Respiratory Disease Season Outlook

CDC released an update to this outlook on February 8, 2024. View the latest update below.
CDC anticipates that total hospitalizations for COVID-19, influenza and RSV will decline but remain elevated into February. We have moderate confidence in this assessment because current levels of emergency department visits for viral respiratory illnesses are stable or decreasing across most areas of the country. However, further increases in one or more viral respiratory diseases are still possible and influenza has recently been increasing in some parts of the country and in some key indicators. Hospitalization rates observed during December 2023 (the highest values observed so far this season) reached levels similar to those observed last season, aligning with scenarios described in the September assessment1.
- COVID-19 surveillance data, hospital admission forecasts, and growth estimates indicate that COVID-19 activity remains elevated but has decreased and is likely to continue decreasing into February. We continue to track variants of COVID-19, including the JN.1 variant. The emergence of a COVID-19 variant that causes more severe illnesses could change our assessment.
- After a few weeks of declining or stable trends, influenza activity is increasing in parts of the country and in some key indicators. Hospital admission forecasts and growth estimates indicate that influenza activity will remain elevated into February. CDC continues to monitor for an additional period of increased influenza activity.
- RSV activity remains elevated but is decreasing nationally. The national per capita hospitalization rate remains lower than the peak for last season. Other indicators, such as emergency department visits with diagnosed RSV and RSV test positivity, are also decreasing.
We do not anticipate producing additional respiratory disease outlooks during the remainder of the 2023-2024 season. We continue to monitor respiratory diseases and will update this outlook should we identify any unusual events, such as significant resurgence of disease.
Vaccination remains the best way to protect yourself and your loved ones against serious outcomes of these viral respiratory illnesses. Vaccination is especially important for people at increased risk for severe disease, including infants, older adults, pregnant people, and people with certain disabilities or underlying medical conditions. For COVID-19 and influenza, prescription antiviral medications are an important addition to vaccination for people at higher risk of serious illness. These antivirals should be started as early as possible.
You can take more actions to protect yourself and others from viral respiratory illnesses. Learn about how to reduce your risk of getting sick from these viruses.
1The combined weekly hospitalization rate for COVID-19 and influenza from CDC’s National Healthcare Safety Network during the week of December 30, 2023, was 87.5% of last year’s peak (16.8 vs 19.2 admissions per 100,000).
CDC expects the upcoming fall and winter respiratory disease season will likely have a similar number of total hospitalizations compared to last year. As with last year, the number of hospitalizations is expected to be higher than that experienced prior to the COVID-19 pandemic, when severe disease was caused primarily by the influenza virus and the respiratory syncytial virus (RSV).
However, it remains possible that hospitalizations this season may be higher than last year, with more widespread illness and healthcare system strain. This increase could result from the emergence of a new COVID-19 variant with an increased ability to evade the body’s prior immunity, or from a severe influenza season combined with COVID-19 and RSV waves that are similar to last year, or, as we saw last year, an increase in RSV infections. A key factor is the timing of the peak number of hospitalizations associated with each disease and whether those peaks coincide.
This outlook is based on expert judgment, historical data, and scenario modeling for COVID-19. We have low to moderate confidence in this assessment because of uncertainties in anticipating the timing of when diseases will peak and levels of disease.
Vaccination remains the best way to protect yourself and your loved ones against serious outcomes of these diseases. Vaccination is especially important for people who are at higher risk of developing serious complications.
CDC is offering this outlook to provide decision-makers information to assist with public health preparedness planning, including potential surges in hospital demand.
Infectious disease experts and scenario models provide evidence that this season is likely to bring a moderate COVID-19 wave, causing around as many hospitalizations at the peak as occurred at last winter’s peak.
- There is widespread, population-level protective immunity to COVID-19 from prior infections and/or vaccinations, making it unlikely that COVID-19 will cause very large waves of severe disease or hospitalization, according to modeling by the COVID-19 Scenario Modeling Hub.
- COVID-19 could peak earlier than last season, however, because of limited summer activity compared to past years.
Experts anticipate that the influenza season will fall in the typical range of severity. However, even typical seasons vary widely in the number of illnesses, hospitalizations, and deaths.
- Experts do not believe that the COVID-19 pandemic—and associated interventions and behavior changes—will continue to have a major impact on influenza transmission, following reduced influenza activity in 2020-2021 and an early peak for the 2022-2023 season.
Experts anticipate that RSV is likely to return to normal season patterns following a severe season last year.
- Last year’s season likely elevated population immunity to typical levels, which had previously been lower because of reduced RSV circulation early in the COVID-19 pandemic.
- There are also new RSV prevention tools available, which could potentially decrease hospital burden. These include vaccines for those aged 60 years and older and an immunization for infants.
High immunization uptake could reduce the number of hospitalizations substantially. i,ii,iii,iv It is difficult to predict the size and timing of peak activity for each disease, as well as how the timing might overlap. These factors will affect the level of strain on the healthcare system. There is also considerable uncertainty about the level of vaccine uptake, particularly for the RSV vaccine for older adults and RSV immunization for infants that are new this season.
The COVID-19 pandemic changed patterns for influenza and RSV circulation, and there could be lingering effects on population immunity or behavior that continue to affect influenza or RSV levels this season. Other disease-specific uncertainties include the following:
- The virus that causes COVID-19 is constantly changing, and a new variant could emerge which is less effectively mitigated by immunity from past infections or from existing vaccines and treatments. COVID-19 has not yet occurred as a regular seasonal disease, so we do not yet fully understand how the timing and magnitude of waves will vary.
- We do not yet know which influenza viruses will predominate, which can affect the number of severe illnesses and hospitalizations. We also do not yet know how effective vaccines will be against the predominant viruses.
- Particularly for RSV, we have less precise estimates for the burden of illnesses and hospitalizations data on past seasons to inform expectations for this fall/winter.
CDC developed two hypothetical scenarios for the peak hospital burden of COVID-19, influenza, and RSV. These scenarios illustrate how the additional burden from COVID-19 during a moderate season for the three respiratory diseases may generate more hospital demand – potentially resulting in hospital strain – than a severe influenza and RSV season prior to the emergence of COVID-19 (Figure 1).
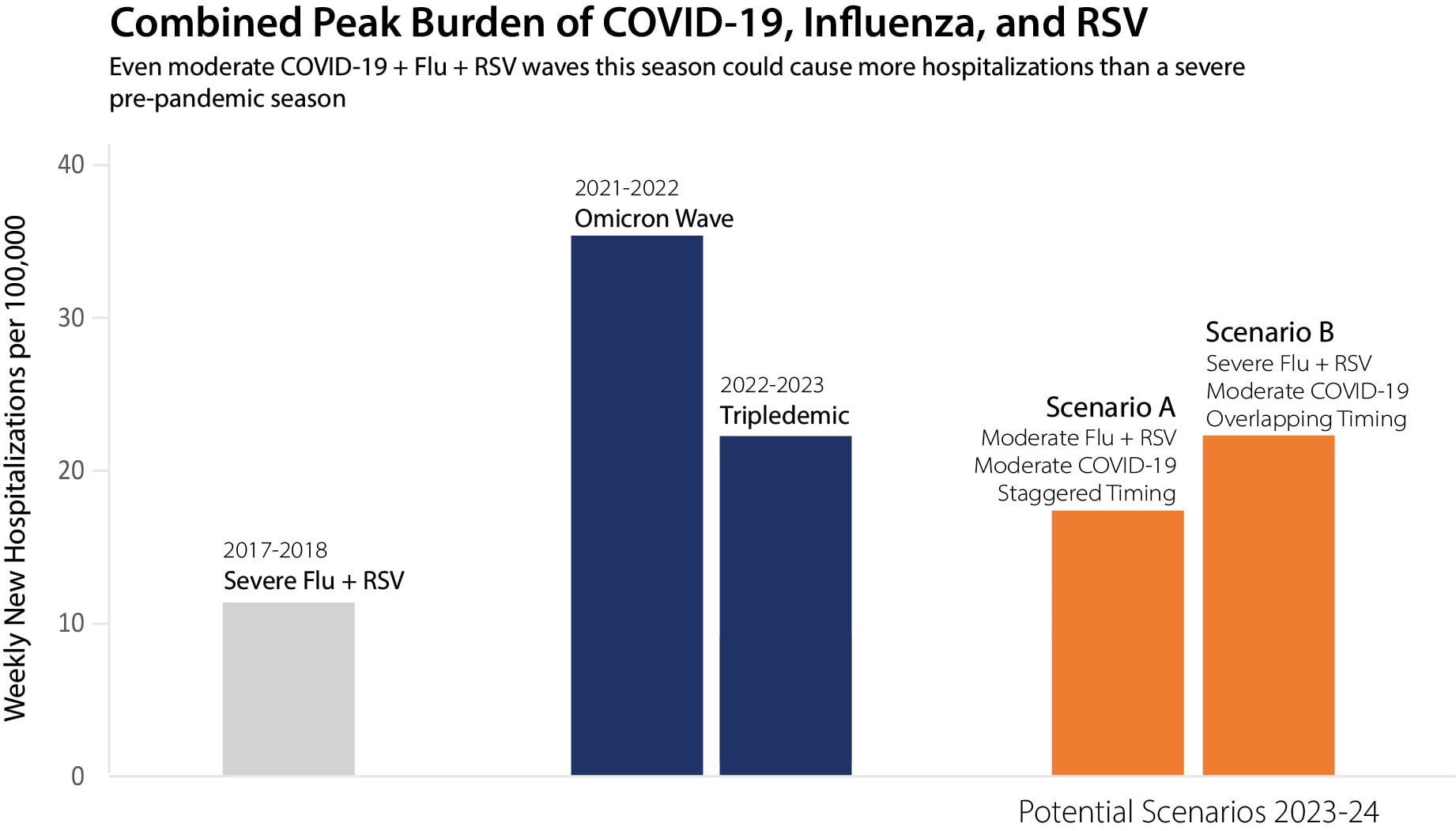
The graph above shows that a moderate influenza and RSV season with a moderate COVID-19 wave (the combined orange bar on the left) could generate more hospital strain than a severe, pre-COVID-19 influenza and RSV season (the light gray bar on the left). While we cannot predict the precise timing and impact of these three pathogens each season, these are two plausible scenarios.
- In scenario A, we combine a moderate past season peak for influenza and RSV equal to 2019-20 with a moderate COVID-19 wave equal to winter 2022-23. We also shift the timing of the COVID-19 wave so that the peak occurs three weeks prior to the peak of influenza + RSV hospitalizations. In this scenario, the peak hospitalization rate is roughly 20% lower than the 2022-2023 peak. The peak is higher than the level for a severe season of influenza and RSV combined, as illustrated by Scenario B.
- In scenario B, we combine a severe past season peak for influenza and RSV equal to 2017-18 with a moderate COVID-19 wave equal to winter 2022-23. We also shift the timing of the COVID-19 wave so that its peak occurs in the same week as influenza + RSV peak hospitalizations. In this scenario, the peak hospitalization rate is similar to that of the 2022-2023 season and slightly higher than the peak hospitalization rate for COVID-19 alone in the 2020-2021 season.
At this time, we do not know enough about BA.2.86 to assess its potential impact on the upcoming disease season, though the scenarios outlined here likely account for the emergence of a wide range of variants.
CDC is continually monitoring for new variants and studying their potential impact on public health. Scientists are evaluating the effectiveness of the updated COVID-19 vaccine.
CDC’s current assessment is that this updated vaccine will be effective at reducing severe disease and hospitalization. At this point, there is no evidence that this variant is causing more severe illness. That assessment may change as additional scientific data are collected.
We are monitoring carefully and will update this outlook as we learn more.
- CDC has a robust system of domestic and global monitoring and early warning systems, which include tracking data on hospitalizations, emergency department visits, laboratory tests, genomic sequencing, and wastewater testing.
- CDC is also working to improve real-time analysis and forecasting for these diseases. CDC produces regular influenza forecasts throughout the season. For COVID-19, we are producing regular forecasts and working to improve these predictions through integrating past data on COVID-19 activity to understand seasonal variation in epidemic timing and magnitude.
CDC will update this outlook as we learn more about respiratory virus activity this season.
This outlook was prepared by CDC’s Center for Forecasting and Outbreak Analytics (CFA) and National Center for Immunization and Respiratory Diseases (NCIRD).
iii Economics of Vaccinating U.S. Adults greater than or equal to 60 years old against RSV (cdc.gov)
iv CDC internal modeling on hospitalizations averted by COVID-19, influenza, and RSV immunizations.