of Columbia through the Vital Statistics Cooperative Program. Deaths of nonresidents (e.g., nonresident aliens, nationals living abroad, residents of Puerto Rico, Guam, the Virgin Islands, and other territories of the US) and fetal deaths are excluded. Accessed at http://wonder.cdc.gov/mcd-icd10.html on August 23, 2019. CDC WONDER dataset documentation and technical methods can be accessed at https://wonder.cdc.gov/wonder/help/mcd.html#.
* Rates for race/ethnicity, sex, and the overall total are age-adjusted per 100,000 U.S. standard population in 2000 using the following age group distribution (in years): <1, 1–4, 5–14, 15–24, 25–34, 35–44, 45–54, 55–64, 65–74, 75–84, and 85+. Missing data are not included. Rates where death counts were less than 20 were not displayed due to the instability associated with those rates or where CDC WONDER did not have the functionality to calculate rates (e.g., for the “Other” race/ethnicity group). For age-adjusted death rates, the age-specific death rate is rounded to one decimal place before proceeding to the next step in the calculation of age-adjusted death rates for NCHS Multiple Cause of Death on CDC WONDER. This rounding step may affect the precision of rates calculated for small numbers of deaths.
† Cause of death is defined as one of the multiple causes of death and is based on the International Classification of Diseases, 10th Revision (ICD-10) codes B15 (hepatitis A).
Note: Numbers are slightly lower than previously reported for 2013–2016 due to NCHS standards which restrict displayed data to US residents.
HEPATITIS B
The number of reported acute hepatitis B cases has remained stable with a slight increase in 2017. The trend is influenced by improved immunization, increasing injection drug use related to the opioid crisis (10), and improved surveillance.
Figure 3.1. Actual number of acute hepatitis B cases submitted to CDC by states and estimated* number of acute hepatitis B cases — United States, 2013–2017.
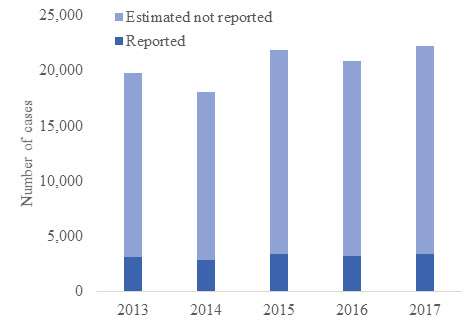
Source: CDC, National Notifiable Diseases Surveillance System.
* The number of estimated viral hepatitis cases was determined by multiplying the number of reported cases by a factor that adjusted for under-ascertainment and under-reporting (5). Corrected multipliers and confidence intervals developed by the CDC are shown in the Appendix A. In this visual representation, the sum of reported and estimated not reported total the estimated number of acute cases.
Downloads of this slide: PDFpdf icon PowerPointppt icon
HEPATITIS B: ACUTE CASES BY STATE
While national incidence of acute hepatitis B has been relatively stable, in 2017 certain states experienced increases. State-level trends were influenced by the opioid crisis (10) and lack of protection among populations for whom vaccination is recommended.
Table 3.1. Number and rate* of reported cases† of acute hepatitis B, by state or jurisdiction and nationally ― United States, 2013–2017.
| State | 2013 No. |
2013 Rate* |
2014 No. |
2014 Rate* |
2015 No. |
2015 Rate* |
2016 No. |
2016 Rate* |
2017 No. |
2017 Rate* |
|---|---|---|---|---|---|---|---|---|---|---|
| Alabama | 90 | 1.9 | 117 | 2.4 | 101 | 2.1 | 59 | 1.2 | 82 | 1.7 |
| Alaska | 1 | 0.1 | 3 | 0.4 | 3 | 0.4 | 6 | 0.8 | 9 | 1.2 |
| Arizona | 28 | 0.4 | 31 | 0.5 | 25 | 0.4 | 14 | 0.2 | 26 | 0.4 |
| Arkansas | 50 | 1.7 | 28 | 0.9 | 36 | 1.2 | 49 | 1.6 | 46 | 1.5 |
| California | 138 | 0.4 | 110 | 0.3 | 160 | 0.4 | 115 | 0.3 | 126 | 0.3 |
| Colorado | 24 | 0.5 | 29 | 0.5 | 28 | 0.5 | 28 | 0.5 | 32 | 0.6 |
| Connecticut | 8 | 0.2 | 9 | 0.3 | 6 | 0.2 | 7 | 0.2 | 10 | 0.3 |
| Delaware | 14 | 1.5 | 8 | 0.9 | 8 | 0.8 | 3 | 0.3 | 9 | 0.9 |
| District of Columbia | — | — | U | U | U | U | U | U | U | U |
| Florida | 323 | 1.7 | 313 | 1.6 | 432 | 2.1 | 558 | 2.7 | 588 | 2.8 |
| Georgia | 104 | 1.0 | 103 | 1.0 | 119 | 1.2 | 100 | 1.0 | 106 | 1.0 |
| Hawaii | 4 | 0.3 | 6 | 0.4 | 14 | 1.0 | — | — | — | — |
| Idaho | 13 | 0.8 | 6 | 0.4 | 8 | 0.5 | 6 | 0.4 | 6 | 0.3 |
| Illinois | 94 | 0.7 | 58 | 0.5 | 55 | 0.4 | 37 | 0.3 | 27 | 0.2 |
| Indiana | 101 | 1.5 | 126 | 1.9 | 133 | 2.0 | 146 | 2.2 | 170 | 2.5 |
| Iowa | 11 | 0.4 | 9 | 0.3 | 16 | 0.5 | 10 | 0.3 | 12 | 0.4 |
| Kansas | 11 | 0.4 | 11 | 0.4 | 19 | 0.7 | 21 | 0.7 | 24 | 0.8 |
| Kentucky | 214 | 4.9 | 164 | 3.7 | 162 | 3.7 | 222 | 5.0 | 236 | 5.3 |
| Louisiana | 82 | 1.8 | 87 | 1.9 | 87 | 1.9 | 48 | 1.0 | 73 | 1.6 |
| Maine | 11 | 0.8 | 12 | 0.9 | 9 | 0.7 | 53 | 4.0 | 77 | 5.8 |
| Maryland | 43 | 0.7 | 40 | 0.7 | 40 | 0.7 | 27 | 0.4 | 34 | 0.6 |
| Massachusetts | 71 | 1.1 | 30 | 0.4 | 25 | 0.4 | 31 | 0.5 | 51 | 0.7 |
| Michigan | 53 | 0.5 | 50 | 0.5 | 56 | 0.6 | 45 | 0.5 | 61 | 0.6 |
| Minnesota | 19 | 0.4 | 16 | 0.3 | 19 | 0.3 | 21 | 0.4 | 23 | 0.4 |
| Mississippi | 55 | 1.8 | 48 | 1.6 | 50 | 1.7 | 31 | 1.0 | 44 | 1.5 |
| Missouri | 61 | 1.0 | 31 | 0.5 | 35 | 0.6 | 40 | 0.7 | 31 | 0.5 |
| Montana | 4 | 0.4 | — | — | 4 | 0.4 | 1 | 0.1 | 3 | 0.3 |
| Nebraska | 9 | 0.5 | 8 | 0.4 | 3 | 0.2 | 8 | 0.4 | 10 | 0.5 |
| Nevada | 29 | 1.0 | 21 | 0.7 | 25 | 0.9 | 22 | 0.7 | 30 | 1.0 |
| New Hampshire | 2 | 0.2 | 4 | 0.3 | — | — | — | — | — | — |
| New Jersey | 65 | 0.7 | 77 | 0.9 | 85 | 0.9 | 59 | 0.7 | 57 | 0.6 |
| New Mexico | 3 | 0.1 | 2 | 0.1 | 2 | 0.1 | 1 | 0.0 | 1 | 0.0 |
| New York | 117 | 0.6 | 95 | 0.5 | 80 | 0.4 | 103 | 0.5 | 81 | 0.4 |
| North Carolina | 75 | 0.8 | 100 | 1.0 | 165 | 1.6 | 170 | 1.7 | 190 | 1.8 |
| North Dakota | — | — | — | — | 2 | 0.3 | 2 | 0.3 | — | — |
| Ohio | 225 | 1.9 | 171 | 1.5 | 409 | 3.5 | 299 | 2.6 | 285 | 2.4 |
| Oklahoma | 40 | 1.0 | 57 | 1.5 | 37 | 0.9 | 32 | 0.8 | 41 | 1.0 |
| Oregon | 32 | 0.8 | 32 | 0.8 | 24 | 0.6 | 20 | 0.5 | 23 | 0.6 |
| Pennsylvania | 43 | 0.3 | 68 | 0.5 | 61 | 0.5 | 43 | 0.3 | 69 | 0.5 |
| Rhode Island | U | U | U | U | U | U | U | U | U | U |
| South Carolina | 58 | 1.2 | 37 | 0.8 | 30 | 0.6 | 34 | 0.7 | 40 | 0.8 |
| South Dakota | 5 | 0.6 | 3 | 0.4 | 2 | 0.2 | 2 | 0.2 | 2 | 0.2 |
| Tennessee | 262 | 4.0 | 232 | 3.5 | 243 | 3.7 | 204 | 3.1 | 215 | 3.2 |
| Texas | 142 | 0.5 | 122 | 0.5 | 159 | 0.6 | 156 | 0.6 | 106 | 0.4 |
| Utah | 5 | 0.2 | 11 | 0.4 | 10 | 0.3 | 5 | 0.2 | 18 | 0.6 |
| Vermont | 2 | 0.3 | 4 | 0.6 | 3 | 0.5 | 2 | 0.3 | 1 | 0.2 |
| Virginia | 72 | 0.9 | 61 | 0.7 | 69 | 0.8 | 56 | 0.7 | 61 | 0.7 |
| Washington | 33 | 0.5 | 44 | 0.6 | 34 | 0.5 | 45 | 0.6 | 45 | 0.6 |
| West Virginia | 195 | 10.5 | 186 | 10.1 | 272 | 14.7 | 268 | 14.6 | 212 | 11.7 |
| Wisconsin | 9 | 0.2 | 11 | 0.2 | 5 | 0.1 | 9 | 0.2 | 14 | 0.2 |
| Wyoming | — | — | U | U | U | U | U | U | 2 | 0.3 |
| Total | 3,050 | 1.0 | 2,791 | 0.9 | 3,370 | 1.1 | 3,218 | 1.0 | 3,409 | 1.1 |
Source: CDC, National Notifiable Diseases Surveillance System.
* Rate per 100,000 population.
† For case definition, see https://wwwn.cdc.gov/nndss/conditions/hepatitis-b-acute/
—: No reported cases. The reporting jurisdiction did not submit any cases to CDC.
N: Not reportable. The disease or condition was not reportable by law, statue, or regulation in the reporting jurisdiction.
U: Unavailable. The data are unavailable.
Figure 3.2. Rates of reported acute hepatitis B cases, by state compared to the 2017 overall rate of acute hepatitis B — United States, 2016 and 2017.
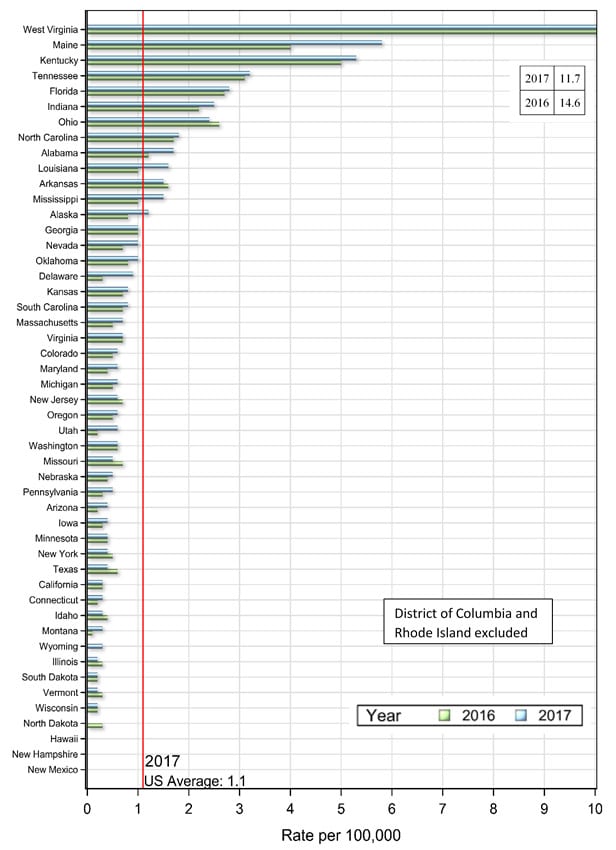
Source: CDC, National Notifiable Diseases Surveillance System.
Downloads of this slide: PDFpdf icon
HEPATITIS B: SUBGROUP TRENDS FOR ACUTE CASES
Age groups showed different trends in reported acute hepatitis B cases per 100,000 population:
- Rates of hepatitis B infection remained low in children and adolescents, likely due to childhood vaccinations.
- Rates decreased for young adults aged 20–29, likely because this is the first age cohort to reach young adulthood who were vaccinated as children or offered catch-up vaccination as adolescents. This group influenced the overall trend to remain stable, even as some older age groups experienced increases.
- For the first time between 2002 and 2017, adults aged 40–49 had the highest rate of acute hepatitis B in 2017. Risk factors such as injection drug use and having multiple sex partners, combined with lack of protection by vaccination, put older age groups at risk for infection.
Males have historically experienced higher rates of reported hepatitis B compared to females, consistent with risk factors being more common in males (8). Trends by race/ethnicity revealed the following differences in trends:
- For non-Hispanic whites, rates transitioned from being the lowest among all categories in 2002 to being the highest in 2015–2017.
- Rates among non-Hispanic blacks and American Indian/Alaska Natives were very high in 2002, subsequently decreased, and stabilized in recent years to just below the national average.
- Rates among Hispanics and Asians/Pacific Islanders were high in 2002, subsequently decreased, and stabilized in recent years to well below the national average.
Figure 3.3. Rates of reported acute hepatitis B, by age group — United States, 2002–2017.
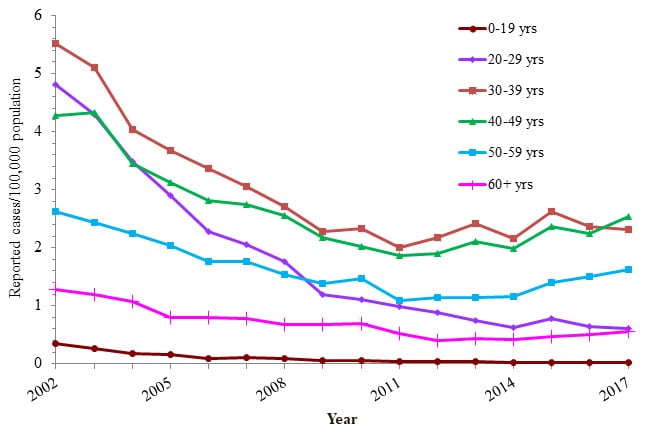
Source: CDC, National Notifiable Diseases Surveillance System.
Downloads of this slide: PDFpdf icon PowerPointppt icon
Figure 3.4. Rates of reported acute hepatitis B, by sex — United States, 2002–2017.
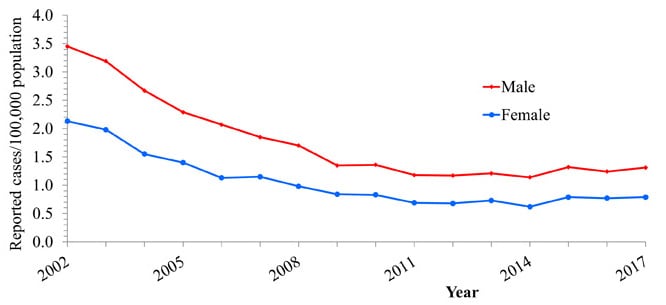
Source: CDC, National Notifiable Diseases Surveillance System.
Downloads of this slide: PDFpdf icon PowerPointppt icon
Figure 3.5. Rates of reported acute hepatitis B, by race/ethnicity — United States, 2002–2017.
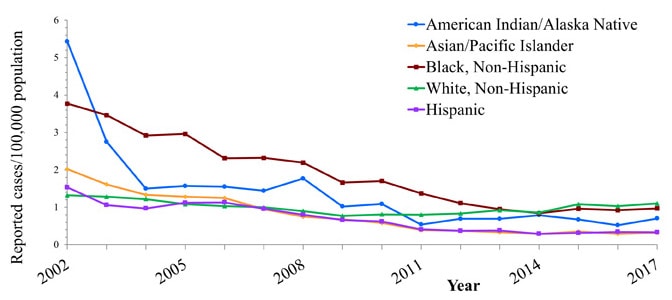
Source: CDC, National Notifiable Diseases Surveillance System.
Downloads of this slide: PDFpdf icon PowerPointppt icon
Table 3.2. Number and rate* of reported cases† of acute hepatitis B, by selected characteristics — United States 2013–2017.
| 2013 No. |
2013 Rate* |
2014 No. |
2014 Rate* |
2015 No. |
2015 Rate* |
2016 No. |
2016 Rate* |
2017 No. |
2017 Rate* |
|
|---|---|---|---|---|---|---|---|---|---|---|
| Total§ | 3,050 | 1.0 | 2,791 | 0.9 | 3,370 | 1.1 | 3,218 | 1.1 | 3,409 | 1.1 |
| Age group | ||||||||||
| 0 – 19 years | 25 | 0.0 | 14 | 0.0 | 19 | 0.0 | 18 | 0.0 | 16 | 0.0 |
| 20 – 29 years | 332 | 0.8 | 282 | 0.6 | 348 | 0.8 | 286 | 0.6 | 271 | 0.6 |
| 30 – 39 years | 980 | 2.4 | 888 | 2.2 | 1,094 | 2.6 | 1,000 | 2.4 | 998 | 2.3 |
| 40 – 49 years | 880 | 2.1 | 818 | 2.0 | 961 | 2.4 | 906 | 2.2 | 1,028 | 2.5 |
| 50 – 59 years | 496 | 1.1 | 504 | 1.2 | 615 | 1.4 | 655 | 1.5 | 700 | 1.6 |
| 60+ years | 272 | 0.4 | 272 | 0.4 | 312 | 0.5 | 342 | 0.5 | 395 | 0.6 |
| Sex | ||||||||||
| Male | 1,873 | 1.2 | 1,778 | 1.1 | 2,080 | 1.3 | 1,957 | 1.2 | 2,095 | 1.3 |
| Female | 1,163 | 0.7 | 1,001 | 0.6 | 1,280 | 0.8 | 1,252 | 0.8 | 1,301 | 0.8 |
| Race/ethnicity | ||||||||||
| American Indian/Alaskan Native | 18 | 0.7 | 21 | 0.8 | 18 | 0.7 | 14 | 0.5 | 19 | 0.7 |
| Asian/Pacific Islander | 58 | 0.3 | 53 | 0.3 | 67 | 0.4 | 56 | 0.3 | 64 | 0.3 |
| Black, Non-Hispanic | 382 | 0.9 | 343 | 0.8 | 398 | 1.0 | 386 | 0.9 | 411 | 1.0 |
| White, Non-Hispanic | 1,830 | 0.9 | 1,713 | 0.9 | 2,150 | 1.1 | 2,059 | 1.0 | 2,197 | 1.1 |
| Hispanic | 205 | 0.4 | 158 | 0.3 | 175 | 0.3 | 194 | 0.3 | 196 | 0.3 |
| HHS Region¶ | ||||||||||
| Region 1 | 94 | 0.7 | 59 | 0.4 | 43 | 0.3 | 93 | 0.7 | 139 | 1.0 |
| Region 2 | 182 | 0.6 | 172 | 0.6 | 165 | 0.6 | 162 | 0.6 | 138 | 0.5 |
| Region 3 | 367 | 1.2 | 363 | 1.2 | 450 | 1.5 | 397 | 1.3 | 385 | 1.3 |
| Region 4 | 1,181 | 1.9 | 1,114 | 1.8 | 1,302 | 2.0 | 1,378 | 2.1 | 1,501 | 2.3 |
| Region 5 | 501 | 1.0 | 432 | 0.8 | 677 | 1.3 | 557 | 1.1 | 580 | 1.1 |
| Region 6 | 317 | 0.8 | 296 | 0.7 | 321 | 0.8 | 286 | 0.7 | 267 | 0.6 |
| Region 7 | 92 | 0.7 | 59 | 0.4 | 73 | 0.5 | 79 | 0.6 | 77 | 0.5 |
| Region 8 | 38 | 0.4 | 43 | 0.4 | 46 | 0.4 | 38 | 0.3 | 57 | 0.5 |
| Region 9 | 199 | 0.4 | 168 | 0.3 | 224 | 0.4 | 151 | 0.3 | 182 | 0.4 |
| Region 10 | 79 | 0.6 | 85 | 0.6 | 69 | 0.5 | 77 | 0.6 | 83 | 0.6 |
Source: CDC, National Notifiable Diseases Surveillance System.
* Rate per 100,000 population.
† For the case definition, see https://wwwn.cdc.gov/nndss/conditions/hepatitis-b-acute/
§ Numbers reported in each category may not add up to the total number of reported cases in a year due to cases with missing data or, in the case of race/ethnicity, cases categorized as “Other”.
¶ Health and Human Services Regions were categorized according to the grouping of states and US territories assigned under each of the ten Department of Health and Human Services regional offices (https://www.hhs.gov/about/agencies/iea/regional-offices/index.htmlexternal icon). For the purposes of this report, regions with US territories (Region 2 and Region 9) contain data from states only.
HEPATITIS B: RISK FACTORS FOR ACUTE CASES
Risk data were missing for 37.4% of acute hepatitis B cases reported to CDC in 2017, down from 51.9% in 2016.
The most common risk factors reported in 2017 were injection drug use, multiple sex partners, and men who have sex with men.
Figure 3.6. Availability of information on risk behaviors/exposures* associated with reported cases of acute hepatitis B — United States, 2017.
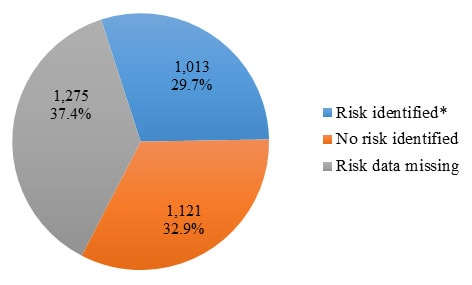
Source: CDC, National Notifiable Diseases Surveillance System.
* Includes case reports indicating the presence of at least one of the following risks 6 weeks to 6 months prior to onset of symptomatic hepatitis B: 1) injection drug use; 2) sexual contact with suspected/confirmed hepatitis B patient; 3) being a man who has sex with men; 4) multiple sex partners concurrently; 5) household contact with suspected/confirmed hepatitis B patient; 6) occupational exposure to blood; 7) hemodialysis patient; 8) received a blood transfusion; 9) sustained a percutaneous injury; and 10) underwent surgery.
Downloads of this slide: PDFpdf icon PowerPointppt icon
Figure 3.7. Reported cases of acute hepatitis B*, by risk behavior/exposure† — United States, 2017.
Source: CDC, National Notifiable Diseases Surveillance System.
* A total of 3,409 case reports of hepatitis B were received in 2017.
† More than one risk behavior/exposure may be indicated on each case report.
§ No risk data reported.
¶ A total of 2,095 acute hepatitis B cases were reported among males in 2017.
Downloads of this slide: PDFpdf icon PowerPointppt icon
HEPATITIS B: HOSPITALIZATION FOR ACUTE CASES
Hospitalization data were missing for 25.8% of acute hepatitis B cases submitted to CDC in 2017, down from 42.0% in 2016.
Of those with hospitalization data, 62.8% (1,589 of 2,530) were hospitalized in 2017, which was higher than 58.2% in 2016.
HEPATITIS B: CHRONIC CASES
In 2017, 38 states submitted 13,391 cases of chronic hepatitis B cases to CDC, which is less than the 14,847 cases submitted by 43 states in 2016.
Table 3.3. Number of newly reported cases* of confirmed chronic hepatitis B and reporting status, by state or jurisdiction — United States, 2017.
| State/Jurisdiction | No. chronic hepatitis B case reports submitted† |
|---|---|
| Alabama | N |
| Alaska | 50 |
| Arizona | 192 |
| Arkansas | N |
| California | — |
| Colorado | 129 |
| Connecticut | N |
| Delaware | 118 |
| District of Columbia | U |
| Florida | 2,117 |
| Georgia | 860 |
| Hawaii | U |
| Idaho | 53 |
| Illinois | 593 |
| Indiana | 285 |
| Iowa | 53 |
| Kansas | 60 |
| Kentucky | N |
| Louisiana | 184 |
| Maine | 60 |
| Maryland | 689 |
| Massachusetts | 406 |
| Michigan | 456 |
| Minnesota | 344 |
| Mississippi | N |
| Missouri | 411 |
| Montana | 23 |
| Nebraska | 59 |
| Nevada | 26 |
| New Hampshire | U |
| New Jersey | 244 |
| New Mexico | 39 |
| New York | 2,053 |
| North Carolina | 551 |
| North Dakota | 30 |
| Ohio | 733 |
| Oklahoma | 69 |
| Oregon | 122 |
| Pennsylvania | 870 |
| Rhode Island | — |
| South Carolina | 195 |
| South Dakota | 32 |
| Tennessee | N |
| Texas | N |
| Utah | 73 |
| Vermont | 44 |
| Virginia | 526 |
| Washington | 335 |
| West Virginia | 295 |
| Wisconsin | — |
| Wyoming | 12 |
| Total | 13,391 |
Source: CDC, National Notifiable Diseases Surveillance System.
* For case definition, see https://wwwn.cdc.gov/nndss/conditions/hepatitis-b-chronic/
† Reports may not reflect unique cases.
—: No reported cases. The reporting jurisdiction did not submit any cases to CDC.
N: Not reportable. The disease or condition was not reportable by law, statue, or regulation in the reporting jurisdiction.
U: Unavailable. The data are unavailable.
HEPATITIS B: MORTALITY
In 2017, there were 1,727 death certificates among US residents that listed hepatitis B as the underlying or a contributing cause of death.
- While the overall annual mortality rate remained constant during 2015—2017, the number of deaths decreased slightly from 2015 to 2016 and increased slightly from 2016 to 2017.
- While death rates steadily decreased each year among adults aged 55 to 64 years, older age groups did not experience the same decrease.
- Asians/Pacific Islanders have historically experienced the highest hepatitis B-related mortality rates, and the age-adjusted death rate for this group increased from 2015 to 2017.
- Males have historically experienced a higher age-adjusted hepatitis B-related mortality rate than females; this trend continued through 2017.
Only 23 hepatitis B deaths were reported through NNDSS. No additional information, including US resident status, was submitted through NNDSS.
Table 3.4. Number and rate* of deaths with hepatitis B listed as a cause of death† among US residents, by demographic characteristic and year – United States, 2013–2017.
| Demographic characteristic | 2013 No. |
2013 Rate (95% CI) |
2014 No. |
2014 Rate (95% CI) |
2015 No. |
2015 Rate (95% CI) |
2016 No. |
2016 Rate (95% CI) |
2017 No. |
2017 Rate (95% CI) |
|---|---|---|---|---|---|---|---|---|---|---|
| Age Group (years) | ||||||||||
| 0–34 | 39 | 0.03 (0.02-0.04) |
35 | 0.02 (0.02-0.03) |
30 | 0.02 (0.01- 0.03) |
39 | 0.03 (0.02-0.04) |
29 | 0.02 (0.01-0.03) |
| 35–44 | 146 | 0.36 (0.30-0.42) |
126 | 0.31 (0.26-0.37) |
118 | 0.29 (0.24-0.34) |
116 | 0.29 (0.23-0.34) |
106 | 0.26 (0.21-0.31) |
| 45–54 | 388 | 0.89 (0.80-0.97) |
384 | 0.88 (0.80-0.97) |
330 | 0.76 (0.68-0.85) |
324 | 0.76 (0.67-0.84) |
323 | 0.76 (0.68-0.85) |
| 55–64 | 701 | 1.78 (1.65-1.91) |
682 | 1.70 (1.57-1.83) |
610 | 1.49 (1.37-1.61) |
576 | 1.39 (1.28-1.50) |
548 | 1.30 (1.20-1.41) |
| 65–74 | 342 | 1.36 (1.21-1.50) |
356 | 1.35 (1.21-1.49) |
382 | 1.39 (1.25-1.53) |
383 | 1.34 (1.20-1.47) |
417 | 1.40 (1.27-1.54) |
| 75+ | 250 | 1.28 (1.12-1.44) |
254 | 1.28 (1.12-1.44) |
236 | 1.17 (1.02-1.32) |
252 | 1.22 (1.07-1.37) |
303 | 1.43 (1.27-1.59) |
| Race/ethnicity | ||||||||||
| White, NH (non-Hispanic) | 866 | 0.32 (0.30-0.34) |
851 | 0.33 (0.30-0.35) |
805 | 0.28 (0.26-0.30) |
767 | 0.29 (0.27-0.31) |
776 | 0.28 (0.26-0.30) |
| Black, NH | 384 | 0.98 (0.88-1.08) |
330 | 0.81 (0.72-0.89) |
318 | 0.75 (0.67-0.84) |
315 | 0.73 (0.65-0.81) |
320 | 0.74 (0.66-0.83) |
| Hispanic | 150 | 0.37 (0.31-0.43) |
156 | 0.40 (0.33-0.46) |
136 | 0.32 (0.27-0.38) |
128 | 0.30 (0.25-0.36) |
109 | 0.26 (0.21-0.32) |
| Asian/Pacific Islander | 446 | 2.59 (2.34-2.84) |
475 | 2.69 (2.44-2.93) |
419 | 2.23 (2.01-2.45) |
454 | 2.38 (2.16-2.60) |
492 | 2.45 (2.23-2.67) |
| American Indian/Alaskan Native |
13 | – | 10 | – | 13 | – | 16 | – | 17 | – |
| Sex | ||||||||||
| Male | 1,373 | 0.79 (0.75-0.83) |
1,301 | 0.74 (0.70-0.78) |
1,270 | 0.70 (0.66-0.74) |
1,231 | 0.67 (0.64-0.71) |
1,275 | 0.70 (0.66-0.74) |
| Female | 493 | 0.26 (0.23-0.28) |
536 | 0.27 (0.24-0.29) |
437 | 0.21 (0.19-0.23) |
459 | 0.22 (0.20-0.24) |
452 | 0.23 (0.20-0.25) |
| Overall | 1,866 | 0.53 (0.50-0.55) |
1,837 | 0.50 (0.47-0.52) |
1,707 | 0.46 (0.44-0.49) |
1,690 | 0.45 (0.43-0.48) |
1,727 | 0.46 (0.44-0.49) |
Source: CDC, National Center for Health Statistics, Multiple Cause of Death 1999–2017 on CDC WONDER Online Database. Data are from the 2013–2017 Multiple Cause of Death files and are based on information from all death certificates filed in the vital records offices of the fifty states and the District of Columbia through the Vital Statistics Cooperative Program. Deaths of nonresidents (e.g., nonresident aliens, nationals living abroad, residents of Puerto Rico, Guam, the Virgin Islands, and other territories of the US) and fetal deaths are excluded. Accessed at http://wonder.cdc.gov/mcd-icd10.html on August 23, 2019. CDC WONDER dataset documentation and technical methods can be accessed at https://wonder.cdc.gov/wonder/help/mcd.html#.
* Rates for race/ethnicity, sex, and the overall total are age-adjusted per 100,000 U.S. standard population in 2000 using the following age group distribution (in years): <1, 1–4, 5–14, 15–24, 25–34, 35–44, 45–54, 55–64, 65–74, 75–84, and 85+. Missing data are not included. Rates where death counts were less than 20 were not displayed due to the instability associated with those rates. For age-adjusted death rates, the age-specific death rate is rounded to one decimal place before proceeding to the next step in the calculation of age-adjusted death rates for NCHS Multiple Cause of Death on CDC WONDER. This rounding step may affect the precision of rates calculated for small numbers of deaths.
† Cause of death is defined as one of the multiple causes of death and is based on the International Classification of Diseases, 10th Revision (ICD-10) codes B16, B17.0, B18.0, B18.1 (hepatitis B).
Note: Numbers are slightly lower than previously reported for 2013–2016 due to NCHS standards which restrict displayed data to US residents.
PERINATAL HEPATITIS B
In 2017, 17 states notified CDC of perinatal hepatitis B cases, up from 13 in 2016.
Table 3.5. Number of newly reported cases* of perinatal hepatitis B, by state or jurisdiction — United States, 2017.
| State/Jurisdiction | No. Perinatal hepatitis B case reports submitted |
|---|---|
| Alabama | 1 |
| Arizona | 1 |
| California | 5 |
| Georgia | 1 |
| Hawaii | 2 |
| Indiana | 1 |
| Kentucky | 1 |
| Louisiana | 1 |
| Michigan | 1 |
| Mississippi | 1 |
| Nevada | 1 |
| New York | 5 |
| North Carolina | 2 |
| Ohio | 3 |
| Oregon | 1 |
| Pennsylvania | 2 |
| Texas | 2 |
| Total | 31 |
Source: CDC, National Notifiable Diseases Surveillance System.
*For case-definition, see https://wwwn.cdc.gov/nndss/conditions/hepatitis-b-perinatal-virus-infection/
HEPATITIS C
Steady increases in the number of reported acute hepatitis C cases have occurred each year since 2013. This trend is influenced by increasing injection drug use related to the opioid crisis (10) and improved surveillance.
Figure 4.1. Actual number of acute hepatitis C cases submitted to CDC by states and estimated* number of acute hepatitis C cases — United States, 2013–2017.
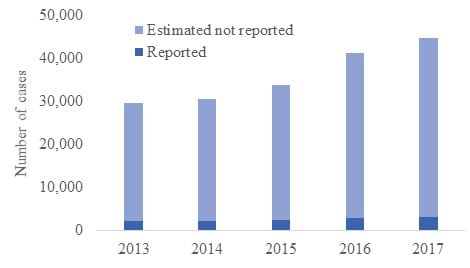
Source: CDC, National Notifiable Diseases Surveillance System.
* The number of estimated viral hepatitis cases was determined by multiplying the number of reported cases by a factor that adjusted for under-ascertainment and under-reporting (5). Corrected multipliers and confidence intervals developed by the CDC are shown in the Appendix A. In this visual representation, the sum of reported and estimated not reported total the estimated number of acute cases.
Downloads of this slide: PDFpdf icon PowerPointppt icon
HEPATITIS C: ACUTE CASES BY STATE
Most states experienced increases in reported acute hepatitis C infections from 2013 to 2017; trends varied from state to state and were influenced by the opioid crisis (10).
Table 4.1. Number and rate* of reported cases† of acute hepatitis C, by state or jurisdiction and nationally ― United States, 2013–2017.
| State | 2013 No. |
2013 Rate* |
2014 No. |
2014 Rate* |
2015 No. |
2015 Rate* |
2016 No. |
2016 Rate* |
2017 No. |
2017 Rate* |
|---|---|---|---|---|---|---|---|---|---|---|
| Alabama | 30 | 0.6 | 35 | 0.7 | 70 | 1.4 | 32 | 0.7 | 17 | 0.3 |
| Alaska | — | — | N | N | N | N | N | N | N | N |
| Arizona | U | U | U | U | U | U | U | U | U | U |
| Arkansas | 30 | 1.0 | 13 | 0.4 | 2 | 0.1 | — | — | 1 | 0.0 |
| California | 72 | 0.2 | 73 | 0.2 | 59 | 0.2 | 60 | 0.2 | 103 | 0.3 |
| Colorado | 21 | 0.4 | 33 | 0.6 | 40 | 0.7 | 35 | 0.6 | 42 | 0.7 |
| Connecticut | — | — | — | — | — | — | 17 | 0.5 | 9 | 0.3 |
| Delaware | U | U | U | U | 4 | 0.4 | 25 | 2.6 | 4 | 0.4 |
| District of Columbia | — | — | U | U | U | U | U | U | U | U |
| Florida | 134 | 0.7 | 93 | 0.5 | 126 | 0.6 | 236 | 1.1 | 357 | 1.7 |
| Georgia | 48 | 0.5 | 57 | 0.6 | 84 | 0.8 | 93 | 0.9 | 100 | 1.0 |
| Hawaii | — | — | — | — | — | — | — | — | — | — |
| Idaho | 14 | 0.9 | 6 | 0.4 | 4 | 0.2 | 7 | 0.4 | 8 | 0.5 |
| Illinois | 37 | 0.3 | 27 | 0.2 | 31 | 0.2 | 21 | 0.2 | 39 | 0.3 |
| Indiana | 175 | 2.7 | 122 | 1.8 | 138 | 2.1 | 146 | 2.2 | 191 | 2.9 |
| Iowa | — | — | U | U | U | U | U | U | U | U |
| Kansas | 17 | 0.6 | 28 | 1.0 | 22 | 0.8 | 15 | 0.5 | 19 | 0.7 |
| Kentucky | 226 | 5.1 | 176 | 4.0 | 119 | 2.7 | 103 | 2.3 | 83 | 1.9 |
| Louisiana | 19 | 0.4 | 22 | 0.5 | 24 | 0.5 | 5 | 0.1 | 7 | 0.1 |
| Maine | 8 | 0.6 | 31 | 2.3 | 30 | 2.3 | 25 | 1.9 | 21 | 1.6 |
| Maryland | 53 | 0.9 | 42 | 0.7 | 38 | 0.6 | 35 | 0.6 | 32 | 0.5 |
| Massachusetts | 174 | 2.6 | 228 | 3.4 | 249 | 3.7 | 424 | 6.2 | 327 | 4.8 |
| Michigan | 74 | 0.7 | 78 | 0.8 | 83 | 0.8 | 107 | 1.1 | 152 | 1.5 |
| Minnesota | 47 | 0.9 | 40 | 0.7 | 37 | 0.7 | 51 | 0.9 | 57 | 1.0 |
| Mississippi | U | U | U | U | U | U | U | U | U | U |
| Missouri | 6 | 0.1 | 6 | 0.1 | 8 | 0.1 | 24 | 0.4 | 49 | 0.8 |
| Montana | 16 | 1.6 | 13 | 1.3 | 15 | 1.5 | 20 | 1.9 | 14 | 1.3 |
| Nebraska | 2 | 0.1 | 2 | 0.1 | 8 | 0.4 | 2 | 0.1 | 2 | 0.1 |
| Nevada | 9 | 0.3 | 6 | 0.2 | 12 | 0.4 | 16 | 0.5 | 35 | 1.2 |
| New Hampshire | N | N | N | N | N | N | N | N | 25 | 1.9 |
| New Jersey | 106 | 1.2 | 113 | 1.3 | 130 | 1.5 | 122 | 1.4 | 125 | 1.4 |
| New Mexico | 12 | 0.6 | 16 | 0.8 | 40 | 1.9 | 18 | 0.9 | 16 | 0.8 |
| New York | 131 | 0.7 | 126 | 0.6 | 121 | 0.6 | 179 | 0.9 | 188 | 0.9 |
| North Carolina | 79 | 0.8 | 111 | 1.1 | 144 | 1.4 | 82 | 0.8 | 114 | 1.1 |
| North Dakota | 4 | 0.6 | — | — | — | — | 1 | 0.1 | 1 | 0.1 |
| Ohio | 116 | 1.0 | 105 | 0.9 | 122 | 1.1 | 187 | 1.6 | 159 | 1.4 |
| Oklahoma | 40 | 1.0 | 45 | 1.2 | 35 | 0.9 | 32 | 0.8 | 46 | 1.2 |
| Oregon | 14 | 0.4 | 15 | 0.4 | 13 | 0.3 | 19 | 0.5 | 35 | 0.8 |
| Pennsylvania | 81 | 0.6 | 69 | 0.5 | 129 | 1.0 | 225 | 1.8 | 224 | 1.7 |
| Rhode Island | U | U | U | U | U | U | U | U | U | U |
| South Carolina | — | — | 4 | 0.1 | 5 | 0.1 | 10 | 0.2 | 13 | 0.3 |
| South Dakota | 1 | 0.1 | — | — | — | — | 20 | 2.3 | 19 | 2.2 |
| Tennessee | 98 | 1.5 | 123 | 1.9 | 173 | 2.6 | 150 | 2.3 | 142 | 2.1 |
| Texas | 28 | 0.1 | 47 | 0.2 | 48 | 0.2 | 40 | 0.1 | 35 | 0.1 |
| Utah | 11 | 0.4 | 38 | 1.3 | 30 | 1.0 | 76 | 2.5 | 81 | 2.6 |
| Vermont | 3 | 0.5 | 4 | 0.6 | 1 | 0.2 | 5 | 0.8 | 9 | 1.4 |
| Virginia | 41 | 0.5 | 54 | 0.6 | 52 | 0.6 | 43 | 0.5 | 62 | 0.7 |
| Washington | 63 | 0.9 | 82 | 1.2 | 63 | 0.9 | 62 | 0.9 | 52 | 0.7 |
| West Virginia | 58 | 3.1 | 62 | 3.4 | 63 | 3.4 | 94 | 5.1 | 102 | 5.6 |
| Wisconsin | 40 | 0.7 | 49 | 0.9 | 64 | 1.1 | 103 | 1.8 | 94 | 1.6 |
| Wyoming | — | — | U | U | U | U | U | U | 5 | 0.9 |
| Total | 2,138 | 0.7 | 2,194 | 0.7 | 2,436 | 0.8 | 2,967 | 1.0 | 3,216 | 1.0 |
Source: CDC, National Notifiable Diseases Surveillance System.
* Rate per 100,000 population.
† For case definition, see https://wwwn.cdc.gov/nndss/conditions/hepatitis-c-acute/
—: No reported cases. The reporting jurisdiction did not submit any cases to CDC.
N: Not reportable. The disease or condition was not reportable by law, statue, or regulation in the reporting jurisdiction.
U: Unavailable. The data are unavailable.
Figure 4.2. Rates of reported acute hepatitis C cases, by state compared to the 2017 overall rate of acute hepatitis C — United States, 2016 and 2017.
Source: CDC, National Notifiable Diseases Surveillance System.
Downloads of this slide: PDFpdf icon
HEPATITIS C: SUBGROUP TRENDS FOR ACUTE CASES
Age groups showed different trends in the number of reported acute hepatitis C cases per 100,000 population:
- Rates rapidly increased for young adults aged 20–29 years and aged 30–39 years from 2009 to 2017. These age groups have been most affected by the nation’s opioid crisis (10).
- For the first time since 2014, adults aged 40–49 years experienced a decrease in infection rates from 2016 to 2017.
- Rates increased among adults aged 50–59 years and aged ≥60 years from 2015 to 2017 to the highest rate reported from 2002 through 2017.
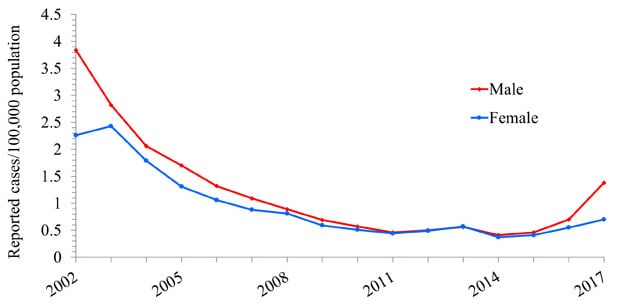
Both males and females experienced an increased rate of reported acute hepatitis C from 2010 to 2017, although the increase for males was more pronounced.
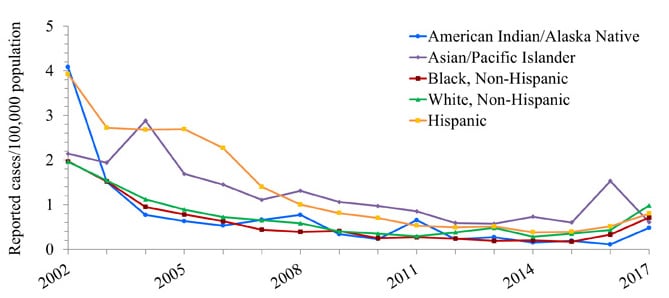
Trends by race/ethnicity revealed the following differences in trends:
- Rates among American Indian/Alaska Natives remain higher than other groups, and the increase since 2010 is more pronounced in this group despite some instability due to the small size of the population.
- Rates among non-Hispanic whites began a marked increase in 2010 that continued through 2017.
- Hispanics and non-Hispanic blacks experienced increases each year from 2014 to 2017.
The rate for Asian/Pacific Islanders remained low and decreased from 2016 to 2017.
Figure 4.3. Rates of reported acute hepatitis C, by age group — United States, 2002–2017.
Source: CDC, National Notifiable Diseases Surveillance System.
Downloads of this slide: PDFpdf icon PowerPointppt icon
Figure 4.4. Rates of reported acute hepatitis C, by sex — United States, 2002–2017.
Source: CDC, National Notifiable Diseases Surveillance System.
Downloads of this slide: PDFpdf icon PowerPointppt icon
Figure 4.5. Rates of reported acute hepatitis C, by race/ethnicity — United States, 2002–2017.
Source: CDC, National Notifiable Diseases Surveillance System.
Downloads of this slide: PDFpdf icon PowerPointppt icon
Table 4.2. Number and rate* of reported cases† of acute hepatitis C, by selected characteristics — United States 2013–2017.
| 2013 No. |
2013 Rate* |
2014 No. |
2014 Rate* |
2015 No. |
2015 Rate* |
2016 No. |
2016 Rate* |
2017 No. |
2017 Rate* |
|
|---|---|---|---|---|---|---|---|---|---|---|
| Total§ | 2,138 | 0.7 | 2,194 | 0.7 | 2,436 | 0.8 | 2,967 | 1.0 | 3,216 | 1.0 |
| Age group | ||||||||||
| 0 – 19 years | 102 | 0.1 | 88 | 0.1 | 99 | 0.1 | 86 | 0.1 | 103 | 0.1 |
| 20 – 29 years | 831 | 2.0 | 918 | 2.2 | 999 | 2.4 | 1,135 | 2.7 | 1,189 | 2.8 |
| 30 – 39 years | 519 | 1.3 | 643 | 1.7 | 682 | 1.7 | 868 | 2.2 | 937 | 2.3 |
| 40 – 49 years | 294 | 0.7 | 282 | 0.7 | 337 | 0.9 | 452 | 1.2 | 441 | 1.1 |
| 50 – 59 years | 189 | 0.5 | 166 | 0.4 | 240 | 0.6 | 264 | 0.6 | 332 | 0.8 |
| 60+ years | 59 | 0.1 | 70 | 0.1 | 77 | 0.1 | 141 | 0.2 | 185 | 0.3 |
| Sex | ||||||||||
| Male | 1,142 | 0.8 | 1,167 | 0.8 | 1,334 | 0.9 | 1,627 | 1.1 | 1,775 | 1.2 |
| Female | 993 | 0.7 | 1,025 | 0.7 | 1,093 | 0.7 | 1,310 | 0.8 | 1,431 | 0.9 |
| Race/ethnicity | ||||||||||
| American Indian/Alaskan Native | 38 | 1.7 | 29 | 1.3 | 39 | 1.7 | 70 | 3.1 | 67 | 2.9 |
| Asian/Pacific Islander | 13 | 0.1 | 11 | 0.1 | 16 | 0.1 | 25 | 0.1 | 23 | 0.1 |
| Black, Non-Hispanic | 75 | 0.2 | 74 | 0.2 | 112 | 0.3 | 130 | 0.3 | 202 | 0.5 |
| White, Non-Hispanic | 1,527 | 0.8 | 1,569 | 0.8 | 1,724 | 0.9 | 2,109 | 1.1 | 2,227 | 1.2 |
| Hispanic | 114 | 0.2 | 124 | 0.2 | 148 | 0.3 | 191 | 0.4 | 234 | 0.4 |
| HHS Region¶ | ||||||||||
| Region 1 | 185 | 2.1 | 263 | 3.0 | 280 | 3.2 | 471 | 3.8 | 391 | 2.8 |
| Region 2 | 237 | 0.8 | 239 | 0.8 | 251 | 0.9 | 301 | 1.0 | 313 | 1.1 |
| Region 3 | 233 | 0.8 | 227 | 0.8 | 286 | 1.0 | 422 | 1.4 | 424 | 1.4 |
| Region 4 | 615 | 1.0 | 599 | 1.0 | 721 | 1.2 | 706 | 1.1 | 826 | 1.3 |
| Region 5 | 489 | 0.9 | 421 | 0.8 | 475 | 0.9 | 615 | 1.2 | 692 | 1.3 |
| Region 6 | 129 | 0.3 | 143 | 0.4 | 149 | 0.4 | 95 | 0.2 | 105 | 0.2 |
| Region 7 | 25 | 0.2 | 36 | 0.3 | 38 | 0.3 | 41 | 0.4 | 70 | 0.6 |
| Region 8 | 53 | 0.5 | 84 | 0.8 | 85 | 0.8 | 152 | 1.4 | 162 | 1.4 |
| Region 9 | 81 | 0.2 | 79 | 0.2 | 71 | 0.2 | 76 | 0.2 | 138 | 0.3 |
| Region 10 | 91 | 0.7 | 103 | 0.8 | 80 | 0.6 | 88 | 0.7 | 95 | 0.7 |
Source: CDC, National Notifiable Diseases Surveillance System.
* Rate per 100,000 population.
† For the case definition, see https://wwwn.cdc.gov/nndss/conditions/hepatitis-c-acute/
§ Numbers reported in each category may not add up to the total number of reported cases in a year due to cases with missing data or, in the case of race/ethnicity, cases categorized as “Other”.
¶ Health and Human Services Regions were categorized according to the grouping of states and US territories assigned under each of the ten Department of Health and Human Services regional offices (https://www.hhs.gov/about/agencies/iea/regional-offices/index.htmlexternal icon). For the purposes of this report, regions with US territories (Region 2 and Region 9) contain data from states only.
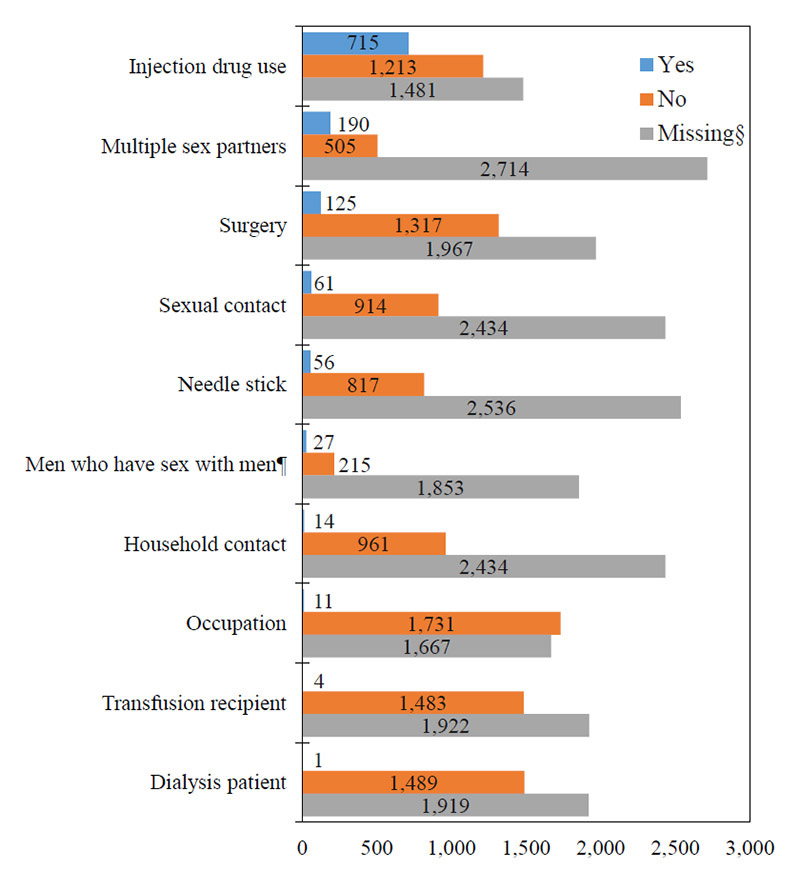
HEPATITIS C: RISK FACTORS FOR ACUTE CASES
Risk data were missing for 48.1% of acute hepatitis C cases reported to CDC in 2017, down from 52.5% in 2016.
The most common risk factors reported in 2017 were injection drug use and multiple sex partners.
Figure 4.6. Availability of information on risk behaviors/exposures* associated with reported cases of acute hepatitis C — United States, 2017.
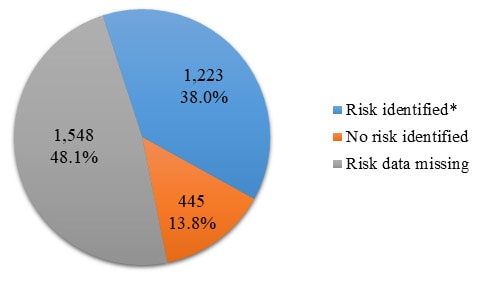
Source: CDC, National Notifiable Diseases Surveillance System.
* Includes case reports indicating the presence of at least one of the following risks 2 weeks to 6 months prior to onset of acute, symptomatic hepatitis C: 1) injection drug use; 2) sexual contact with suspected/confirmed hepatitis C patient; 3) being a man who has sex with men; 4) multiple sex partners concurrently; 5) household contact with suspected/confirmed hepatitis C patient; 6) occupational exposure to blood; 7) hemodialysis patient; 8) received a blood transfusion; 9) sustained a percutaneous injury; and 10) underwent surgery.
Downloads of this slide: PDFpdf icon PowerPointppt icon
Figure 4.7. Reported cases of acute hepatitis C*, by risk behavior/exposure† — United States, 2017.
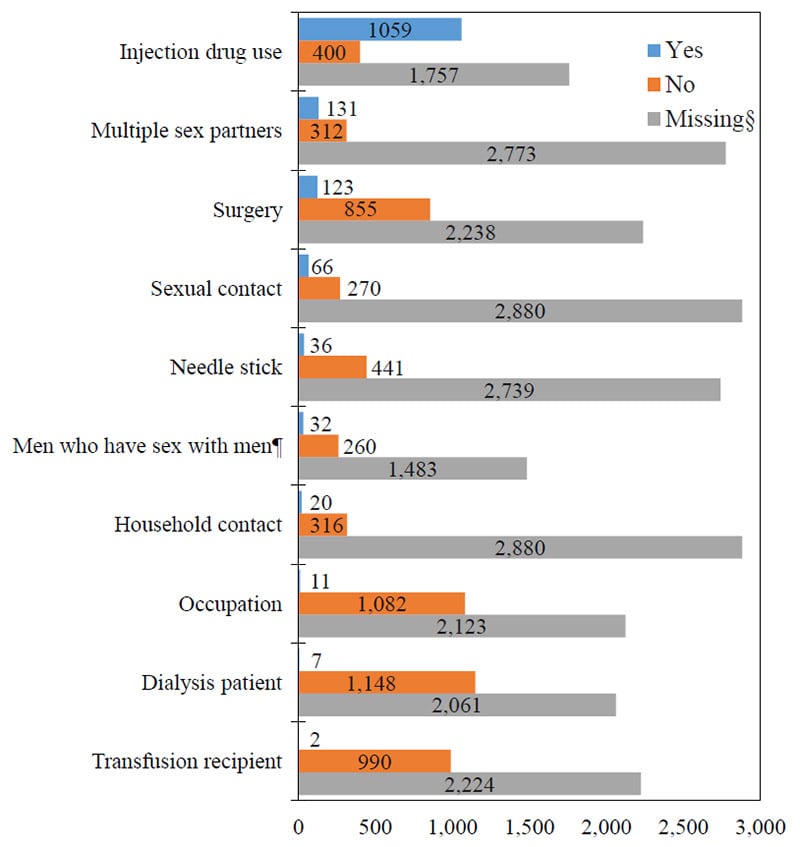
Source: CDC, National Notifiable Diseases Surveillance System.
* A total of 3,216 case reports of acute hepatitis C were received in 2017.
† More than one risk behavior/exposure may be indicated on each case report.
§ No risk data reported.
¶ A total of 1,775 acute hepatitis C cases were reported among males in 2017.
Downloads of this slide: PDFpdf icon PowerPointppt icon
HEPATITIS C: HOSPITALIZATION FOR ACUTE CASES
Hospitalization data were missing for 46.4% of reported acute hepatitis C cases submitted to CDC in 2017, up from 32.8% in 2016.
Of those with hospitalization data, 48.3% (1,029 of 2,130) were hospitalized in 2017, which was higher than 46.3% in 2016.
HEPATITIS C: CHRONIC CASES
In 2017, 38 states submitted 143,286 cases of chronic hepatitis C cases to CDC, which is less than the 148,932 cases submitted by 42 states in 2016.
Table 4.3. Number of newly reported cases* of confirmed chronic hepatitis C and reporting status, by state or jurisdiction, 2017.
| State/Jurisdiction | No. chronic hepatitis C case reports submitted† |
|---|---|
| Alabama | N |
| Alaska | 766 |
| Arizona | U |
| Arkansas | N |
| California | — |
| Colorado | 2,735 |
| Connecticut | 1,760 |
| Delaware | U |
| District of Columbia | U |
| Florida | 18,164 |
| Georgia | 7,376 |
| Hawaii | U |
| Idaho | 834 |
| Illinois | 5,695 |
| Indiana | N |
| Iowa | 1,472 |
| Kansas | 1,197 |
| Kentucky | N |
| Louisiana | 3,340 |
| Maine | 439 |
| Maryland | 4,327 |
| Massachusetts | 4,174 |
| Michigan | 4,751 |
| Minnesota | 1,475 |
| Mississippi | — |
| Missouri | 4,897 |
| Montana | 1,042 |
| Nebraska | 772 |
| Nevada | 106 |
| New Hampshire | 158 |
| New Jersey | 4,601 |
| New Mexico | 783 |
| New York | 8,963 |
| North Carolina | N |
| North Dakota | 581 |
| Ohio | 12,460 |
| Oklahoma | 622 |
| Oregon | 3,389 |
| Pennsylvania | 13,545 |
| Rhode Island | — |
| South Carolina | 3,341 |
| South Dakota | 440 |
| Tennessee | 11,086 |
| Texas | N |
| Utah | 1,113 |
| Vermont | 568 |
| Virginia | 5,228 |
| Washington | 5,126 |
| West Virginia | 3,232 |
| Wisconsin | 2,344 |
| Wyoming | 384 |
| Total | 143,286 |
Source: CDC, National Notifiable Diseases Surveillance System
* For case definition, see https://wwwn.cdc.gov/nndss/conditions/hepatitis-c-chronic/
† Reports may not reflect unique cases.
—: No reported cases. The reporting jurisdiction did not submit any cases to CDC.
N: Not reportable. The disease or condition was not reportable by law, statue, or regulation in the reporting jurisdiction.
U: Unavailable. The data are unavailable.
HEPATITIS C: MORTALITY
In 2017, there were 17,253 death certificates among US residents that listed hepatitis C as the underlying or a contributing cause of death.
- The overall hepatitis C-related mortality rate decreased from 2013 to 2017.
- Decreasing hepatitis C-related mortality rates occurred for adults aged 35 to 64. Other age groups experienced a decrease from 2015 to 2016, but the decrease did not continue in 2017.
- American Indians/Alaskan Natives have historically experienced the highest age-adjusted hepatitis C-related mortality rates, and the rate increased from 2016 to 2017.
- Males have historically experienced a higher age-adjusted hepatitis C-related mortality rate than females, but rates decreased for both sexes from 2016 to 2017.
Only 17 hepatitis C deaths were reported through NNDSS. No additional information, including US resident status, was submitted through NNDSS.
Table 4.4. Number and rate* of deaths with hepatitis C listed as a cause of death† among US residents, by demographic characteristic and year – United States, 2013–2017.
| Demographic characteristic | 2013 No. |
2013 Rate (95% CI) |
2014 No. |
2014 Rate (95% CI) |
2015 No. |
2015 Rate (95% CI) |
2016 No. |
2016 Rate (95% CI) |
2017 No. |
2017 Rate (95% CI) |
|---|---|---|---|---|---|---|---|---|---|---|
| Age Group | ||||||||||
| 0–34 | 121 | 0.08 (0.07-0.10) |
162 | 0.11 (0.09-0.13) |
196 | 0.13 (0.11-0.15) |
164 | 0.11 (0.09-0.13) |
180 | 0.12 (0.10-0.14) |
| 35–44 | 571 | 1.41 (1.30-1.53) |
549 | 1.36 (1.24-1.47) |
592 | 1.46 (1.34-1.58) |
532 | 1.31 (1.20-1.43) |
507 | 1.24 (1.13-1.35) |
| 45–54 | 4,327 | 9.89 (9.59-10.18) |
4,108 | 9.45 (9.16-9.74) |
3,659 | 8.47 (8.20-8.75) |
3,026 | 7.07 (6.82-7.32) |
2,556 | 6.03 (5.80-6.27) |
| 55–64 | 9,879 | 25.13 (24.63-25.62) |
9,976 | 24.89 (24.40-25.38) |
9,678 | 23.68 (23.20-24.15) |
9,011 | 21.73 (21.28-22.18) |
8,275 | 19.70 (19.28-20.13) |
| 65–74 | 2,997 | 11.88 (11.46-12.31) |
3,382 | 12.81 (12.38-13.24) |
4,009 | 14.55 (14.10-15.00) |
4,071 | 14.22 (13.78-14.66) |
4,397 | 14.81 (14.38-15.25) |
| 75+ | 1,423 | 7.30 (6.92-7.68) |
1,431 | 7.21 (6.84-7.58) |
1,431 | 7.08 (6.71-7.45) |
1,288 | 6.25 (5.91-6.59) |
1,329 | 6.28 (5.94-6.61) |
| Race/ ethnicity | ||||||||||
| White, NH (non-Hispanic) | 12,188 | 4.41 (4.32-4.49) |
12,438 | 4.42 (4.34-4.50) |
12,329 | 4.35 (4.27-4.43) |
11,389 | 3.95 (3.88-4.03) |
10,781 | 3.70 (3.63-3.78) |
| Black, NH | 3,520 | 8.33 (8.05-8.62) |
3,535 | 8.12 (7.85-8.39) |
3,602 | 8.13 (7.86-8.40) |
3,360 | 7.42 (7.16-7.68) |
3,262 | 7.03 (6.79-7.28) |
| Hispanic | 2,747 | 7.03 (6.76-7.30) |
2,792 | 6.90 (6.63-7.16) |
2,737 | 6.48 (6.23-6.74) |
2,510 | 5.76 (5.53-6.00) |
2,399 | 5.29 (5.08-5.51) |
| Asian/Pacific Islander | 473 | 2.95 (2.68-3.23) |
419 | 2.43 (2.19-2.67) |
415 | 2.32 (2.09-2.55) |
384 | 2.03 (1.82-2.24) |
368 | 1.86 (1.67-2.05) |
| American Indian/Alaskan Native |
285 | 10.79 (9.50-12.08) |
287 | 10.05 (8.86-11.24) |
324 | 11.45 (10.18-12.73) |
285 | 9.80 (8.63-10.97) |
299 | 10.24 (9.04-11.44) |
| Sex | ||||||||||
| Male | 13,705 | 7.37 (7.24-7.49) |
13,962 | 7.38 (7.26-7.51) |
14,043 | 7.27 (7.15-7.40) |
12,815 | 6.48 (6.36-6.59) |
12,287 | 6.12 (6.01-6.23) |
| Female | 5,614 | 2.86 (2.78-2.94) |
5,651 | 2.82 (2.75-2.90) |
5,523 | 2.71 (2.63-2.78) |
5,278 | 2.54 (2.47-2.61) |
4,966 | 2.32 (2.26-2.39) |
| Overall | 19,319 | 5.03 (4.95-5.10) |
19,613 | 5.01 (4.93-5.08) |
19,566 | 4.91 (4.84-4.98) |
18,093 | 4.42 (4.36-4.49) |
17,253 | 4.13 (4.07-4.20) |
Source: CDC, National Center for Health Statistics, Multiple Cause of Death 1999–2017 on CDC WONDER Online Database. Data are from the 2013–2017 Multiple Cause of Death files and are based on information from all death certificates filed in the vital records offices of the fifty states and the District of Columbia through the Vital Statistics Cooperative Program. Deaths of nonresidents (e.g., nonresident aliens, nationals living abroad, residents of Puerto Rico, Guam, the Virgin Islands, and other territories of the US) and fetal deaths are excluded. Accessed at http://wonder.cdc.gov/mcd-icd10.html on August 23, 2019. CDC WONDER dataset documentation and technical methods can be accessed at https://wonder.cdc.gov/wonder/help/mcd.html#.
* Rates for race/ethnicity, sex, and the overall total are age-adjusted per 100,000 U.S. standard population in 2000 using the following age group distribution (in years): <1, 1–4, 5–14, 15–24, 25–34, 35–44, 45–54, 55–64, 65–74, 75–84, and 85+. Missing data are not included. For age-adjusted death rates, the age-specific death rate is rounded to one decimal place before proceeding to the next step in the calculation of age-adjusted death rates for NCHS Multiple Cause of Death on CDC WONDER. This rounding step may affect the precision of rates calculated for small numbers of deaths.
† Cause of death is defined as one of the multiple causes of death and is based on the International Classification of Diseases, 10th Revision (ICD-10) codes B17.1, and B18.2 (hepatitis C).
Note: Numbers are slightly lower than previously reported for 2013–2016 due to NCHS standards which restrict displayed data to US residents.
MAIN SOURCES
- Centers for Disease Control and Prevention. Hepatitis A Questions and Answers for Health Professionals. Accessed June 11, 2019; Available from: https://www.cdc.gov/hepatitis/hav/havfaq.htm.
- Doshani, M., et al., Recommendations of the Advisory Committee on Immunization Practices for Use of Hepatitis A Vaccine for Persons Experiencing Homelessness. MMWR Morb Mortal Wkly Rep, 2019. 68(6): p. 153-156. Available from doi: 10.15585/mmwr.mm6806a6.
- Centers for Disease Control and Prevention. Hepatitis B Questions and Answers for Health Professionals. May 16, 2019, Accessed June 11, 2019; Available from: https://www.cdc.gov/hepatitis/hbv/hbvfaq.htm.
- Centers for Disease Control and Prevention. Hepatitis C Questions and Answers for Health Professionals. April 9, 2019, Accessed June 11, 2019; Available from: https://www.cdc.gov/hepatitis/hcv/hcvfaq.htm.
- Klevens, R.M., et al., Estimating acute viral hepatitis infections from nationally reported cases. Am J Public Health, 2014. 104(3): p. 482-7. Available from PubMed Central PMCID PMC3953761external icon.
- Patel, E.U., et al., Prevalence of Hepatitis B and Hepatitis D Virus Infections in the United States, 2011-2016. Clin Infect Dis, 2019. Available on 2020-01-30 from PubMed Central PMCID PMC6669285external icon.
- Hofmeister, M.G., et al., Estimating Prevalence of Hepatitis C Virus Infection in the United States, 2013-2016. Hepatology, 2019. 69(3): p. 1020-1031.
- Foster, M., et al., Hepatitis A Virus Outbreaks Associated with Drug Use and Homelessness – California, Kentucky, Michigan, and Utah, 2017. MMWR Morb Mortal Wkly Rep, 2018. 67(43): p. 1208-1210. Available from PubMed Central PMCID PMC6319801external icon.
- National Institutes of Health, National Institute on Drug Abuse. Substance Use in Women. July 2018, Accessed June 11, 2019; Available from: https://www.drugabuse.gov/publications/research-reports/substance-use-in-women/summaryexternal icon.
- Gomes, T., et al., The Burden of Opioid-Related Mortality in the United States. JAMA Netw Open, 2018. 1(2): p. e180217. Available from PubMed Central PMC6324425external icon.
APPENDIX A
Number of acute viral hepatitis cases reported and estimated* with 95% bootstrap confidence intervals — United States, 2010-2017.
| Year | Hepatitis A Reported |
Hepatitis A Estimated* (95% bootstrap confidence interval) |
Hepatitis B Reported |
Hepatitis B Estimated* (95% bootstrap confidence interval) |
Hepatitis C Reported |
Hepatitis C Estimated* (95% bootstrap confidence interval) |
|---|---|---|---|---|---|---|
| 2010 | 1,670 | 3,300 (2,300-3,700) |
3,350 | 21,800 (12,400-53,300) |
850 | 11,800 (9,400-40,300) |
| 2011 | 1,398 | 2,800 (2,000-3,100) |
2,903 | 18,900 (10,700-46,200) |
1,232 | 17,100 (13,600-58,400) |
| 2012 | 1,562 | 3,100 (2,200-3,400) |
2,895 | 18,800 (10,700-46,000) |
1,778 | 24,700 (19,600-84,300) |
| 2013 | 1,781 | 3,500 (2,500- 3,900) |
3,050 | 19,800 (11,300-48,500) |
2,138 | 29,700 (23,500-101,400) |
| 2014 | 1,239 | 2,500 (1,700- 2,800) |
2,791 | 18,100 (10,300-44,400) |
2,194 | 30,500 (24,200-104,200) |
| 2015 | 1,390 | 2,800 (1,900- 3,100) |
3,370 | 21,900 (12,500-53,600) |
2,436 | 33,900 (26,800-115,500) |
| 2016 | 2,007 | 4,000 (2,800–4,400) |
3,218 | 20,900 (11,900–51,200) |
2,967 | 41,200 (32,600– 140,600) |
| 2017 | 3,366 | 6,700 (4,700–7,400) |
3,409 | 22,200 (12,600–54,200) |
3,216 | 44,700 (35,400– 152,400) |
Source: CDC, National Notifiable Diseases Surveillance System.
* To account for under-estimation, a probabilistic model to estimate the true incidence (symptomatic and asymptomatic cases) of acute hepatitis A, B, and C from reported (symptomatic) cases has been published previously (5). The model includes the probabilities of symptoms, referral to care and treatment, and rates of reporting to local and state health departments. The published multipliers have since been corrected by CDC to indicate that each reported case of hepatitis A represents 2.0 estimated cases (95% bootstrap confidence interval [CI], 1.4-2.2), each reported case of acute hepatitis B represents 6.5 estimated cases (95% CI, 3.7-15.9), and each reported case of hepatitis C represents 13.9 estimated cases (95% CI 11.0-47.4).
APPENDIX B
The following revisions have been made to the Surveillance for Viral Hepatitis – United States, 2017 report, originally released on September 10, 2019.
- Update in reporting conditions: All viral hepatitis conditions with no reported cases or characterized as “Not Reportable” or “Data Unavailable” for 2017 in a jurisdiction’s final signed report to CDC’s National Center for Surveillance, Epidemiology, and Laboratory Services (CSELS) were updated according to the following notation used by CSELS:
| Notation | Interpretation |
|---|---|
| — | No reported cases. The reporting jurisdiction did not submit any cases to CDC. |
| N | Not reportable. The disease or condition was not reportable by law, statute, or regulation in the reporting jurisdiction. |
| U | Unavailable. The data are unavailable. |
- The following adjustments were made to case counts and corresponding figures:
| Condition | State | Original 2017 VH Summary |
Current Revision to 2017 VH Summary |
|---|---|---|---|
| Acute hepatitis B | Wyoming | U | 2 |
| Chronic hepatitis B | Connecticut | 75 | N |
| Chronic hepatitis B | Tennessee | 626 | N |
| Chronic hepatitis B | Kentucky | 14 | N |
| Perinatal hepatitis B | New York | 4 | 5 |
| Acute hepatitis C | New Hampshire | U | 25 |
| Acute hepatitis C | Wyoming | U | 5 |
| Chronic hepatitis C | Delaware | 1,224 | U |
| Chronic hepatitis C | Kentucky | 3 | N |
- Updated risk factor information for hepatitis A: The hepatitis A risk factor information was modified to include all cases that were reported as outbreak-associated, including person-to-person outbreaks and foodborne outbreaks.
- Updating viral hepatitis multiplier estimates: Additional information is included about methodology described by Klevens, et al. (including an unpublished erratum and confidence interval calculations used to estimate true incidence of viral hepatitis based on reported cases).