Key points
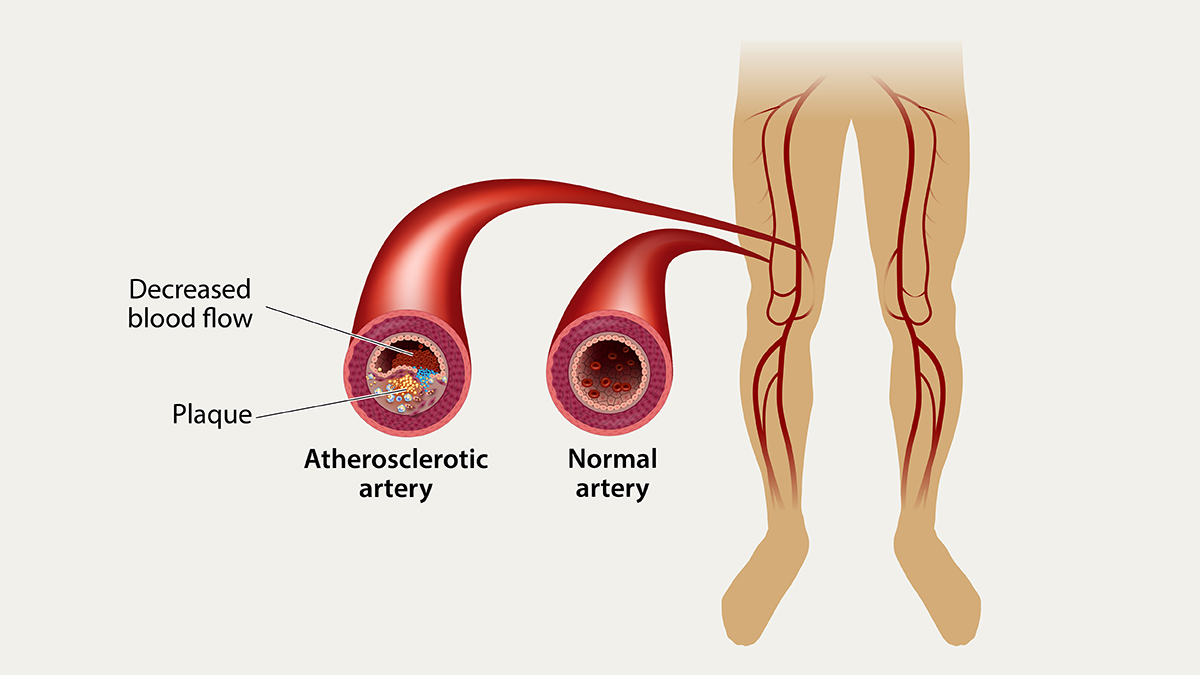
- Peripheral arterial disease (PAD) is the narrowing or blockage of the vessels that carry blood from the heart to the legs.
- Other health conditions and disorders of arteries can mimic the symptoms of PAD.
What it is
Peripheral arterial disease (PAD) in the legs or lower extremities is the narrowing or blockage of the vessels that carry blood from the heart to the legs. It is primarily caused by the buildup of fatty plaque in the arteries. This is called atherosclerosis. PAD can happen in any blood vessel, but it is more common in the legs than the arms.
Signs and symptoms
The classic symptom of PAD is pain in the legs with physical activity, such as walking, that gets better after rest. However, up to 4 in 10 people with PAD have no leg pain.1 Symptoms of pain, aches, or cramps with walking (claudication) can happen in the buttock, hip, thigh, or calf.2
Physical signs in the leg that may indicate PAD include:
Risk factors
- Smoking
- High blood pressure
- Atherosclerosis
- Diabetes
- High cholesterol
- Age above 60 years
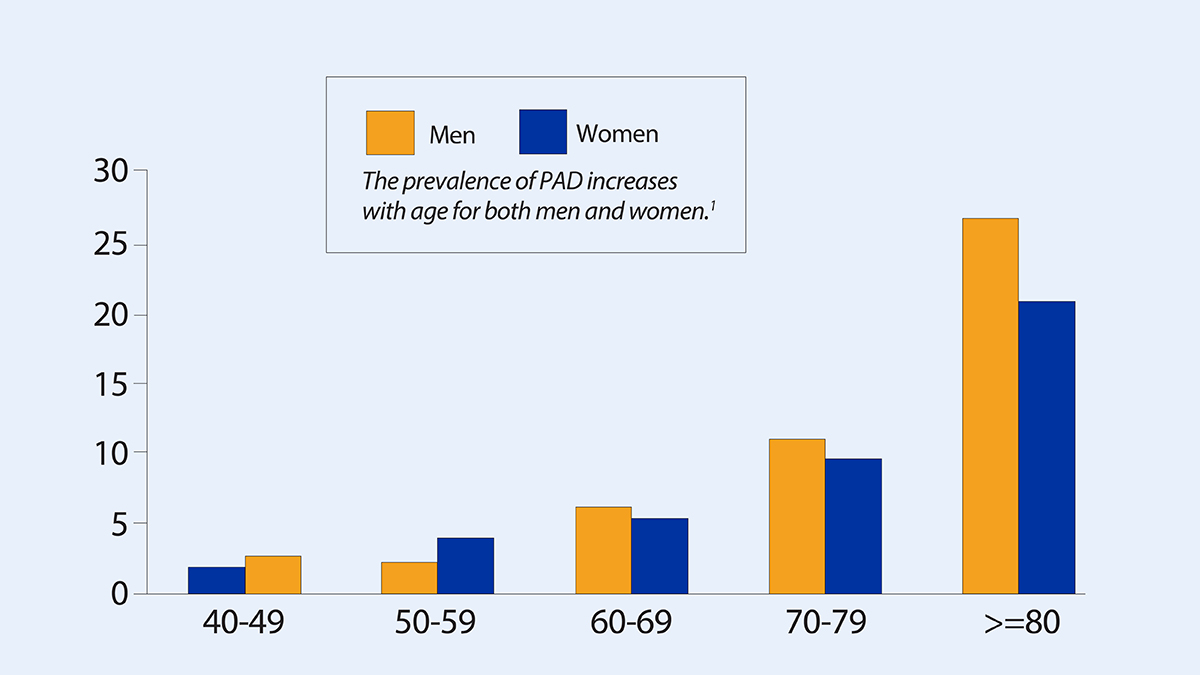
Both men and woman are affected by PAD; however, African Americans people have an increased risk of PAD. Hispanic people may have similar to slightly higher rates of PAD compared with non-Hispanic White people. Approximately 6.5 million people age 40 and older in the United States have PAD.1
Other health conditions and disorders of arteries can mimic the symptoms of PAD, and not all PAD is due to atherosclerosis.23
If you have PAD, you are at risk for developing coronary artery disease and cerebrovascular disease, which could lead to a heart attack or stroke.4
Prevention
Get plenty of physical activity to help prevent PAD or improve symptoms of PAD.2
Do not use tobacco. Smoking increases the risk of PAD and makes PAD symptoms worse.4
Control high blood pressure and manage high blood cholesterol and diabetes.
If you have PAD, participating in supervised exercise training programs can improve and prolong your ability to walk longer distances.
Diagnosis
Prevalence of PAD (%) by age group (years)
If you have symptoms of PAD, your doctor may do an ankle brachial index (ABI). This is a noninvasive test that measures the blood pressure in the ankles and compares it with the blood pressure in the arms at rest and after exercise. Your doctor may also do imaging tests such as ultrasound, magnetic resonance angiography (MRA), and computed tomographic (CT) angiography.123
Treatment and recovery
Your doctor may recommend that you take aspirin or other similar antiplatelet medicines. These medicines could prevent serious complications from PAD and associated atherosclerosis. You may also need to take medicine to reduce your blood cholesterol.24
If you smoke, quit. Talk with your doctor about ways to help you quit smoking.
You may need surgery to bypass blocked arteries.
A supervised exercise program is recommended for people with pain caused by too little blood flow to muscles. Such a program could improve quality of life, and reduce leg symptoms.5
- Virani SS, Alonso A, Aparicio HJ, et al. Heart disease and stroke statistics—2021 update: a report from the American Heart Association. Circulation. 2021;143:e254–e743.
- Creager MA, Loscalzo J. Arterial diseases of the extremities. In: Jameson J, Fauci AS, Kasper DL, Hauser SL, Longo DL, Loscalzo J, eds. Harrison's principles of internal medicine. 20th ed. McGraw-Hill; 2018.
- Cohoon KP, Wennberg PW, Rooke TW. Diagnosis and management of diseases of the peripheral arteries. In: Fuster V, Harrington RA, Narula J, Eapen ZJ, eds. Hurst's The Heart. 14th ed. McGraw-Hill; 2017.
- Gerhard-Herman MD, Gornik HL, Barrett C, et al. 2016 AHA/ACC guideline on the management of patients with lower extremity peripheral artery disease: executive summary: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Circulation. 2017;135(12):e686–e725.
- Gerhard-Herman MD, Gornik HL, Barrett C, et al. 2016 AHA/ACC guideline on the management of patients with lower extremity peripheral artery disease: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. J Am Coll Cardiol. 2017;69(11):e71–e126.
