Appendices
Interpretation of an Epidemic Curve
An epidemic curve (epi curve) shows progression of illnesses in an outbreak over time. Epi curves depict when people became ill by day, week, or month. This information is often shown by the week people became ill. The horizontal axis (x-axis) is the week when a person became ill, also called the week of illness onset. The vertical axis (y-axis) is the number of persons that meet the case definition each week. During ongoing outbreak investigations, the epi curve is updated as new data becomes available. There are several important issues in understanding and interpreting epi curves during ongoing outbreak investigations.
Example of an epidemic (epi) curve from an outbreak investigation of cryptosporidiosis in Milwaukee, 1993.
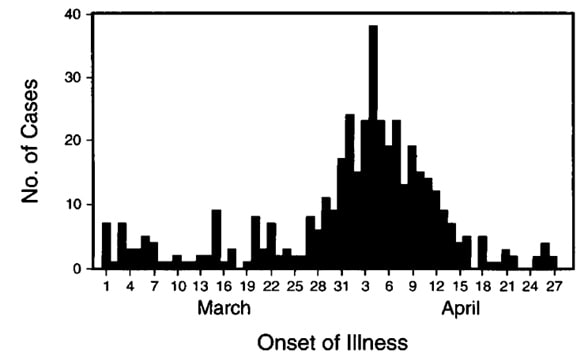
Figure 3. Reported Date of the Onset of Watery Diarrhea during the Period from March 1 through April 28, 1993, in 436 Cases of Infection Identified by a Random-Digit Telephone Survey of the Greater Milwaukee Area.
- There is an inherent delay between the date that an illness starts and the date that the case is reported to public health authorities. This delay can be several weeks; someone who became ill last week is very unlikely to have his or her infection reported to public health authorities by now, and someone who became ill 3 weeks ago may have just had it reported.
- Some background cases of illness are likely to occur that would have happened even without an outbreak. This makes it difficult to say exactly which case is the first in an outbreak. Epidemiologists typically focus on the first recognized cluster (group) of illnesses, rather than the very first case. Due to the inherent reporting delay described above, the cluster is sometimes not detected until several weeks after the persons initially became ill.
- For some cases, the date of illness onset is not known because it takes time before someone from the health department can do an interview to ask for this information. Sometimes, this interview never occurs. If investigators know the date that a specimen from an ill person arrived in the laboratory for testing, they may estimate the date of illness onset as 2 or 3 days before the specimen collection or submission date.
- It can be difficult to determine when cases start to decline because of the reporting delay. This information will become clearer as time passes.
It can be difficult to say when the outbreak is over because of the reporting delay. The delay means that the curve for the most recent 3 weeks always looks like the outbreak could be ending even during an active outbreak. The full shape of the curve is clear only after the outbreak is over.
Confirming Diagnosis
The tables below are intended to assist health departments with developing hypotheses about the possible cause of waterborne diseases and outbreaks during the outbreak investigation. If some of the clinical or exposure information is known, it might direct laboratory testing. Additionally, historical water exposure information might provide clues for developing investigation tools.
| Etiology | Incubation period | Signs and symptoms | Duration of illness | Possible exposure categoriesi | Notes on water exposure |
|---|---|---|---|---|---|
| Bacillus anthracis | 2 days – weeks | Nausea, vomiting, malaise, bloody diarrhea, abdominal pain | Weeks | Water Food Animal contact Environment |
Drinking, recreational: naturally-occurring spores, intentional contamination |
| Campylobacter jejuni | 2 – 7 days | Fever, cramps, vomiting, diarrhea (can be bloody) | 2 – 10 days | Water Food Animal contact Environment |
Drinking: human feces, animal (mammals, poultry, waterfowl) feces |
| Cronobacter spp. | Unknown | Diarrhea possible, sometimes bloody; sepsis; meningitis | Variable; meningitis associated with brain abscesses and prolonged illness | Water Food Environment |
Drinking: powdered infant formula prepared with contaminated water |
| Enterotoxigenic Escherichia coli (ETEC) | 12 – 72 hours | Cramps, watery diarrhea, nausea and vomiting less common | 3 – >7 days | Water Food Animal contact Person-to-person |
Drinking, recreational: human feces, domestic sewage, animal feces |
| Shiga toxin-producing Escherichia coli (STEC) | 1 – 8 days | Abdominal pain, vomiting, watery diarrhea that becomes bloody. Usually no fever. | 5 – 10 days | Water Food Animal contact Person-to-person |
Drinking, recreational: human feces, domestic sewage, animal (cattle) feces |
| Francisella tularensis | 1 – 10 days | Tularemia can present as cutaneous ulcers, fever, chills, muscle aches, painful lymphadenopathy, headache, vomiting, abdominal pain, rash, general malaise. Symptoms may last for several days, remit, and then begin again. Learn more | Up to >3 months | Water Animal contact Environment |
Drinking, recreational: animal (wild mammals) blood and tissue, arthropods |
| Legionella spp. | 2 – 10 days for Legionellosis 24 – 72 hours for Pontiac fever |
Legionnaire’s disease: Pneumonia, diarrhea, cough, vomiting, abdominal pain
Pontiac fever: milder self-limiting flu-like illness (fever, headache, and muscle aches) |
LD: Variable
Pontiac fever: 2 – 5 days |
Water Environment |
Drinking, recreational, other exposures to water: aerosolized mist from cooling towers, evaporative condensers, whirlpools, fountains, large plumbing systems, and respiratory therapy equipment- inadequate disinfection/biofilm removal, dead end systems, lack of maintenance |
| Leptospira spp. | 4 – 19 days Learn more |
Fever, chills, headaches, diarrhea, vomiting, jaundice, kidney failure, stiff neck. Learn more | Variable | Water Food Animal contact Environment |
Drinking, recreational, other exposures to water: animal (rodents, cattle, pigs, dogs, horses, wild animals) urine and body fluids contamination water sources, cisterns exposure |
| Non-tuberculous Mycobacterium spp. | Weeks – months | Insidious onset of cough with purulent sputum, fever, weight loss, night sweats; lymphadenitis, skin, soft tissue, and skeletal infections; disseminated disease in severely immunocompromised hosts, such as AIDS patients. Learn more | Variable | Water Food Animal contact Person-to-person Environment |
Drinking, recreational, other exposures to water: naturally-occurring (fresh/saltwater), biofilm-associated |
| Plesiomonas shigelloides | 24 – 48 hours | Diarrhea (usually watery), vomiting, fever, chills, and abdominal pain. Usually a self-limiting infection. Learn more [PDF – 1 page] | 1 – 7 days | Water Food Animal contact Environment |
Drinking: naturally-occurring (fresh/saltwater), potentially domestic sewage |
| Pseudomonas aeruginosa | 8 hours – >5 days Learn more |
Generalized rash, pustules, ear infection, corneal infection, healthcare-associated (UTI, pneumonia, septicemia, etc.) | Variable | Water Person-to-person Environment |
Drinking, recreational, other exposures to water: biofilm-associated, inadequate cleaning/chlorination- hot tub, pools, and water vessels |
| Salmonella spp. | 6 – 72 hours 7 – 28 days for typhoid/ paratyphoid fevers |
Fever, cramps, vomiting, diarrhea. S. Typhi and S. Paratyphi cause typhoid, characterized by fever, headache, constipation, myalgias, and abdominal pain | 4 – 7 days | Water Food Animal contact Person-to-person Environment |
Drinking: human feces and urine, domestic sewage, animal (poultry, amphibians, reptiles, rodents) feces; farm runoff, meat/poultry processing plant wastes, back siphonage, inadequate disinfection |
| Shigella spp. | 12 hours – 7 days | Fever, cramps, vomiting, tenesmus, diarrhea that can be bloody and mucoid | 4 – 7 days | Water Food Person-to-person Environment |
Drinking, recreational: human feces, domestic sewage; back siphonage, inadequate disinfection |
| Vibrio cholerae (toxin) | 1 – 5 days | Profuse watery diarrhea (rice-water stool), vomiting, reduced skin turgor. Severe dehydration and death can occur within hours | 3 – 7 days | Water Food Environment |
Drinking: human feces, domestic sewage, naturally-occurring (saltwater, warm weather) |
| Vibrio parahaemolyticus | 2 – 48 hours | Cramps, nausea, vomiting, watery diarrhea, wound/ear infections | 2 – 5 days | Water Food Environment |
Recreational: naturally-occurring (brackish/saltwater, warm weather) + open wound |
| Vibrio vulnificus | Around 16 hours | Vomiting, abdominal pain, diarrhea, bacteremia, wound infections. More common in the immunocompromised and in those with chronic liver disease | 2 – 8 days | Water Food Environment |
Recreational: naturally-occurring (brackish/saltwater, warm weather) + open wound + immunosuppression |
| Yersinia enterocolytica and Y. pseudo-tuberculosis | 1 – 7 days | Appendicitis-like symptoms (fever, abdominal pain, diarrhea, vomiting), typically in older children and young adults. Y. pseudotuberculosis may cause scarlitiniform rash | 1 – 3 weeks | Water Food Animal contact Person-to-person Environment |
Drinking: animal (pigs, rodents) feces and urine |
i Please refer to National Outbreak Reporting System (NORS) Guidance document for more information regarding exposure categories.
| Etiology | Incubation period | Signs and symptoms | Duration of illness | Possible exposure categoriesi | Notes on water exposure |
|---|---|---|---|---|---|
| Hepatitis A | 15 – 50 days | Diarrhea, jaundice, flu-like symptoms | Variable 2 weeks- 3 months |
Water Food Animal contact Person-to-person |
Drinking: human feces and urine, domestic sewage; back siphonage, inadequate disinfection |
| Norovirus | 12 – 48 hours | Nausea, vomiting, watery, large-volume diarrhea; fever rare | 1 – 3 days | Water Food Animal contact Person-to-person |
Drinking: human feces and vomit, domestic sewage |
| Rotavirus | 1 – 3 days | Low-grade fever, vomiting, severe watery diarrhea, dehydration, inappetence. Temporary lactose intolerance may occur | 4 – 8 days | Water Food Animal contact Person-to-person |
Drinking, recreational: human feces, domestic sewage |
| Other viral agents (astroviruses, caliciviruses, adenoviruses, parvoviruses) | 12 – 72 hours | Headache, fever possible, nausea, vomiting, diarrhea, malaise, rash | 2 – 9 days | Water Food Animal contact Person-to-person |
Drinking, recreational: human feces, domestic sewage |
i Please refer to National Outbreak Reporting System (NORS) Guidance document for more information regarding exposure categories.
| Etiology | Incubation period | Signs and symptoms | Duration of illness | Possible exposure categoriesi | Notes on water exposure |
|---|---|---|---|---|---|
| Acanthamoeba spp. | Unknown (possibly weeks or months) | Encephalitis: Fever, headache, mental status change, loss of coordination, other neurologic problems Cutaneous: firm, reddish nodules, non-healing ulcers, or abscesses Other symptoms depending on organ system affected. |
Variable (weeks, months, encephalitis is usually fatal.) | Water Environment |
Drinking: used for nasal or sinus rinsing |
| Acanthamoeba keratitis | Unknown (possibly days or weeks) | Eye pain, eye redness, blurred vision, sensitivity to light, sensation of something in the eye, excessive tearing | Variable (weeks, months) | Water Environment |
Drinking: when used for cleaning and storing contact lenses |
| Angiostrongylus cantonensis | 1 week – >1 month | Severe headache, neck stiffness, nausea, vomiting, paresthesias, seizures, other neurologic symptoms | weeks to months | Water Food |
Drinking: whole animal (snail/slug) and body fluids |
| Cryptosporidium | 2 – 10 days | Low-grade fever, cramps, nausea, vomiting, anorexia, prolonged diarrhea (usually watery) | In those with Healthy immune systems, symptoms resolve within 2-3 weeks. Might remit and relapse over weeks to months | Water Food Animal contact Person-to-person Environment |
Drinking/recreational: human feces, domestic sewage, animal (ruminants, cats, rodents) feces, animal waste; inadequate disinfection/filtration |
| Cyclospora cayeanensis | 1 – 11 days | Cramps, nausea, vomiting, anorexia, weight loss, prolonged diarrhea (usually watery), fatigue | May remit and relapse over weeks to months | Water Food |
Drinking: human feces, domestic sewage |
| Entamoeba histolytica | Few days to several months, typically 2 – 4 weeks | Lower abdominal pain, diarrhea (can be bloody), fever, chills, liver abscess | May last weeks to months | Water Food Person-to-person Environment |
Drinking: human feces, domestic sewage; inadequate disinfection/filtration, back siphonage, water and sewer lines in same pits |
| Giardia | 1 – 4 weeks | Cramps, diarrhea (pale, greasy, malodorous stool), flatulence, bloating, vomiting, fatigue, fever | Days to weeks | Water Food Animal contact Person-to-person Environment |
Drinking, recreational: human feces, domestic sewage, animal (beavers, ruminants, birds, dogs, cats, etc.) feces; inadequate disinfection/filtration |
| Naegleria fowleri | 1 – 9 days | Headache, fever, nausea, vomiting, neck stiffness, seizures, altered mental status, hallucinations, coma | 1-18 days. Almost always fatal | Water | Recreational, drinking: Water containing Naegleria fowleri enters the nose |
| Toxoplasma gondii (enteric exposure) |
4 – 28 days | Generally asymptomatic. 20% may develop cervical lymphadenopathy and/or flu-like symptoms. Immunocompromised patients can get CNS disease, myocarditis, or pneumonitis | Months | Water Food Environment |
Drinking: animal (cat) feces; inadequate filtration |
i Please refer to National Outbreak Reporting System (NORS) Guidance document for more information regarding exposure categories.
| Etiology | Incubation period | Signs and symptoms | Duration of illness | Possible exposure categoriesi | Notes on water exposure |
|---|---|---|---|---|---|
| Algal toxins | Few hours – years | May be in stages: vomiting, nausea, vomiting, fever, headache; then liver damage, multiple organ failure. Also, skin irritation, sore throat, muscle and joint pain, mouth ulcers, seizures | Variable | Water Food Environment |
Drinking, recreational: naturally-occurring algal blooms (fresh/brackish/saltwater) |
| Antimony | 5 minutes – 8 hours, depending on dose | Vomiting, metallic taste | Variable | Water Food Environment |
Drinking: natural deposits, industrial contamination (freshwater) |
| Arsenic | 5 minutes – 8 hours, depending on dose | Vomiting, cramps, diarrhea, cancer, skin changes, encephalopathy and peripheral neuropathy with high-dose exposure; lower-dose, chronic exposure may not produce GI symptoms | Several days | Water Food Environment |
Drinking: natural deposits, agricultural/industrial contamination (freshwater); pesticides, back siphonage, indiscriminate disposal |
| Cadmium | Several months | Abdominal pain, salivation, nausea, vomiting, myalgia, kidney damage, lung damage, fragile bones | Variable | Water Food Environment |
Drinking: natural deposits, agricultural/mining/industrial contamination (freshwater); galvanized pipe corrosion, volcanic eruptions, metal refinery discharge, waste battery and paint runoff |
| Copper | Minutes – hours, depending on dose | Nausea, vomiting with blue or green vomitus, liver or kidney damage | Variable | Water Food Environment |
Drinking: natural deposits, agricultural/mining/industrial contamination (freshwater); surface water copper treatment or cooling from power plants, copper pipes and fittings, plumbing material corrosion, fungicides |
| Lead | Weeks – months | Irritability, anorexia, abdominal pain, high blood pressure, kidney problems, Developmental delays, cerebral edema, encephalopathy, seizures, death | Weeks – months | Water Food Environment |
Drinking: plumbing/water pipe corrosion (freshwater) |
| Nitrite | 1 – 2 hours Variable, depending on dose and concentration |
Headache, dizziness, loss of consciousness, nausea, vomiting, cyanosis (blue baby syndrome- bluish skin and brownish blood) | Hours – days | Water Food Environment |
Drinking: natural-occurring, animal feces, agricultural contamination (freshwater); fertilizer |
| Pesticides (organophosphates or carbamates) | Minutes – few hours | Headache, nervousness, twitching, convulsions, miosis, cramps, nausea, vomiting, diarrhea, chest pain, cyanosis | Weakness/ neuropathy may last weeks |
Water Food Environment |
Drinking: agricultural contamination; back siphonage, seepage following soil-foundation spraying |
| Sodium fluoride | Minutes – months | Salty/soapy taste, numbness in mouth, vomiting, diarrhea, dilated pupils, spasms, pallor, shock, collapse; severe hypocalcemia, hyperkalemia, bone disease | Variable | Water Food Environment |
Drinking: natural deposits, water treatment plant malfunction |
i Please refer to National Outbreak Reporting System (NORS) Guidance document for more information regarding exposure categories.